PCC 8.15 Release
In the first quarter of 2021, PCC will release version 8.15 of our electronic charting and practice management software to all PCC users.
PCC 8.15 includes group chat, improved user management, COVID-19 vaccine support, improvements to preparing an encounter for billing, and much more!
Watch a Video Series: Want to see videos about the updates in this release? Watch the PCC 8.15 Release Video Series.
Implementation: PCC 8.15 includes features that require configuration and user-specific software training. Read about the features below and then review the PCC 8.15 Migration Considerations article.
Read below to learn more, and contact PCC Support for information about these new features or about any PCC product or service.
Chat With Groups in Your Office
When you want to chat with a group of PCC EHR users at your practice, select a chat group and enter your message.
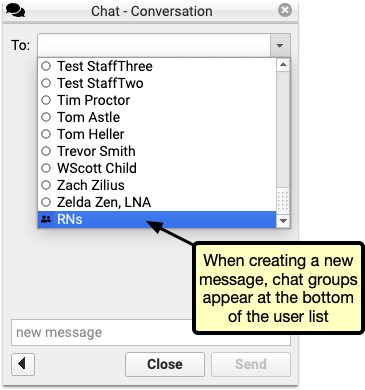
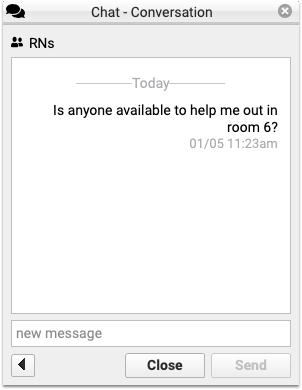
The message appears to the whole group, and any replies will be marked with the replying user’s name.
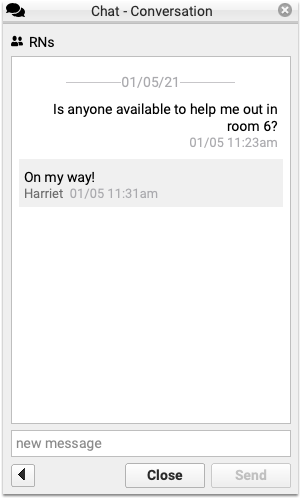
Set Up Your Practice's Chat Groups: You can create and edit chat groups through the User Administration tool. See PCC 8.15 Migration Considerations to learn how.
Configure Which PCC EHR Queues Appear for Each User
Your practice can define which PCC EHR queues will appear when a user logs in. For example, a staff member at the front desk may not need to see prescription renewals or signing. Their PCC EHR screen could look like this:
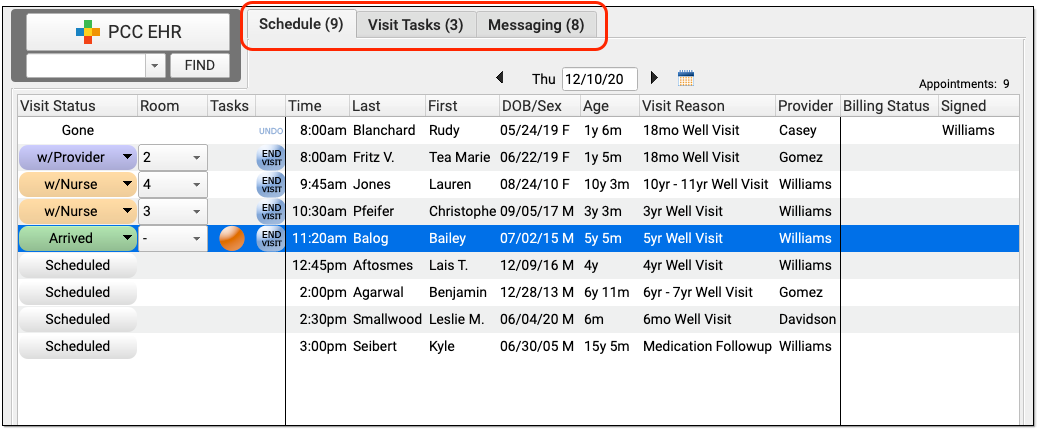
And a biller may only need to review today’s schedule and messages in order to post charges:
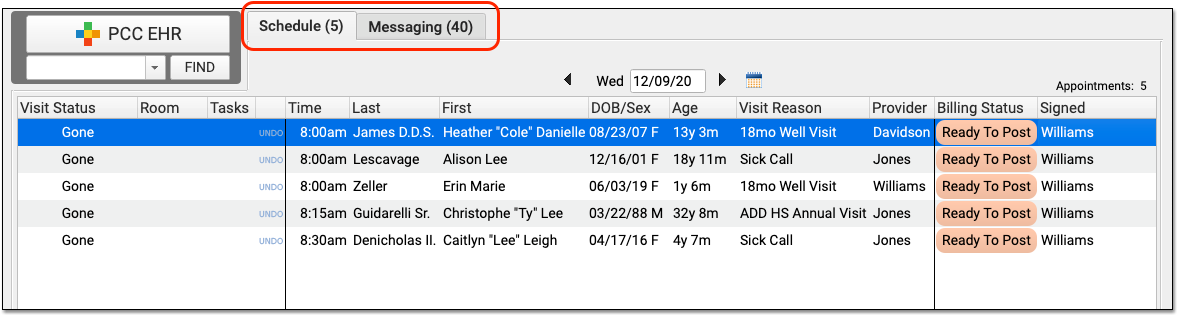
Use the User Administration tool to define which roles will see each PCC EHR queue.
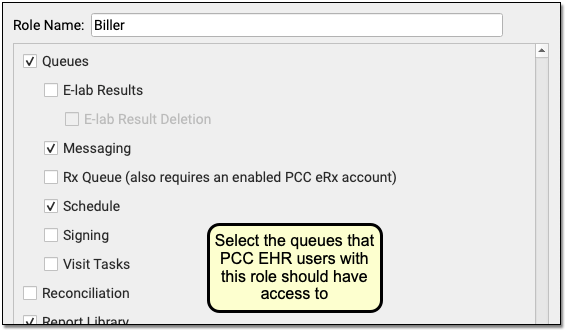
Read the PCC 8.15 Migration and Implementation guide to learn more.
By fine-tuning which queues appear for each user role in your practice, you can make PCC EHR easier to use and you can control who has access to different functions in PCC EHR.
All Users Will Still Have Access After the PCC 8.15 Update: Configurable queues are brand new! The PCC 8.15 update won’t hide any queues. When users log in after the update, they will see the same queues they have always seen. After the update, your practice’s office manager or system administrator can configure roles for your users, and also set expectations about the change. If you need help, contact PCC Support.
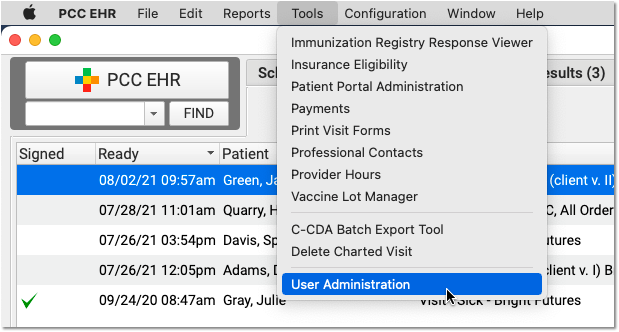
Manage All Usernames and Passwords in PCC EHR
PCC 8.15 automatically syncs authentication between PCC EHR and the Practice Management window. Your practice can use PCC EHR’s User Administration tool to manage user accounts for all PCC products.
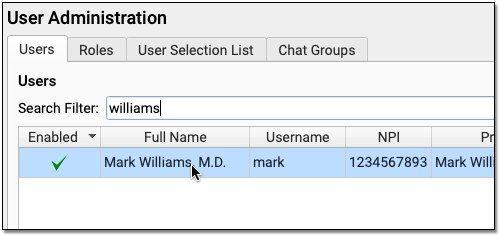
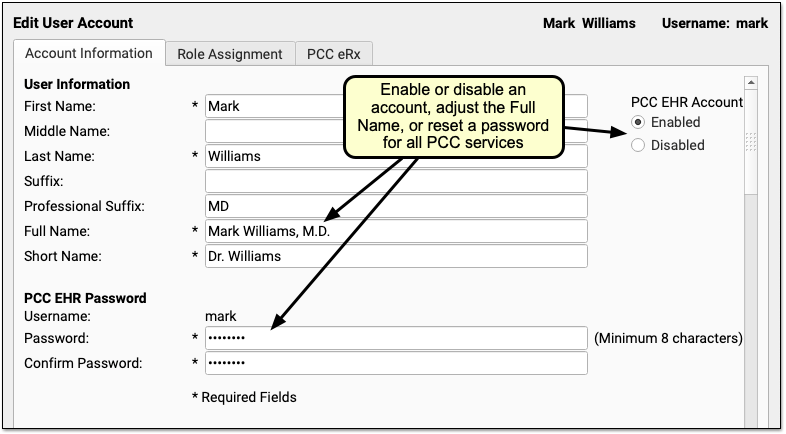
When you enable or disable an account, adjust a Full Name, or change a password, the changes will affect all of PCC’s products for the user, including both Secure Connect access, PCC email accounts, and the Practice Management window.
When you create a new user account, PCC EHR will automatically create accounts and sync the authentications that each user needs.
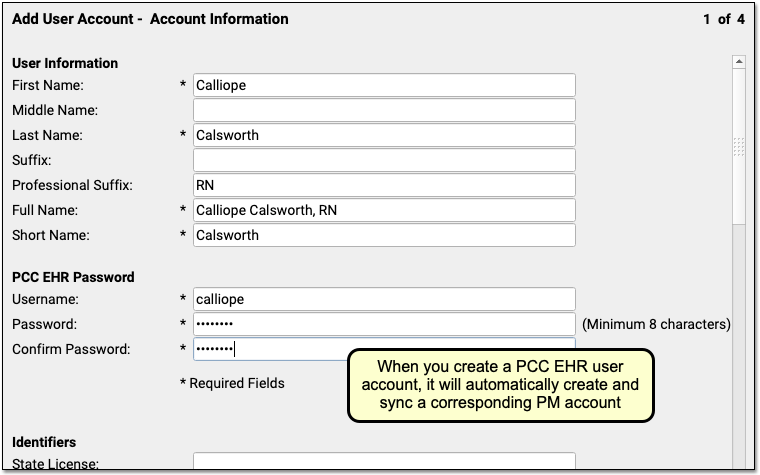
If a user updates their own password in PCC EHR, that will automatically update their password for all PCC products.
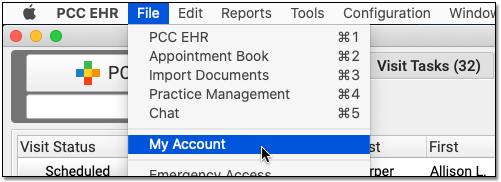
The new “one stop shopping” for user account administration in PCC 8.15 will save time and reduce username and password problems, especially for your staff who access both PCC EHR and the advanced billing tools found in the Practice Management window.
Prepare for Password and Username Updates: While the password and username transition will be seamless for most users at your practice, there are special circumstances which may lead to confusion after the PCC 8.15 update. Please have your practice’s system administrator take a look at the Prepare for Username and Password Updates Across PCC Products and Services section of the PCC 8.15 migration article.
Configure, Order, Administer, and Track COVID-19 Vaccines in PCC EHR
In December and January, PCC applied several updates to your system to support COVID-19 vaccines. The PCC 8.15 software update includes further adjustments to improve COVID-19 vaccine support. Your practice can configure, order, administer, and track all available COVID-19 vaccines in PCC EHR.
For a complete guide, read COVID-19 Vaccines in PCC EHR: Configure, Order, Administer, and Track.
Here’s a list of the related updates that arrived during the PCC 8.15 release cycle:
-
CVX and MVX for Pfizer, Moderna, Janssen and AstraZeneca Vaccines: Mid-release updates to your system added CVX codes 208 and 207 for Pfizer-BioNTech and Moderna COVID-19 vaccines. PCC 8.15 adds CVX 212 and 210, for Janssen (J&J) and AstraZeneca. The MVX table is also updated to support new codes for Pfizer-BioNTech, Janssen, and AstraZeneca (PFR, JSN, and ASZ).
-
VIS Entries for Pfizer, Moderna, Janssen and AstraZeneca: There are no VIS forms for the COVID-19 vaccines. In their place, the CDC has worked with manufacturers to provide EUA Fact Sheets. PCC added VIS table entries for the EUA Fact Sheets for both the Pfizer-BioNTech and Moderna COVID-19 vaccines to all practice systems in a mid-release patch. PCC 8.15 adds entries for Janssen (J&J) and AstraZeneca EUA Fact Sheets for their COVID-19 vaccines.
-
0.3mL Dosage Support for Pfizer COVID-19 Vaccine: PCC 8.15 adds support for a 0.3mL dose in vaccine record keeping, which is the dosage used for the Pfizer-BioNTech COVID-19 vaccine. Prior to this update, the vaccine could be recorded with an “unspecified” dose. After the update, your practice may want to adjust your configuration and update those records if you administered any Pfizer-BioNTech COVID-19 vaccines.
-
Immunization Forecasting for Pfizer and Moderna COVID-19 Vaccines: PCC’s Immunization Forecasting partner, STC, updated the underlying schedule logic to support both the new Pfizer-BioNTech and Moderna mRNA vaccines, when identified by the 208 and 207 CVX codes.
-
Immunization Forecasting with an Unspecified COVID-19 Vaccine: Your practice can optionally add a “COVID-19 (Unspecified)” vaccine to your system, using CVX 213, in order to record a shot on a patient’s record when you do not know the specific vaccine. A recent STC update to Immunization Forecasting logic allows for that vaccine to be valid. For example, an unspecified COVID-19 vaccine can report as valid for Dose 2 of a vaccine schedule that began with a Pfizer-BioNTech or Moderna vaccine. (Note that an unspecified vaccine entry should not used to record immunization administration.)
-
Vaccine Family 33 for Immunization Forecasting: PCC 8.15 adds the vaccine code family of 33, for COVID-19, to the underlying data structure for immunization forecasting. This allows Immunization Forecasting to display a line and label for COVID-19 forecasting.
Details on Forecasting for COVID-19: PCC 8.15 will not forecast an expected or missing immunization for COVID-19 until a patient has received a first dose in a two-dose series. Additionally, we expect Immunization Forecasting for COVID-19 vaccination to change in the coming year. Recent updates to your system lay the groundwork for forecasting, but COVID-19 forecasting results at this time may not produce the expected result.
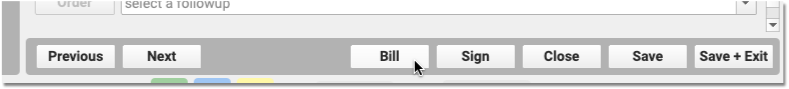
Prepare an Encounter for Billing More Easily
PCC 8.15 includes two improvements to how your clinicians prepare encounters for billing in PCC EHR. Linked codes from orders and the consolidation of duplicate diagnoses will save time and reduce errors.
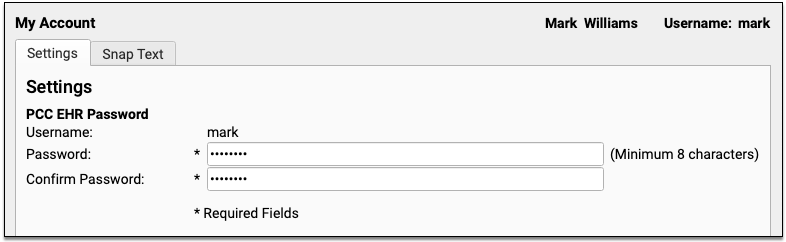
Automatically Link Diagnoses and Procedures From Orders
When you create an order for a patient, the correct diagnoses and procedures can now appear linked when you prepare the encounter for billing.
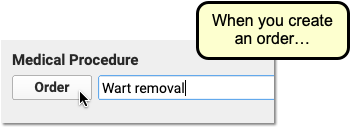
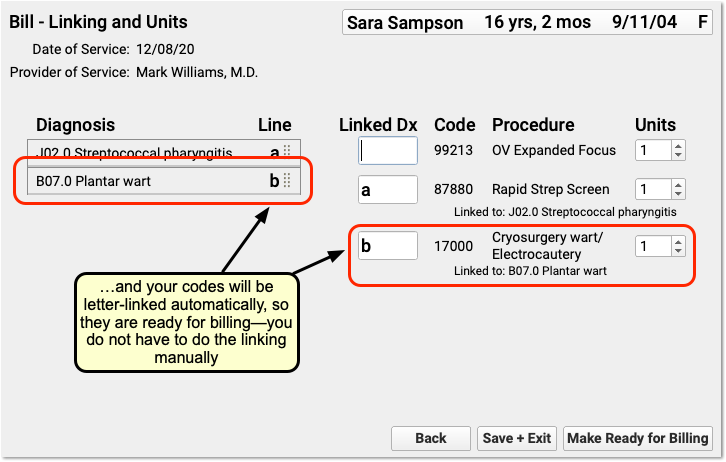
When a user creates an order in PCC EHR, it can automatically add diagnoses and procedures to the Bill window (also called the electronic encounter form). For example, you might configure a Wart Removal order to add both a plantar wart diagnosis and a cryosurgery procedure code for billing. In PCC 8.15, these codes will automatically be linked and ready for charge posting.
Billing codes for diagnoses and procedures are based on your practice configuration. Once you’ve set up your orders, both your clinician and biller will save time, as they will not need to manually indicate which diagnoses correspond to the billing procedures for the order.
Configure Your Orders: Your practice can configure exactly which diagnoses and procedures are triggered for each order. Use the Billing Configuration tool to add diagnoses and procedures to orders. Use the Protocol Configuration tool to specify which orders appear on each chart note.
No More Duplicate Diagnoses on the Bill Screen
When you prepare an encounter for billing, you will no longer see duplicate diagnoses from orders. For example, when your practice orders multiple immunizations, PCC EHR will consolidate the Z23 diagnosis into a single entry.
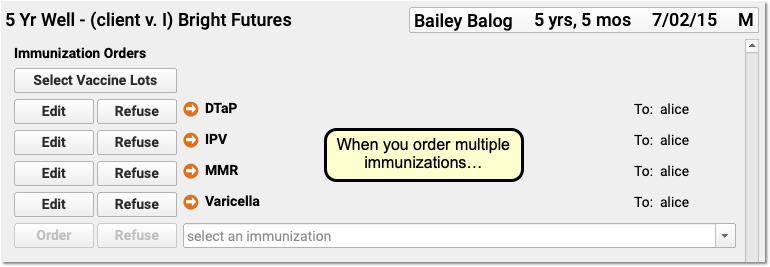
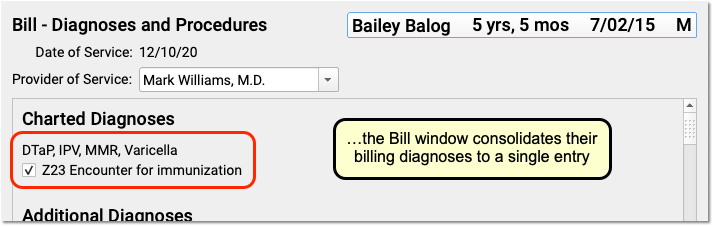
In the Bill window, all orders that have the same configured diagnosis will appear on a single line. Based on your practice’s configuration, the diagnosis will also be automatically linked to the procedure codes you use to bill each order.
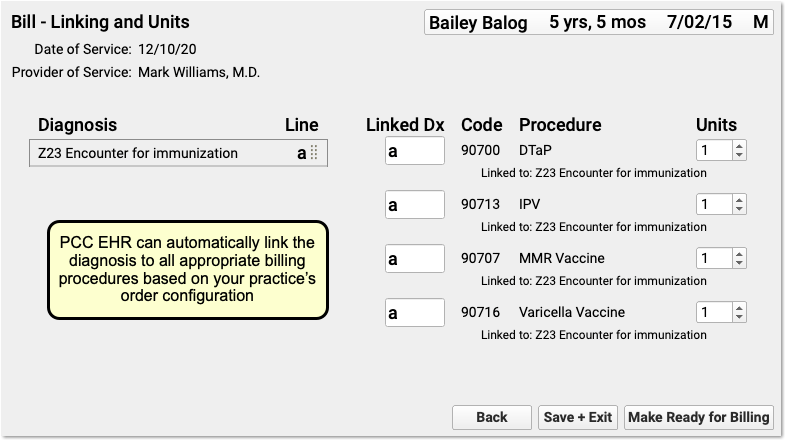
If the clinician needs to link an additional procedure or make other changes, they can spot the diagnosis more quickly and link it without the confusion of seeing duplicate entries.
After the clinician clicks “Make Ready for Billing”, Post Charges in PCC EHR will also deduplicate and only display the diagnosis once, making it easier for the biller to review details and post charges.
Deduplication is Only in PCC EHR: If your practice still uses the post charges tool in the Partner Practice Management system, sometimes called chuck or checkout, billers may still see a diagnosis multiple times. The older charge posting program does not deduplicate diagnoses.
Update an Encounter’s Billing Provider Separately from the Scheduled Appointment Provider
In PCC 8.15, you can schedule an appointment for one provider and then easily select a different provider for billing. Your practice could potentially use different clinicians when you schedule, see the patient, and bill for an encounter.
When you need to change the scheduled appointment provider for an encounter, you can adjust it in the Appointment Book, or right at the top of the chart note:
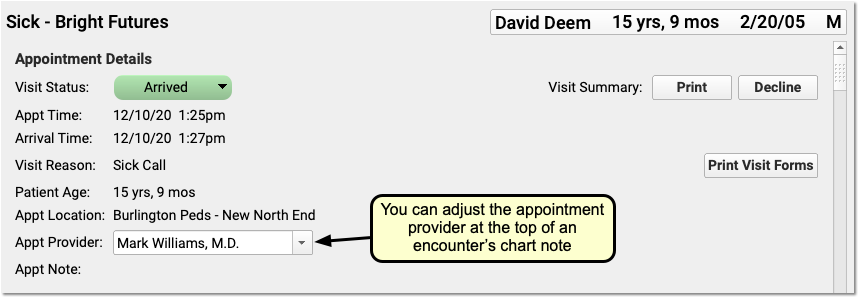
When you need to select a different billing provider, you can make that change at the top of the Bill window (the electronic encounter form) when you prepare the encounter for billing.
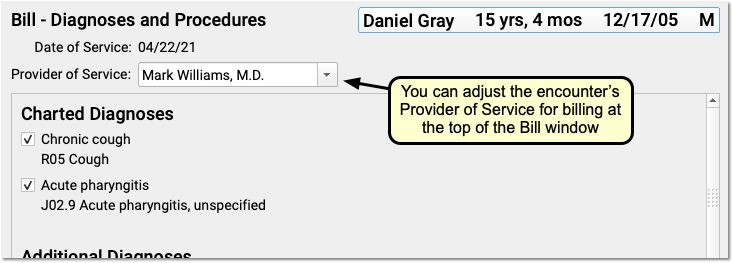
Alternatively, the biller can make that adjustment later, when they post charges.
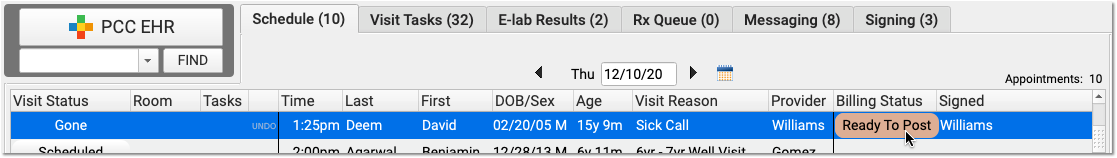
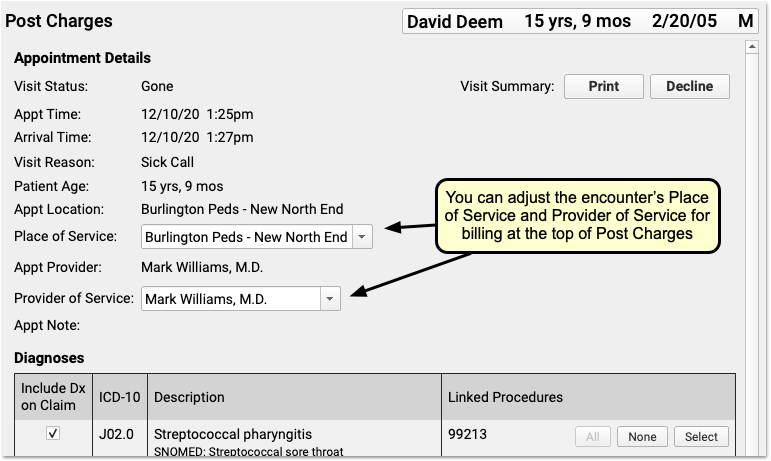
You can change the billing provider without changing the scheduled appointment provider. PCC EHR’s records will display both the Appointment Provider and the Provider of Service in the patient’s Billing History.
When Would I Need to Change the Provider for an Encounter?: Your practice might schedule a stand-in “Flu” provider in the Appointment Book. Then on the day of the encounter, you might change the scheduled clinician for the appointment to Nurse John, who gives the patient the flu shot. Afterwards, when you prepare the encounter for billing, you might define the supervising Provider of Service as the credentialed M.D., Dr. Williams. PCC supports these and other workflows, and in PCC 8.15 you can more easily adjust the provider of service while not altering the appointment provider.
Apply Past Credits When You Post Charges in PCC EHR
When you post charges, PCC EHR will display any credits on the patient’s Billing Account in the Payments component.
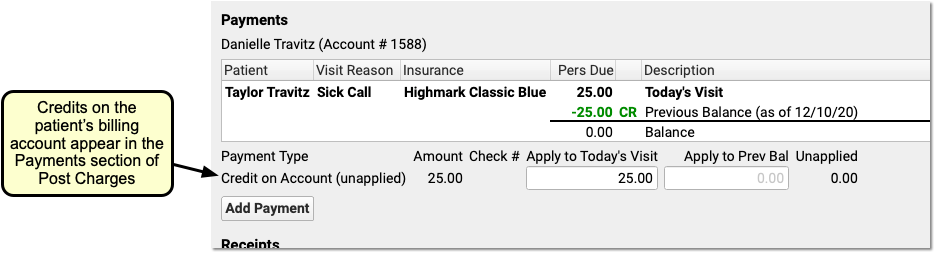
By default, the full credit will be applied towards any personal (non-insurance) charges for today. Optionally, you can adjust the amount you wish to link to today’s charges.
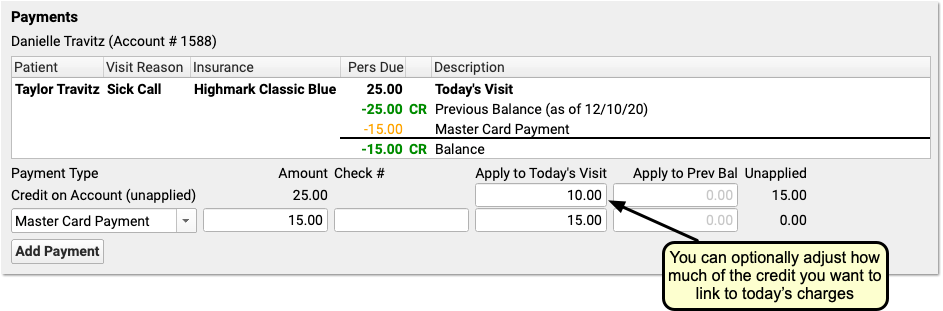
You might do this in order to apply only the amount of a copay, for example, or if only part of the credit should be applied.
When you are finished reviewing charges and payments, click Save and Post. PCC EHR will link the payment from the past directly to the charges that have a personal amount due.
Review and Fix Invalid ICD-10 Codes When You Post Charges
When you post charges, and an ICD-10 code is expired (or not yet in effect), PCC EHR will warn you and prevent posting. The diagnosis will appear in red text and include an explanation in parentheses. For example, this screenshot was taken in December of 2020:
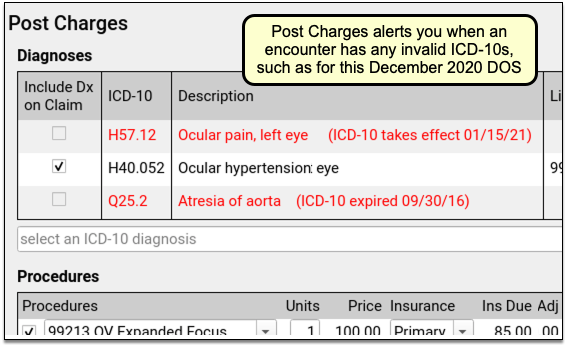
PCC EHR will not allow you to post charges with diagnoses that are invalid for the date of service. You can immediately add the correct code into the Diagnoses component, link and post the charges, and queue up a claim.
Fix Your Diagnosis Configuration: If an invalid ICD-10 appears on the Post Charges screen, you can fix the problem so it doesn’t appear again. For example, you might have an order that is configured to trigger the old diagnosis, or an expired ICD-10 might be manually mapped to a SNOMED description. You can fix these issues in the Billing Configuration tool. In Billing Configuration, you can only map ICD-10 diagnoses that are valid or will be valid in the future; expired ICD-10s are not available for mapping.
Help Families Resubscribe to Broadcast Emails and Opt In to Your Practice’s Text Messages
When a patient or their caregiver indicates that they did not receive your latest text (SMS) message or broadcast email, you can easily determine if it is because they have opted out of communication from your practice.
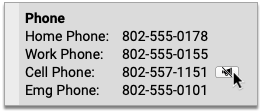
Look up the person’s phone number or email address in PCC EHR and see if an icon appears beside it.
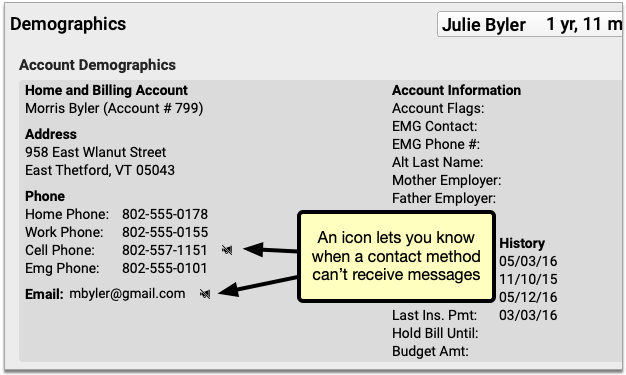
If you see an icon, it indicates that the contact method has been opted out of communication from your practice.
Unsubscribed Email Addresses Still Receive Portal Notifications: Patients and families who unsubscribe from your practice’s broadcast emails are still able to receive email portal notifications.
Opted-Out Phone Numbers Cannot Receive Any Text Messages from Your PCC System: Patients and families who opt their phone numbers out of text messages from your practice cannot receive any kind of text message sent from your PCC system, including broadcast messages, single text messages, and patient portal notifications.
Click the icon to learn how you can help the person opt back in to communication from your practice.
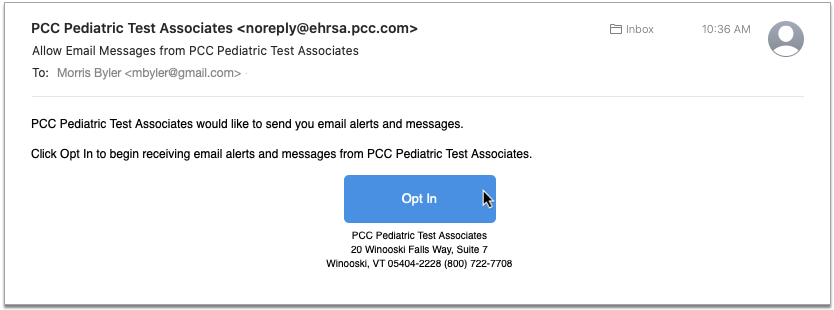
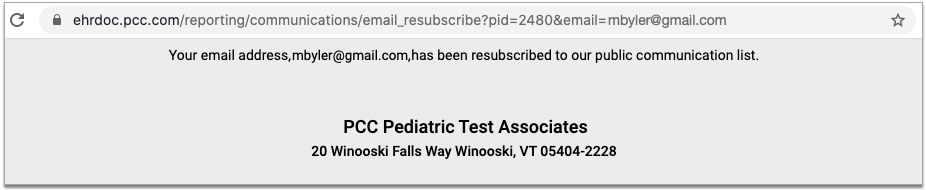
If the contact method is an email address, you can send a resubscribe email.
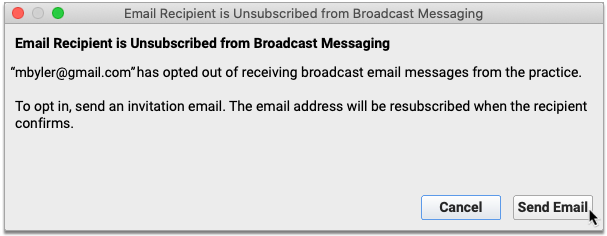
The recipient must open the email and click the “Opt-In” button in order to complete the process.
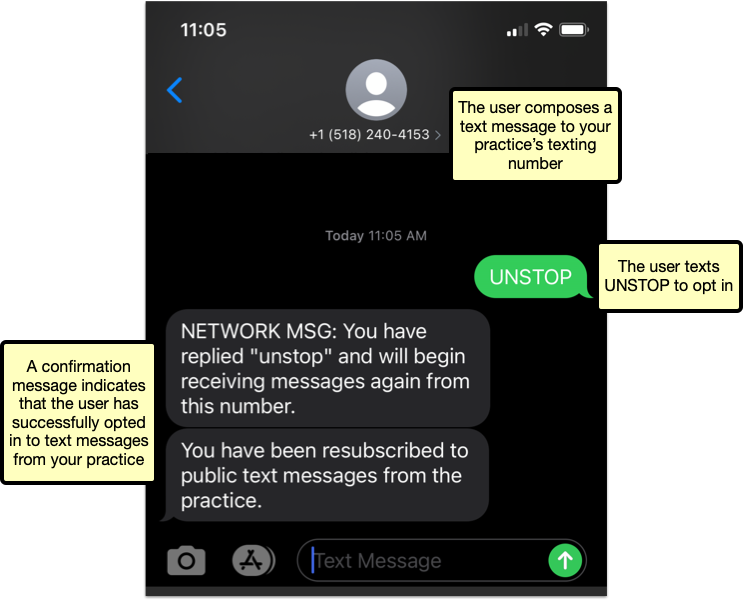
If the contact method is a mobile phone number, the person whose number it is must text “UNSTOP” to your practice’s texting number. You can find your practice’s texting number in the instructions that pop up when you click the icon beside the opted-out number.
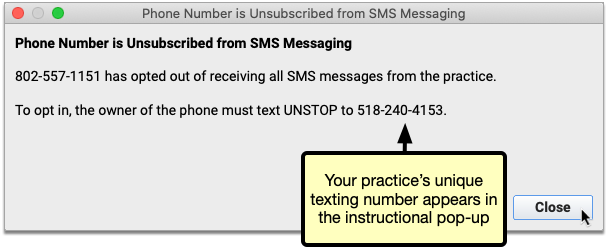
As soon as the person texts the word “UNSTOP” to your practice’s texting number, they receive confirmation that they have opted back in.
The icon in PCC EHR disappears once a contact method can receive messages again.
Where Does My Practice’s Texting Number Come From?: A text messaging number is automatically assigned to your practice by the telecommunications vendor PCC works with to provide broadcast messaging services. It is not possible to alter or customize this number.
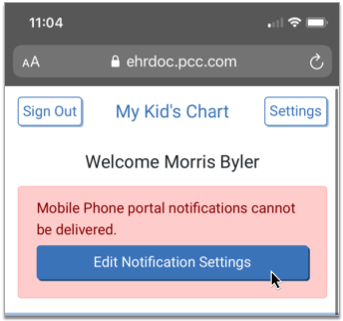
Portal Users Can Opt In Mobile Phone Numbers from the Patient Portal
Portal users see a message in the patient portal if their phone number cannot receive portal notifications. They can click “Edit Notification Settings” to correct the issue.
The button brings the user to the Edit Account page.
A message at the top of the page explains why the opted-out phone number cannot receive notifications and how to fix it. The opted-out phone number is highlighted in red at the bottom of the page.
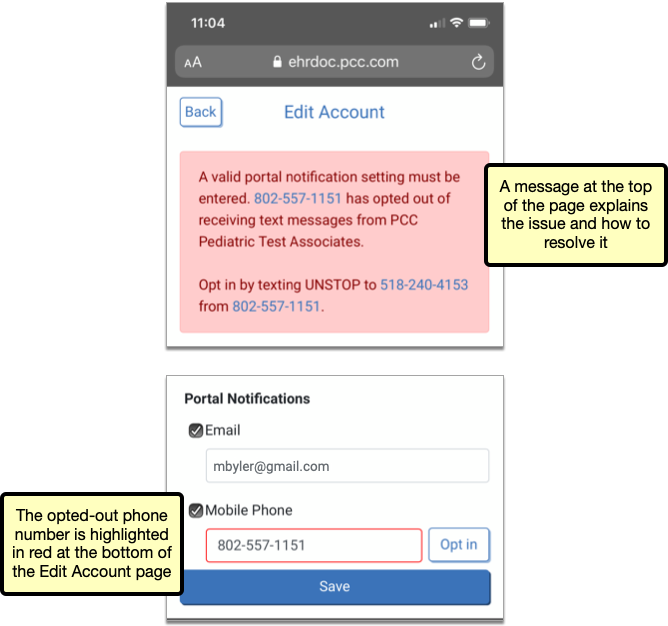
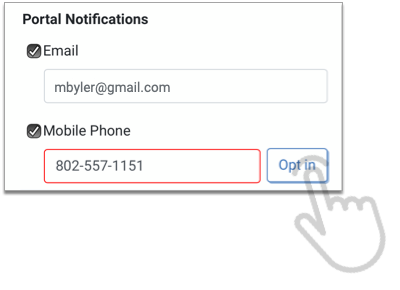
If the user is signed into the portal on their phone, an “Opt in” button appears beside the opted-out number. When tapped, the “Opt in” button automatically composes a text message to your practice with the word “UNSTOP” in the body.
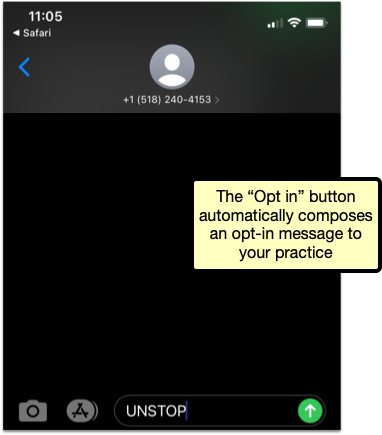
Once the person opts the phone number in, they can once again receive text messages from your practice, including portal notifications.
Portal users can find opt-in instructions in the My Kid’s Chart User’s Guide.
Opt In the Right Device: Users should only resubscribe via the “Opt in” button if they are signed in to the portal on the mobile device associated with the unsubscribed phone number.
Some Contacts Intentionally Opt Out of Text Messages: Contacts who intentionally opt out of text message communication from your practice should remove opted-out numbers from their portal notification settings.
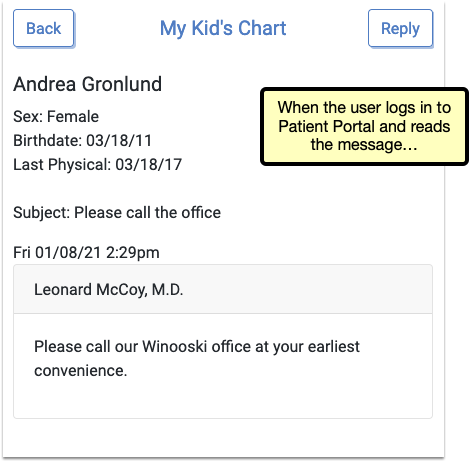
See if a Patient or Family Member Read Your Patient Portal Message
Learn exactly when your patients and families read your portal messages, so you can be sure you’re reaching them.
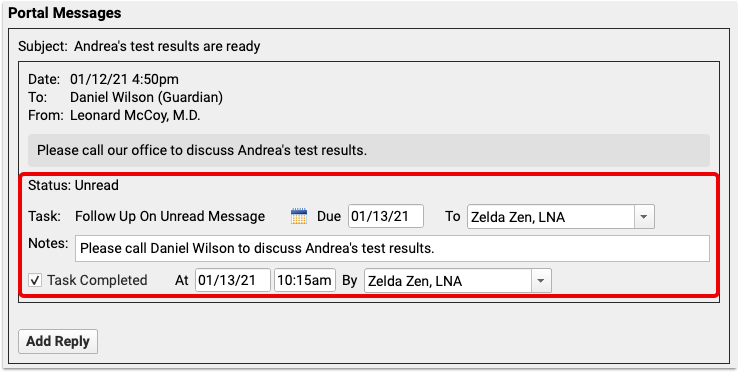
When you review a patient’s Portal Messages in PCC EHR, check the “status” line for each portal message. When the recipient opens a Patient Portal message, the status updates from “Unread” to “Read” with a timestamp of exactly when the message was opened, and which user opened it.
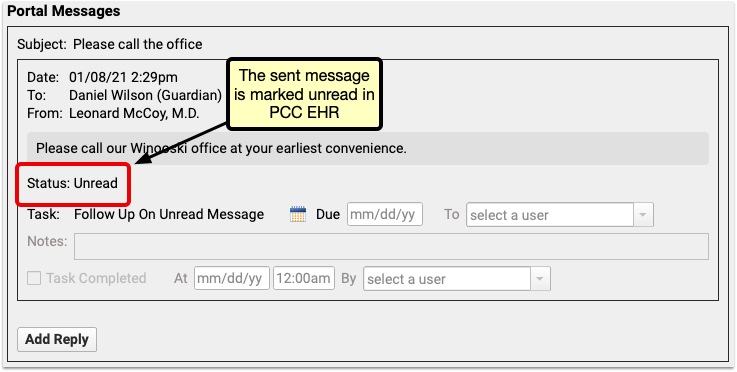
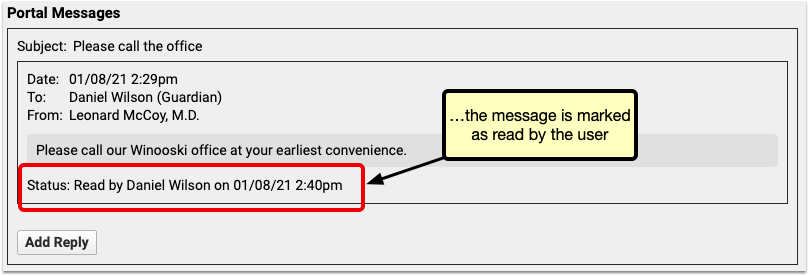
Make sure your message is received by assigning a follow-up task. Unread messages include the option to create a new “Follow Up On Unread Message” task. This new task type can be assigned to a user, but will also automatically be marked as completed if the message recipient reads the message before the assigned user marks it as completed.
More Easily View Portal Message Attachments in pocketPCC
Use pocketPCC to review attachments sent to your office via the Patient Portal to stay in complete contact with your patients from anywhere.
When you view a portal message in pocketPCC, any attachments appear below the message text. Click the arrow to the right of the file name to hide or show the attachment.
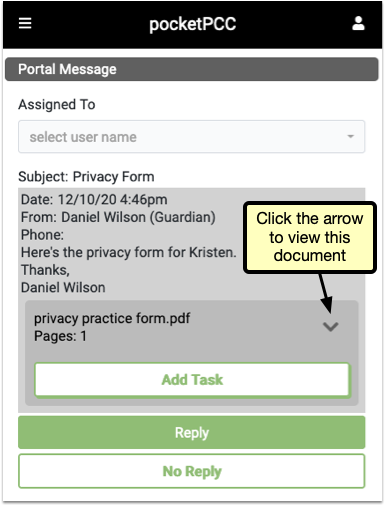
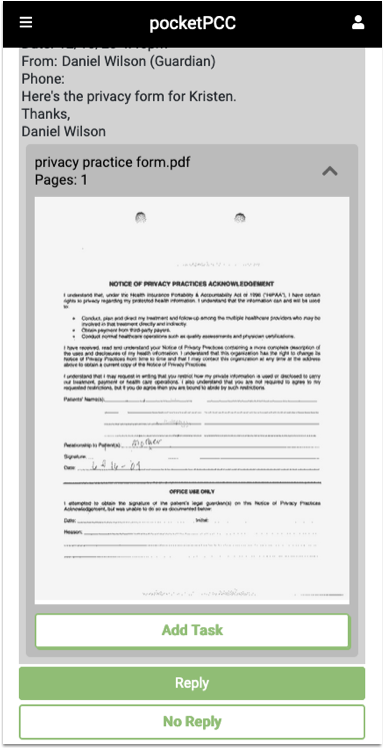
Click the arrow again to hide the image.
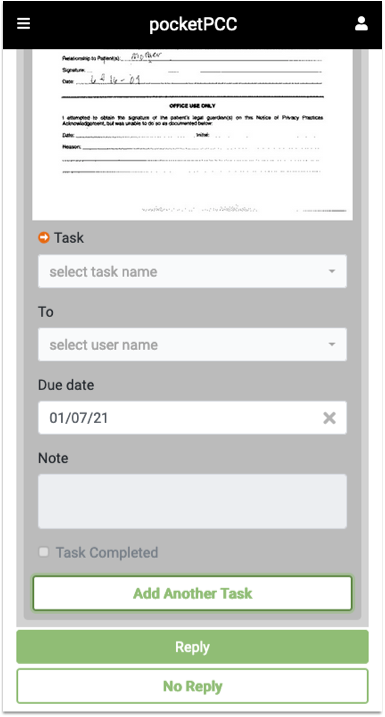
Click “Add Task” to create a new task associated with this document.
Quickly Find Recently Added Documents in pocketPCC
PCC 8.15 changes how documents are sorted and managed within pocketPCC, bringing it in line with PCC EHR, so you can quickly find a patient’s most recent documents.
The Recent Documents category appears at the top of each patient’s Documents and includes the five documents most recently added for the selected patient. Each document can also be found under its own category.
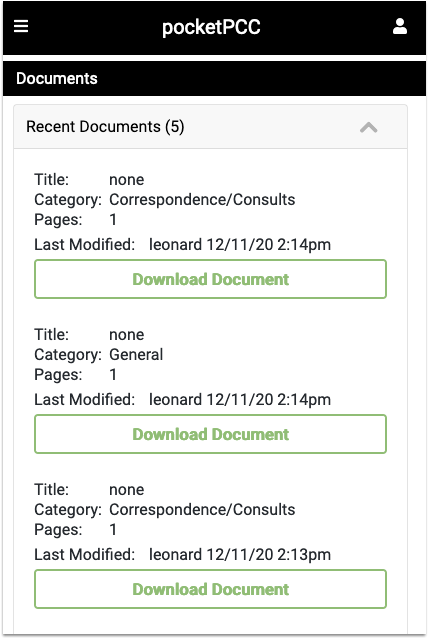
Likewise, within each document category, documents are sorted by date, with the most recent documents at the top of the list, so you can find the documents you’re looking for quickly.
Pick From Your Last 10 Patients When You Import Documents
When you need to import documents to a recent patient’s chart, you can now select from the last 10 patients in the Import Documents window.
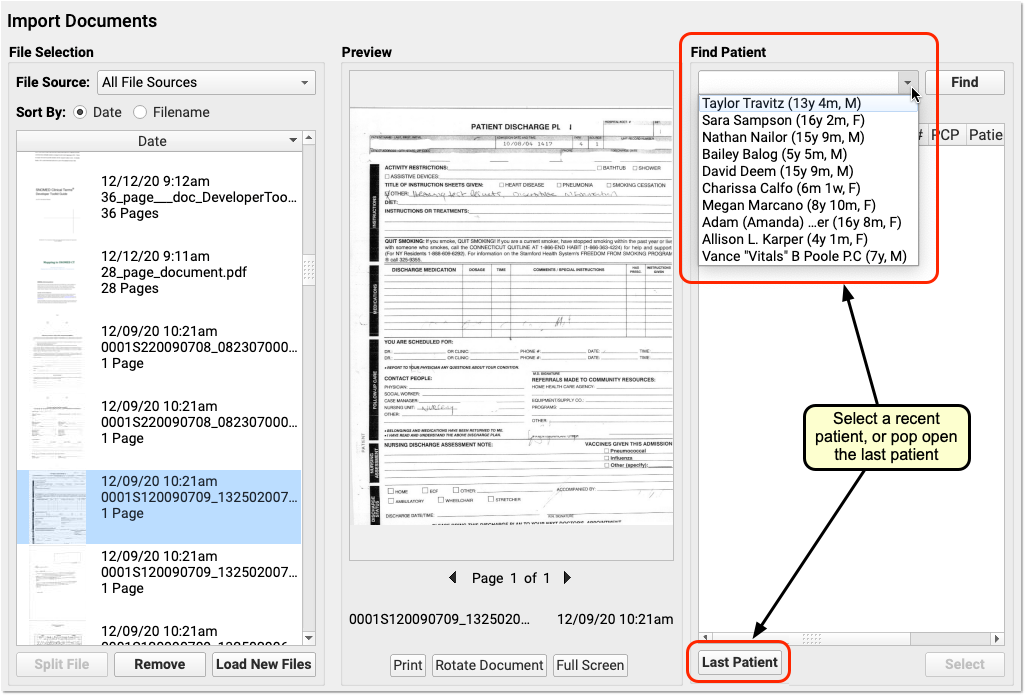
In addition to the quick “Last Patient” button, you can now easily pick from any patient you worked with recently.
The last 10 patients menu now appears wherever you search for patients—in Import Documents, but also in the PCC EHR Audit Log, the Delete Charted Visit window, the Immunization Registry Message Viewer, and more.
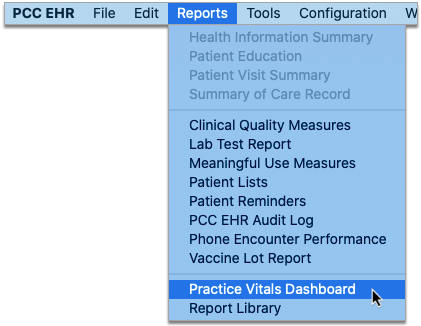
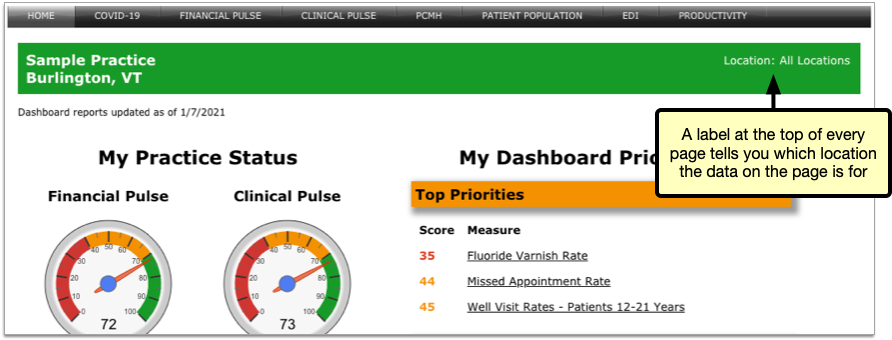
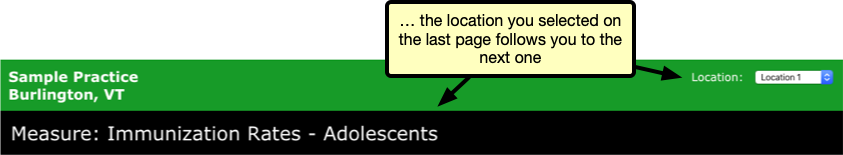
See Clinical Measures for Each of Your Office Locations in the Dashboard
The Practice Vitals Dashboard helps you monitor the health of your entire pediatric practice at a glance.
In PCC 8.15, multi-location practices can drill down even further to measure how well each specific location delivers patient care.
Launch the Practice Vitals Dashboard from the Reports menu in PCC EHR.
A new label in the top-right corner of each page tells you which location the data on the page is for.
On pages that have location-specific data, the location label turns into a drop-down list and you can select the location you want to view.
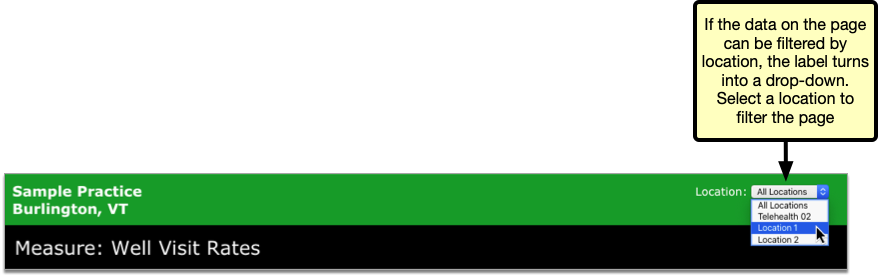
When you change the location filter, the page automatically refreshes and updates the measures and benchmark calculations with data specific to your selection.
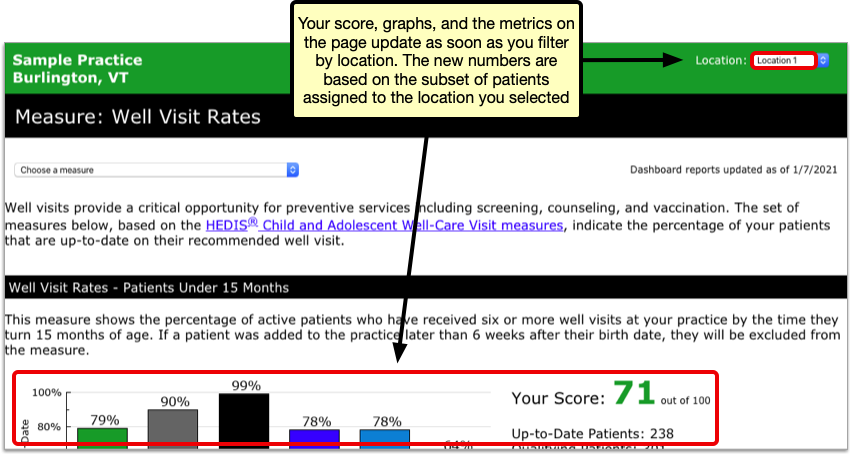
Location-specific calculations are based on the patients who are assigned to the location that is selected. At most, each patient at your practice is represented only once in location-specific data sets for each measure.
How Are Patients Assigned to Office Locations for Dashboard Measure Calculations?: Patients who have had a well visit are assigned to the location of their last well visit. Patients who have never had a well visit are assigned to the location of their most recent office visit. Patients who have had neither a well visit nor an office visit are excluded from location-specific data sets.
You can filter all Clinical Pulse and PCMH measures by location, except for weight assessment and counseling measures and the measures for influenza immunization rates.
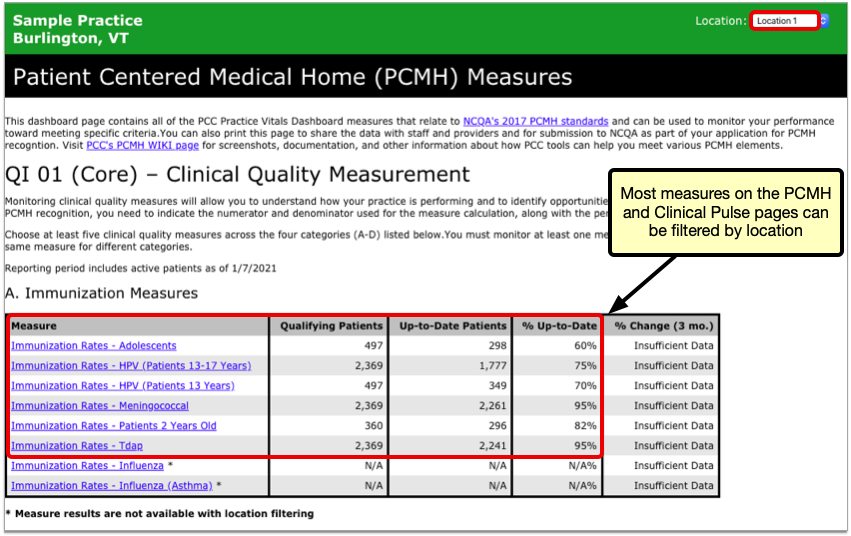
When navigating between pages that have location-specific datasets, the Dashboard remembers the last location you selected.
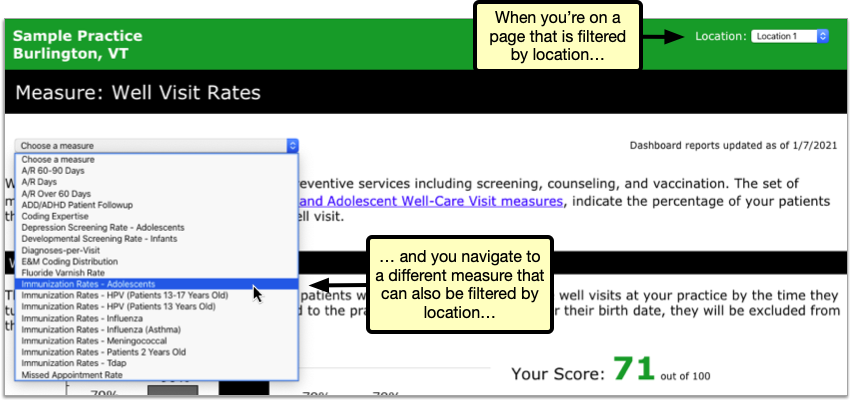
Location-specific Dashboard measures can help you understand if a location needs extra help in the clinic or is providing particularly good care to patients.
Practices working toward Patient-Centered Medical Home (PCMH) recognition can also use location-specific datasets in the Dashboard to attest to the fact that they are meeting program benchmarks.
Contact your PCC Client Advocate for help interpreting information in the Practice Vitals Dashboard, including data about specific practice locations.
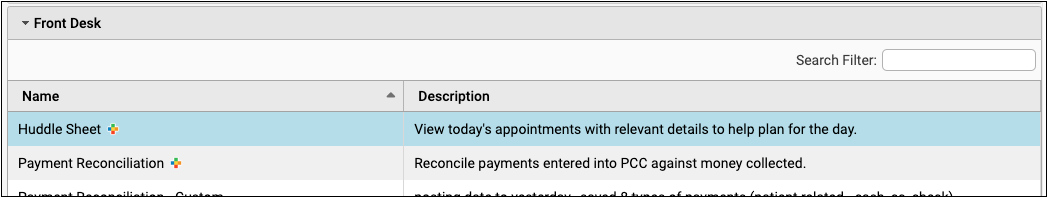
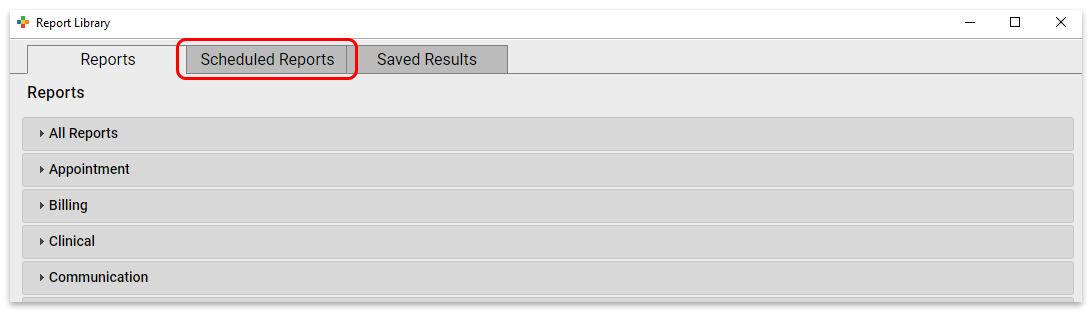
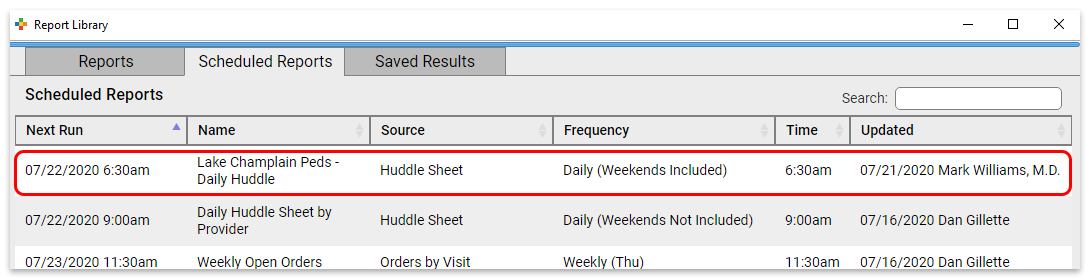
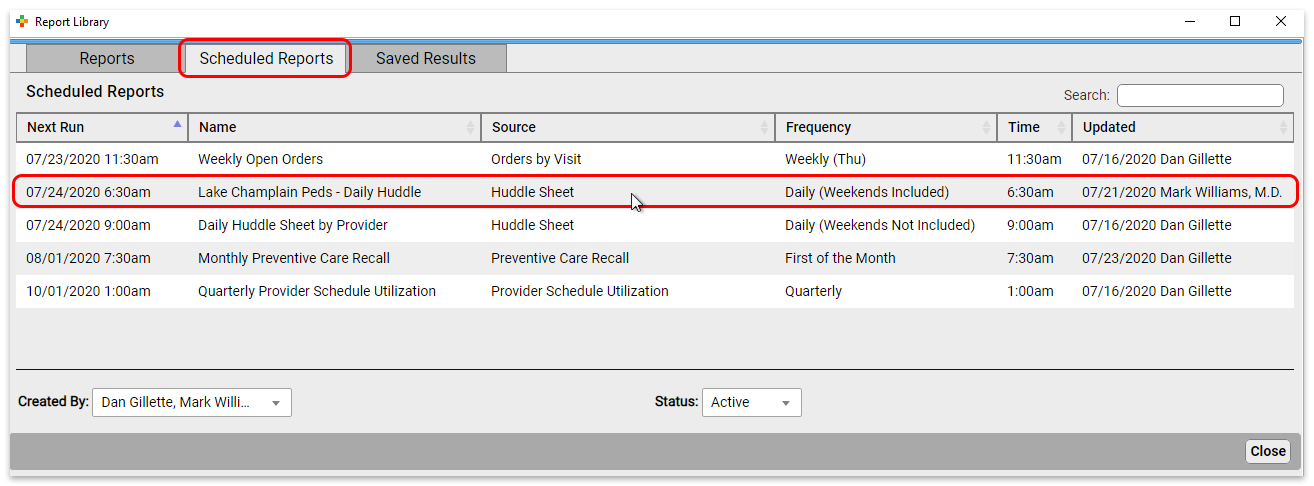
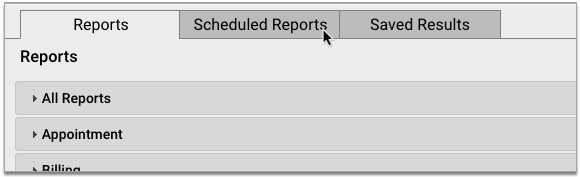
Delete Scheduled Reports
Clean up your list of scheduled reports in PCC EHR by deleting those you no longer need.
Open the Report Library from the Reports menu, then click the Scheduled Reports tab.
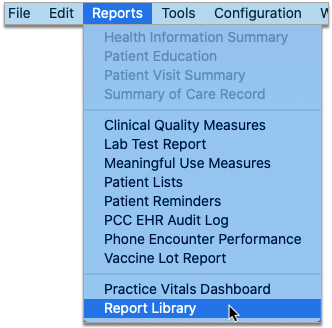
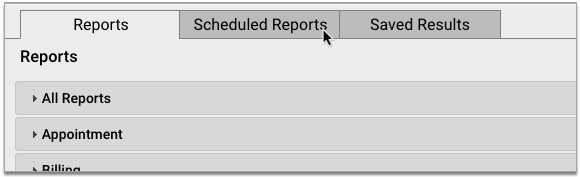
Select a schedule you never plan to use again, then click the Delete button.
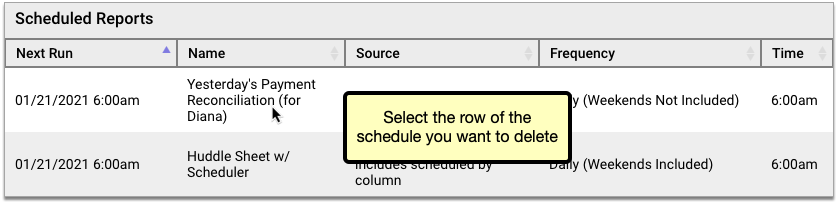
Deleted scheduled reports are permanently removed from the Report Library and cannot be re-enabled. If you want to temporarily disable a scheduled report, try stopping it instead.
You can continue to view past saved results of deleted scheduled reports in the Report Library in the Saved Results tab.
Only Users With Permission Can Delete: The ability to delete scheduled reports is restricted to users who have permission to do so. You can set this permission in User Administration.
Report More Easily on Hospital and Billing-Only Encounters
Improvements in the PCC EHR Report Library make it easier to report on hospital and billing encounters.
Find Hospital Visits and Billing-Only Encounters by Billing Status
The Encounters by Billing Status report can now include hospital and billing encounters.
When building your report, you can use the Encounter Type filter to include or exclude hospital and billing encounters from the results.
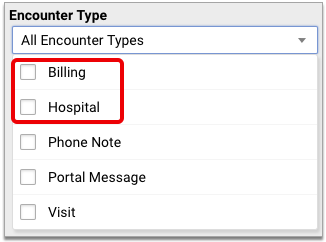
You can also use the Location filter to include or exclude encounters that occurred at hospital locations.
Report on Diagnoses Billed for Hospital Visits
The Billed Diagnoses by Date report can now include hospital encounters.
You can include or exclude hospital encounters from the report using the Location filter on the report criteria screen.
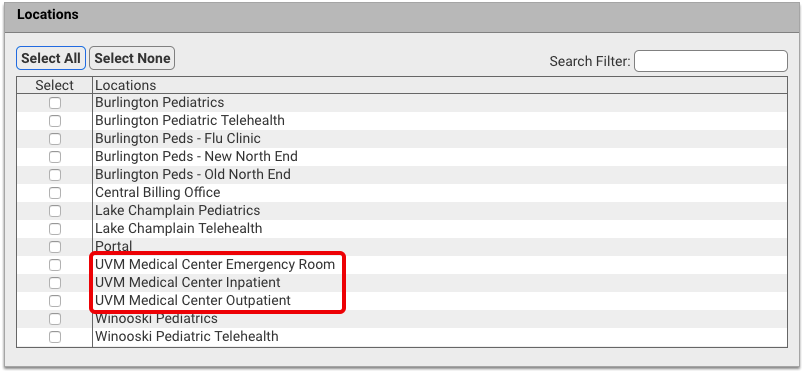
When you run the report for all locations, the results include hospital encounters.
Other Report Library Improvements
PCC 8.15 tweaks and tunes the Report Library to make it an even more powerful tool for your practice.
-
See When You Last Reviewed Care Plans: The date of last review for care plans has been added to the Care Plans by Date report. This change helps all practices track the progress of care plans more closely, and especially helps offices working toward PCMH recognition.
-
Filter and Sort Care Plan Reports by Patient Flag: You can now filter and sort by patient flag in the Care Plans by Date report. This change is most useful if you want to exclude inactive patients from the report so that you can focus on active patients with care plans.
-
When You Delete a Custom Report, See If It Is Scheduled: When you delete a custom report that was used as the basis for scheduled reports, the Report Library notifies you of the schedules before deleting the report. You can use this information to decide if you want to keep the report in place or delete it anyway. If you choose to delete it, the associated schedules will also be deleted.
-
No More Canceled and Missed Appointments When Reporting by Billing Status: The Encounters by Billing Status report now excludes canceled and missed appointments, allowing you to focus on the visits which did occur and might need some biller or clinician follow-up.
-
More Locations When Reporting By Billing Status: As of PCC 8.15, the Location filter for the Encounters by Billing Status Report allows you to select both scheduling and non-scheduling locations.
-
Navigate the Report Library More Quickly: Performance improvements introduced in this release result in a Report Library that loads screens faster and smoother than before.
Coming Soon: Look Up and Import Immunization Records from Your State’s Registry
When a new patient joins your practice or an established patient comes in after a hiatus, you want to be sure you have the most complete and up-to-date version of their immunization history.
PCC 8.15 gives pilot practices the ability to look up and import vaccine records from their local immunization registry without ever leaving PCC EHR.
If you are interested in using this feature once a connection has been established with your registry, speak with PCC Support.
Open the Patient’s Immunization History in PCC EHR
Open a patient’s chart in PCC EHR and navigate to the Immunization History.
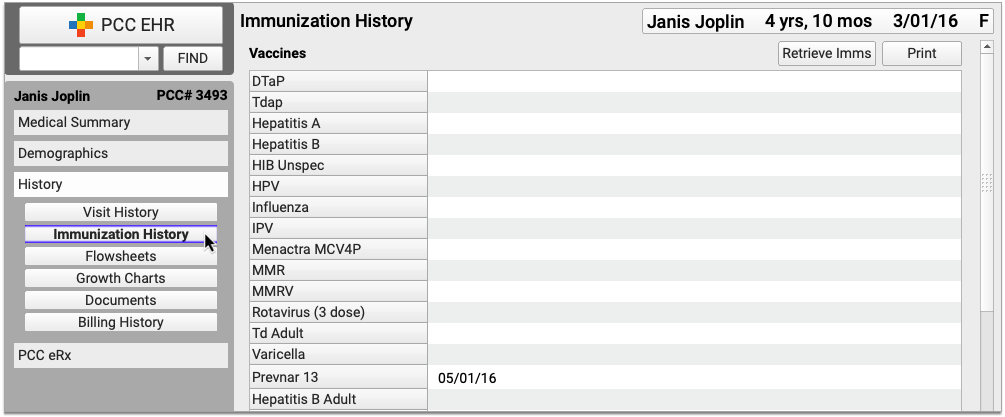
You can get to the Immunization History from the History section of the chart or within the Immunizations component if you’re in a visit protocol.
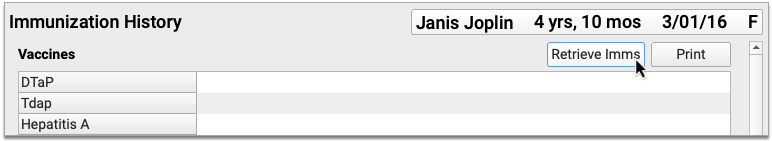
Click the “Retrieve Imms” Button
Click the “Retrieve Imms” button to request the patient’s immunization history from your state registry.
Confirm the Patient Match
The registry searches its records for your patient and PCC EHR asks you to confirm that it found the right person.
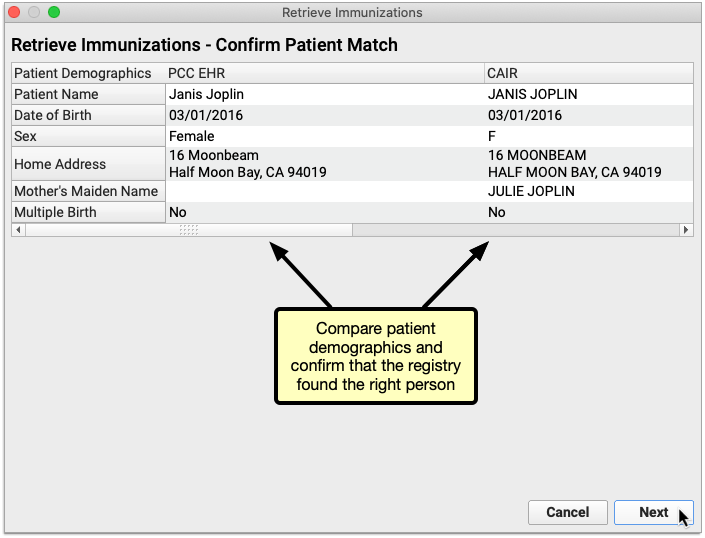
Once you confirm that the registry found the right patient, click “Next” to view the patient’s vaccine history.
You Can Only Proceed with a Unique Patient Match: If the registry finds several possible matches for your patient or finds no exact matches you will not be able to retrieve the patient’s vaccine history from the registry within PCC EHR. Close the Retrieve Immunizations window and try looking up the patient’s vaccine history directly on the registry website.
Review the Information Sent by the Registry
Review the vaccine history from the registry. Information that is already in the patient’s chart appears in a black font, while new information from the registry appears in an orange font. You can decide what to do with the new information on the next screen.
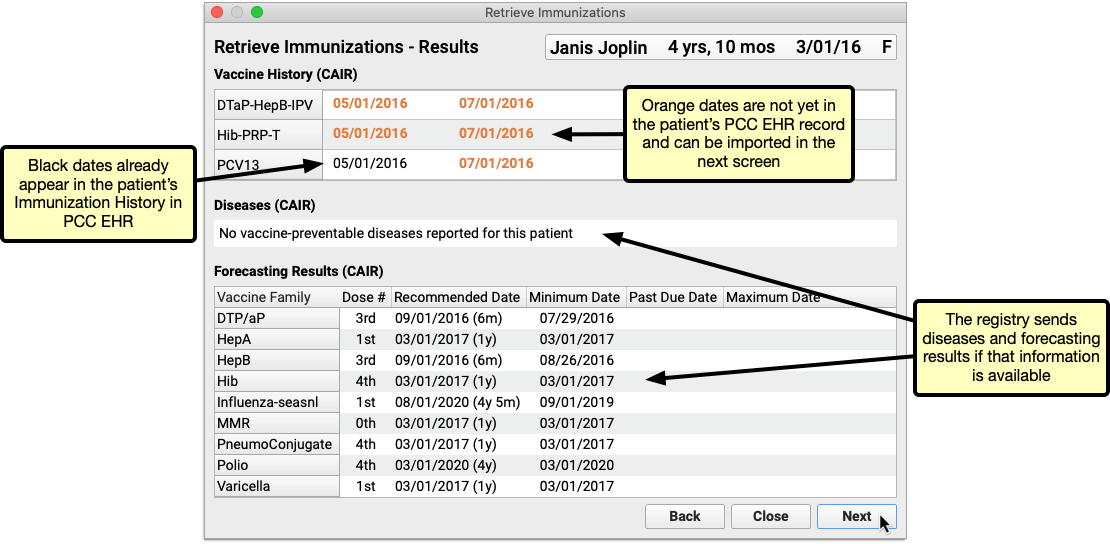
Click “Next” to begin importing new information from the registry into PCC EHR.
Immunization Registry Forecasting and Disease Data: Some registries send vaccine forecasting and/or vaccine-preventable disease data in addition to the patient’s vaccine history. You can view this information if the registry sends it, but you cannot import it into PCC EHR.
How Does PCC EHR Determine if a Vaccine is Already in the Patient's History?: For each immunization reported by the registry, PCC EHR checks to see if the associated CVX code and date already exist in the patient’s chart.
Import New Vaccine History Information from the Registry into PCC EHR
Select the immunizations and dates you wish to import from the registry into the patient’s PCC EHR record. You can only import new entries from the registry; entries that already exist in the EHR are excluded from the import window.
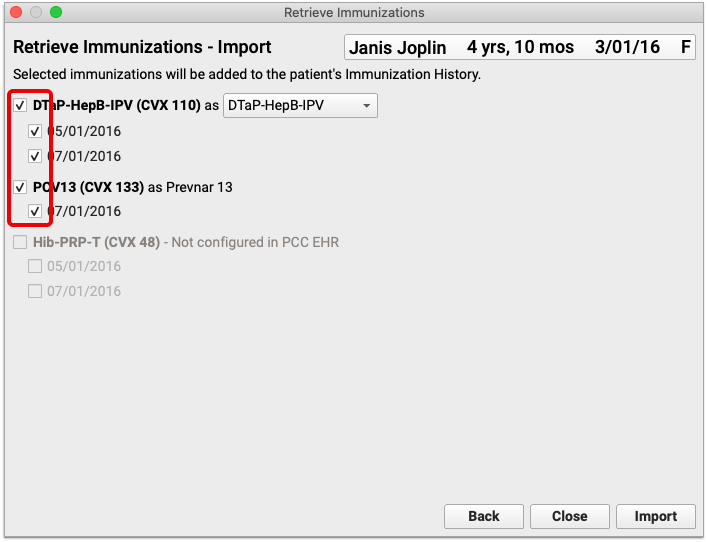
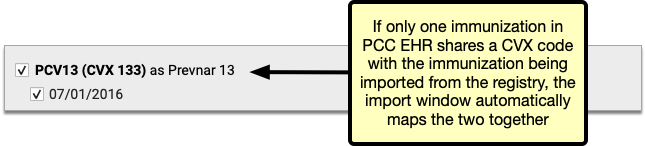
Once selected, immunizations from the registry are automatically mapped by CVX code to their equivalents in the EHR.
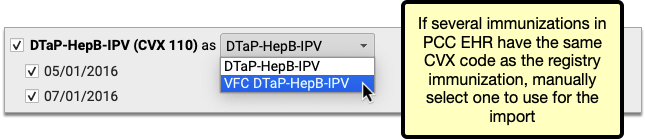
If a registry immunization has several equivalents in the EHR, all of the options are presented in a drop-down field in the import window. Review the options and manually select one to use for the import.
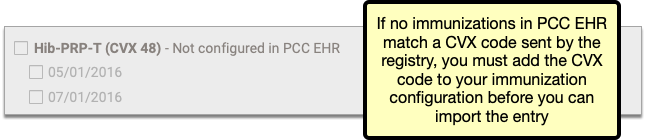
Sometimes new entries from the registry use CVX codes that are not configured in your PCC system. You must add the missing CVX codes to your immunization configuration in order to import these entries. Contact PCC Support if you need help adding CVX codes to your immunization configuration.
Once you have selected and mapped the immunizations you plan to import from the registry, click the “Import” button.
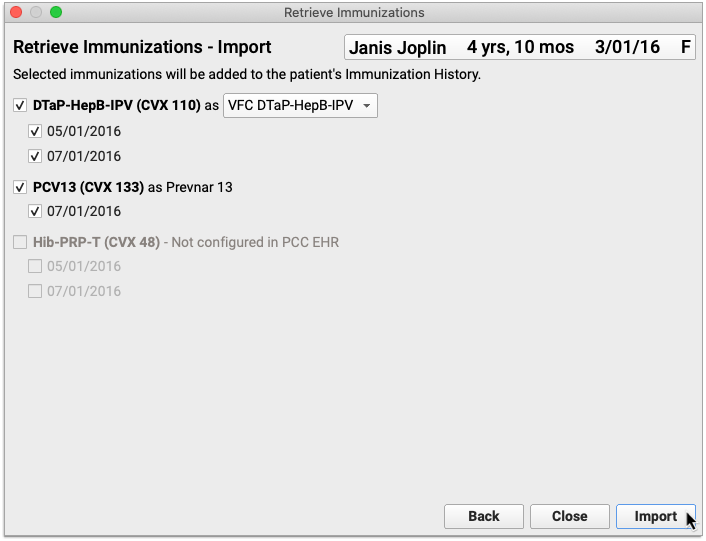
The information imports into PCC EHR and the Retrieve Immunization window closes on its own.
View and Edit Imported Entries in the Patient’s Immunization History
Information imported from the registry appears immediately in the patient’s Immunization History in PCC EHR.
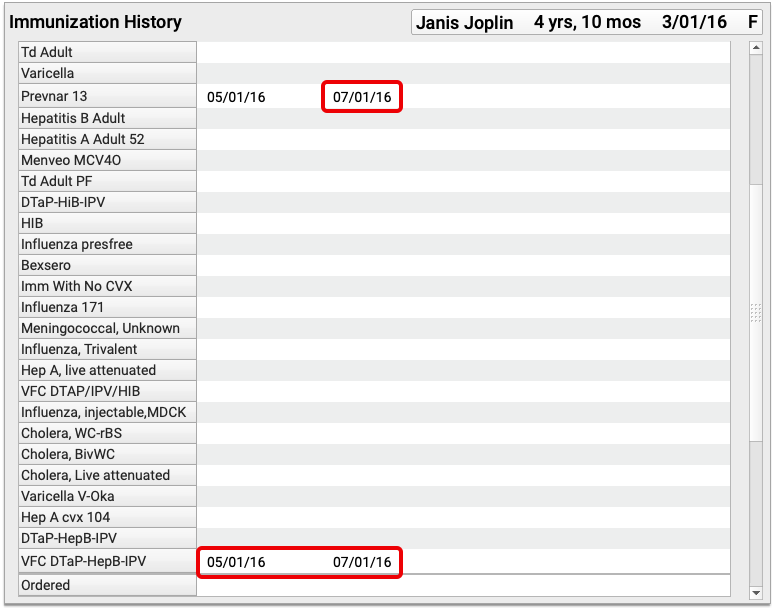
You can view details about the immunizations imported from the registry by editing the patient’s Immunization History.
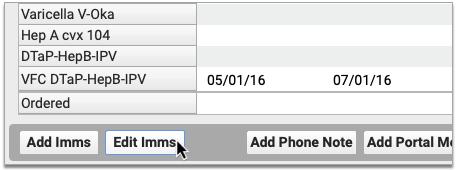
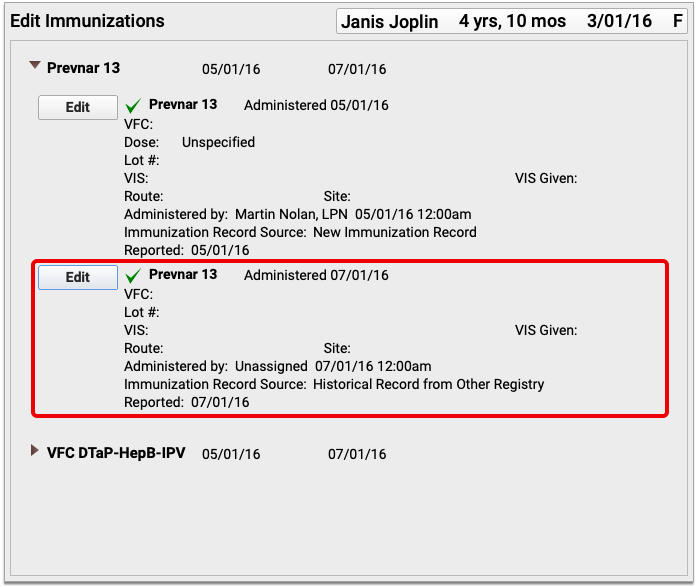
Historic immunizations imported from the registry are recorded in the patient’s chart with the source “Historical Record from Other Registry”. The imported entries can also include information about the vaccine dose, lot number, site, route, and funding source.
You can edit or delete an imported immunization just like any other item in the patient’s Immunization History.
Continued Pilot Test: Send CHADIS Questionnaires to Families in the Patient Portal
PCC continues piloting the integration of CHADIS questionnaires into PCC EHR and PCC’s Patient Portal. If your practice is part of our pilot testing, your Patient Portal now links directly to CHADIS, so your portal users can get started on their patient’s CHADIS questionnaires as soon as their appointment is booked.
Coming Soon: CHADIS integration into PCC is currently in pilot testing and not yet available to all PCC clients. Stay tuned for additional functionality and the wide release. CHADIS integration into PCC EHR requires that your practice has a CHADIS subscription.
Continued Pilot Test: Securely Retrieve Patient Information from Hospitals and Other Practices
Do your patients see other doctors? Do you wish you could retrieve records from those providers on demand?
Pilot testers can request and securely retrieve their patients’ records from other healthcare organizations right within PCC EHR. This is the latest addition to PCC’s Clinical Document Exchange functionality.
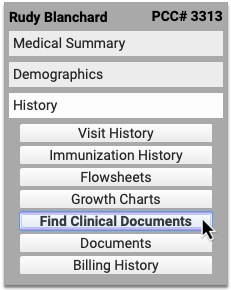
To retrieve a document, click “Find Clinical Documents” within the History section of the patient’s chart.
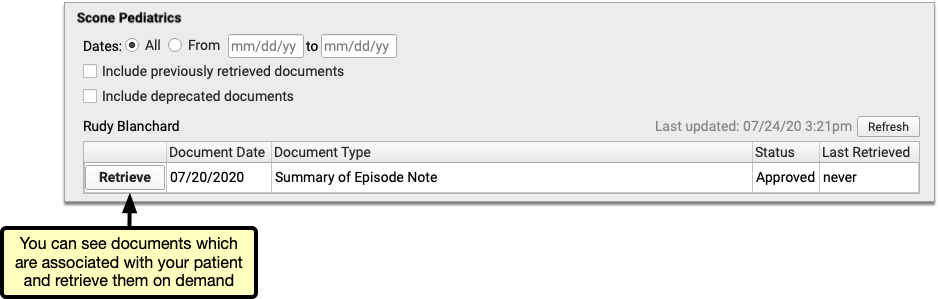
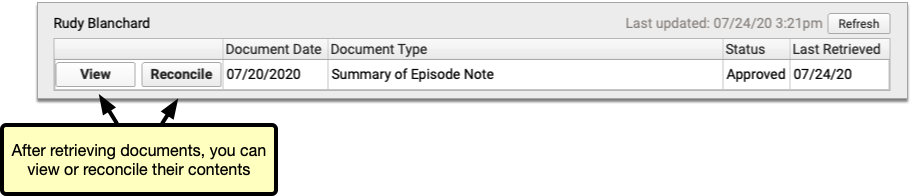
Select one or several healthcare organizations to query, then search for your patient within their records. If you find matches for your patient, you can then see if the organizations have clinical documents to share, and retrieve any you wish to view and save to PCC EHR.
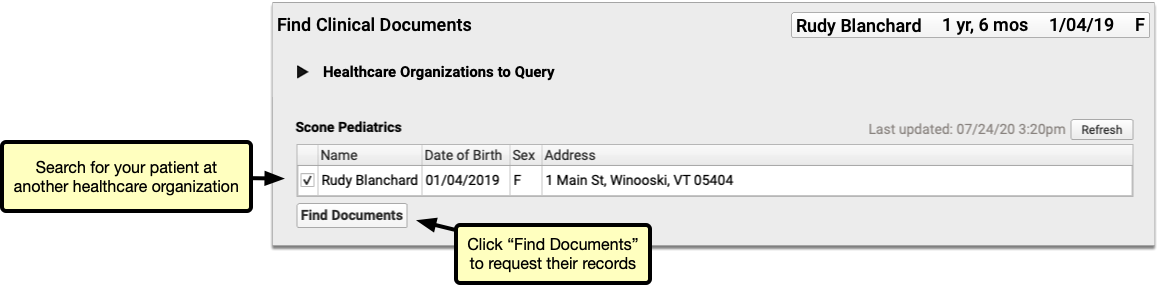
You can set up default healthcare organizations to query for each of your patients, and also decide if certain organizations (such as local hospitals or urgent care clinics) should be queried for all patients.
Users need special permissions in PCC EHR in order to request patient records from other organizations. All PCC EHR users can view retrieved documents after they have been saved in patients’ charts.
How do I Participate?
Although it is not yet possible to sign up to securely retrieve your patients’ records from other healthcare providers, you can prepare for the feature by becoming a Clinical Document Exchange Responder.
Clinical Document Exchange Responders allow other healthcare organizations who participate in the Carequality interoperability framework to retrieve their patients’ records for treatment purposes. In order to eventually be able to initiate records requests, you must first enroll to respond to requests from others.
To become a Clinical Document Exchange Responder, contact PCC Support.
Learn About Clinical Document Exchange
Is Clinical Document Exchange secure? How does it work? Which organizations can I query for my patients’ records? Find answers to all of these questions and more in the PCC Learn article about Clinical Document Exchange.
Other Feature Improvements and Bug Fixes in PCC 8.15
In addition to the features described above, PCC 8.15 includes these smaller improvements and squashed bugs.
-
Delete Hospital and Administrative Fee Billing Encounters: When you use Correct Mistakes (
oops) to delete all diagnoses, procedures, payments and adjustments for a hospital encounter or other charge that does not have an appointment, PCC EHR will automatically remove that encounter from the Billing History and the Visit History sections of the patient’s chart. -
Diagnoses and Procedures Remain Available in Post Charges: When you need to delete and repost charges, or return and finish posting additional items for an encounter, the Post Charges workflow will continue to display all of the diagnoses and procedures originally added to the encounter.
-
2021 RVU Values for Reporting: During the PCC 8.15 release cycle, PCC updated all practices with RVU values for 2021. This updates many reports, such as the RVU-Per-Visit measure in the Practice Vitals Dashboard.
-
0.3ml Dose Amounts: PCC EHR now supports the recording and tracking of immunizations that require a 0.3ml dose.
-
Additional COVID-19 Terms Available as Diagnoses: Among other updates in support of charting COVID-19 related encounters, the PCC 8.15 update adds three SNOMED situations to the standard Diagnosis favorites list so they can be used as diagnoses: Suspected disease caused by severe acute respiratory coronavirus (mapped to B97.21), History of disease caused by Severe acute respiratory syndrome coronavirus (mapped to Z86.19), and Disease caused by Severe acute respiratory syndrome coronavirus 2 absent (mapped to Z03.89).
-
See If PocketPCC or the Patient Portal is Being Updated When You Sign In:
Users who try to sign in to PocketPCC or the patient portal while PCC is updating your software to a new release will be notified that an update is in progress and that they should try again later.
Users who are signed in to PocketPCC or the patient portal when an update begins will be logged out the next time they take an action. They will be redirected to a page explaining that an update is underway. Any unsaved work will be lost.
PCC 8.15 Migration Considerations
The PCC 8.15 release includes new features that may need configuration and for which you may want to do extra planning or training. Read below to learn more, and share relevant details with your physicians and staff.
Read the PCC 8.15 Release article for complete details on these features.
Contact PCC Support for information about these or any features in PCC 8.15.
Update Your Workstations, Expect Some Slowness On Day 1
After a PCC update, your practice will need to update workstations around your office. Users will see an update reminder on their login screen.
Update Slowness: After you install a PCC EHR update on a workstation, the software needs to cache the code it uses to display information. You will experience slowness until this finishes.
Add COVID-19 Vaccines to Your PCC System
For a complete guide to adding COVID-19 vaccines to your PCC system, read Configure, Track, and Administer COVID-19 Vaccines in PCC EHR (COMING SOON).
In addition to other COVD-19 vaccine updates, PCC 8.15 adds the 0.3ml as an option for dosage. If your practice added the Pfizer COVID-19 vaccine to your system prior to PCC 8.15, you should update the dosage from “Unspecified” to “0.3ml”.
Configure Which PCC EHR Queues Appear for Each User
To adjust which queues are visible for each user at your practice, first open the User Administration tool and edit a user role.
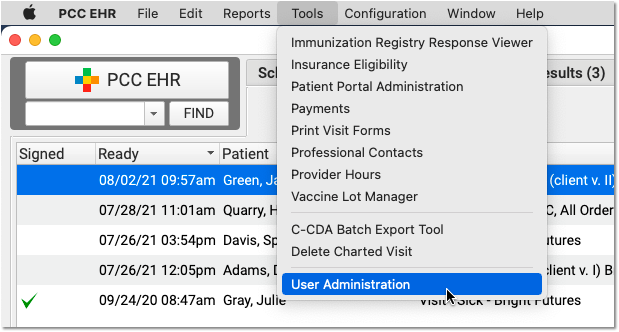
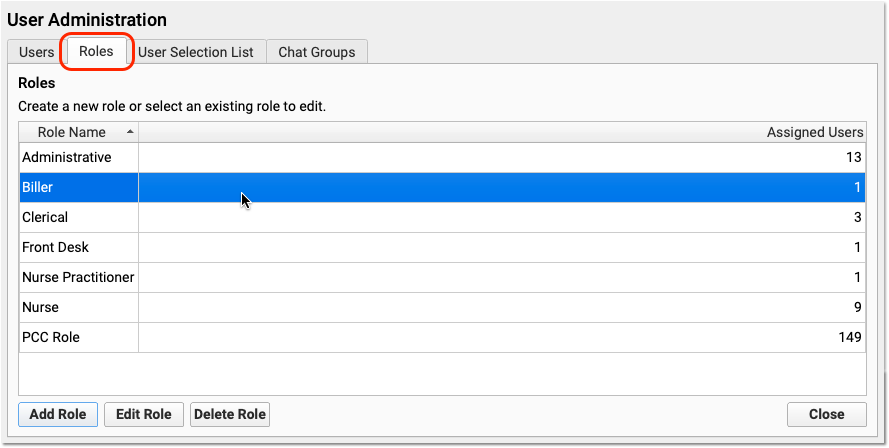
Use one of your existing roles or create a new one. Double-click on the role to adjust permission settings.
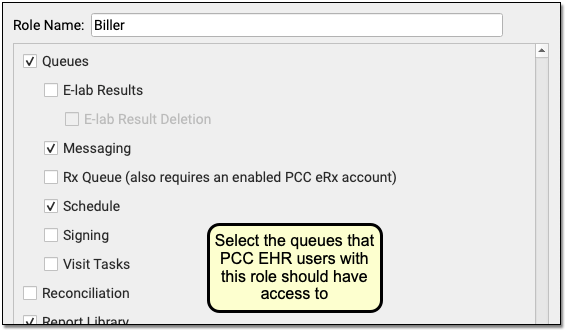
Select each queue that users with this role should have access to. Repeat this process for each role at your practice.
As you design roles, remember that users can be assigned more than one. Each user will see all the queues available for any of their assigned roles. Also, note that the eRx Tasks queue only appears for users who have both a role with the queue permission and an enabled PCC eRx account.
Next, edit each user’s account and adjust their assigned roles.
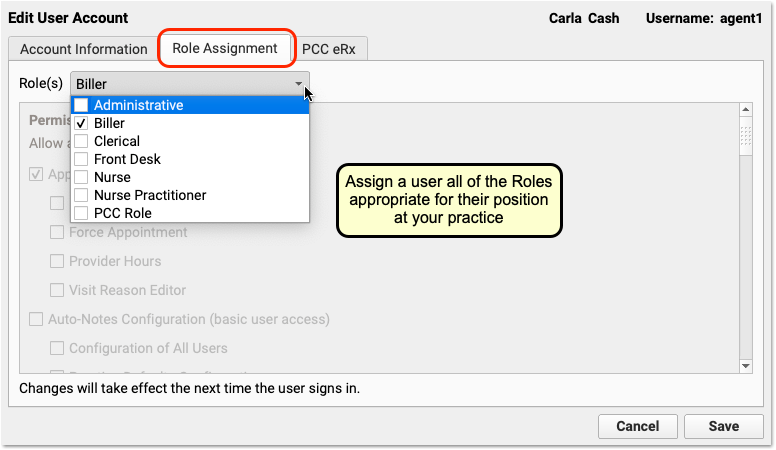
By fine-tuning which queues appear for each user role in your practice, you can make PCC EHR easier to use and you can control who has access to different functions in PCC EHR.
All Users Will Still Have Access After the PCC 8.15 Update: Configurable queues are brand new! The PCC 8.15 update won’t hide any queues. When users log in after the update, they will see the same queues they have always seen. After the update, your practice’s office manager or system administrator can configure roles for your users, and also set expectations about the change. If you need help, contact PCC Support.
Adjust Order Configuration to Make Billing Easier
PCC 8.15 improves how orders (including labs, immunizations, and others) show up when the clinician prepares the encounter for billing. Orders can now automatically add linked diagnoses and procedures to the Bill window, and duplicate diagnoses (such as for immunizations) will now consolidate into a single entry.
After your PCC 8.15 update, your practice may wish to adjust what codes are triggered by common orders at your practice.
If your practice uses PCC EHR to post charges, for example, you can add the Z23 diagnosis to every immunization order without worrying about a long list of Z23s for busy well visits. Use the Billing Configuration tool to adjust the diagnoses and procedure codes for each order at your practice. Use the Protocol Configuration tool to adjust which orders appear for each visit reason.
If your practice still uses the Practice Management tools (chuck, checkout) to post charges, you may decide not to do this, as the previous system does not deduplicate diagnoses.
Prepare for Username and Password Updates Across PCC Products and Services
PCC 8.15 automatically syncs authentication between PCC EHR, the Practice Management window, and other PCC products and services. Your practice can use PCC EHR’s User Administration tool to manage user accounts for all PCC products. This includes password, username, and each user’s “Full Name” which appears in various programs. This syncing will occur the first time a user logs into PCC EHR.
After the update, your practice should be on the lookout for the following:
-
What If My Passwords Were Different Before PCC 8.15?: If you previously used synced accounts on PCC EHR and Practice Management, but those accounts had different passwords, PCC 8.15 will update your Practice Management password to match your PCC EHR password when you next log in to PCC EHR. Your practice should share this information with some users, particularly if they access the Practice Management tools directly using terminal emulation software, such as AniTa.
-
Use Your PCC EHR Password for All Logins: If a user connects to your PCC server using a Secure Connect connection or other remote connection technology, they will now use their PCC EHR password.
-
Web-Based Email Login: If your practice uses a web-based email program to access an email account run on your PCC server, such as Roundcube, that password will also be synced to the user’s PCC EHR password.
-
What If I Used Different PCC EHR and Practice Management User Account Names Before PCC 8.15?: If you had two different login usernames on your PCC system, one for PCC EHR and one for the Practice Management window, PCC 8.15 will not touch your accounts and you can continue to use them without interruption.
-
What If My Practice Shares User Accounts Among Multiple People?: If your practice shares either PCC EHR or Practice Management account logins among multiple employees, PCC strongly suggests you work with PCC Support to end this practice, as it represents a security risk and makes it impossible to audit account access. After your PCC 8.15 update, only one PCC EHR account can be linked to a Practice Management username and password. Prior to the PCC 8.15 update, PCC will proactively contact your practice if you have multiple PCC EHR users connected to a single Practice Management account.
-
Attribution in Some Programs May Look Different: If a user had a different Full Name in their PCC EHR account than they used in their Practice Management account, they may notice differences in how their name appears in some programs after the PCC 8.15 update. For example, if your practice uses initials to indicate who performed various advanced billing functions (like correcting and rebatching a claim), those initials will now match the full name from their PCC EHR account. Contact PCC Support for assistance.
Allow Users to Delete Scheduled Reports
A new permission in User Administration grants users the ability to delete scheduled reports in the Report Library.
You can add the permission to any role which requires it.
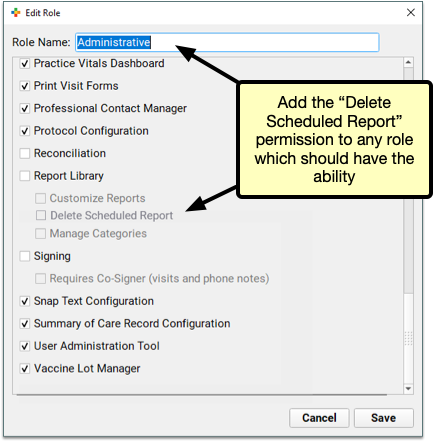
With the update to PCC 8.15, the permission will be granted by default to all users who already have both Report Library *and* User Administration access. If you need step-by-step instructions about how to assign permissions to users in PCC EHR, read Set User Roles for Permissions and Security.
Get Started with Bidirectional Immunization Functions in PCC EHR
The ability to look up and retrieve immunizations from your local registry within PCC EHR is currently in pilot testing with California Immunization Registry (CAIR).
If you are interested in using this feature once a connection has been established with your registry, contact PCC Support.
Continued Pilot Test: Securely Retrieve Patient Information from Hospitals and Other Practices
PCC continues to roll out the ability to securely retrieve patient documents from other healthcare providers in PCC EHR to practices who are already Clinical Document Exchange responders.
Clinical Document Exchange responders allow other providers to securely retrieve patient documents from their PCC system. You must become a responder before you can enable the ability to retrieve patient documents from other healthcare organizations.
Contact your PCC Client Advocate if you wish to become a Clinical Document Exchange responder in preparation for the ability to retrieve patient documents from other providers.
Or, learn more about Clinical Document Exchange.
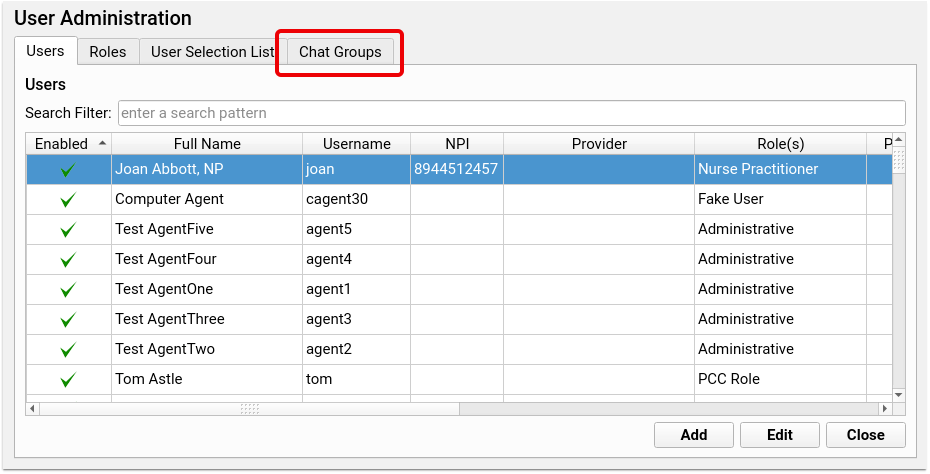
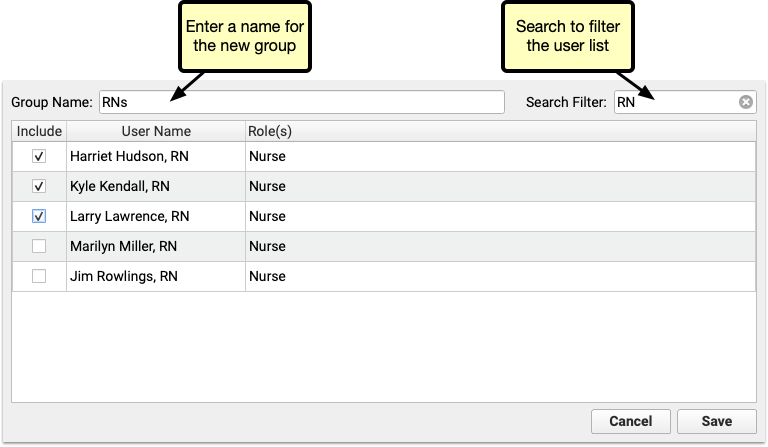
Create Chat Groups For Your Practice
Expand your communication reach using PCC EHR’s chat feature by creating groups of users. With a chat group, you can send a message to a list of users all at once.
Create, manage and edit groups through the User Administration tool’s Chat Groups tab. Click “Add Group” to create a new group of users.
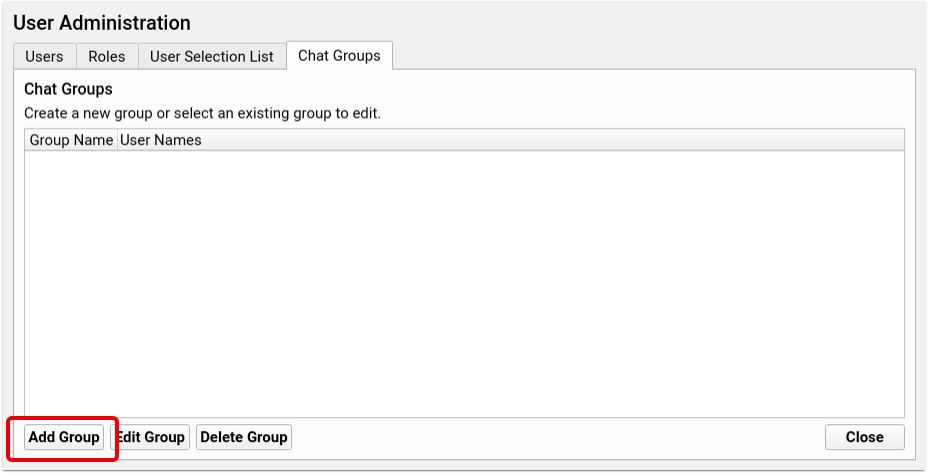
Check the box alongside each user’s name to add that user to the new group. Name the group at the top of the window and click save. Each group name can only be used once, so you won’t be able to duplicate group names, but to avoid confusion, be sure that your group names don’t match existing users. For example, if you have a user called “Nurse” make sure to name your group of nurses something like “Nurse Group” to differentiate the group from the individual.
When you’ve created one or more groups, they’re available in the chat window’s “To” menu.
You can edit or delete groups at any time in the User Administration tool. To add or remove users, or rename a group, select the group in the Chat Groups tab and click Edit.
Check or uncheck the box to add or remove a user, then click Save.
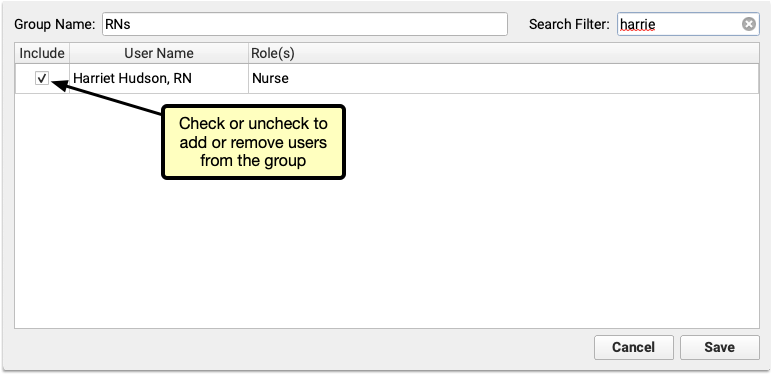
When a user is removed from the group, they’ll still be able to see the message history, but will no longer see any new messages or have the option to send messages to the group.

If your practice deletes a group, the same is true. Each user will be able to see the history of the conversation, but the option to send a message will be removed, and replaced with “This conversation is closed.”
Review Custom Report Settings
PCC 8.15 introduces many Report Library improvements. Although none of the improvements changed your custom report settings, the settings you already had in place might now work a little differently.
-
Encounters by Billing Status Report: Check the settings of your custom Encounters by Billing Status reports. If they are set up to report on all locations and/or all encounter types, hospital and billing-only encounters will be included in the report results.
-
Billed Diagnoses by Date Report: Check the settings of your custom Billed Diagnoses by Date reports. If they are set up to report on all locations, hospital encounters will be included in the report results.
Update Your MacOS 10.12 or 10.13 Workstations and Your Windows 7 PCs
When a manufacturer stops providing security updates for an operating system, PCC ends support as well. If your practice is still using workstations that run Windows 7 or MacOS 10.12, that support has already ended and you should upgrade those machines.
Apple is expected to end support for 10.13 in 2021. PCC 8.15 includes a reminder at login to review and update your workstation’s operating system. Contact PCC Support for recommendations.
PCC EHR requires a workstation running on Windows 8 or higher, or MacOS 10.14 or higher. For more information, read Hardware Guide: Your Personal Computer and Equipment.
Record Sexual Orientation and Gender Identity in a Patient’s Chart
Use PCC’s Sexual Orientation and Gender Identity components to securely record information in a patient’s chart. When a patient decides their gender identity is public, your practice can optionally display a patient’s pronoun and preferred name in the Appointment Book and elsewhere in PCC EHR.
Watch a Video: You can watch a video guide to these features: Record Sexual Orientation and Gender Identity.
Record Sexual Orientation in a Patient’s Chart
When your practice charts a patient’s sexual orientation, you can record the patient’s information in the Sexual Orientation component.
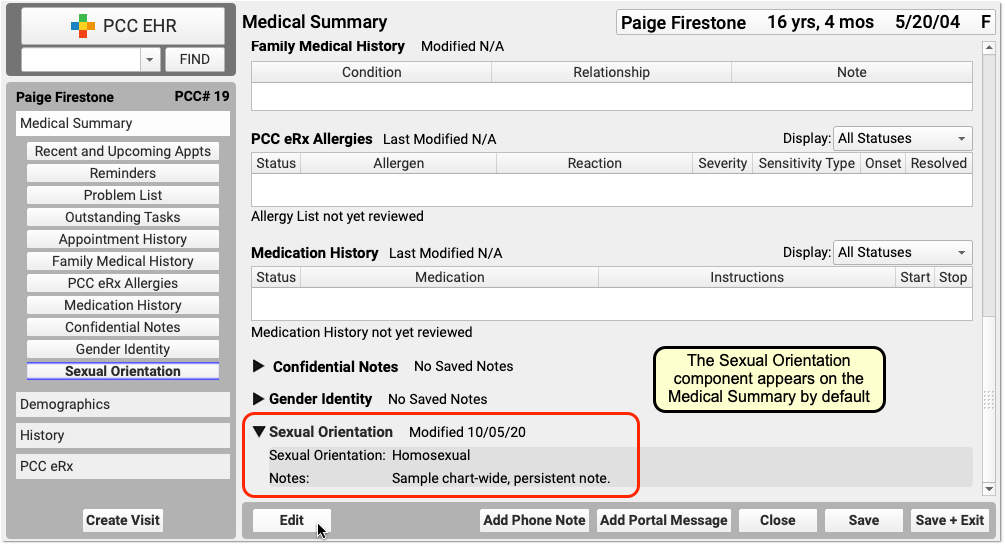
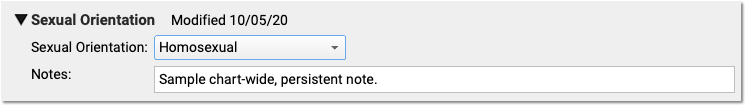
Your practice can add this chart-wide component to chart note protocols or anywhere you need it for your workflow.
Sexual Orientation is a Confidential Component: When you open a chart, the contents of this component are hidden. A clinician or other PCC EHR user must click the disclosure arrow to display the contents of the Sexual Orientation component. PCC EHR records that this information was accessed, and your practice can review who accessed the information in the PCC EHR Audit Log.
Record Gender Identity, Preferred Name, and Pronoun in a Patient’s Chart
Use the Gender Identity component to record a patient’s gender identity, preferred name, pronoun, and notes.
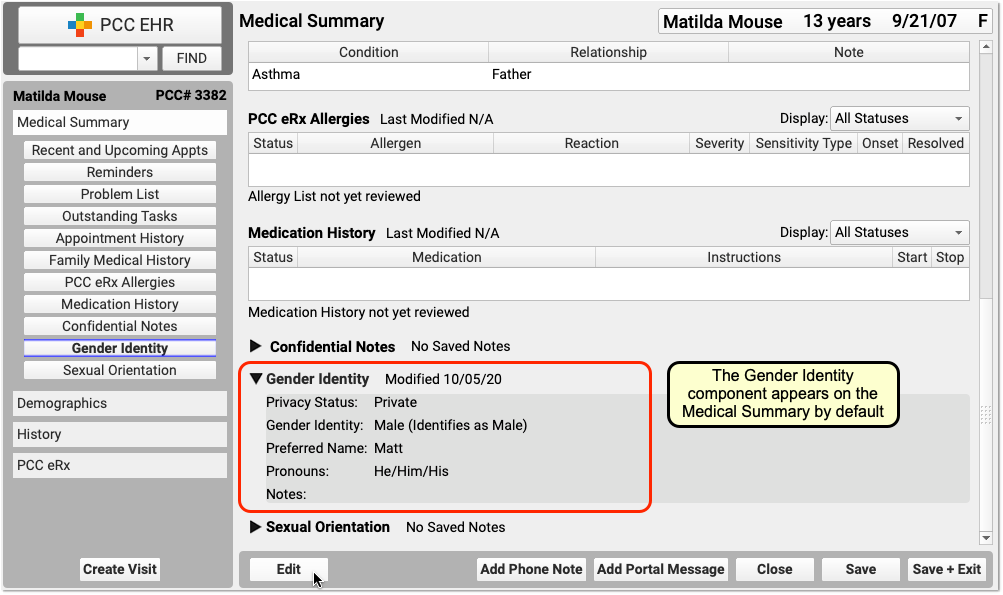
The component appears on the Medical Summary by default. Your practice can move it, remove it, and add this chart-wide component to chart note protocols or anywhere you need it for your workflow.
Patient information in this component is marked private by default. When private, the fields in the component are not visible anywhere in PCC EHR except in the Gender Identity component.
Gender Identity is a Confidential Component: When you open a chart, the contents of this component are hidden. A clinician or other PCC EHR user must click the disclosure arrow to display the contents of the Gender Identity component. PCC EHR records whenever this information was accessed, and your practice can review who accessed the information in the PCC EHR Audit Log.
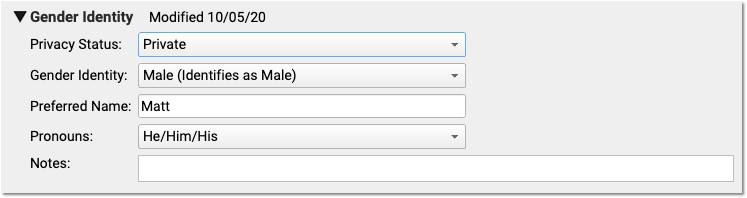
Make a Patient’s Preferred Name and Pronoun Visible On Various Screens in PCC EHR
When a patient’s gender identity information is no longer private, select Public in the “Privacy Status” drop-down menu.
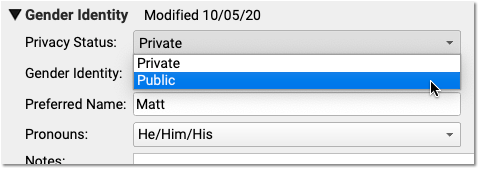
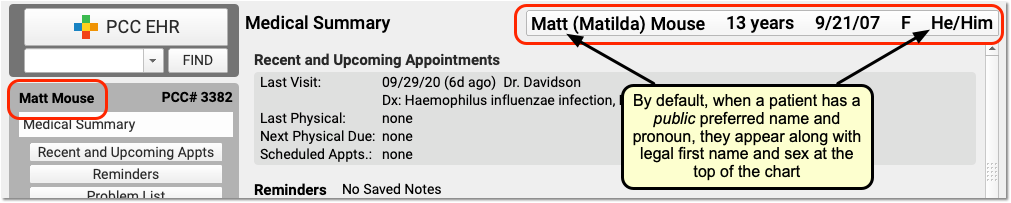
When Public is selected, PCC EHR and pocketPCC can display the patient’s preferred name and pronoun in the Patient Banner as well as in other places in PCC EHR.
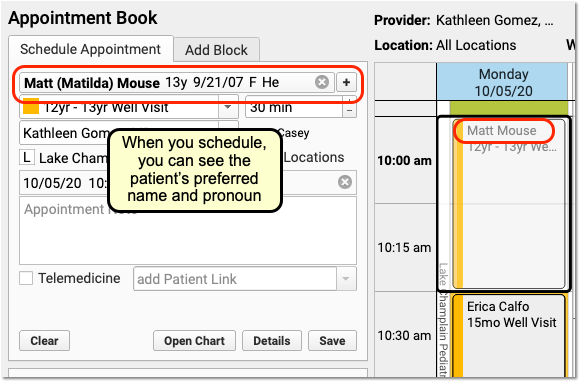
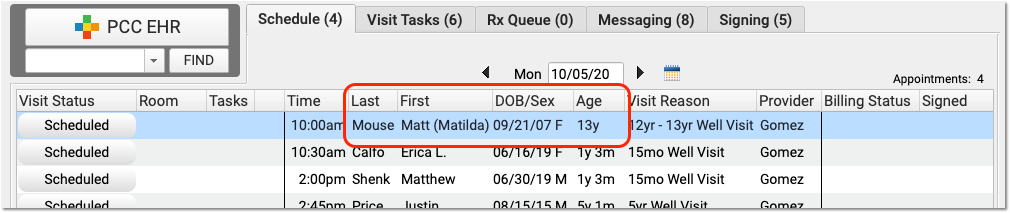
On the Appointment Book, for example, your staff will be able to see the patient’s preferred name and pronoun as they make an appointment. The preferred name can also appear on the Schedule screen and PCC EHR queues, except for the Rx Queue (which uses the patient’s legal name) and the E-lab Results queue (where a patient’s name is provided by a lab vendor). Your practice can find the patient by searching for either the preferred or legal name.
The patient’s preferred name can also appear at the top of forms and patient and family-facing reports that include the green name header. This includes the Patient Visit Summary:
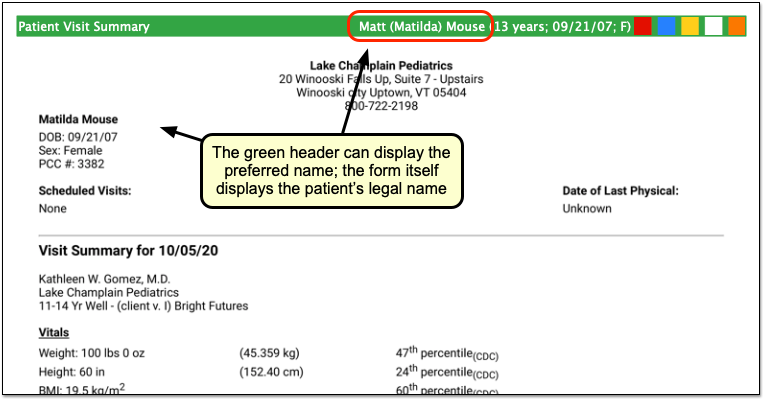
Note that the patient’s legal name and sex appear elsewhere on the form. Documents that can include the preferred name in the green header include: Care Plans, PDF versions of Continuity of Care Documents, Growth Charts, the Health Information Summary, Lab Order Details, the Patient Visit Summary, Summary of Care Record, and Visit and Billing History printouts.
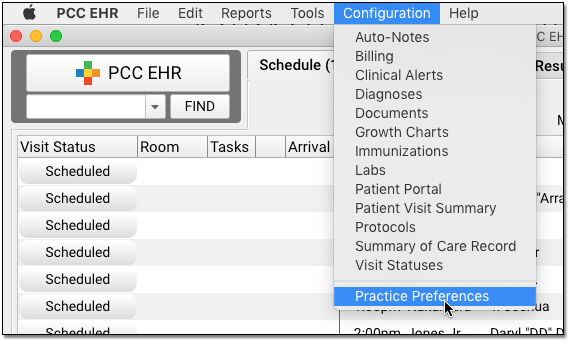
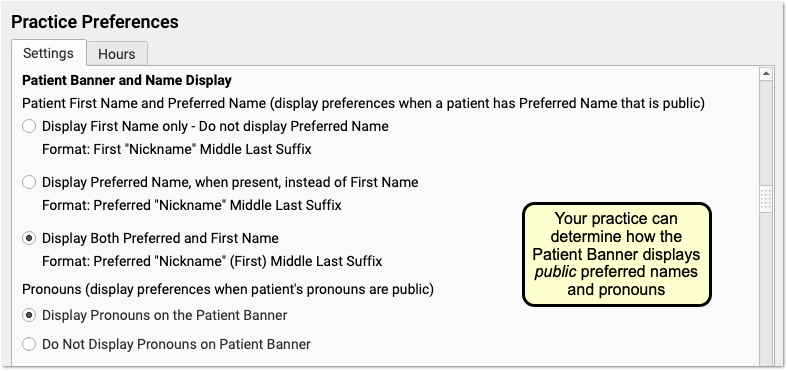
Configure How Your Practice Displays Preferred Name and Pronoun
A patient’s preferred name and pronoun do not appear at all if their Gender Identity component is set to Private. Your practice can configure whether PCC EHR displays only a patient’s legal name, only the preferred name, or both the legal and preferred names when they are set to Public in a patient’s chart. You can also optionally turn off the preferred pronoun display.
Open Practice Preferences to review your options.
In addition to adjusting your practice’s display preferences, your practice may wish to change the location of the component. You can also adjust your practice’s existing workflows for patients. For example, if a patient’s preferred name was kept in the Nickname field in Demographics, you can use the Gender Identity component instead.
Other PCC EHR Tools to Support Patients: Some practices use a patient status flag, an entry in the Reminders component, or a Clinical Alert to inform clinical staff when a patient has gender identity information they should be aware of. For example, if a patient shares private information about their gender identity with a clinician, the practice may record that information in the confidential Gender Identity component. A flag and a corresponding Clinical Alert could inform clinical staff that they should review that component prior to the appointment.
Fall 2020 SNOMED-CT and ICD-10 Updates Add COVID-19-Related Issues and Other Diagnoses
On September 20th of 2020, PCC updated the SNOMED-CT diagnostic terms and the ICD-10 diagnosis billing codes on your practice’s system.
PCC regularly updates your system’s ICD-10, LOINC, SNOMED-CT, NDC, RVU, VIS, and other standardized lists so you won’t encounter challenges when you chart, order a lab, interface with a care provider, or bill for a visit. (Your practice’s local system automatically updates your practice’s procedure code validation, as well.)
In PCC EHR, clinicians enter diagnoses using SNOMED, which maps to ICD-10 billing codes for claims. We updated both of these codesets in order to provide you with the most up-to-date diagnostic language in the chart, and to support the 2021 edition of ICD-10, which takes effect for dates of service after 2020-10-01.
Read the sections below to learn about the updates, educational opportunities, and diagnosis codes and descriptions of particular interest to pediatricians.
Use 2021 ICD-10 Diagnosis Billing Codes, Including New COVID-Related Codes
The 2021 ICD-10 update includes new sections for COVID-19-related infections and vaping-related disorders. You can review the complete, updated guidelines in the CDC’s ICD-10-CM Official Guidelines for Coding and Reporting.
The new codes and guidelines take effect for dates of service starting on 10/1/2020. You can learn about the updates that are of most interest to pediatric practices by attending PCC Web labs held by Jan Blanchard (CPC, CPEDC). Missed a web lab? You can watch a recorded session as well.
In addition to COVID-19 and vaping-related guidelines and codes, Jan notes that the 2021 ICD-10 update includes more specificity for substance abuse codes, several adjustments to influenza coding, and new codes for reflux, headaches/face pain, and more. In the “curiosities” bucket, the update includes “Pedestrian on electric scooter and standing micro-mobility pedestrian conveyance (hoverboard, segway)” added to V00-V06.
Chart Diagnoses Mapped to Deprecated ICD-10 Billing Codes: Were there any 2021 code changes for items that your practice frequently bills? You can review your system configuration using the snomedmap report. While there were no major disruptions in the 2021 ICD-10 update, it’s always worth taking a look at your code mapping reports to head off any billing challenges.
Use the Latest SNOMED Diagnoses, Including New COVID-Related Descriptions
The SNOMED-CT update includes thousands of new descriptions for diagnoses, allergies, therapies, and procedures. It also updates thousands of text descriptions for diagnoses and their mapped ICD-10 billing codes. You can review information about the update on the National Library of Medicine website.
Review Your COVID-19 SNOMED to ICD-10 Mapping: As codesets continue to change in response to COVID-19, PCC recommends you review the diagnoses you use to chart and bill for COVID-19 issues. For example, this update includes a new recommended mapping of the Exposure to SARS-CoV-2 SNOMED description to the Z20.828 ICD-10 code. This mapping was not included by default in the previous SNOMED standard. You can double-check your practice’s diagnosis billing configuration in the Billing Configuration tool.
New COVID-19-Related Diagnosis Descriptions
The update includes 22 new diagnoses for the use of identifying when an issue is related to COVID-19. For example, there are new descriptions for otitis media and several new descriptions for respiratory distress and infections, pneumonia, bronchitis, and similar. For a complete guide to COVID-19-related descriptions, you can read the COVID-19 section of the SNOMED-CT International Release Notes.
| Acute bronchitis caused by SARS-CoV-2 |
| Asymptomatic SARS-CoV-2 |
| Acute hypoxemic respiratory failure due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Acute kidney injury due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Acute respiratory distress syndrome due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| At increased risk of exposure to Severe acute respiratory syndrome coronavirus 2 |
| Cardiomyopathy due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Conjunctivitis due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Dyspnea caused by Severe acute respiratory syndrome coronavirus 2 |
| Encephalopathy due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Fever caused by Severe acute respiratory syndrome coronavirus 2 |
| Infection of upper respiratory tract caused by Severe acute respiratory syndrome coronavirus 2 |
| Lower respiratory infection caused by SARS-CoV-2 |
| Lymphocytopenia due to Severe acute respiratory syndrome coronavirus 2 |
| Myocarditis due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Pneumonia caused by SARS-CoV-2 |
| Otitis media due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Rhabdomyolysis due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Sepsis due to disease caused by Severe acute respiratory syndrome coronavirus 2 |
| Severe acute respiratory syndrome coronavirus 2 detected |
| Severe acute respiratory syndrome coronavirus 2 not detected |
| Thrombocytopenia due to Severe acute respiratory syndrome coronavirus 2 |
New Favorites Available in Diagnosis Quick Search
The update adds 2043 diagnosis descriptions to your system. PCC added 245 of them to the “Favorites” quick search feature of all diagnosis fields in PCC EHR.
In preparation for the update, PCC’s certified coder, Jan Blanchard, assembled a list of 245 new SNOMED-CT descriptions of interest to pediatricians. The update added these diagnoses to your practice’s default Favorites list for quick searching, unless your practice has specifically requested otherwise.
What is a diagnosis 'Favorites' list?: As you type or search in any diagnosis field, PCC EHR automatically searches a customizable list of Favorites. Use the Diagnosis Configuration tool to adjust your practice’s list of Favorites. You can also right-click on any diagnosis field in PCC EHR to search your system’s full SNOMED-CT diagnosis library.
You can review the list of 245 new Favorite descriptions. Attend PCC’s monthly coding weblabs to learn more about the new descriptions and other coding topics.
Deprecated SNOMED Diagnosis Descriptions
The Fall 2020 SNOMED-CT update removes or replaces many codes common to pediatric practices. Your practice may want to take special note of them.
Here are the top 25 codes from PCC’s pediatric practices that have been removed from the SNOMED-CT diagnosis library in 2020. When these codes appeared for selection on a chart note protocol, PCC added a replacement if available. For other diagnoses, your providers can usually find new appropriate descriptions with a search, but you may want to plan ahead.
| Allergy to edible egg | 91930004 |
| Seborrhea | 86708008 |
| Sprain, ankle joint, lateral | 209532000 |
| Allergic reaction to insect bite | 213024000 |
| Dermoid cyst of skin | 276729007 |
| Hearing loss in right ear | 1091501000119106 |
| Pilonidal cyst with abscess | 85224001 |
| Allergic reaction, due to correct medicinal substance properly administered | 57302007 |
| Toxic erythema | 58767000 |
| Infective hepatitis immunization | 275849001 |
| Sprained finger/thumb | 287097007 |
| Adverse effect, due to correct medicinal substance properly administered | 45376003 |
| Pilonidal cyst without abscess | 76545008 |
| Adverse reaction to vaccine properly administered | 699017007 |
| Allergic reaction to bite and/or sting | 418484009 |
| Gastrointestinal allergy to food | 414314005 |
| Photosensitization due to sun | 258155009 |
| Sprain of toe joint | 262998001 |
| Angioedema of eyelids | 402405007 |
| Angioedema of lips | 402406008 |
| Adverse drug reaction resulting from treatment of disorder | 708809007 |
| Discharge of eye | 18628002 |
| Allergic reaction to systemically administered drug affecting oral mucosa | 702559001 |
| Facial seborrheic dermatitis | 402210009 |
SNOMED Codes Mapped to ICD-10 for Billing
The SNOMED-CT update includes new mappings to ICD-10 billing codes. Many previous mappings have been updated.
You may wish to review billing configuration for your diagnoses. You can open the Billing Configuration tool to configure which ICD-10 diagnoses are mapped to each SNOMED-CT description in PCC EHR. You can also use the snomedmap report tool to examine your practice’s diagnoses that may need updating.
Schedule Reports in PCC EHR
You can schedule reports to run in the future in PCC EHR.
Schedule a Report to Run Automatically
Use scheduled reports to automate recall lists, billing oversight reporting, and other workflows.
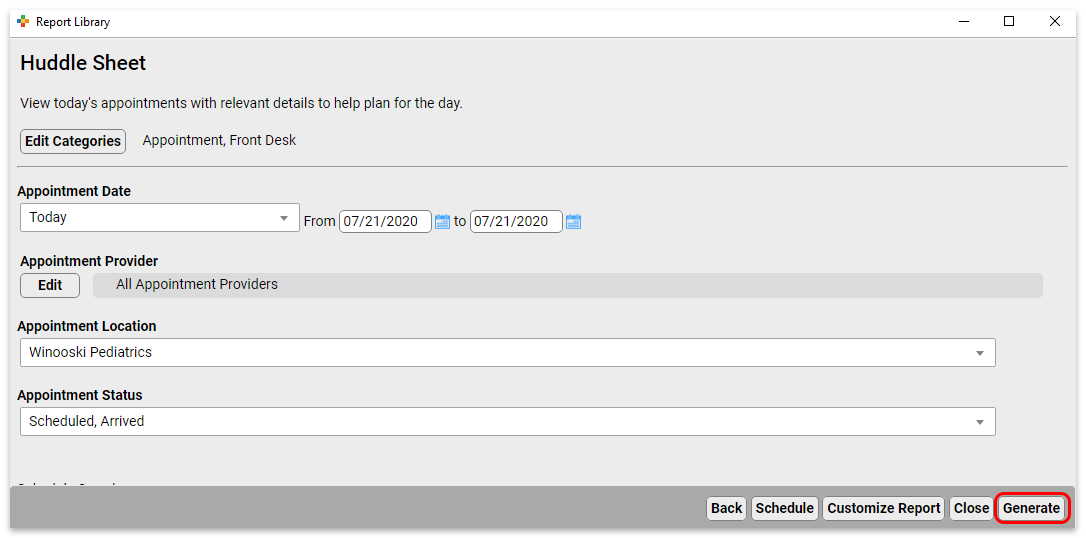
Select a Report
Open the Report Library and select the report you would like to schedule.
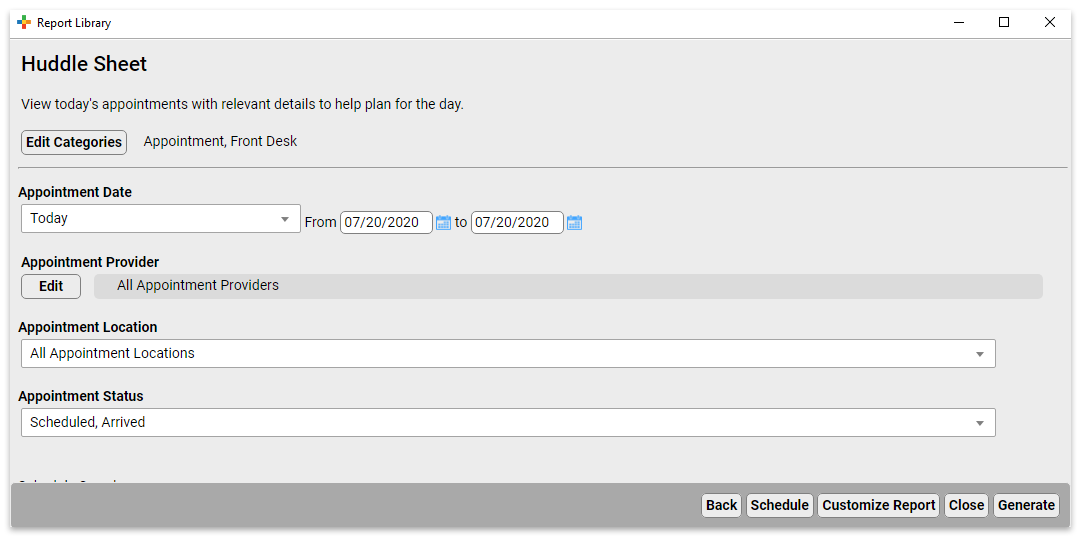
Set Report Filters and Click “Schedule”
Set the filters for the report, then click “Schedule”.
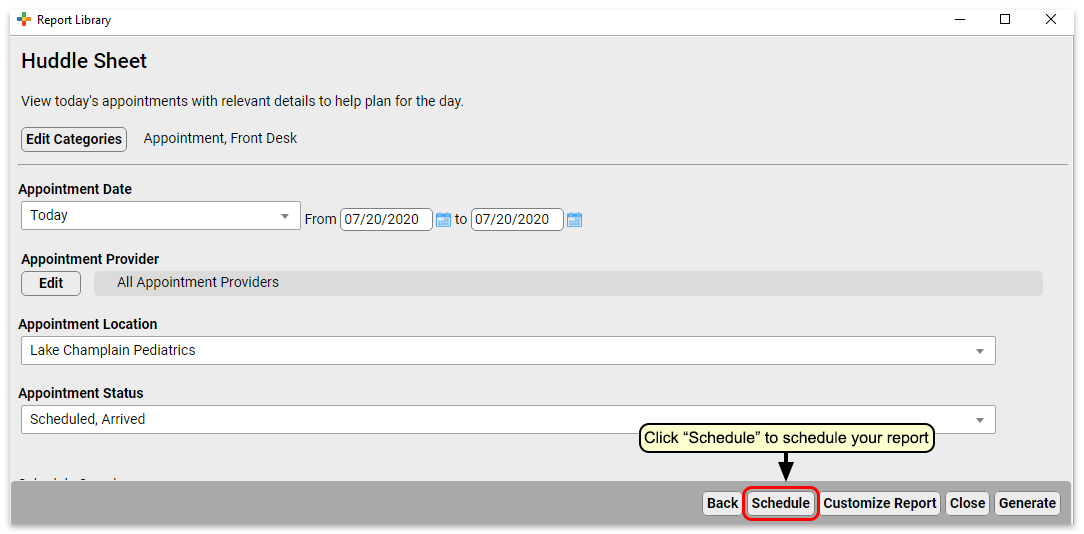
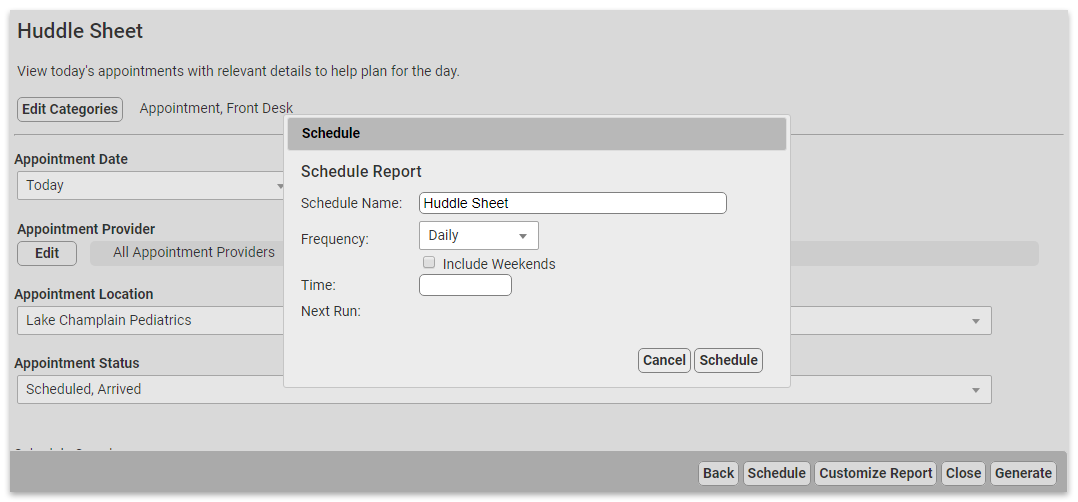
Set up the Report Schedule
Choose a name for this scheduled report and the frequency at which you want it to run. You may want to schedule multiple instances of the same report with different filter settings, or to run on different schedules. Choose a name that will help identify which instance of a report this is.
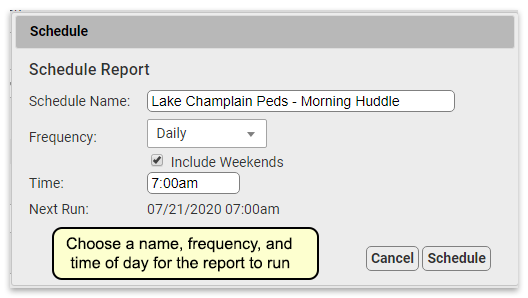
Finish Scheduling the Report
Click “Schedule” to finish scheduling the report.
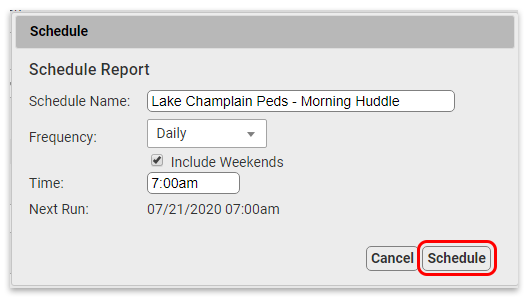
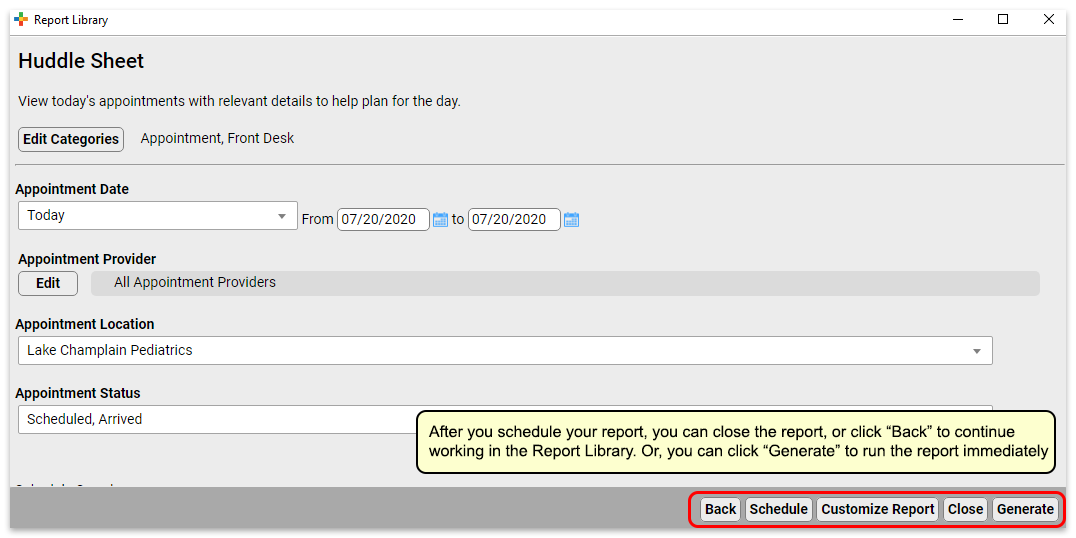
Your report is scheduled. If you’d like, you can click “Generate” to generate the report immediately or move on to other tasks.
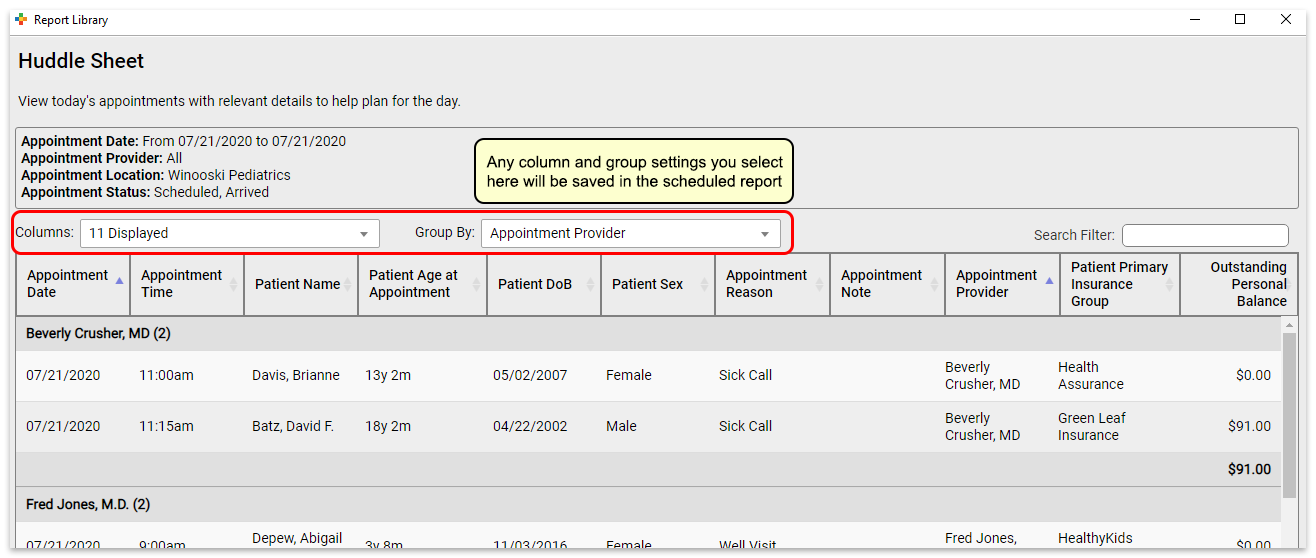
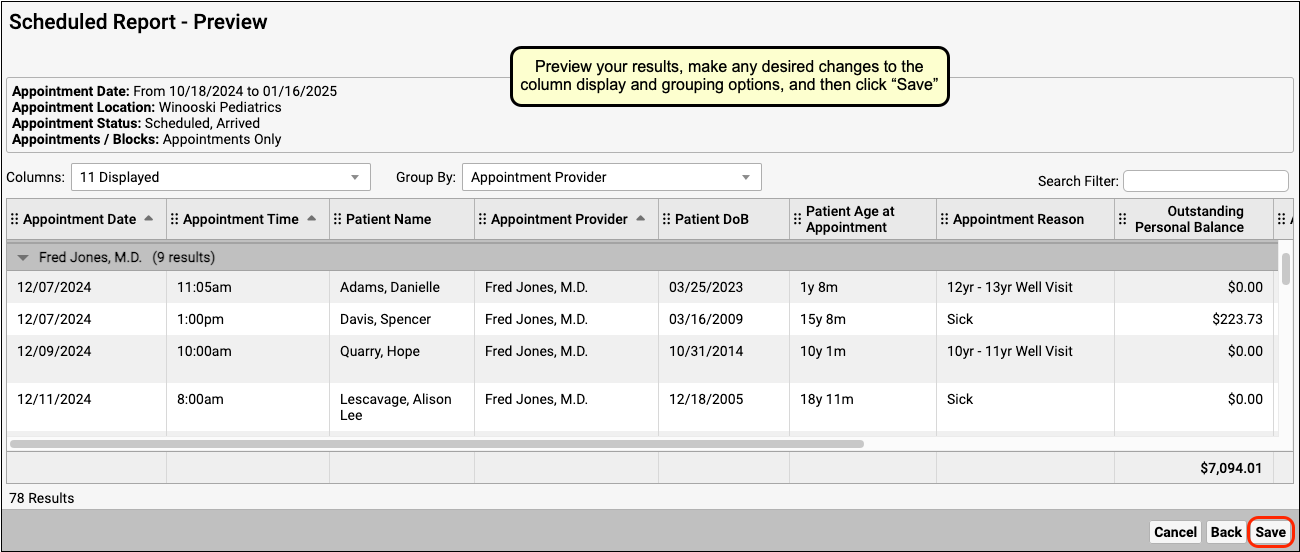
Preview Results and Save Output Settings
What if you want to check the output of the report before you schedule it, or you want to save column and group by (subtotaling) settings with your output? You can schedule from the results page of a report, which will retain any column and group settings you configure.
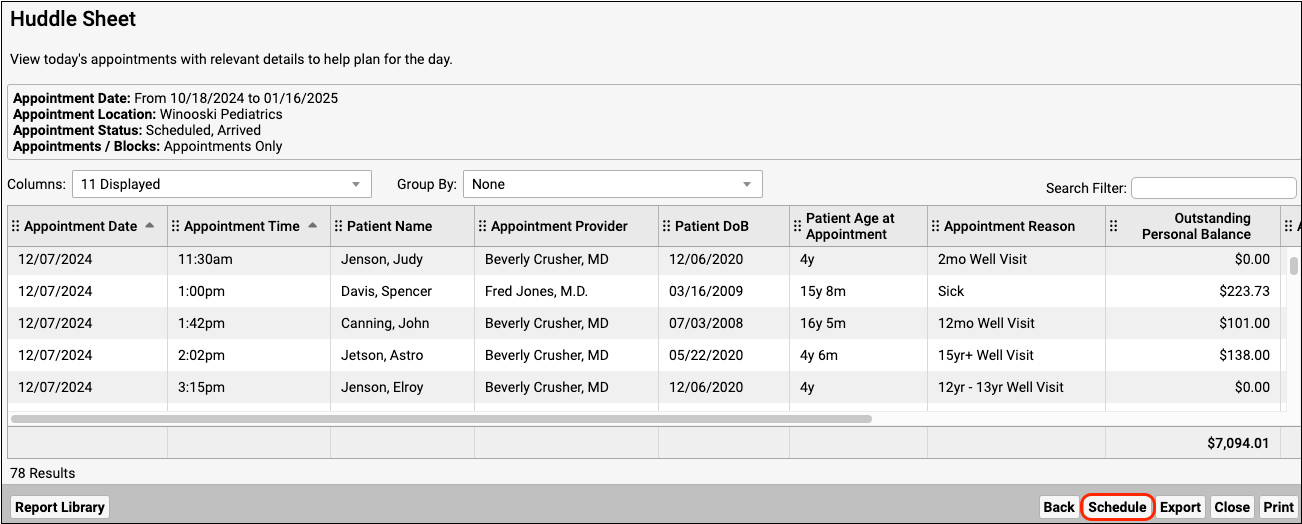
Reports scheduled in this manner will retain any column and group settings you configure here.
View Scheduled Report Results
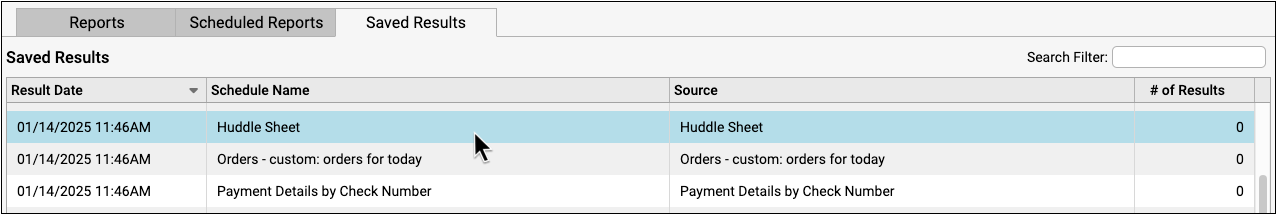
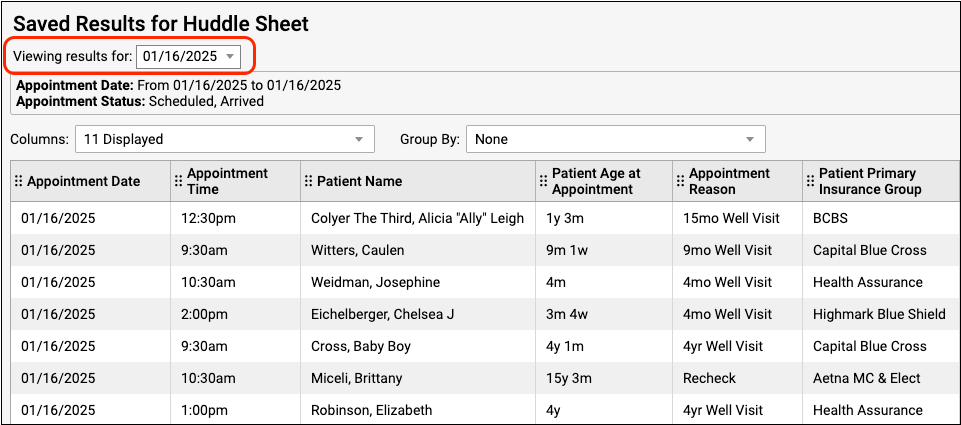
You can view scheduled report results in the Saved Results tab.
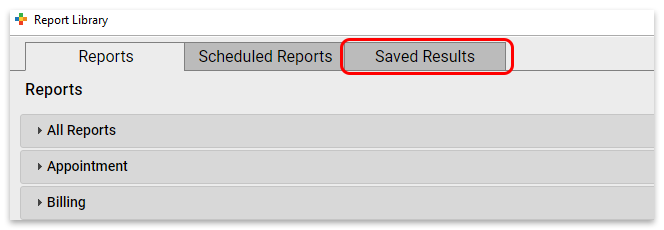
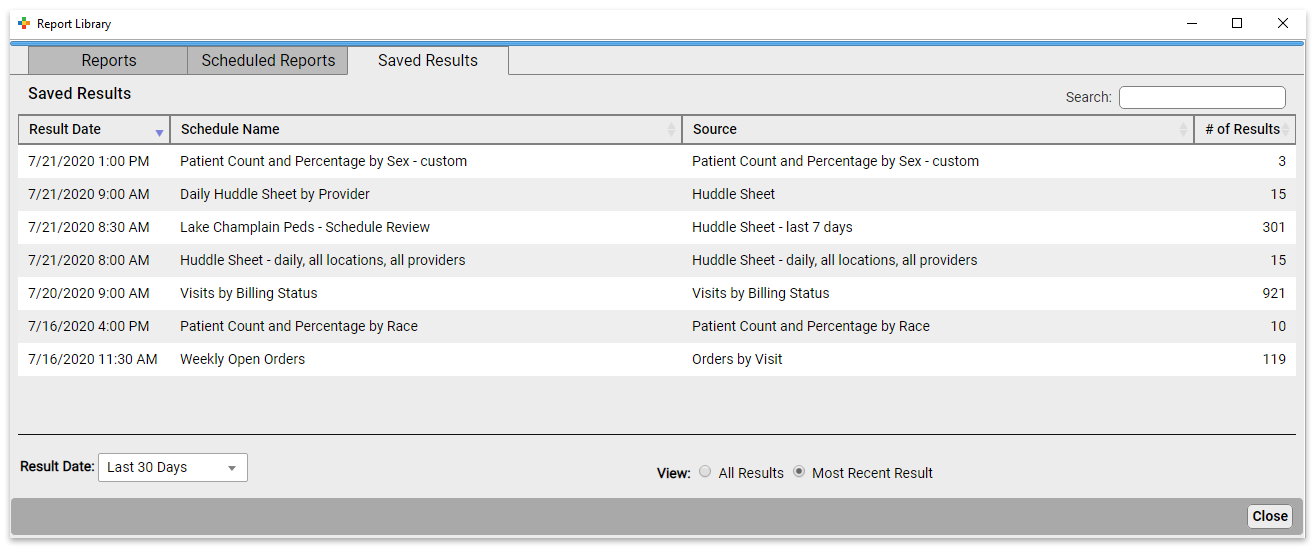
Here you can see the results for all scheduled reports.
You can see the date the report was run, the name of the schedule, the name of the source report the scheduled report was based on, and the number of results in the report.
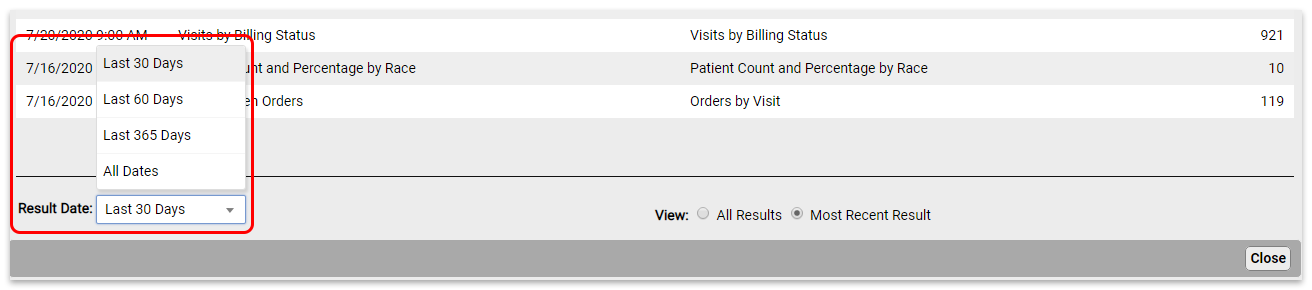
To see reports that last ran more than 30 days ago, change the “Result Date” filter setting.
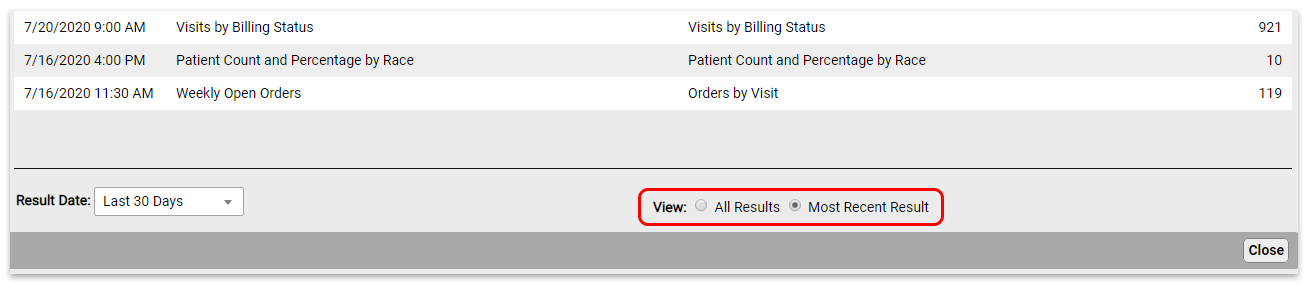
By default, you will see only the most recent results for each scheduled report. To see all results, change the “View” filter setting.
Click on the report you want to view to open the results.
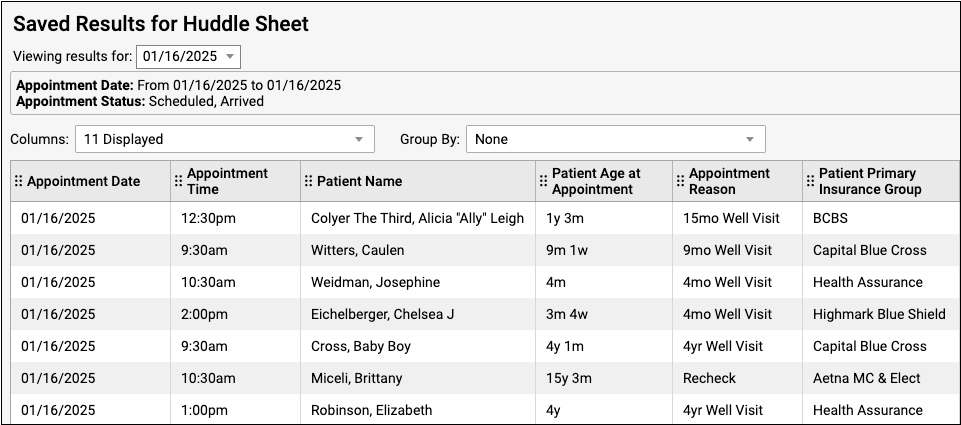
From here, you can export or print the results.
If a report has been run more than once, you can use the drop-down at the top of the report results to switch between results without going back to the Results tab.
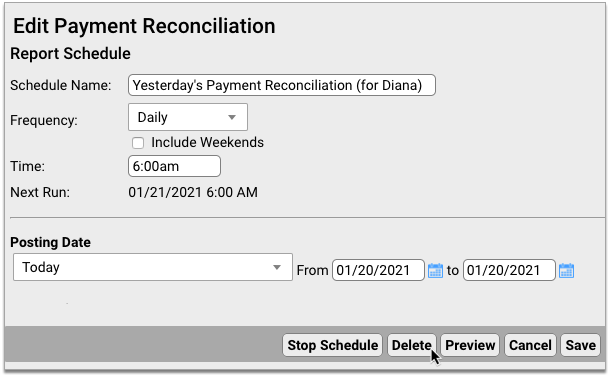
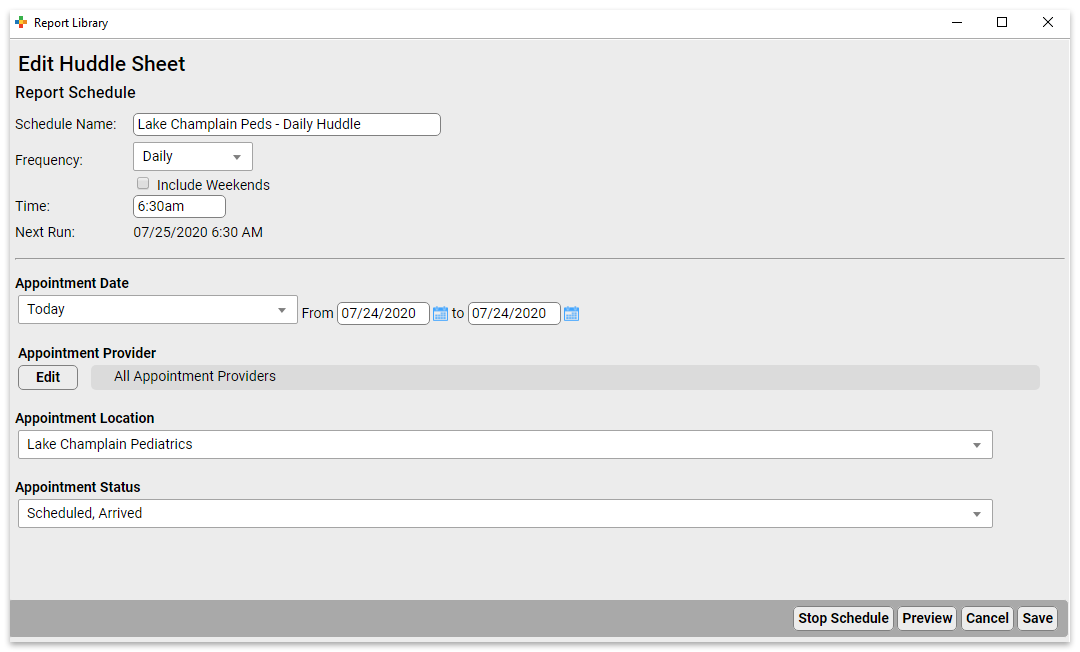
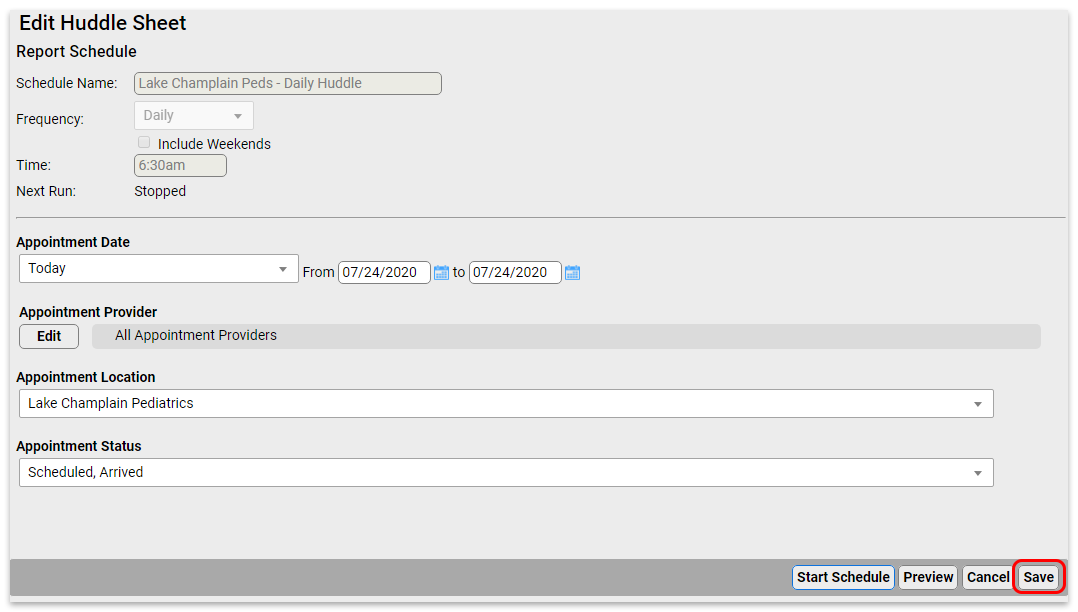
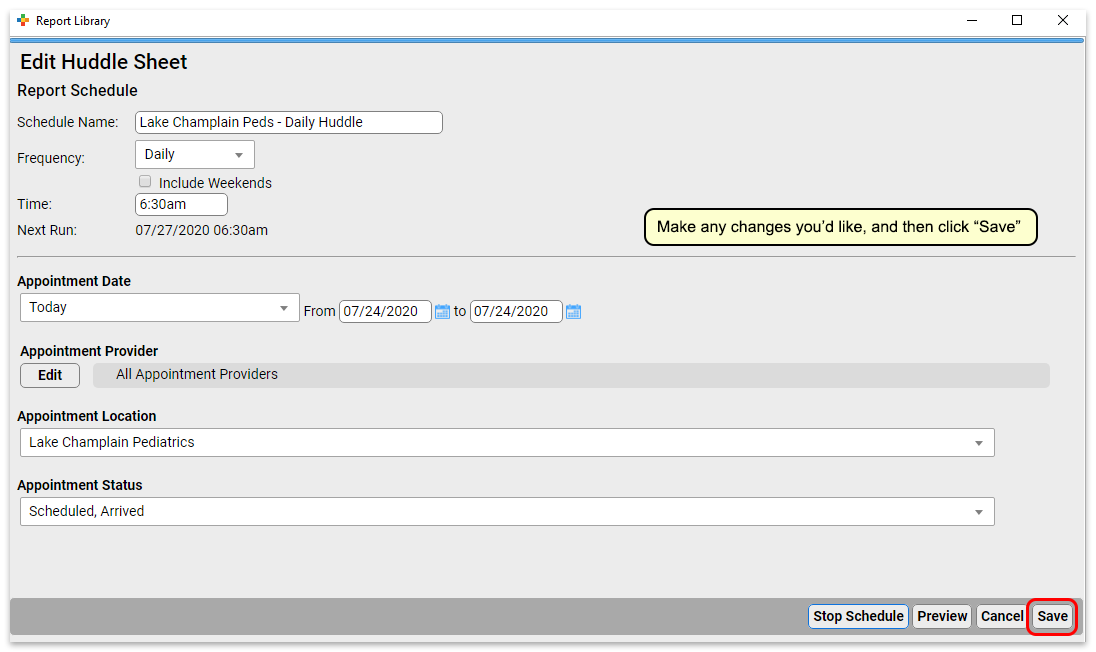
Edit Scheduled Reports
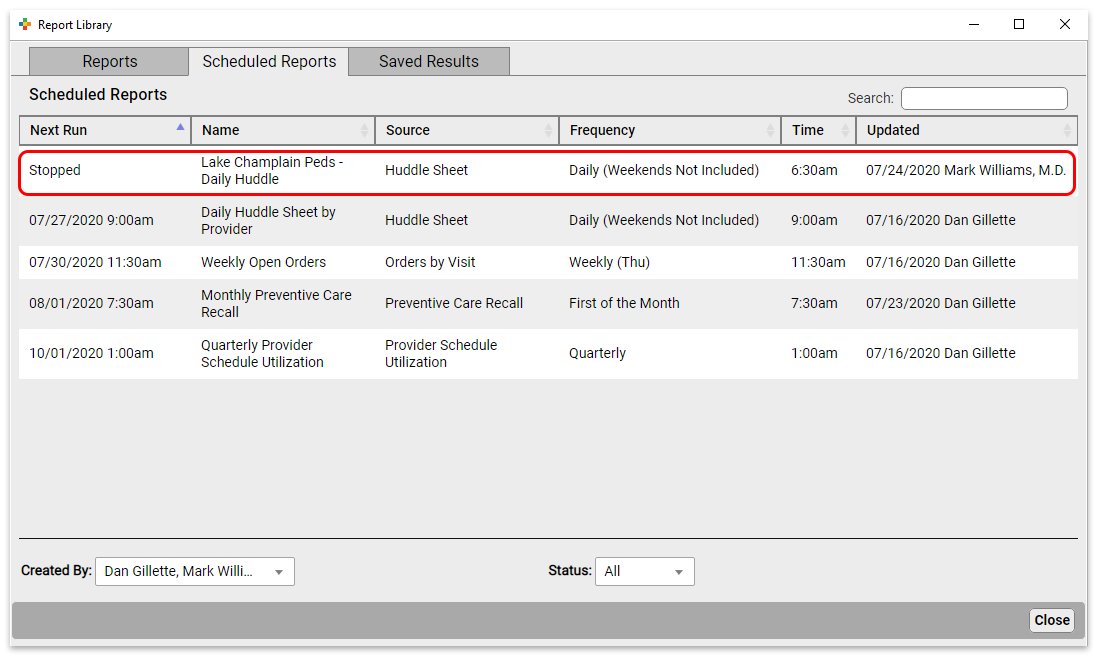
To edit a report, click the Scheduled Reports tab. Here you can see all scheduled reports.
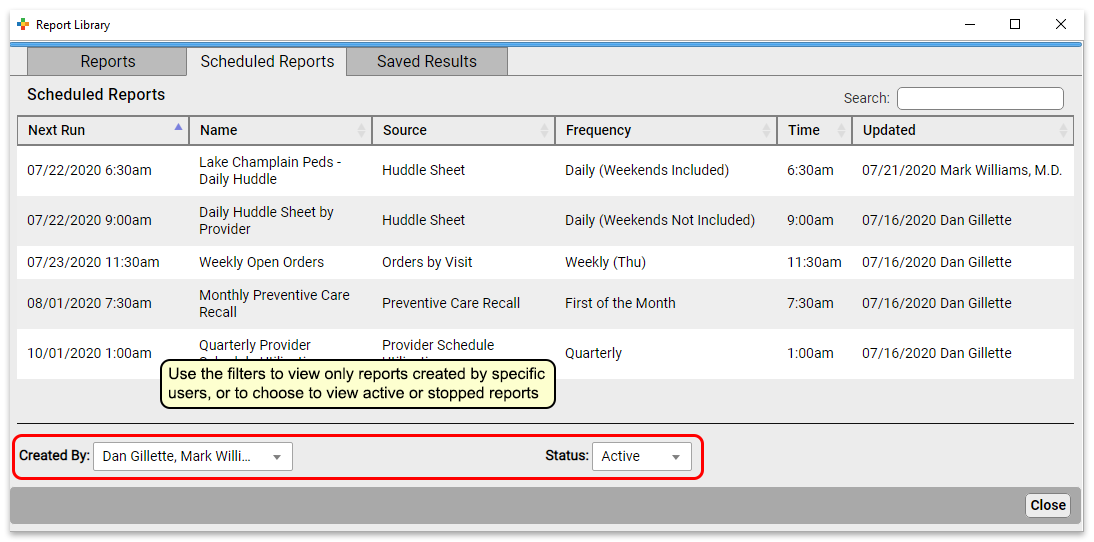
Click a report to edit it.
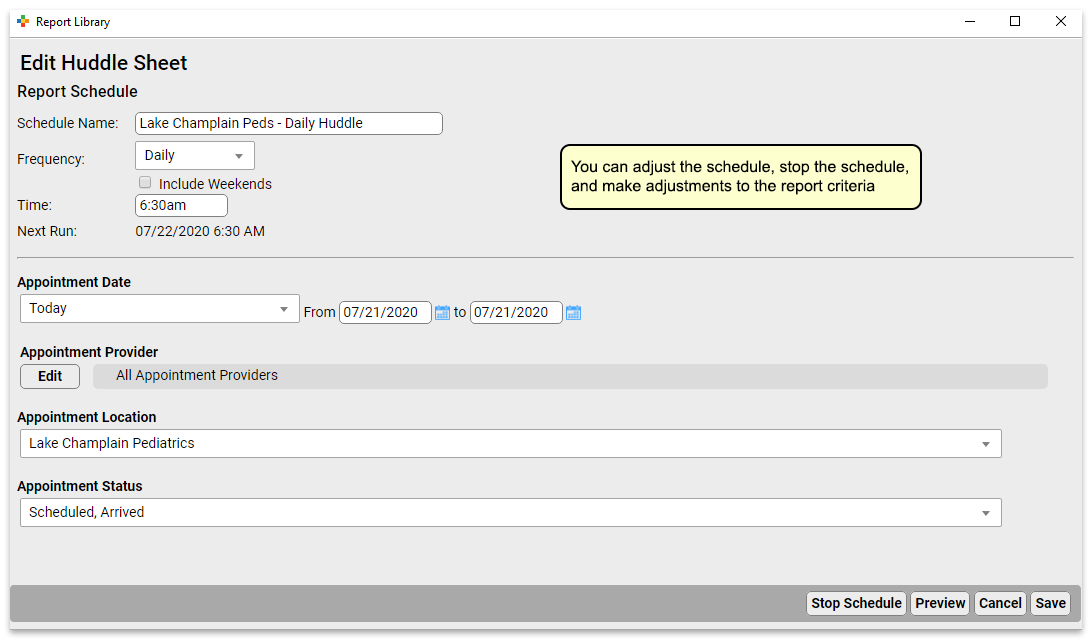
At the top of the report, you can change the schedule name, and the frequency and time the report will run. Below that, you can adjust the filter settings for all future runs of this report.
Click “Save” to save your edits. Or, if you’d like to make edits to the output formatting or to preview your report, click “Preview” to view report results.
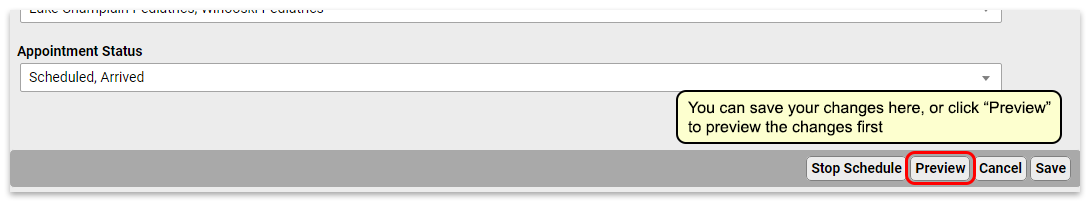
Previewing Reports Takes Time: Previewing a report will run an instance of the report. If it’s a report that takes a long time to generate, this will take a while.
Stop and Start Reports
To stop a scheduled report from running, open it from the Scheduled Reports tab.
Click “Stop Schedule” to stop running the report.
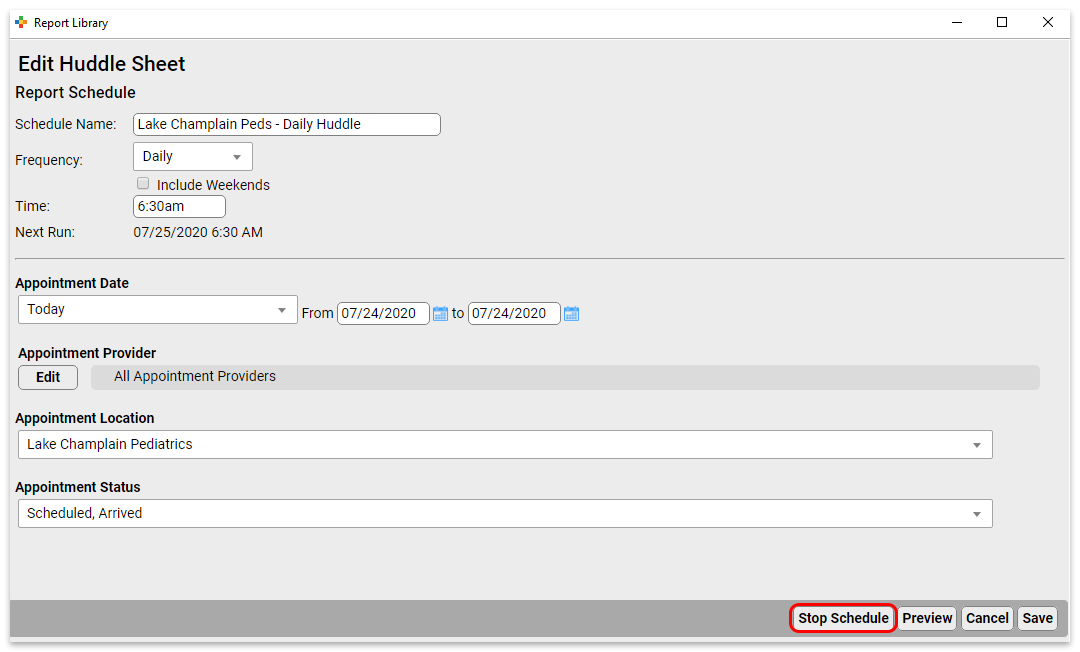
Click “Save” to commit the change.
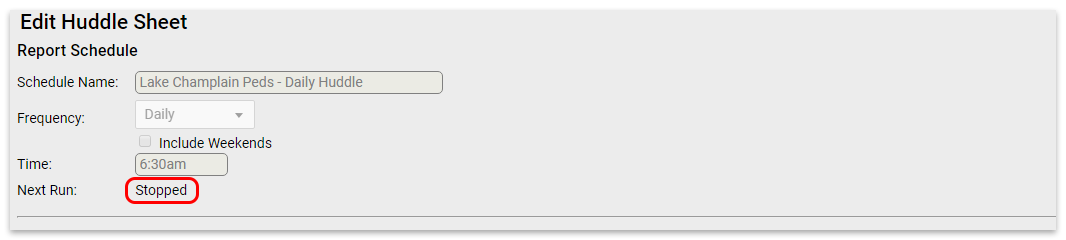
To start a previously stopped report, open it from the Scheduled Reports tab.
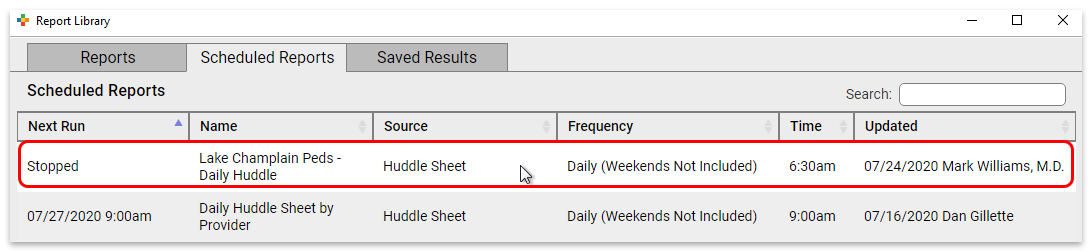
Click “Start Schedule” to activate the report.
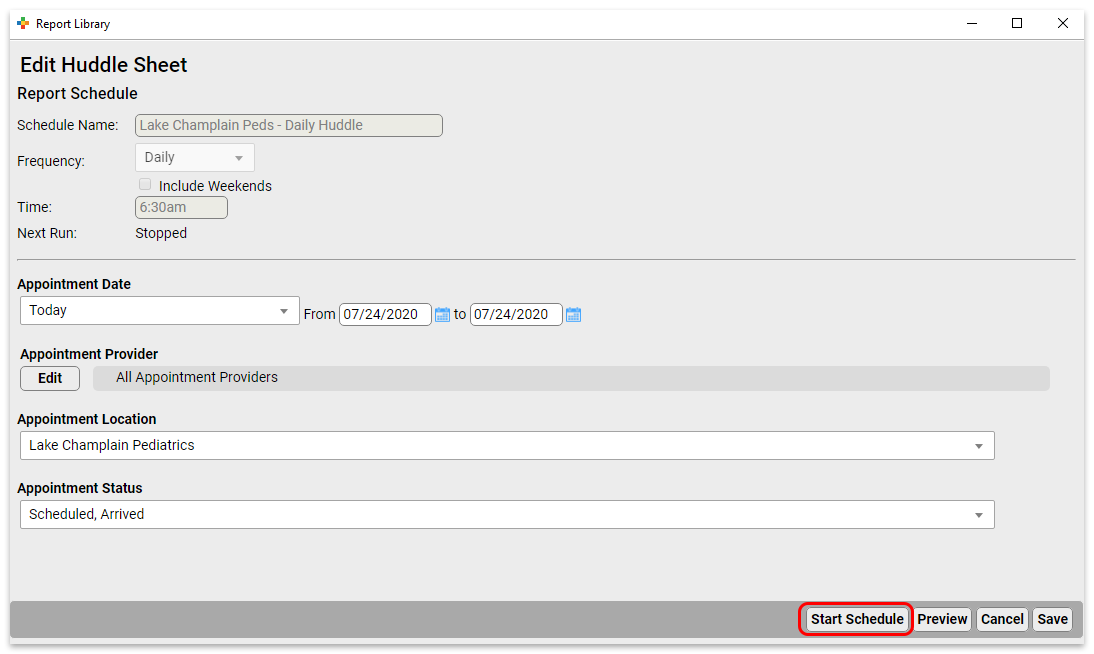
Make any adjustments you want to the name, frequency, and filters, and then save (or preview and save) the report.
Delete Scheduled Reports
To delete a scheduled report from the Report Library, open it from the Scheduled Reports tab.
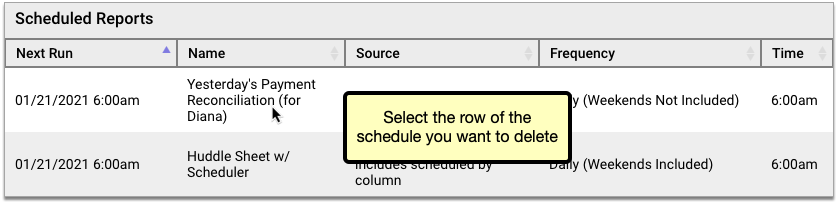
Click the “Delete” button, then confirm that you truly want to delete the schedule.
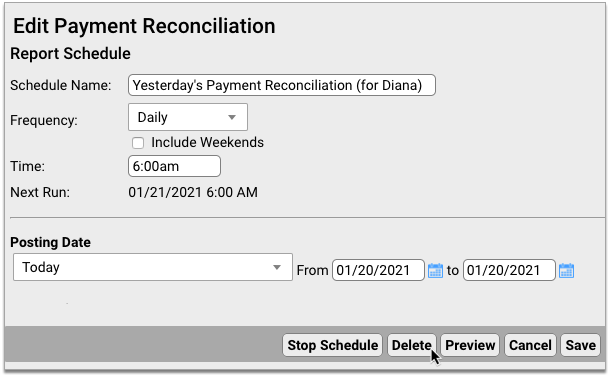
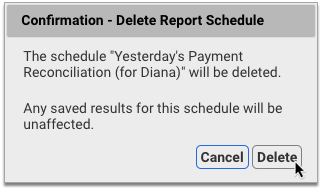
Deleted schedules are permanently removed from the Report Library and cannot be re-enabled. You can continue to view past saved results of deleted scheduled reports in the Saved Results tab of the Report Library.
Run a Pediatric Drive-Up Flu or COVID-19 Shot Clinic
Your practice can use PCC EHR to perform a shot clinic while also meeting COVID-19 safety protocols.
PCC has worked with several practices who are running “drive through” or “curb side” flu clinics. In addition to providing your families and communities with a vital service, by running a drive through flu shot clinic, you can prepare your practice for for participation in other vaccine clinics, such as expected upcoming vaccinations for COVID-19.
Learn More From the Experts: PCC spoke with several practices to draw together the ideas and tips below. We especially learned a lot from Dr. Jeanne Marconi, who delivered a seminar sharing her experience and expertise in running this kind of flu clinic. You can watch a recording of her seminar.
Check Out PCC's Blog Post: PCC posted a great guide to How to Open a Drive Thru Flu Clinic at a Pediatric Practice! It includes our notes below and so much more. Take a look!
Watch PCC Pediatric Flu Clinic Roundtable: In September of 2020, PCC hosted a Flu Clinic roundtable, talking about drive-thru strategies and more!
Pick a Location
If you’re reading this article, then your practice wants to run a vaccine clinic, but (especially during COVID-19), you do not want to do so in your physical office space. Where can you hold an outdoor, drive-thru flu shot clinic?
You may have a parking lot or other large enough area near your practice to support a drive-through clinic, or you may not. A local business might. Consider reaching out to banks, stores, and/or your local municipality to find a location.
If your practice does not own your parking lot, you may wish to take additional precautions or seek permission.
You may want to double-check your location’s general liability policy. It usually covers things that happen in your parking lot, even if you rent or lease your property. You may want to share your policy with your landlord, or connect with your insurance company to discuss the issue.
Prepare Things You Will Need
How will you maintain the cold-chain for your vaccines? Do you need traffic cones? What additional PPE will you need? And can you buy a tent from Walmart?
Some practices erect pop-up tents for checkin and administration stations. You’ll need to plan time for erecting and disassembling your tents. If there’s no rain, you might decide to skip the tent that day.
The CDC website hosts an excellent preparation checklist that covers the more serious issues, like vaccine storage, supplies, and rules around administration.
Plan for Safety
Your practice should plan the drive-up visit workflow to ensure safety. Ask yourself how you will “shepherd” cars, and where do they will wait when they pull in. Your location may have specific safety needs, and you will need to plan for traffic flow.
You should also make safety parameters clear to your families and all attendees. For example, instructing families that they should always stay in their car, and instruct staff to not approach a car until it has been placed in park.
You may need additional staff to help monitor and direct traffic so you are not blocking a major roadway.
Set Expectations and Get Your Staff On Board
You can hold a full, all-hands meeting: our practice is going to do a drive-thru flu clinic! Explain how this will help your families and your community. Every staff member plays a part, even if its just promoting the clinic at each contact point.
Dr. Marconi recommends having a “champion” on staff to be the point person, to help clarify and handle questions that come up. Offer food and other encouragement to your staff!
Pick a Date(s)
When will you host your drive-through flu shot clinic? You’ll need a date with adequate staff, and you’ll need to calculate how many patients or families you are likely going to be able to see.
Since you are looking for low traffic and wide open parking lots, a weekend date may work best.
Promote Your Drive-Thru Flu Shot Clinic
How will you get the word out?
Talk to families, use PCC’s Broadcast Messaging, and provide verbal reminders at every point of contact. Dig into social media, update your practice’s home page, Facebook, your phone hold announcement, and consider sending a press release to publications in your community.
Are you the first one in your community to offer this valuable service? Local media might help you promote the flu clinic, and/or report on it, which helps build your practice which in turn means you are better able to support your community.
Schedule Patients
How will you communicate your flu clinic “slot” availability to all patients and families? And how will they Schedule?
High volume visits mean that scheduling has to be easy. You can have families use of PCC’s portal message scheduling template so that families can pick a time or slot. You could also use a service like FullSlate, Calendly, or Acuity. These services create an online website for you so parents can easily sign up for an open slot.
Perform Pre-Visit Patient and Family Preparation
Your flu clinic will run best if you’ve worked with every family before the actual clinic. Send them the VIS beforehand, do pre-visit COVID-19 questions. When you speak with a family, always take the opportunity to do wellness questions, update information about patient chronic problem and care plan maintenance, and review their medications.
You can send the Influenza Vaccine VIS through PCC’s patient portal. You can also laminate a copy and hand it into the car at the time of service.
You can ask COVID-19 screenings ahead of time, or tell the family to expect them at the clinic. Remember to screen all occupants of the car at the time of service. Practices have developed alternative ways of asking kids COVID-19 screening tests, such as asking what they ate for breakfast and what it tasted like.
Use the Opportunity: You’ve got the family or patient on the phone? Use that opportunity to check in on all recall topics. Chronic disease management, updated immunizations, and more. You can schedule Telehealth and Well visits based on what you learn. You should also review and update demographics, verify insurance, and plan how they will pay! (Get credit card on file, for example.)
Plan For Payment
Many practices simply ask for “cash” payment for flu shots: for a non-office visit, occurring as fast as possible, billing insurance may not make sense for you.
Either way, your practice should work to make payment as touch-less and efficient as possible.
You can work with your financial services vendor to set up secure credit card on file, for example.
Set Up Your Intake Station and Your Shot Administration Station
To see patients quickly, you can have each car stop at two stations. First, an intake station for COVID-19 screening and prep, to help the family get ready (loosen clothes, set expectations), and to collect any forms. Next, the shot station, where the clinician should double-check the child’s age and consent, confirm the vaccine they believe they are receiving, administer the vaccine, confirm the patient appears well, and document that the vaccine was administered.
At each station, you’ll want signs (or hand-held posters) with “Stop Here” and “Put your Car in “P”ark!”. Someone should individually verify that a car is in park as they approach.
Have an Emergency Plan
Your practice already knows your emergency procedures when seeing patients at your practice. Take some time to review and update that plan for your drive-thru flu clinic.
If something goes wrong, or the patient has an emergency, everyone should know the plan. Who will call 911?
How Did It Go?
As with all new initiatives, things will go wrong. You’ll learn how to improve, what to do differently next time.
Send a survey to some patients or check in with families. Did it work? And ask your staff: They helped a huge number of patients in a short period of time! Congratulate and reward them for doing this.
Other Things We’ve Heard
Dr. Marconi shared that with practice and experience her staff can now manage to see 10 cars an hour. She uses a pre-check station, with 1 MA, followed by a shot station, with 1 staff. You can create multiple lanes as well.
We also learned from many PCC practices that a drive-thru clinic has a surprising bonus: kids are in their car seats, in familiar surroundings, and ready for what’s coming. Some administrations are harder in a car, but some are actually easier!
Your practice may also want to have a plan for “guest” flu shot customers. If someone is not a patient at your practice, how will you handle them? Schedule them for a new patient visit?
There are a number of great online resources for flu clinics and drive-thru flu clinics! Check out Sanofi’s resources, or the CPP Buying Group’s resources.
Code and Bill for E&M Office Visits
Upon completion of a sick visit encounter, a clinician selects an “Evaluation and Management” or E&M code. This is sometimes called the “office visit” level. E&M level selection is based on the clinician’s medical decision making or the amount of time spent on care for that patient on the calendar date of the encounter.
Procedure Code Guidance: The procedure codes discussed in this article are intended only as examples. You should consult the AMA’s current CPT Coding Guide and work with your insurance payers to verify what codes you should report on claims. Your practice updates and maintains your billable procedure list, codes, and prices in the Procedures table in the Tables configuration tool on your PCC system.
Why is E&M Code Selection Important to a Pediatric Practice?
E&M services make up a large percentage of the work you do as a pediatrician. They represent the cognitive work, information gathering, and decision making that goes into patient care. Because so much of the work you do falls under the umbrella of E&M, it’s vital that you code those services correctly. Many pediatricians under-code their encounters, resulting in significant lost revenue for their practice.
Documenting your encounters is not only important for continuity of care. It also supports collecting and retaining the revenue those services generate.
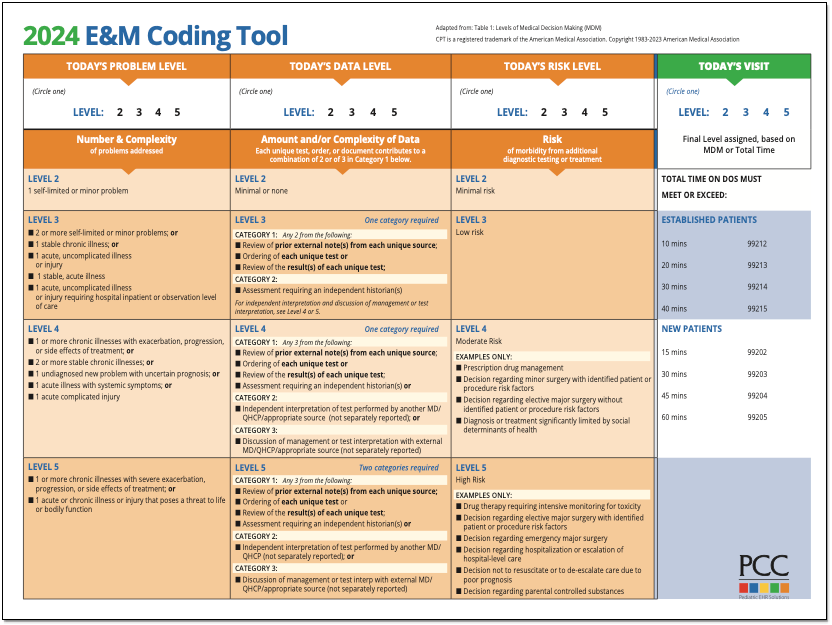
PCC’s E&M Coding Tool
PCC’s Jan Blanchard (CPC, CPEDC) developed a printable guide for E&M Coding.
2021 Transition Resources Archive
On January 1st, 2021, the guidelines for coding and billing an office visit changed significantly. PCC collected resources, created tutorials, and managed an FAQ at that time.
2021 Resource Guide: Some of the details below have changed since 2021. You should consult the current AMA CPT Coding Guide for the most up to date requirements and guidance. Reach out to PCC Support or attend a live PCC Billing Drop-In session to learn more.
How Do I Select an E&M Code for 2021 and Beyond?
For encounters that occur after December 31st, 2020, a clinician no longer uses history or physical exam performed during the encounter as criteria for code selection. Instead, they select a code based on either medical decision making or time spent practicing care for the patient on the day of the visit.
Here’s a brief explanation of how you select a billing code level for an “evaluation and management” or “Office Visit” after January 1st, 2021. These guidelines apply to common visit billing codes, such as 99212, 99213, 99214, or 99215, as well as to the selection of codes 99202 through 99205.
Select a Code Based on Medical Decision Making
You can base your visit level code on medical decision making, which is comprised of three elements:
-
Problems Addressed: The number of problems you addressed for the patient during the day of the encounter.
-
Items Reviewed: The tests, chart information, and other data you reviewed in relation to the problems addressed today.
-
Risk: The level of risk presented to the patient.
- 2021 Evaluation and Management Updates: What changed? This 15 minute video explains the new way of selecting E&M codes in context with how you coded sick office visits before.
- PCC’s 2021 E&M FAQ&A: Frequently asked questions, and a live Q&A about 2021 E&M leveling.
- 2021 E&M Workshop: A live workshop led by PCC, this session includes an overview of the changes and examples of real-world level selection.
- The Impact of 2021 E&M Coding Changes on Pediatrics: Learn about the E&M coding changes in context, and then hear PCC’s ideas about how these changes will affect the business of pediatrics.
- Pediatric Management Institute’s September COVID-19 Webinar: During the September 2020 session of the PMI’s ongoing webinar series, The Business Impact Of COVID19 On Pediatric Practices, this topic is covered along with other current topics. This recorded live webinar includes some additional Q&A.
- PCC Resources
-
Evaluate Your Practice's E&M Habits and Patterns: Your Practice Vitals Dashboard, available from within PCC EHR, provides a number of metrics, tools and recommendations related to E&M coding included on the “E&M Coding Distribution” measure.
-
Confessions of a Pediatric Practice Management Consultant: PCC’s Chip Hart runs a blog and podcast, covering many topics related to practice management, including E&M coding. You can find it here.
-
- Other Resources
- AAP FAQ: E&M 2021 coding questions and answers by the American Academy of Pediatrics.
- AAP MDM Grid: A direct link to the AAP’s chart which illustrates levels of medical decision making. It includes several useful examples. (AAP hosts this file here.)
- MDM Tracker: An online tool for selecting visit level based on medical decision making in 2021.
-
Where can I find PCC’s 2021 MDM Tool?Here it is: PCC’s 2021 E&M Coding Tool.
-
Where can I find the online MDM calculator Chip Hart shared?You can find it on the Confessions of a Pediatric Practice Management Consultant blog post entitled “Free E&M Medical Decision Making Calculator”.
-
Is fever a systemic symptom which can elevate a visit’s level?Sometimes. It depends on the patient’s presentation, and only when paired with an acute illness.
CPT defines systemic symptoms this way:
“Acute illness with systemic symptoms: An illness that causes systemic symptoms and has a high risk of morbidity without treatment. For systemic general symptoms, such as fever, body aches, or fatigue in a minor illness that may be treated to alleviate symptoms, shorten the course of illness, or to prevent complications, see the definitions for self-limited or minor problem or acute, uncomplicated illness or injury. Systemic symptoms may not be general but may be single system. Examples may include pyelonephritis, pneumonitis, or colitis.” (p12-14 2021 CPT Manual)Fever had become a mainstay of complexity expression in E&M documentation. In 2021, not all fevers meet the definition of a systemic symptom. AMA says that in cases where the fever is a “general symptom in a minor illness”, it is *not* systemic. So using it to express visit complexity becomes a case-by-case determination for 2021. Things like age and other risks will be determining factors that clinicians will have to consider when they decide this point.
-
Can we get points for both ordering and reviewing tests and labs in our MDM leveling?No. For any one test or lab, you may include *either* the ordering or reviewing done on the service date. To include both points would be “double dipping”.
Furthermore, the AAP has interpreted the AMA’s position to be that you may not consider tests performed in your office in your MDM level determination. This interpretation is under review.
-
Will documenting multiple diagnoses lead to a higher level of MDM?
Maybe. “Problems” are the units of determination for MDM. So, if you treat three problems in a visit, but there are five ICDs listed, the ICDs do not inherently support higher complexity leveling. Some ICDs are reported because they represent circumstances and/or problems which complicate care but which are not specifically addressed at that visit. Documenting the role that those existing problems play in your thinking could support assigning higher Problem values to what *is* addressed.
-
Can I really get credit every time a parent or guardian contributes history to a visit?Maybe. If you feel confident that the contribution they made is required for appropriate care to be rendered, yes. Document the reason for their perspective being necessary if it is not obvious. For example, little ones who can’t speak for themselves obviously require someone to give their history. But for teens, the necessity of another perspective in, say, behavioral or social concerns where objective input is valuable, document a statement to that effect and take the independent historian point(s).
-
If I spend time reviewing records from a different practice, even if they’re from a practice where I formerly practiced medicine, can I count that time toward my day’s total?Technically, I would say yes. If the patient is familiar to you, the review would likely not take very long, necessarily.
Follow Up Question: What if I am reviewing records at my practice that are “old”, say, greater than 3 yrs?
Answer: No, not the way requirements are currently written: “Review of prior external note(s) from each unique source.” Only records from sources outside your own organization can be considered external and valid for those points. -
How do Social Determinants of Health (SDoH) count toward MDM?Per CPT 2021, SDoHs are “Economic and social conditions that influence the health of people and communities. Examples may include food or housing insecurity.”
Per the Elements of Medical Decision Making grid published by AMA in CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes, an example of Moderate risk of morbidity from additional diagnostic testing or treatment is “Diagnosis or treatment significantly limited by social determinants of health”. I interpret these references to suggest that any SDoH which significantly limits the patient’s ability to carry out the clinician’s plan meets the Level 4 risk requirement.
According to the U.S. Department of Health, Social Determinants of Health are economic and social conditions that influence the health of people and communities. Their examples include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
Some of these may be reported using ICD codes found in “Persons with potential health hazards related to socioeconomic and psychosocial circumstances Z55-Z65”
- Z55 Problems related to education and literacy
- Z56 Problems related to employment and unemployment
- Z57 Occupational exposure to risk factors
- Z59 Problems related to housing and economic circumstances
- Z60 Problems related to social environment
- Z62 Problems related to upbringing
- Z63 Other problems related to primary support group, including family circumstances
- Z64 Problems related to certain psychosocial circumstances
- Z65 Problems related to other psychosocial circumstances
-
How will billing sick care that was rendered during a well visit be affected by the 2021 E&M changes?As a physical exam is not a consideration in leveling 2021 E&M visits, clinicians can now capture sick care for New Patient well visits, and can more easily level any visit that includes both sick and well care.
The new MDM focus on visit leveling represents less subjectivity in discerning which parts of a service were part of the well care and which were part of the sick care.
-
Do I need to document in the note the exact amount of time spent on each activity, or is it ok to just document total time?Full day totals are permissible, but I would feel better seeing at least time segments. Rough estimates for segments would do, but to expect that human brains can recreate a day’s worth of timed detail accurately for work that gets interrupted and broken up and then wrapped up after everyone else has gone home is a stretch which can be avoided.
-
Is there still a Level 1 visit for nurse-only visits?Yes, for established patients only, a Level 1 nurse visit can be reported using 99211. New patient level 1 code 99201 expires on 12/31/20 and is not reportable thereafter. This is due to the identical MDM requirements for both 99201 and 99202. By 2021 standards, 99201 becomes redundant to 99202.
-
If I continue to chart after hours, can I add that time for the purposes of leveling the visit?Yes. Caveat: The only after hours charting time (or any other clinical activity time) you may include in your billed time is the time spent *on the date of service*. If you chart any part of yesterday’s visit today, you may bill by time but you cannot include the time you spent today in the total you use for choosing your level. For example, if on Monday you see an established patient and spend 5 minutes reviewing records, 10 minutes in a visit, 5 minutes on a results call Monday night and 10 minutes charting on Tuesday morning, you may only bill a level 3 visit using Monday time: 5+10+5=20 minutes; Tuesday’s 10 minutes cannot count toward the leveling.
-
Will I get MDM data points for tests like rapid flu or rapid strep for which I also charge?Currently, no. The current interpretation of the relationship between awarding data points for tests and labs and paying for tests and labs is that they are mutually exclusive.
Discussions around this continue, but currently you should not expect to level using data points for test and labs you bill.
-
Are a CBC and differential counted as more than 1 lab? Or for example COVID-19/Flu/RSV combo - is that 1 test or 4 tests?It depends on the number of CPTs. If CBC and differential are one CPT, it is one data point for either ordering or reviewing. If the COVID-19/Flu/RSV combo is one CPT, one point is its data value.
-
Could I count one of several screenings towards data reviewed and bill for the other and not be double-dipping?This is not in the spirit of the requirement, but is still under discussion. Billing effects are impossible to explore here. The sheer variety of payers and policies means the outcome can not be predicted. Furthermore, carrier behavior makes predictions of future claim determinations little more than a guessing game.
-
Do I get credit if some historians are in office and others participate over facetime, phone, etc., for the same visit?Yes. There is no cumulative credit for historians, but if someone other than the patient is required to participate that requirement is met.
-
If you use a formal screen for SDoH that is scored and payable, then you can’t count that screening towards MDM, correct?Currently, that is correct.
-
Does pulse oximetry give a data point?I don’t know, and this question is more complex than it looks. The debate between clinicians about whether pulse ox is a vital sign is a factor. If you consider it a vital, it is not a test, and counting it as a data point is questionable. However, pulse ox has a billable CPT, so some may consider it a test.
Also, the question of whether in-house tests and labs may be used for data credit remains unanswered. I am undecided on this as yet and will count on the clinicians with whom I review encounters to help me arrive at a position on this point in future.
-
We do our huddle and "run the schedule" (i.e. review referrals, lab results, vaccines, and consult notes) the day *before*, not the day of! Can we count that time when leveling each of those encounters?No. Currently, the only “billable” time is that spent by the clinician for that patient on the service date.
-
Does 'undiagnosed new problem with uncertain prognosis' relate to when we don’t yet have a diagnosis, or does it mean a new previously undiagnosed problem that you identified at the visit?This phrase comes from a MDM requirement. Our interpretation is that it means a new problem for the patient that you have never seen before, and for which you are uncertain of the outcome.
CPT 2021 is light on guidance on this point. “Undiagnosed new problem with uncertain prognosis: A problem in the differential diagnosis that represents a condition likely to result in a high risk of morbidity without treatment. An example may be a lump in the breast…” The AAP offered an additional example of a potentially malignant lesion in the Feb 2020 issue of the Coding Newsletter.
-
If we bill for one Vanderbilt, could we then claim MDM credit for the ones from other sources?My sense of this is that doing so is *not* in the spirit of the guideline. Additionally, performing a service and not billing for it will run afoul of many insurance contracts. Also, please see above for information about Data credit for in-house labs and tests.
-
What about the hand-on-the-doorknob minor things that parents like to bring up? If there are enough of these, or significant ones, can I document them in a manner that might bump MDM up a level?
Example: Rash (insect bite) + been a little constipated (give some prune juice), been having stomach aches (few questions to make sure it’s nothing worrisome, asked to schedule another visit to evaluate further)…
Yes, but MDM is based on significance, not the number of problems. The total number of problems does not necessarily increase the credit you can claim for complexity in the Number and Complexity of Problems Addressed element. Rather, the most complex problem addressed (Minimal, Low, Moderate, High) in a given encounter typically represents the level of “problems addressed” which should be used for leveling. Exceptions include self-limited, minor problems (1 = Minimal while 2 = Low) and stable chronic illnesses (1 = Low, 2 = Moderate).
-
Can concussion be considered an acute complicated injury - a head injury that gave other systemic symptoms?Described that way, absolutely. Be sure to familiarize yourself with the AMA’s definition of Systemic Symptoms.
-
What is meant by 'risk'? The guideline only lists examples. Is there a way to determine risk on MDM without these examples? Is that purely a judgment call?Yes, this is a clinical judgment.
From the AMA: “Trained clinicians apply common language usage meanings to terms such as high, medium, low, or minimal risk and do not require quantification for these definitions (though quantification may be provided when evidence-based medicine has established probabilities). For the purposes of MDM, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes MDM related to the need to initiate or forego further testing, treatment, and/or hospitalization.”
-
If you send a kid to the Emergency Department, or for testing due to concern for appendectomy, does that discussion get you to a higher level of risk? Does discussion of a possible ER visit count?Not usually. If the decision is purely for testing consideration, meaning the tests could be done in another care setting without ready access to acute or surgical or inpatient care, I would *not* say that meets the spirit of the requirement.
From the AMA: “… decision about hospitalization includes consideration of alternative levels of care…Examples may include a psychiatric patient with a sufficient degree of support in the outpatient setting or the decision to not hospitalize a patient with advanced dementia with an acute condition that would generally warrant inpatient care, but for whom the goal is palliative treatment.”
-
Will PCC develop a software timer to capture clinician charting time?PCC is not currently developing a timer in PCC EHR. Our research mid-2020 about this feature found that users did not see enough value in having to activate a timer whenever they turned their attention to a particular chart.
For example, if PCC EHR automatically records your time with a chart open, you would be required to close and reopen every chart every time you were interrupted while charting in order for it to be accurate. If you had to actively click a button to stop and start a timer, it would be an ever-present timer that required their attention. Users shared this would be distracting at best and annoying at worst. Most users were happier to state their own estimates of how much time was spent, either in total or in segments to be used for totaling when they were sure services were complete for the whole day.
Select a Code Based on Time
You can base your visit level code selection on the total time that the rendering clinician spent on the patient that day. That can include the time the pediatrician spent before, during, and after the actual encounter.
Watch PCC 2021 E&M Coding Videos
These 2021 videos provide examples of how to level your E&M visits:
Configure PCC EHR to Support Your Clinicians and Billers for E&M Level Selection in 2021
Your practice can add fields to your chart note protocols in order to track time spent before, during, and after the encounter by the clinician. You can also track the number of problems addressed, items reviewed for the problems, and the level of risk present.
As an example, this sample chart note protocol includes components designed to quickly note problems, time and risk.
For help customizing your protocols, check out Configure Chart Note Protocols, and get in touch with PCC Support for assistance.
2021 Additional Resources and Guides
In the lead up to the 2021 transition, PCC published blog posts and other organizations published guides and online tools.
2021 Questions and Answers on Interpreting E&M Guidelines
PCC’s Jan Blanchard works with pediatric practices to help them interpret coding guidelines. Read below to see a selection of the 2021 E&M questions received at the time of the transition. These Q&As were last updated on 2021-01-08, so you should consult your AMA CPT Guide for more recent details.
Questions and Answers
PCC 8.14 Release
In the fourth quarter of 2020, PCC will release version 8.14 of our electronic charting and practice management software to all PCC users.
PCC 8.14 focuses on quickly delivering improvements clients asked for and may need immediately. PCC updated SNOMED-CT, ICD-10, and LOINC code sets to the most recently published standard, which includes COVID-19 terms and codes for billing. PCC 8.14 also introduces new chart features for sexual orientation and gender identity and the next phase of our CHADIS integration, allowing families to open questionnaires from inside the patient portal.
Watch a Video Series: Want to see videos about the updates in this release? Watch the PCC 8.14 Release Video Series.
Read below to learn more, and contact PCC Support for information about these new features or about any PCC product or service.
Send Broadcast Messages for Overdue Immunizations and Much, Much More
You can now send broadcast messages from the PCC EHR Report Library to recall patients who are behind on their vaccines.
Open the Report Library and generate the Overdue Vaccine Recall report.
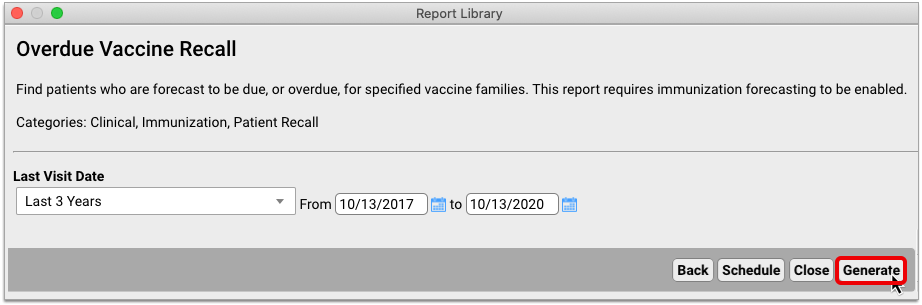
Once the report has generated, click “Export”.
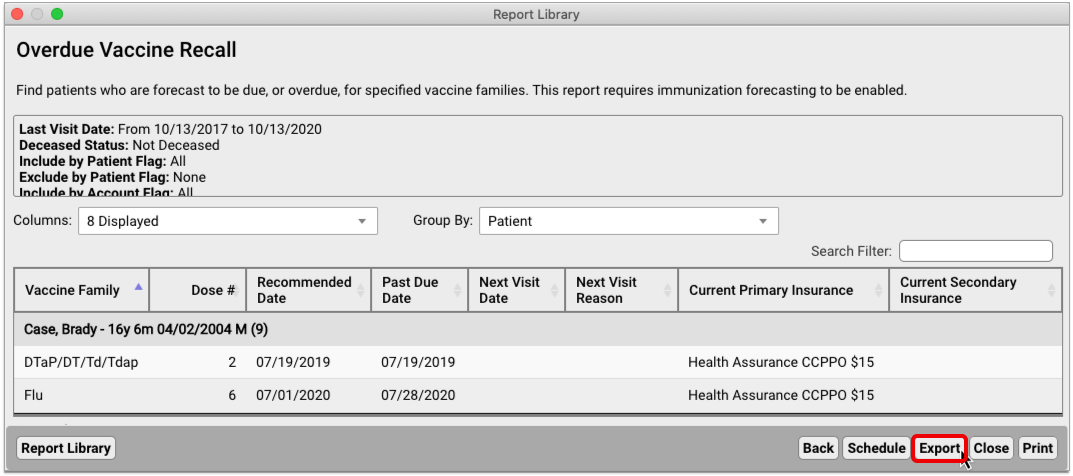
Select the “Send Message to Patients” option to start a broadcast message.
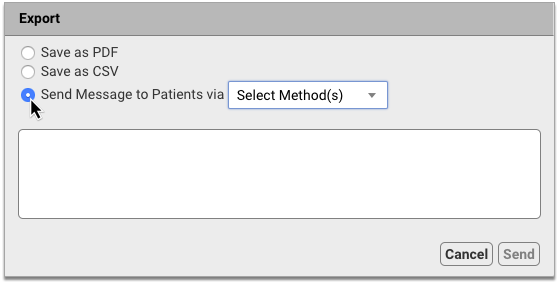
Decide whether to contact patients by text, email, or both. Then, compose your message and hit “Send”.
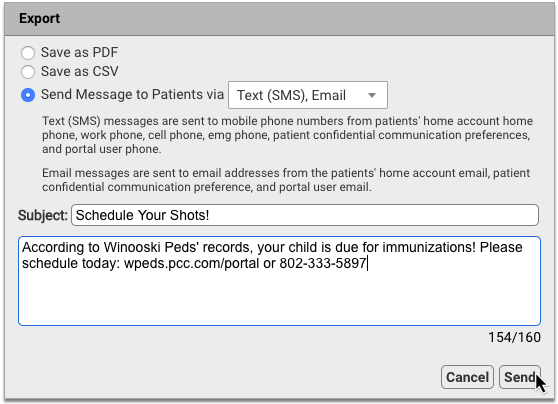
You can also use Broadcast Messaging with most other reports in the PCC EHR Report Library, including Appointment reports, Prescription reports, and Visit reports.
Now you can leverage reports to get in touch with patients in powerful and creative ways:
- Remind families without portal accounts to sign up at their next visit
- Send a message to all patients affected by a medication recall
- Offer tailored guidance to at-risk patients during a public health emergency
Contact PCC Support to explore how Broadcast Messaging can help you stay connected to your patients.
To learn more about how to create, send, and track broadcast messages, read Send Batch Messages to Patients and Families.
Record Sexual Orientation in a Patient’s Chart
When your practice charts a patient’s sexual orientation, you can record the patient’s information in the Sexual Orientation component.
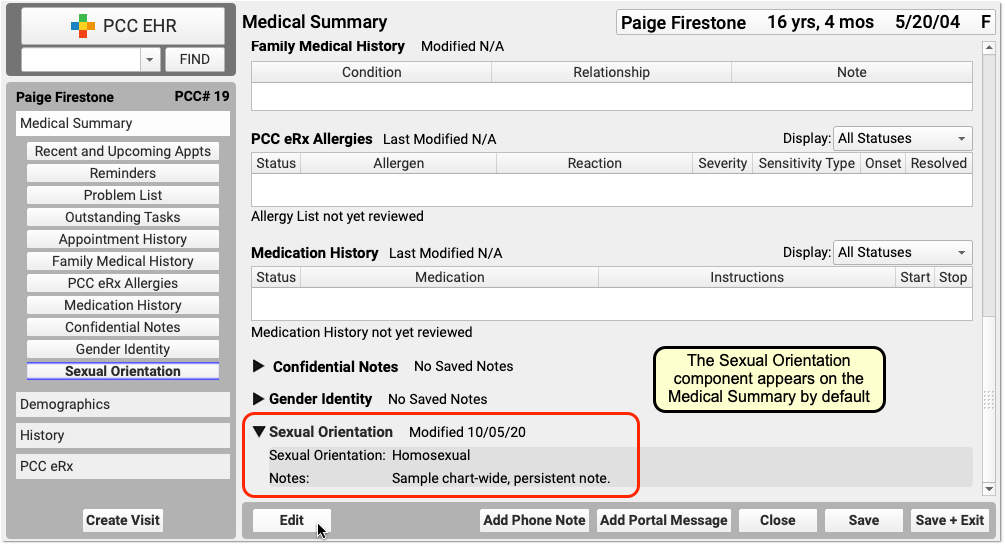
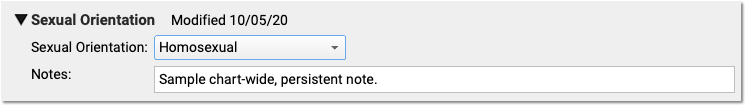
Your practice can add this chart-wide component to chart note protocols or anywhere you need it for your workflow.
Sexual Orientation is a Confidential Component: When you open a chart, the contents of this component are hidden. A clinician or other PCC EHR user must click the disclosure arrow to display the contents of the Sexual Orientation component. PCC EHR records that this information was accessed, and your practice can review who accessed the information in the PCC EHR Audit Log.
Record Gender Identity, Preferred Name, and Pronoun in the Patient’s Chart
Use the Gender Identity component to record a patient’s gender identity, preferred name, pronoun, and notes.
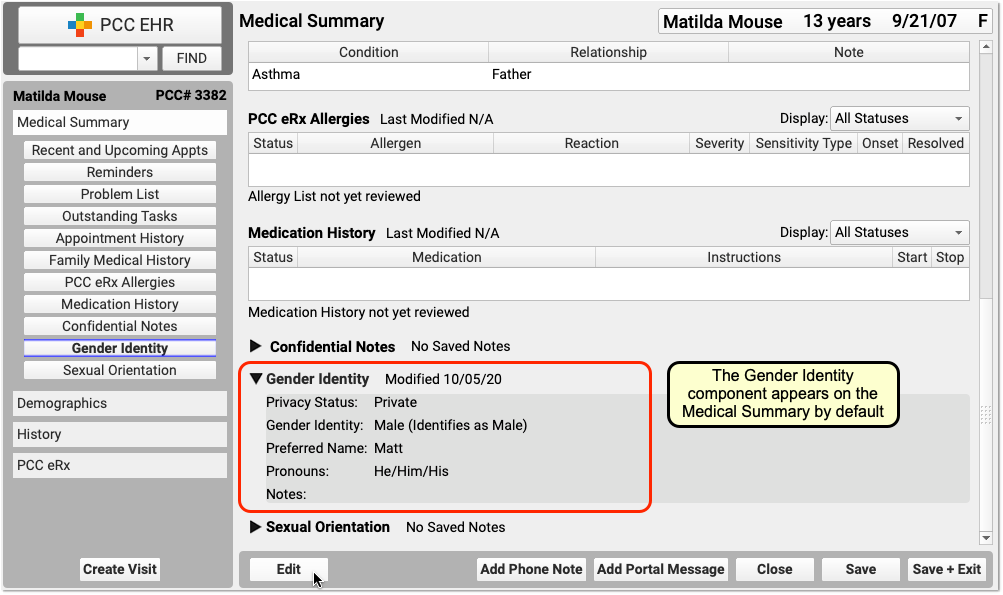
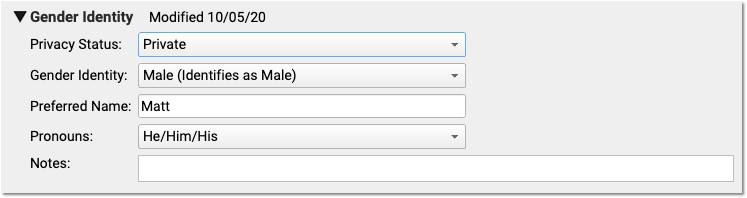
The component appears on the Medical Summary by default. Your practice can move it, remove it, and add this chart-wide component to chart note protocols or anywhere you need it for your workflow.
Patient information in this component is marked private by default. When private, the fields in the component are not visible anywhere in PCC EHR except in the Gender Identity component.
When the information is no longer private, select Public in the “Privacy Status” drop-down menu.
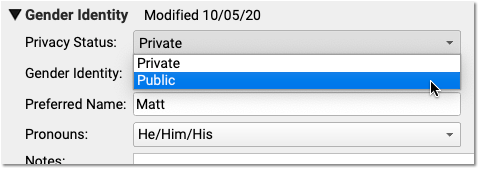
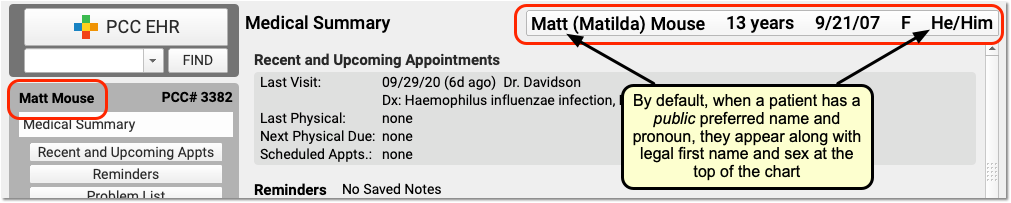
When Public is selected, PCC EHR and pocketPCC can display the patient’s preferred name and pronoun in the Patient Banner as well as in other places in PCC EHR.
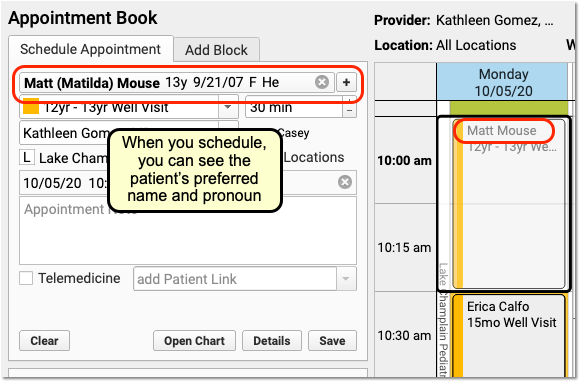
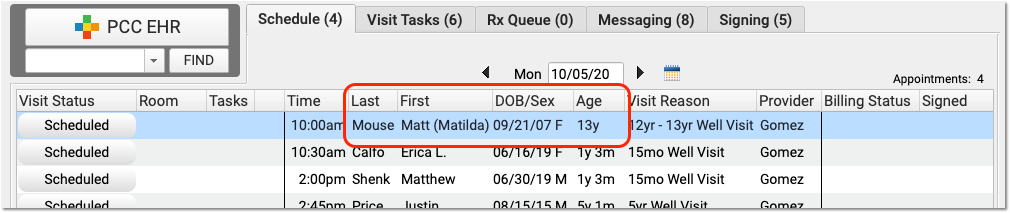
On the Appointment Book, for example, your staff will be able to see the patient’s preferred name and pronoun as they make an appointment. The preferred name can also appear on the Schedule screen and PCC EHR queues, except for the Rx Queue (which uses the patient’s legal name) and the E-lab Results queue (where a patient’s name is provided by a lab vendor). Your practice can find the patient by searching for either the preferred or legal name.
The patient’s preferred name can also appear at the top of forms and patient and family-facing reports that include the green name header. This includes the Patient Visit Summary:
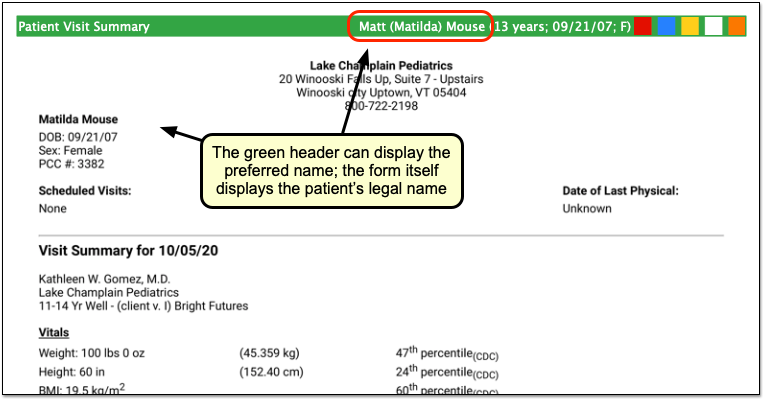
Note that the patient’s legal name and sex appear elsewhere on the form. Documents that can include the preferred name in the green header include: Care Plans, PDF versions of Continuity of Care Documents, Growth Charts, the Health Information Summary, Lab Order Details, the Patient Visit Summary, Summary of Care Record, and Visit and Billing History printouts.
Configure How Your Practice Displays Preferred Name and Pronoun: A patient’s preferred name and pronoun do not appear at all if their Gender Identity component is set to Private. Your practice can configure whether PCC EHR displays only a patient’s legal name, only the preferred name, or both the legal and preferred names when they are set to Public in a patient’s chart. You can also optionally turn off the preferred pronoun display. Open Practice Preferences to review your options.
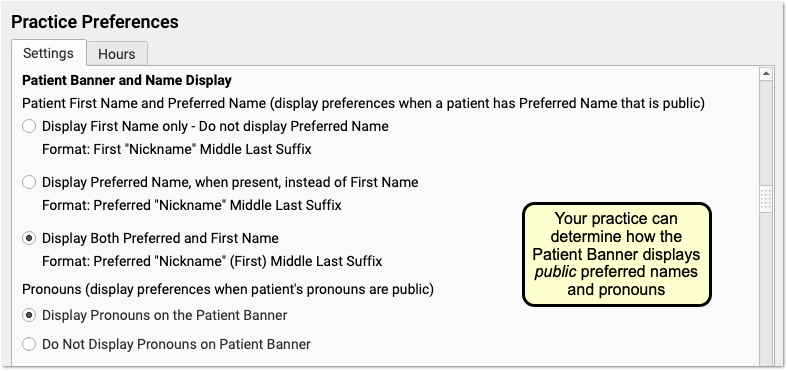
In addition to adjusting your practice’s display preferences, after your PCC 8.14 update your practice may wish to change the location of the component. You can also adjust your practice’s existing workflows for patients. For example, if you formerly used the Nickname field, a patient flag, or a Reminders note to indicate a preferred name or gender identity, you can decide how that usage will change.
Gender Identity is a Confidential Component: When you open a chart, the contents of this component are hidden. A clinician or other PCC EHR user must click the disclosure arrow to display the contents of the Gender Identity component. PCC EHR records whenever this information was accessed, and your practice can review who accessed the information in the PCC EHR Audit Log.
Track Relationship to Patient in Patient Portal
Track the relationship between your Patient Portal users and their patients, and avoid errors by knowing exactly who you’re communicating with.
PCC 8.14 adds a new column to the Patient Portal Administration’s Manage Portal User called “Portal User’s Relationship to Patient”. Each patient has a drop-down menu listing all relationship types – the same list that appears under Personal Contacts in PCC EHR. If the Patient Portal user also appears under the patient’s Personal Contacts in PCC EHR, setting the relationship in Patient Portal Administration will also update the relationship in Personal Contacts. 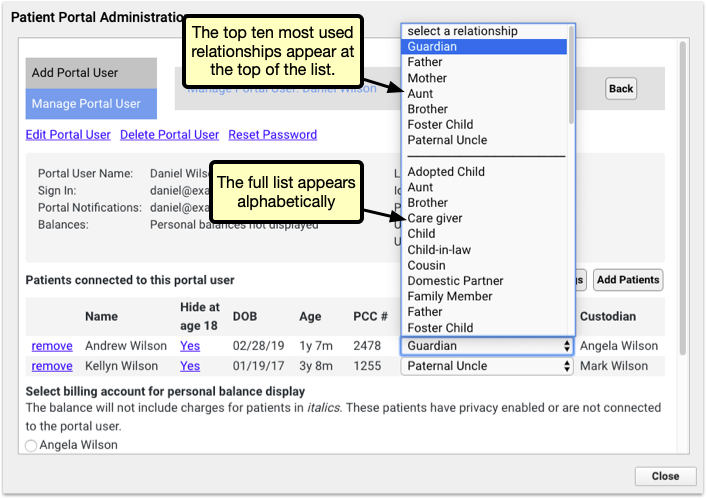
The top of the list shows the ten most frequently used relationships, so that you can quickly select common relationships.
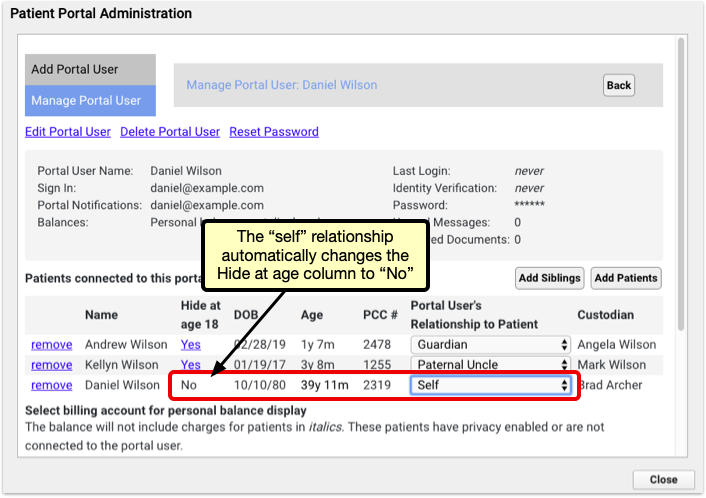
Selecting the “Self” relationship automatically changes the Hide at age of emancipation setting to “no” to avoid locking a user out of their own data.
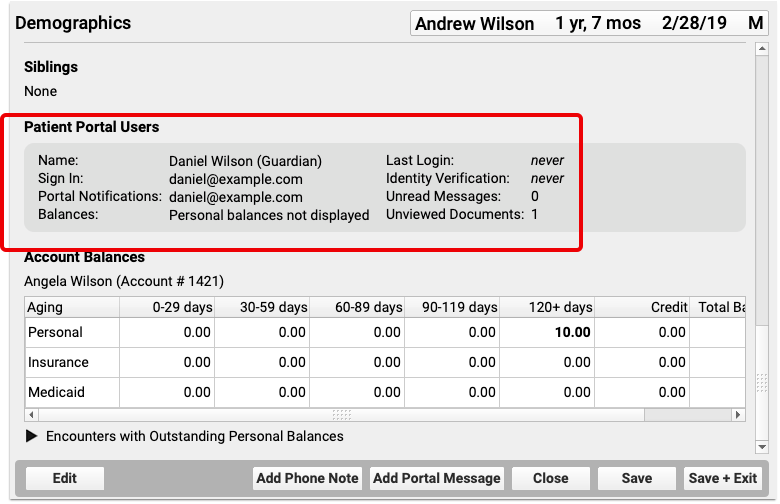
Once you’ve selected your relationship, it will appear in PCC EHR and pocketPCC under the Patient Portal Users component.
Track Vaccine NDC Codes Alongside Other Vaccine Lot Details
PCC EHR’s Vaccine Lot Manager now tracks NDC codes, alongside manufacturer, expiration date, lot number and other details.
Lot Manager Only: NDC codes in the Vaccine Lot Manager are not used for billing. NDC codes needed for billing should still be managed through the Procedures Table.
When scanning a new vaccine into the Vaccine Lot Manager, the NDC code will be added with the rest of the vaccine’s information.
When entering vaccines manually through the Add Lot window, NDC codes can be entered several ways. When adding a new lot, click the NDC drop-down menu to review a list of all active NDC codes. You can skim through the numerical list until you find the code you’re looking for, or begin typing the code to narrow the list to matching results. Selecting an NDC code will automatically enter the immunization name and the manufacturer.
Alternately, by entering an immunization name first, the NDC menu will automatically filter to NDC codes that match your selected immunization. Entering a manufacturer will filter further, to NDC codes that match your immunization and manufacturer.
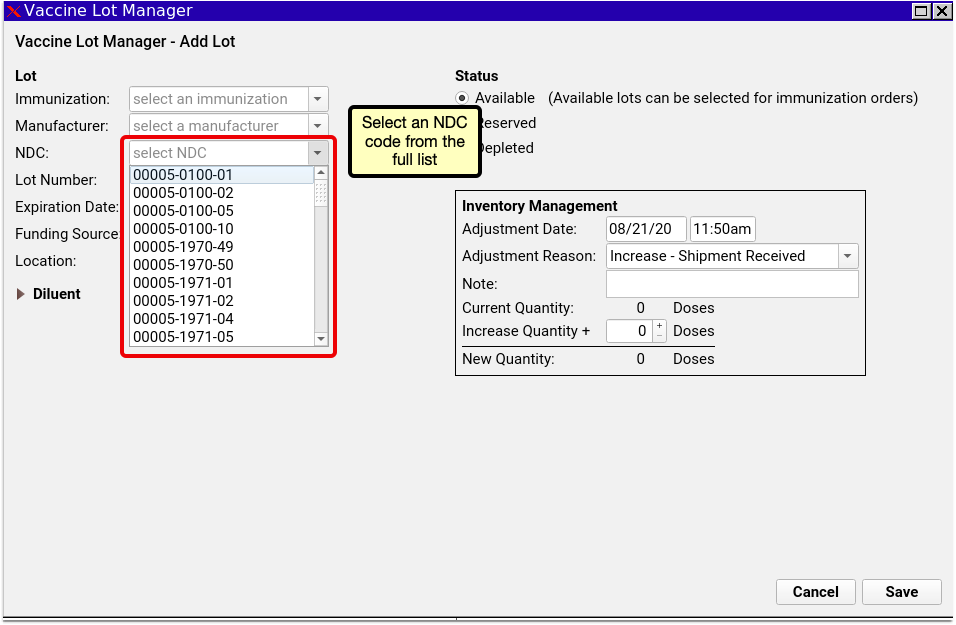
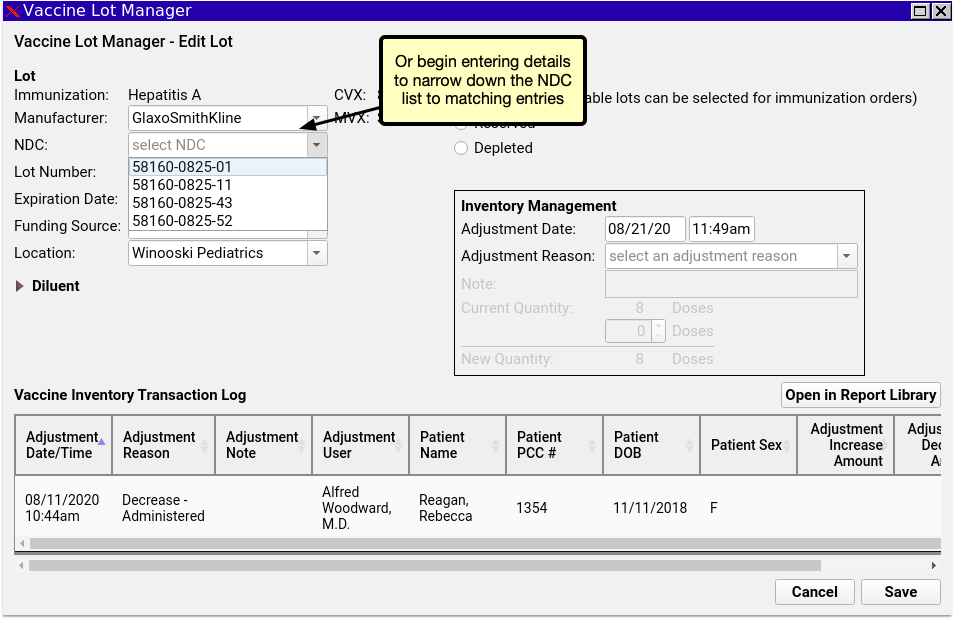
Access CHADIS Questionnaires Directly through the Patient Portal
PCC continues piloting the integration of CHADIS questionnaires into PCC EHR and PCC’s Patient Portal. If your practice is part of our pilot testing, your Patient Portal now links directly to CHADIS, so your portal users can get started on their patient’s CHADIS questionnaires when their appointment is booked.
Coming Soon: CHADIS integration into PCC is currently in pilot testing and not yet available to all PCC Clients. Stay tuned for additional functionality and the wide release.
CHADIS Required: CHADIS integration into PCC EHR requires that your practice has a CHADIS subscription.
Configure CHADIS in PCC EHR
You first need to connect your practice’s visit reasons to CHADIS visit types, so that your patients will receive the appropriate CHADIS questionnaires for their visit. Open the Visit Reason Editor and click on the CHADIS tab.
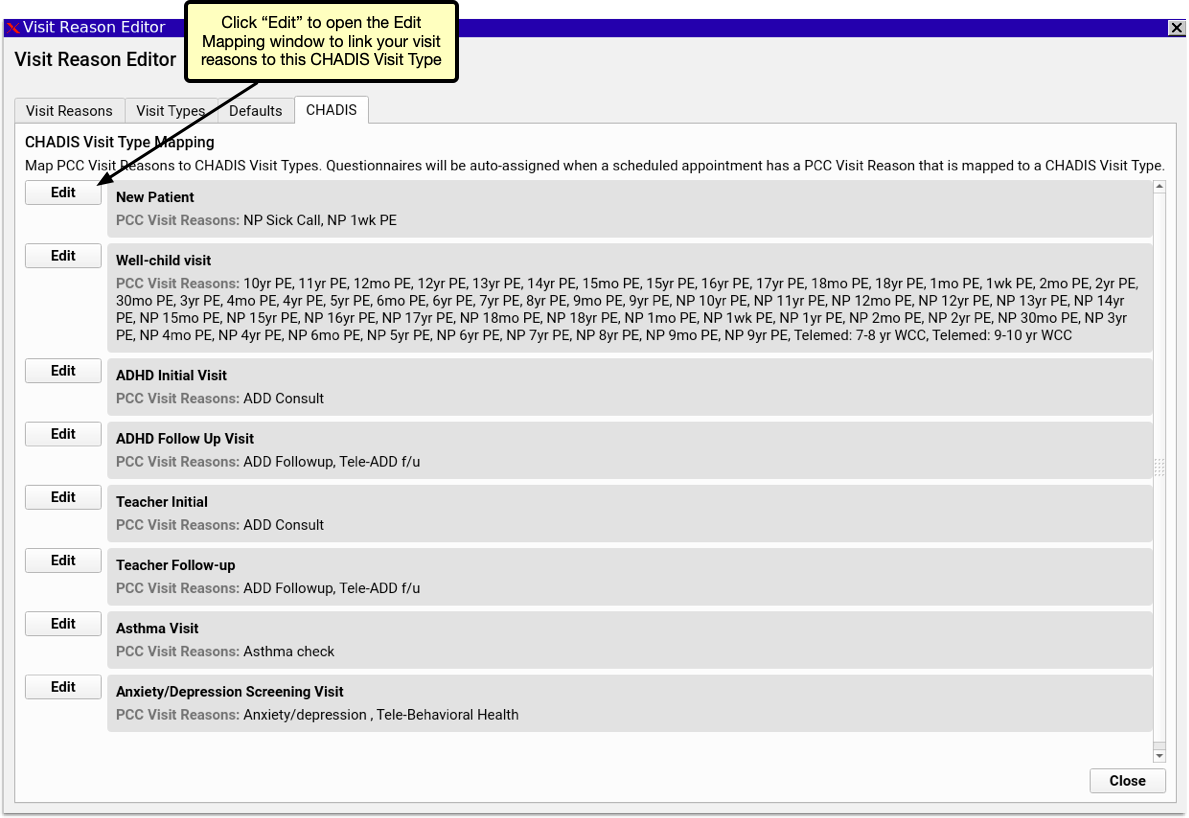
The CHADIS Visit Type Mapping includes a list of each CHADIS visit type and lists the PCC EHR visit reasons associated with each. Click the Edit button.
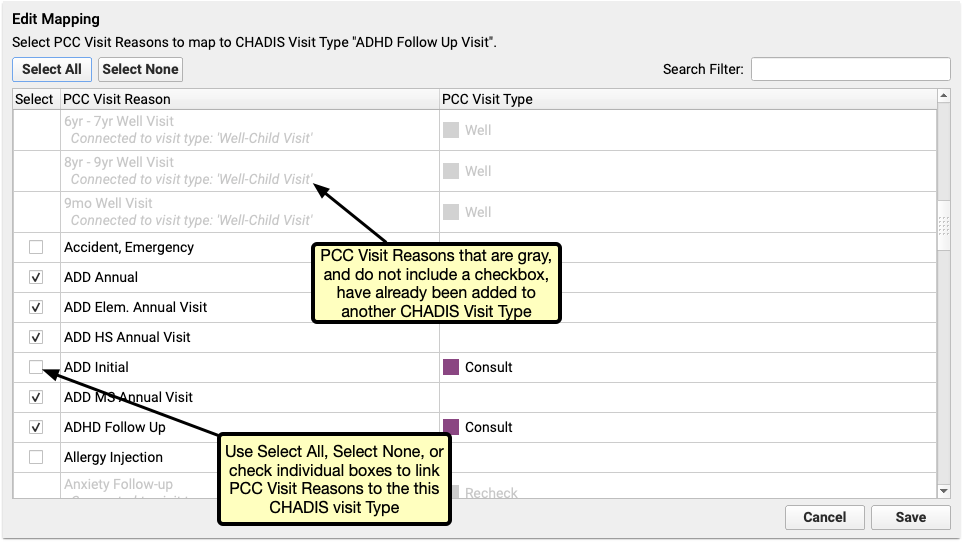
In the Edit Mapping window select which of your Visit Reasons should be assigned to the selected CHADIS Visit Type. Each visit reason can be assigned to multiple CHADIS types, and each CHADIS type can be assigned to any number of visit reasons.
Schedule Visits to Send CHADIS Questionnaires
Once your visit reasons are linked to Visit Types, simply begin scheduling visits. PCC automatically registers your patients with CHADIS and the matching CHADIS questionnaires for the scheduled visit type will be generated by CHADIS 7 days prior to the visit. If the visit is scheduled for less than 7 days in the future, the questinnaires will be made available the day of scheduling.
When a new questionnaire is ready, the patient’s portal user will receive a Patient Portal notification that a questionnaire is waiting for them. When they log into the Patient Portal, they’ll find an orange button inviting them to start their questionnaires. Clicking the orange button opens the questionnaire on CHADIS’s website in a new browser window. If no visit is scheduled or no CHADIS questionnaires are pending, users can access CHADIS from the Patient Portal by clicking the CHADIS Home button.
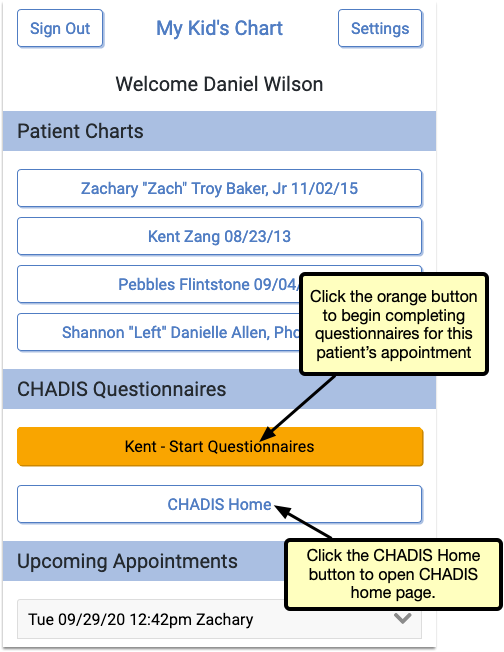
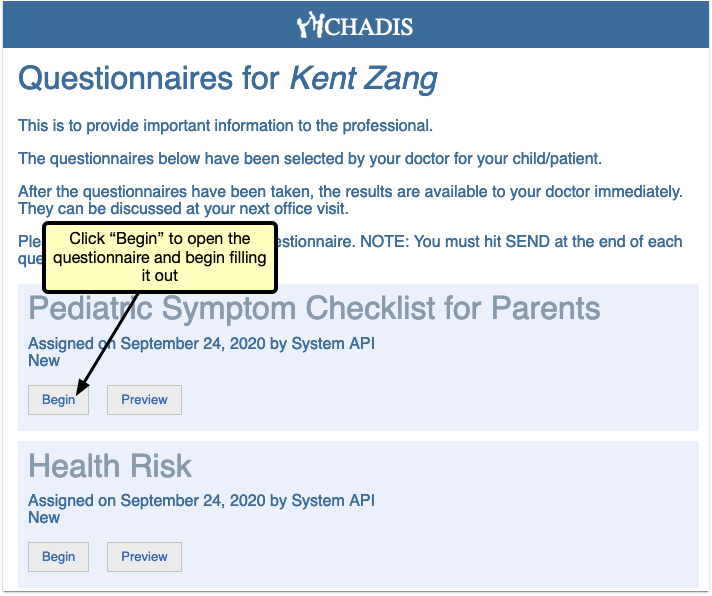
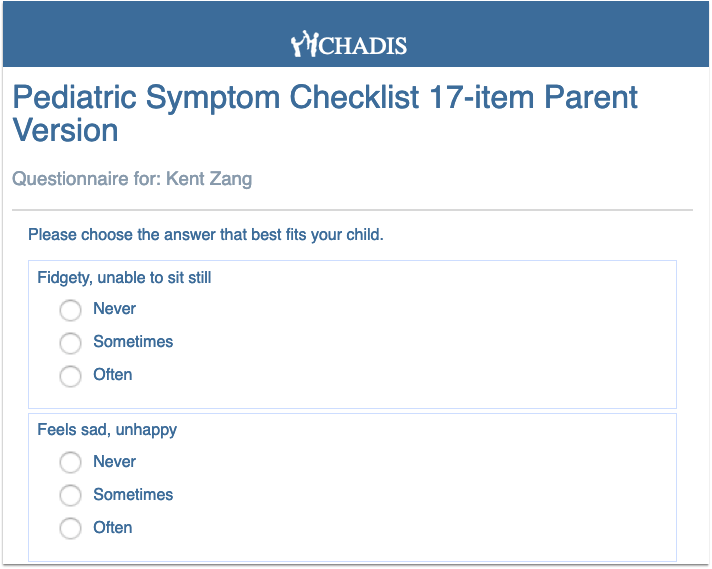
Upcoming PCC updates include importing CHADIS results directly into PCC EHR, where they can be linked directly to a patient and visit.
Improvements to the Practice Vitals Dashboard
PCC 8.14 improves your Practice Vitals Dashboard, making it a more valuable tool for insight to your practice’s clinical and financial trends.
-
The COVID-19 Dashboard Page Now Loads Faster: Under-the-hood improvements to your COVID-19 Dashboard page now allow you to load the same great data in less time. The COVID-19 Dashboard page is designed to help you measure and respond to the impact of COVID-19 on your business. To learn more about this tool, read Analyze and Respond to COVID-19’s Impact in Your Dashboard.
-
Corrections to Adolescent Immunization Rate Benchmarks: More accurate PCC Average and Top 10% benchmark calculations reveal how your adolescent immunization rates for HPV, Meningococcal, and TdaP compare to other PCC clients and top performers.
-
Corrections to Reporting of Sick Visit Modality: The COVID-19 Dashboard page allows you to view trends in how you deliver sick care to patients. Sick visits conducted over the phone or through the patient portal were being reported incorrectly prior to 8.14, and have now been corrected to give you a more accurate view of how patients are receiving sick care at your practice.
Use 2021 ICD-10 Diagnosis Billing Codes, Including New COVID-Related Codes
On September 20th of 2020, PCC updated your practice with 2021 ICD-10 diagnosis billing codes.
The 2021 ICD-10 update includes new sections for COVID-19-related infections and vaping-related disorders. You can review the complete, updated guidelines in the CDC’s ICD-10-CM Official Guidelines for Coding and Reporting.
The new codes and guidelines take effect for dates of service starting on 10/1/2020. You can learn about the updates that are of most interest to pediatric practices by attending PCC Web labs held by Jan Blanchard (CPC, CPEDC). Missed a web lab? You can watch a recorded session as well.
In addition to COVID-19 and vaping-related guidelines and codes, Jan notes that the 2021 ICD-10 update includes more specificity for substance abuse codes, several adjustments to influenza coding, and new codes for reflux, headaches/face pain, and more. In the “curiosities” bucket, the update includes “Pedestrian on electric scooter and standing micro-mobility pedestrian conveyance (hoverboard, segway)” added to V00-V06.
Chart Diagnoses Mapped to Deprecated ICD-10 Billing Codes: Were there any 2021 code changes for items that your practice frequently bills? You can review your system configuration using the snomedmap report tool in Partner. While there were no major disruptions in the 2021 ICD-10 update, it’s always worth taking a look at your code mapping reports to head off any billing challenges.
For more details, read Fall 2020 SNOMED-CT and ICD-10 Updates Add COVID-19-Related Issues and Other Diagnoses.
Use the Latest SNOMED Diagnoses, Including New COVID-Related Descriptions
On September 20th of 2020, PCC updated the SNOMED-CT diagnostic terms on your practice’s system.
The SNOMED-CT update includes thousands of new descriptions for diagnoses, allergies, therapies, and procedures. It also updates thousands of text descriptions for diagnoses and their mapped ICD-10 billing codes. You can review information about the update on the National Library of Medicine web site.
Review Your COVID-19 SNOMED to ICD-10 Mapping: As codesets continue to change in response to COVID-19, PCC recommends you review the diagnoses you use to chart and bill for COVID-19 issues. For example, this update includes a new recommended mapping of the Exposure to SARS-CoV-2 SNOMED description to the Z20.828 ICD-10 code. This mapping was not included by default in the previous SNOMED standard. You can double-check your practice’s diagnosis billing configuration in the Billing Configuration tool.
For more details, read Fall 2020 SNOMED-CT and ICD-10 Updates Add COVID-19-Related Issues and Other Diagnoses.
Use New COVID-19 Test Descriptions With the LOINC 2.68 Update
On August 31st of 2020, PCC patched all practice systems with LOINC 2.68, an update to the standard list of labs used to make tests interoperable between different systems.
PCC reviewed the updates to LOINC before the update: there will not be any disruption to labs your practice currently orders, and you shouldn’t need to take any action to see the effects of the patch.
The update includes over a thousand new terms and updates, including specific LOINC descriptions for SARS-CoV-2 laboratory tests. The update also adds terms for COVID-19 case reporting and related issues.
If your pediatric practice is performing COVID-19 tests, you’ll be able to configure your labs for appropriate tests in the Lab Configuration tool. This includes the new 95209-3 SARS-CoV+SARS-CoV-2 Ag code, among others.
For details on how to add a COVID-19 test or other lab order to your system, you can read Create a COVID-19 Test Lab Order and Lab Configuration.
Continued Pilot Test: Securely Retrieve Patient Information from Hospitals and Other Practices
Do your patients see other doctors? Do you wish you could retrieve records from those providers on demand?
Pilot testers can request and securely retrieve their patients’ records from other healthcare organizations right within PCC EHR. This is the latest addition to PCC’s Clinical Document Exchange functionality.
To retrieve a document, click “Find Clinical Documents” within the History section of the patient’s chart.
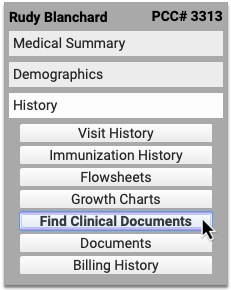
Select one or several healthcare organizations to query, then search for your patient within their records. If you find matches for your patient, you can then see if the organizations have clinical documents to share, and retrieve any you wish to view and save to PCC EHR.
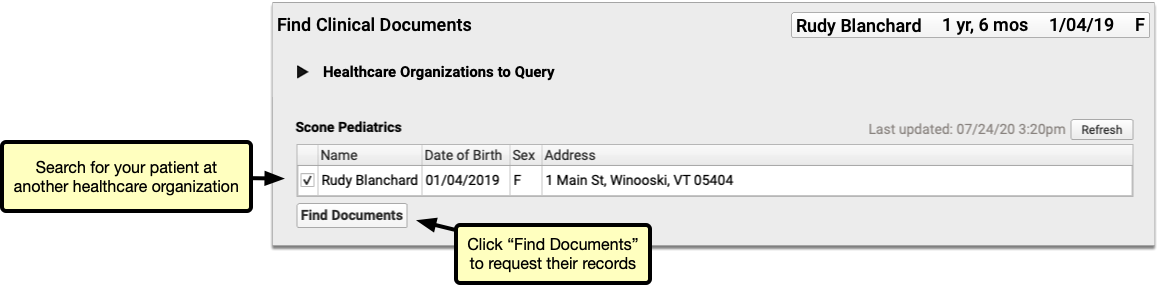
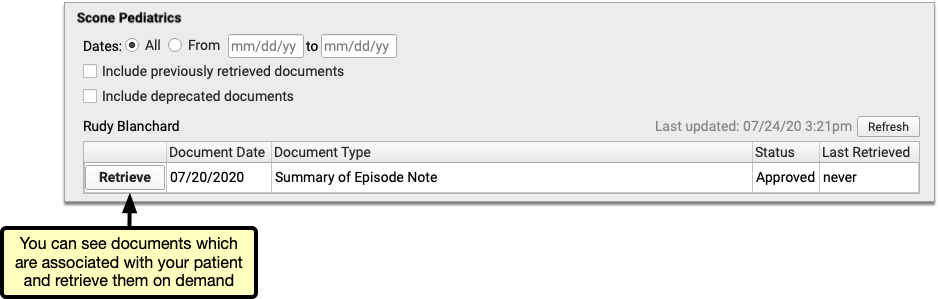
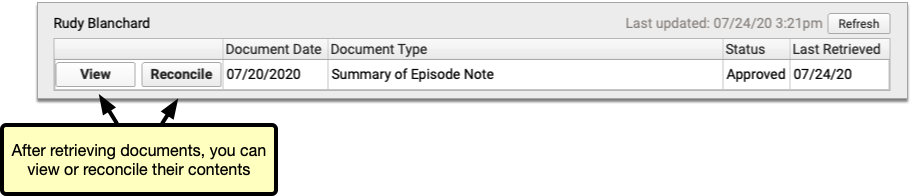
You can set up default healthcare organizations to query for each of your patients, and also decide if certain organizations (such as local hospitals or urgent care clinics) should be queried for all patients.
Users need special permissions in PCC EHR in order to request patient records from other organizations. All PCC EHR users can view retrieved documents after they have been saved in patients’ charts.
How do I Participate?
Although it is not yet possible to sign up to securely retrieve your patients’ records from other healthcare providers, you can prepare for the feature by becoming a Clinical Document Exchange Responder.
Clinical Document Exchange Responders allow other healthcare organizations who participate in the Carequality interoperability framework to retrieve their patients’ records for treatment purposes. In order to eventually be able to initiate records requests, you must first enroll to respond to requests from others.
To become a Clinical Document Exchange Responder, contact PCC Support.
Learn About Clinical Document Exchange
Is Clinical Document Exchange secure? How does it work? Which organizations can I query for my patients’ records? Find answers to all of these questions and more in the PCC Learn article about Clinical Document Exchange.
New and Updated Interfaces Available in PCC 8.14
With each release, PCC’s Interoperability team expands and updates PCC’s direct connections, partnerships, and integrations with insurance payers, immunization registries, and more. Here are the clinical and financial interoperability updates for PCC 8.14:
-
New and Updated Immunization Interfaces: During the PCC 8.14 release cycle, PCC updated our immunization registry interfaces with SCIR (South Carolina), TennIIS (Tennessee), and ORALERT (Oregon).
-
Updated Clinical Interfaces in PCC EHR: PCC added or updated clinical interfaces with Huntsville Hospital, WellCentive, Epic, Wyoming Department of Health, and Affinia.
-
New Insurance Eligibility and Financial Interfaces: PCC also added or improved interfaces with Wyoming BCBS and Boston Medical Center Healthnet.
If your practice would like to take advantage of these connections, or you have another interface need, contact PCC Support.
Immunization Forecasting is Up to Date
During the PCC 8.14 release cycle, PCC updated your immunization forecasting schedules to meet the latest CDC ACIP schedules and to correct unusual schedule scenarios or errors in forecasting.
PCC EHR automatically reviews each patient’s immunization record and provides a table showing any immunizations that were missed, are recommended soon, or that occurred outside of the CDC’s ACIP schedule.
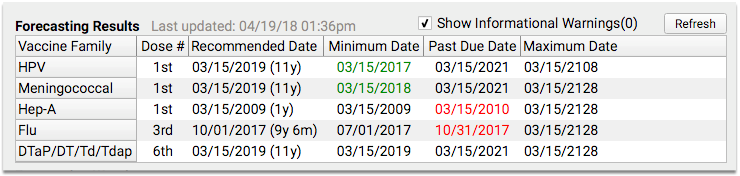
PCC uses immunization logic and calculation services provided by Immucast by STC. During the PCC 8.14 release cycle, STC applied their latest patch (5.24.0), updating and correcting immunization schedules and bringing your system’s Immunization Forecasting in line with the latest ACIP recommendations.
Here’s a summary of the most notable improvements:
-
Influenza: This update adds new influenza CVX codes to the forecaster. Also, under certain circumstances, when a child turned 9 during a flu season, the second dose of an influenza vaccine was marked invalid. This no longer occurs. Finally, when a patient received one dose, and then received a two dose series the following season, the second dose can now be marked as valid.
-
Meningococcal: This update adds new meningococcal CVX codes to the forecaster.
PCC tests all adjustments to the immunization schedules. Please get in touch if you’d like to learn more about the updates, or if you observe a forecasting result or warning that doesn’t match your expectation. You can review the full list of updates by reading the STC ImmuCast 5.24.0 release notes.
To learn more, read the guide to PCC’s Immunization Forecasting features.
Other Feature Improvements and Bug Fixes in PCC 8.14
In addition to the features described above, PCC 8.14 includes these smaller improvements and squashed bugs.
-
Scheduled Reports Update in September: Due to last minute challenges found in beta, PCC delayed the release of the new Schedule Reports feature in PCC 8.13. We updated all systems with this new functionality on 9/2/2020. You can learn more about it by reading the documentation or watching a quick tutorial video.
-
Find Next Available Appointments More Quickly: During the PCC 8.14 release cycle, PCC corrected a problem that caused the Availability Finder in the Appointment Book to take twice as long as it should. This fix was distributed on 9/2/2020.
-
Better Reporting of Immunizations Not Administered on Summary of Care Documents (C-CDAs): In Release 8.14, PCC EHR more accurately reports immunizations which were ordered but not administered on Summary of Care documents (C-CDAs). Practices in Washington State will notice immediate improvement in the way these immunizations are reported to Wellcentive. To learn more about how Summary of Care records can help you exchange patient information with other healthcare providers, read about how to Send and Receive Direct Secure Messages.
-
See Account Number in Open Payments Report: When you track down unlinked payments on accounts with Practice Management’s
openpmtsreport, you can now see the billing family’s PCC#, which makes it easier to identify the account. -
Retire Old Immunizations On Your PCC System: When you need to remove an immunization from available options in PCC, you can now adjust an “Orderable in PCC EHR?” option in the Practice Management’s immunization and disease configuration table. PCC Support makes this adjustment for most clients. This option will not disrupt charted orders or patient records, and it will prevent your practice from selecting the retired immunization in the future. Your practice should no longer use the tilda (~) to retire immunizations.
-
Re-Enable Locked Out Practice Management Users: When your practice re-hires an employee or for some other reason restores access to the Practice Management system, they can now unlock a formerly locked account. For more information, read Partner User Administration.
-
Editing Notes on an Appointment Reset Form Printing: Under certain circumstances, editing the note on an appointment could cause the encounter to switch back to “not printed”, which could result in needless reprinting of visit forms. This no longer occurs.
-
New Flu Shot CVX Code: PCC updated the CVX codes on your system, including the new code 205: Influenza vaccine, quadrivalent, adjuvanted.
-
Improved Patient Search in pocketPCC: PCC 8.14 updates patient searching in pocketPCC. You can now look up patients using the PCC account number. Also, the search algorithm now matches the results in PCC EHR, which includes better guessing on search text that doesn’t quite match the patient’s name.
-
See Who Scheduled an Appointment in Reports: Appointment reports in the Report Library now correctly display the user who created the appointment.
-
Add Complete Lists of Allergies or Problems to a Form: PCC 8.14 includes three new form letter variables (
probs,allers, anderxallers) which you can use to display all of a patient’s Problem List items, PCC EHR allergies, or eRx allergies on a form letter. PCC Support can help you customize your forms to take advantage of these new variables.
Review an Encounter’s Billing History
Use the Billing History in a patient’s chart to see full details of what was billed for an encounter, what payments were collected, when claims were sent, acknowledged, and received, and more.
Video: Watch Work With a Patient’s Billing History to learn more.
Visit the Billing History
Click the “Billing History” button inside the History section of a patient’s chart to review the billing history for any encounter.
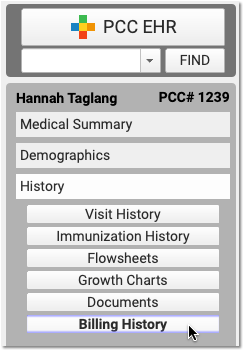
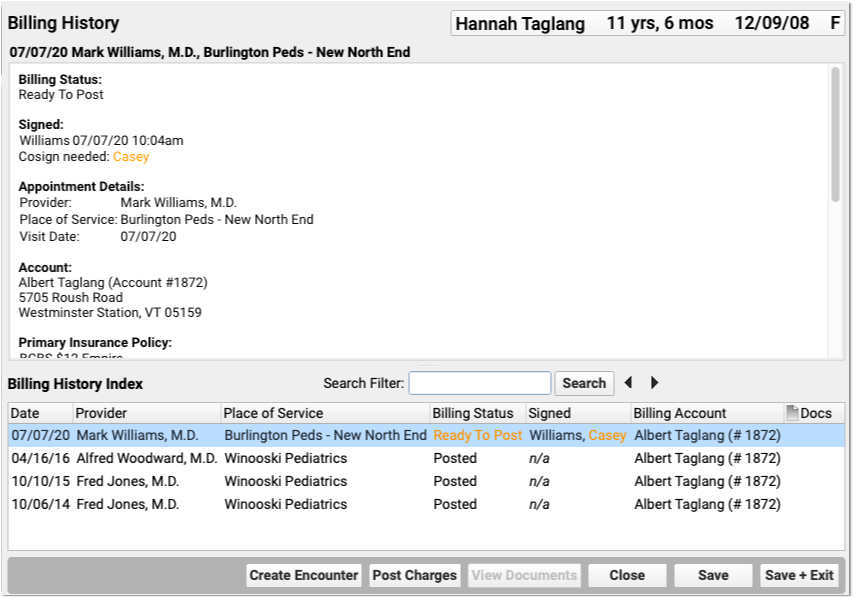
Office visits, telemedicine encounters, phone notes, portal messages, hospital charges, and administrative encounters that have been billed or may be billable appear in the index at the bottom.
When Do Encounters Appear in the History?: An appointment has a billing history entry as soon as an encounter’s status is set to “Arrived” or the patient is checked in. Phone notes and portal messages only have a billing history if the clinician clicked “Bill” and selected “Ready for Billing”. Hospital and administrative encounters appear after a user creates the encounter and posts the charges.
Review the Billing History for a Specific Encounter
Click on an encounter in the index to see details in the window above.
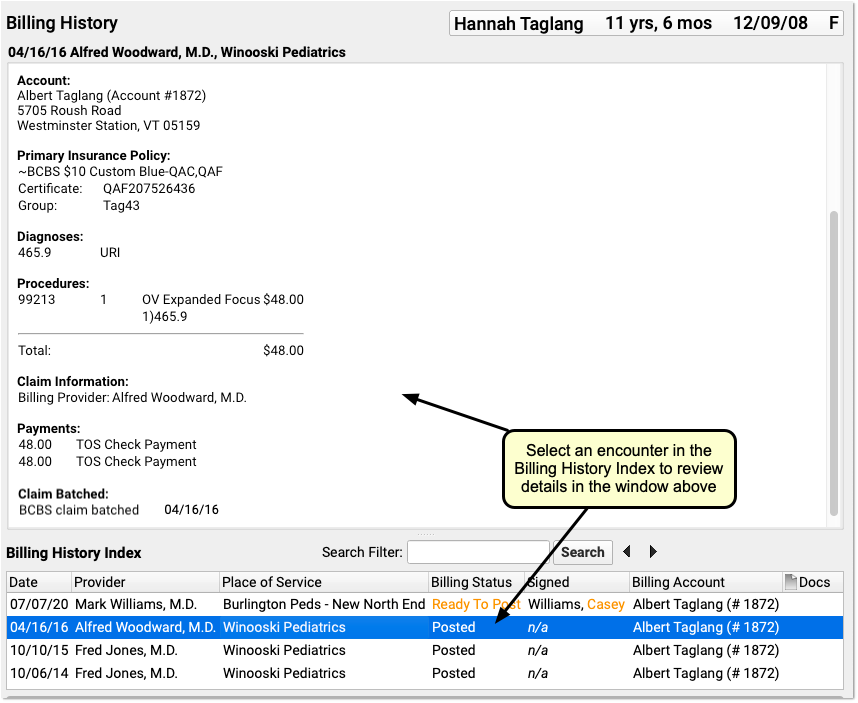
You can review encounter billing details, such as what diagnoses and procedures were posted, a payment history for the encounter, and a claim history for the encounter.
If an encounter still has the “Ready to Post” status, or has new items added to post, you can work with those encounters on this screen. Select the encounter and click “Post Charges” (or double-click on the encounter) to open up Post Charges.

Review Attached Documents: You can review any documents attached to an encounter in the Billing History section of the chart. For example, if a user attached a scanned insurance card, a hospital note, or other document to an encounter, you can double-click to open it.
Review Charge and Payment History for an Encounter
In the Procedures section of an encounter’s billing history, you can review charges for the encounter and a history of all payments.
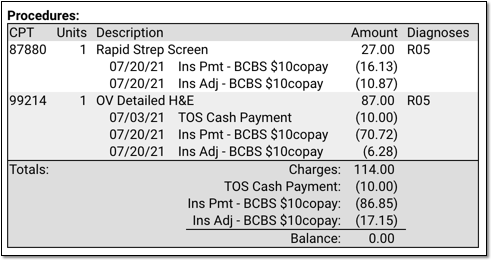
For each charge, you can see personal payments, insurance payments, and adjustments.
If any unapplied (or “unlinked”) payments on an account are paying off charges, you will see the “Payment (Unapplied)” amount indicated for each charge and in the totals section.
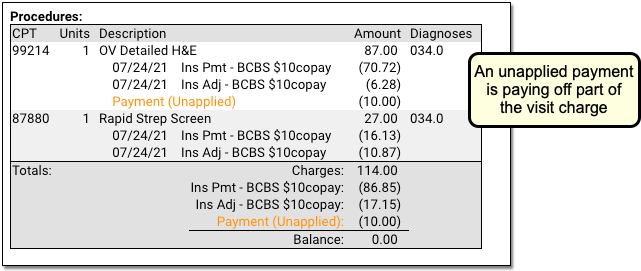
In the Payments section, you can review all payments posted on the same date as the encounter. To configure which payment types appear in this section, contact PCC Support.
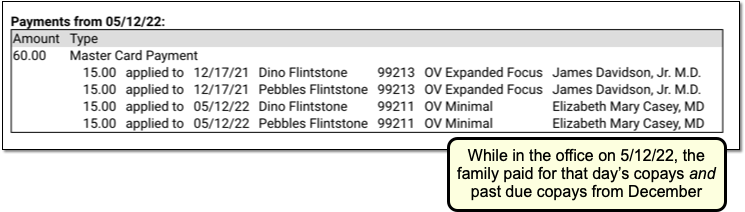
For each payment, you can review what charges the payment applies towards.
For more details about reviewing payment history, see Review Payment History and Edit Payments.
Review Claim History for an Encounter
When you need to understand when a claim was sent, acknowledged, paid, or resubmitted, use the Claim History found in the encounter’s Billing History.
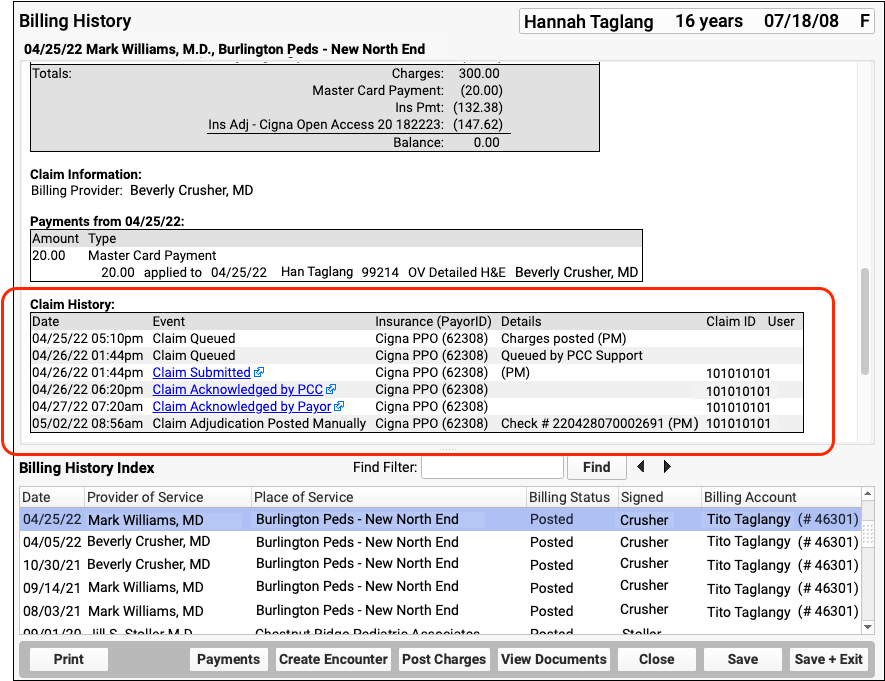
The Claim History shows the lifecycle of all claims for the encounter, from submission to resolution. You can see when a claim was queued, held, delayed, processed, received by PCC’s clearinghouse, acknowledged by the payor, and more.
For each event, you can see the date, the event, and the insurance plan. When available in your system’s records, the component displays additional details, the claim ID, and the user who performed the action.
If an encounter was submitted multiple times, the claim history will show you each submission along with claim acknowledgements and other events.
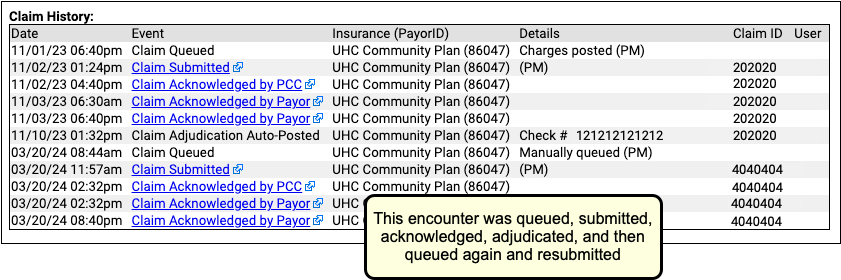
Read Claim Files, Acknowledgements, and Other Responses for an Encounter
When you need to dig deeper into a problem claim, you may want to review the claim submission log, acknowledgement, or other electronic response from a payor. When an electronic record is available for a claim event, you can click on a link to open it.
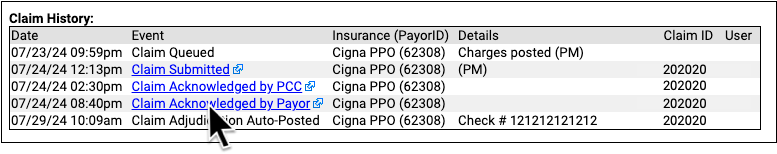
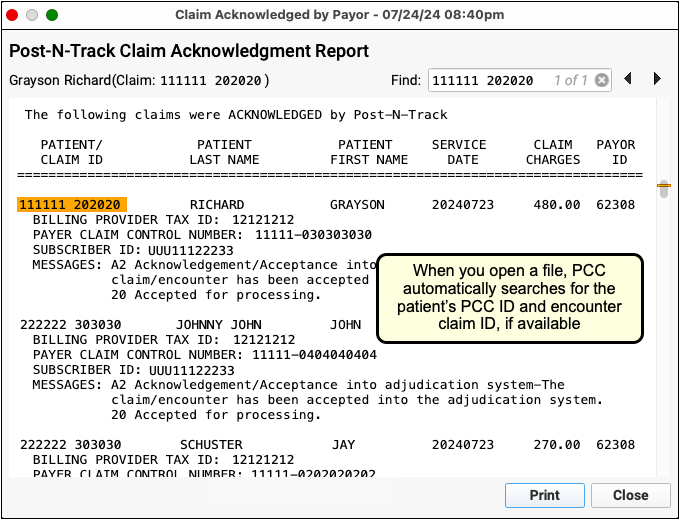
You can review the outgoing electronic claim file, claim acknowledgements, rejections, and most other responses for claims. (To review the ERA, use the Electronic Remittance Advice tool.)
Print an Encounter’s Complete Billing History
Select any encounter and click “Print” to print the billing history. It will include all charge, payment, and adjustment information along with details about the claim.
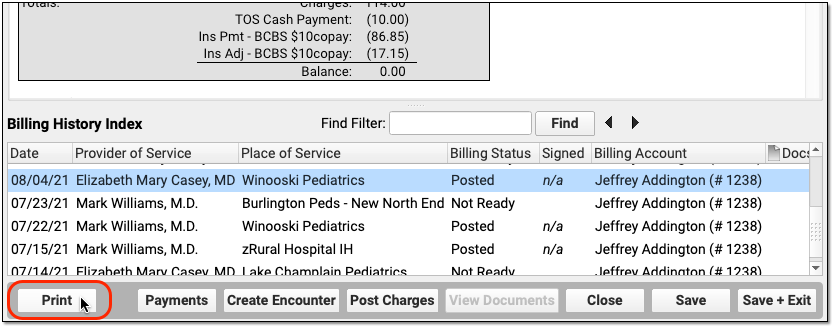
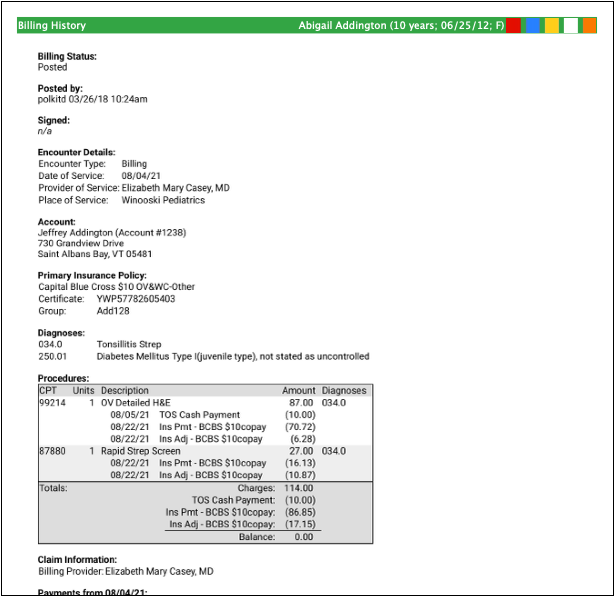
Edit Encounter Charges and Claim Details and Resubmit
If you need to edit the charges on an encounter or claim details, such as the place of service or additional information submitted with the claim, select and encounter and click “Edit Charges”.
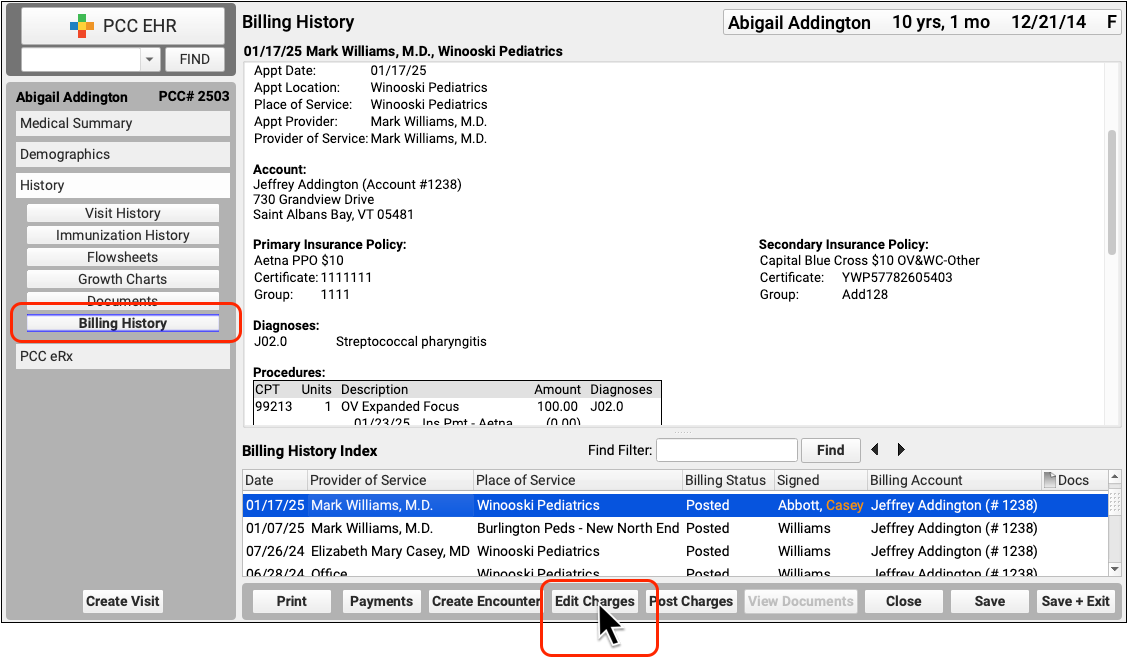
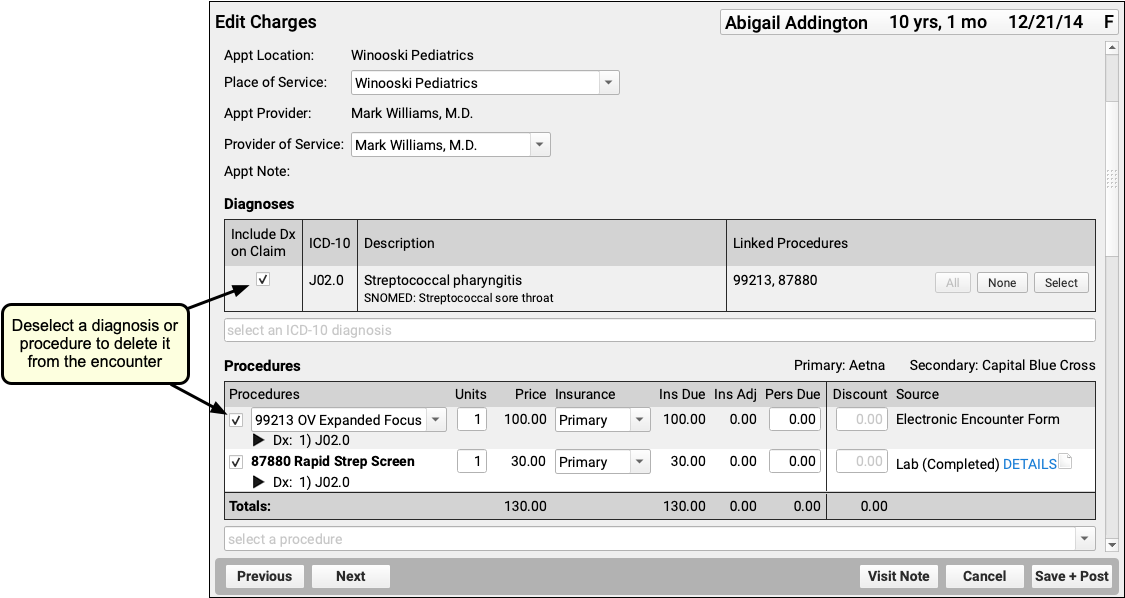
Read Edit Encounter Charges and Other Claim Information to learn more.
Other Ways to Review What Was Billed for an Encounter
In addition to the Billing History, there are two other ways to revisit the diagnoses and procedures for an encounter.
Open the Post Charges Workflow
You can reopen the Post Charges workflow after charges are posted. From there you can see what was posted and optionally add additional items to the claim. Reopen the Post Charges workflow from the patient’s Billing History as shown above or from the Schedule screen.
Click “Posted” or “New Items” on the Schedule screen to return to the Post Charges screen for an encounter your practice has already posted.
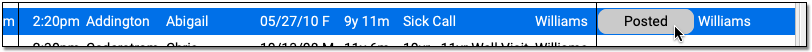
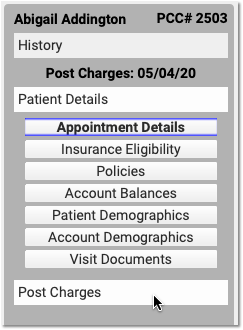
For information about the Post Charges window, read Post Charges and Check Out Patients in PCC EHR.
Review Diagnoses and Procedures on a Chart Note’s Electronic Encounter Form
You can also open a chart note’s “Bill” window and review the Electronic Encounter Form, which shows the selections originally made by the clinician.
Open the Patient Chart
Use the Find tool or double-click on an appointment to open a patient’s chart.
Click “Visit History”
Go to the Visit History section of the chart.
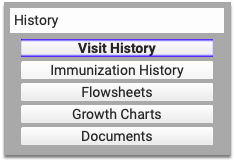
Find the Visit Date You Wish to Review
Use the list at the bottom to locate and select the visit you wish to review.
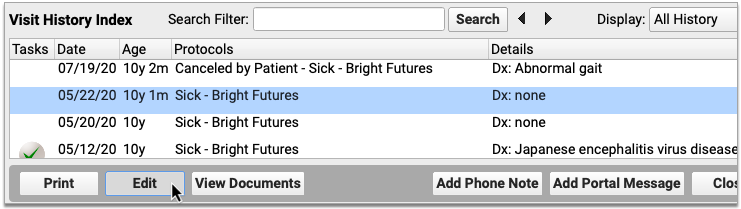
Double-Click or Click “Edit”
Click Edit to open the chart note. It will appear along with chart navigation buttons.
Click “Billed”
Click the “Billed” button at the bottom of the chart note to open the visit’s saved encounter form.
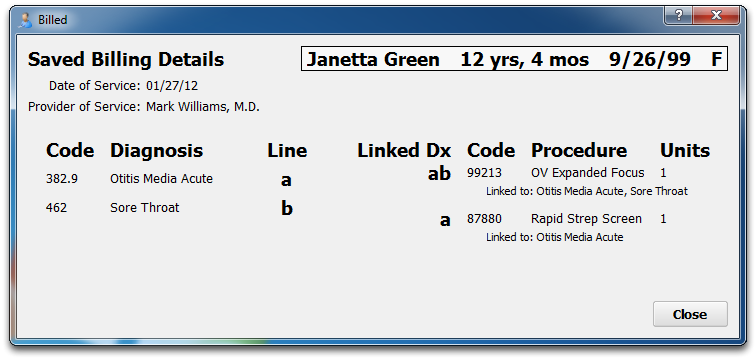
What Was Selected, Not What Was Billed: The Billed window retains a record of the procedures and diagnoses on the electronic encounter form, how they were linked, and how many units were indicated. After that information is made ready for billing, however, the biller can adjust that information when they post the charges and file the claim. The Billed window is a static record of what was made ready for billing by the clinician and does not reflect later changes.
Added After Posting: If a clinician added diagnoses or orders to the chart note after the visit was posted, those items will appear in a special section on the encounter form.
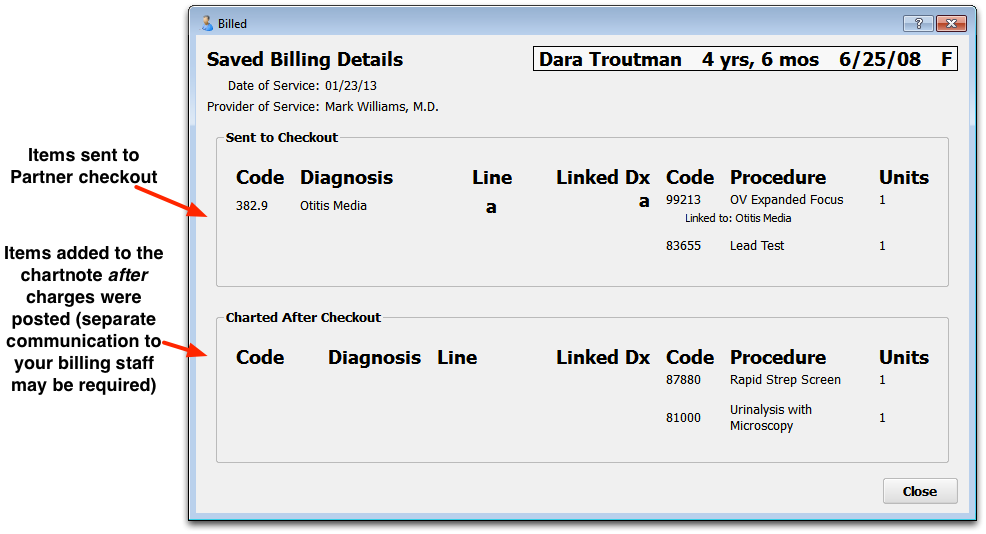
Look Up ICD-10 Codes for a Patient’s Diagnoses During an Encounter
If you are filling out a form or need the ICD-10 code billed for a patient’s diagnosis during an encounter, you can use the Diagnosis Flowsheet in a patient’s chart to quickly get the codes you need.
For more information, read the Look Up ICD-10 Codes for Referrals, DME, Requisitions, and Pre-Authorizations article.
Create a New Encounter
Billers typically post charges for appointments on the Schedule screen, or post charges for phone notes or portal messages from the Messaging queue. You can also create a new encounter in the Billing History section of a patient’s chart.
Click “Create Encounter” to post charges of any kind, without a scheduled appointment. For example, you may want to post a hospital encounter or administrative fees.
Post Hospital Charges
If your practice bills for hospital visits, you can post the charges in PCC EHR and queue up a claim. Read the procedure below to learn how.
Video: Watch Post Hospital Charges in PCC EHR to learn more.
Open the Patient’s Chart and Navigate to Their Billing History
When you are ready to post hospital charges for a patient, open their billing history and create a new encounter.
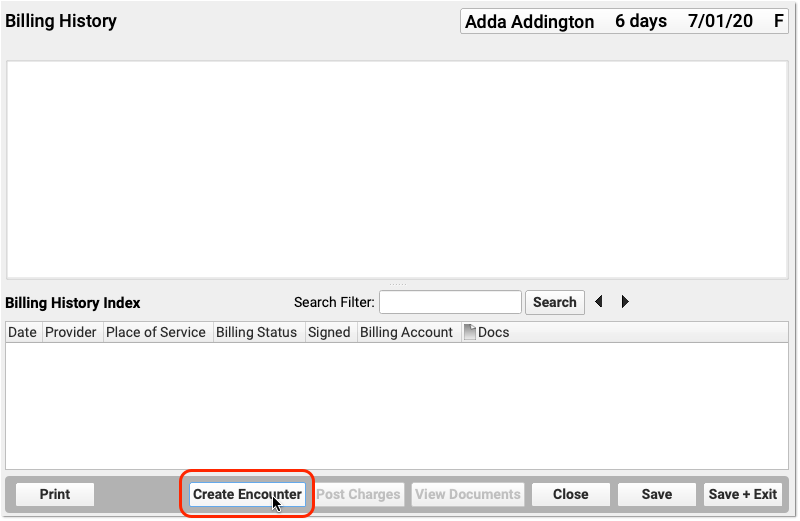
Select the Provider, Location, and Service Dates
PCC EHR will create a blank Post Charges encounter for billing. In the Encounter Details section, select a provider, a hospital location, and enter dates of service.
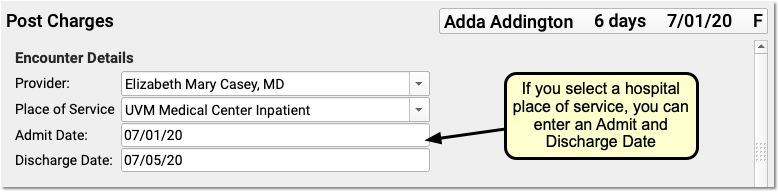
If you select an inpatient hospital location, PCC EHR will display Admit and Discharge fields for the encounter instead of a Service Date field. If the hospital visit was only a single day, you can leave the discharge field blank or enter the same date in both fields.
What If I Don't See the Location I Need, or I Don't See the Admit and Discharge Date Fields?: Your practice can customize your location list and specify which locations are for inpatient visits. Contact PCC Support for help customizing your billing locations.
Select Hospital Diagnoses and Procedures
Use the Diagnoses and Procedures components to search for and select charge information for the hospital encounter.
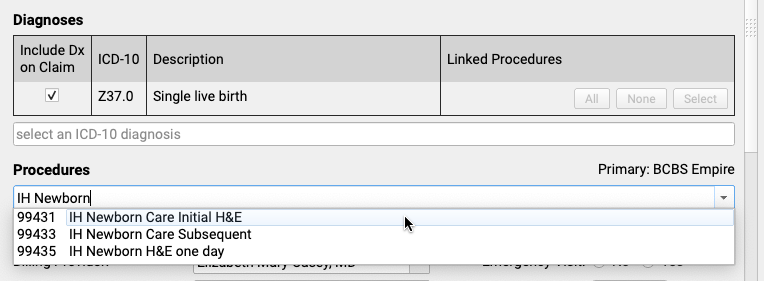
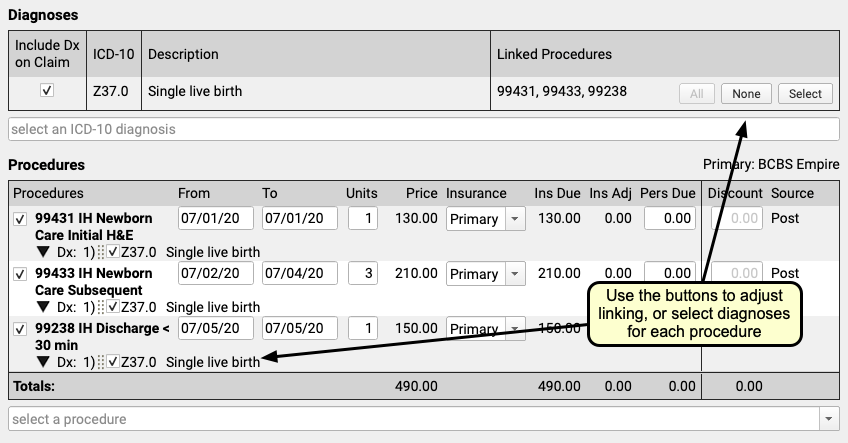
You can optionally enter from and to dates for procedures, or simply use a single date in the From field. You can set units, select insurance or self pay, adjust the personal due amount, and optionally add a discount. If a procedure has no defined price at your practice, you can edit the price field.
Remember to link the appropriate diagnoses with each procedure using the tools in either the Diagnoses or Procedures component.
Optional: Adjust Claim Information, Work w/ Personal Balances and Payments
You can use the Claim Information component to adjust the billing provider or other claim details. While you probably don’t have a personal payment on hand for a hospital visit, you can use the Payments component to review personal balances and enter discounts as well, if needed.
Click “Save + Post” and Review the Encounter
When you are finished entering hospital encounter and charge information, click “Save + Post” to save your work and queue up a claim.
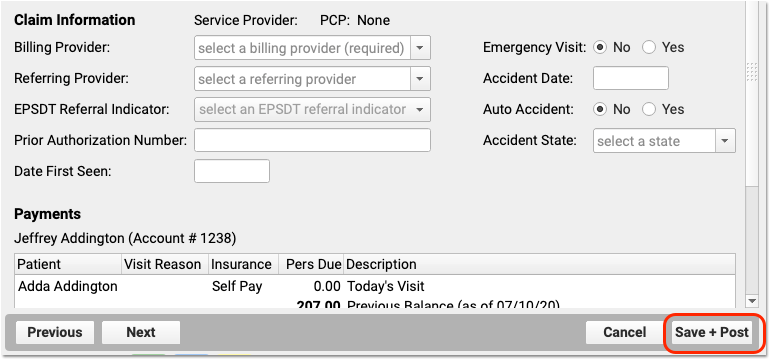
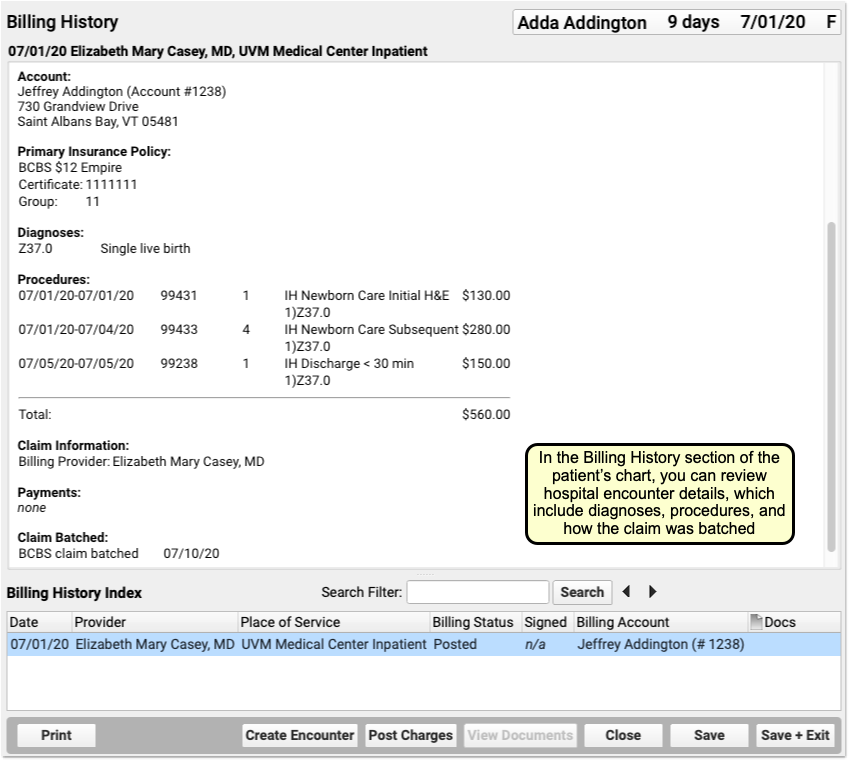
You can review hospital charges in the Billing History. They also appear in the patient’s Visit History.
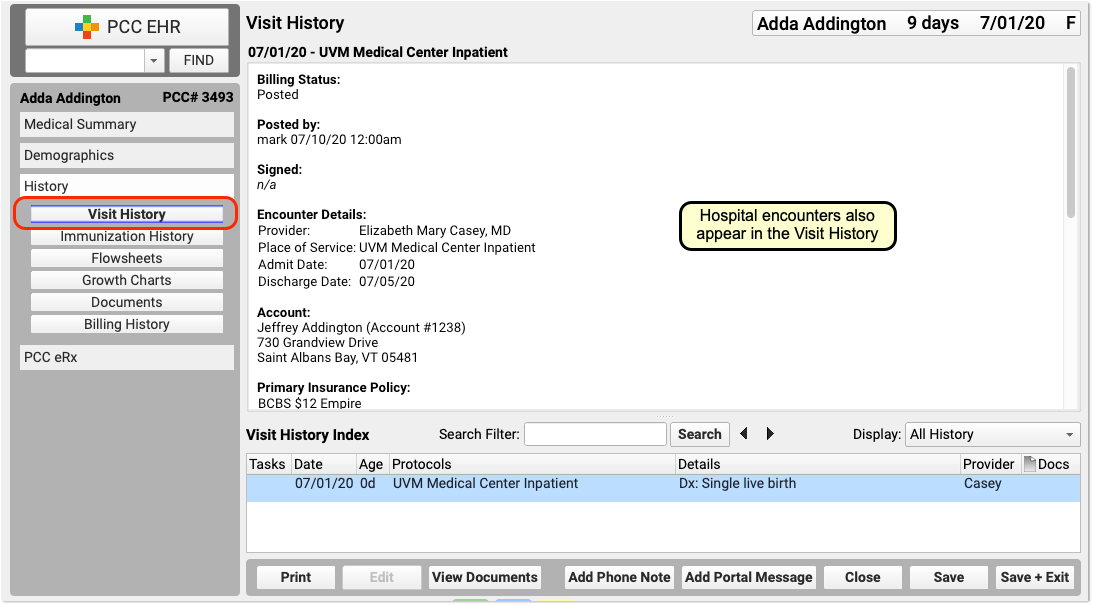
You can use the Search Filter field and the Display Filter drop-down menu in either History chart section to quickly find and review details about hospital encounters.
Optional: Import and Attach Documents
After you post a hospital encounter, you can attach a hospital note or other document to the encounter. Just select the hospital encounter when you import or edit a document.
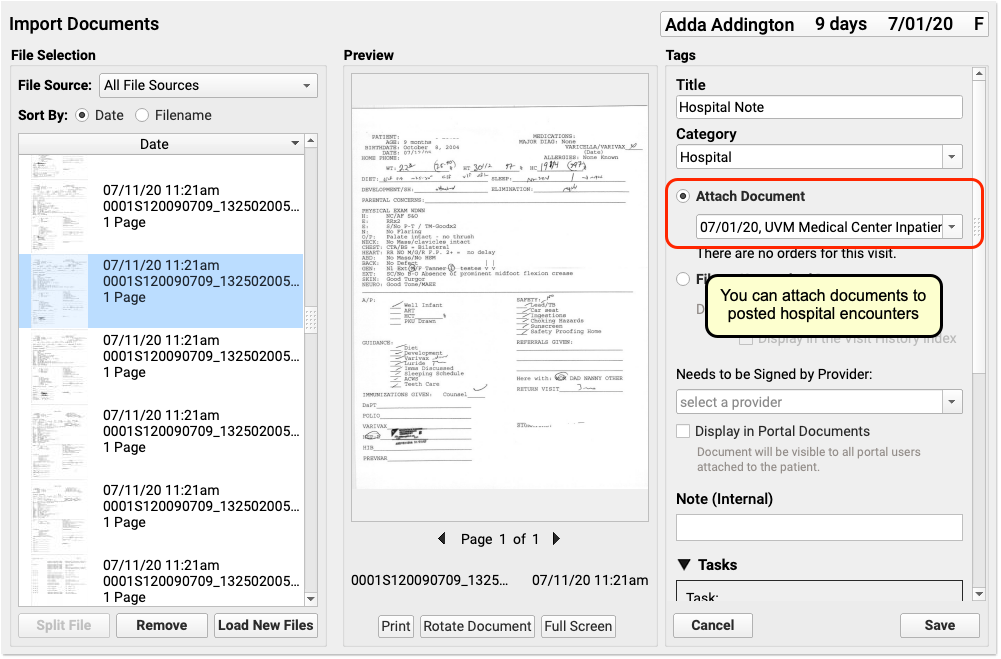
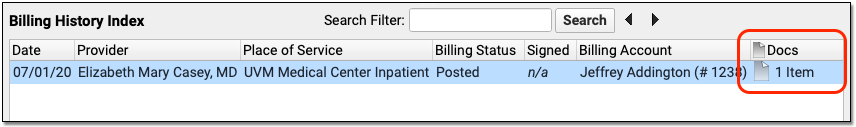
Delete a Hospital Encounter Posted in Error
If you post a hospital encounter to the wrong patient or need to delete it for another reason, return to the Billing History in the patient’s chart. Select the encounter and then click “Edit Charges”. Deselect all diagnoses and procedures from the encounter. When you click “Save + Post”, the encounter will be removed from the patient’s billing record.
Generate Patient Forms with Information from a Specific Encounter in PCC EHR
PCC Support can add forms to your PCC system that auto-insert patient vitals, provider signatures, and other information based on where you generate them in PCC EHR. These auto-insert fields are called variables.
If you need forms that auto-fill with information from a particular visit, phone note, or portal message, ask PCC Support to add encounter variables to your forms. Forms that include encounter variables pay attention to where you are generating them in PCC EHR, and insert information accordingly. If you generate a form with encounter variables from a visit note, the encounter variables populate with information from that visit. If you generate the same form from a generic place in PCC EHR, like a patient’s Medical Summary or the check-in ribbon, the encounter variables populate with information from the patient’s most recent visit.
There are encounter variables for patient vitals, provider of service, place of service, and provider signatures.
Contact PCC Support to get help creating and using form templates that include encounter variables.
Generate a Form with Details from a Specific Visit
Open the Visit in PCC EHR
Open the visit that contains the details you want to print on a form. It can be a visit that is currently in progress or a past visit.
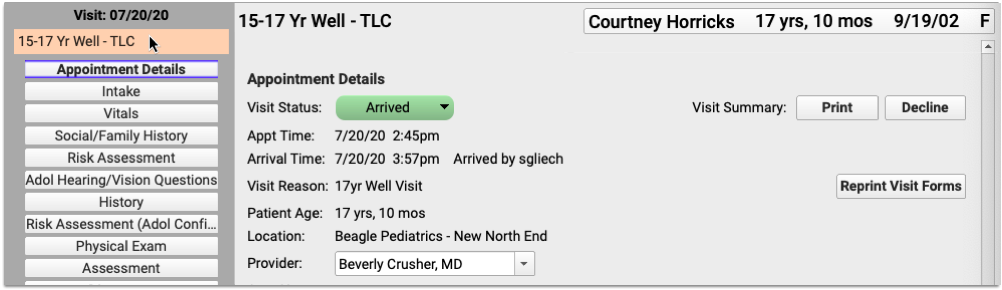
You can open visits from the Schedule screen in PCC EHR, or from the patient’s Visit History.
Generate a Form
Navigate to the Forms component within the visit.
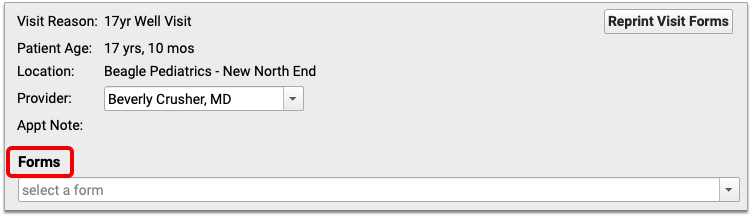
Select the form template that includes encounter variables and generate it.
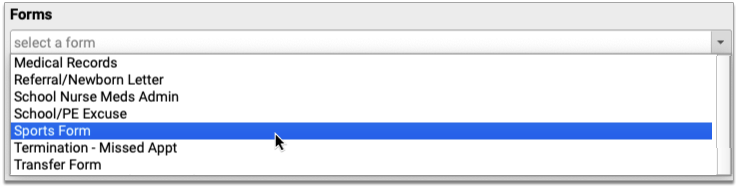
A preview of the form opens in a Document Viewer window.
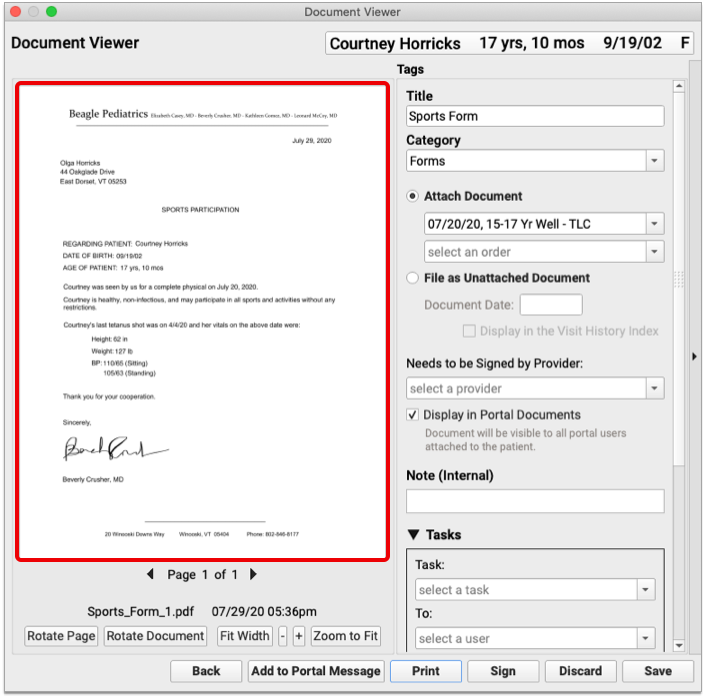
The encounter variables on the form populate with information from the visit where the form was generated.
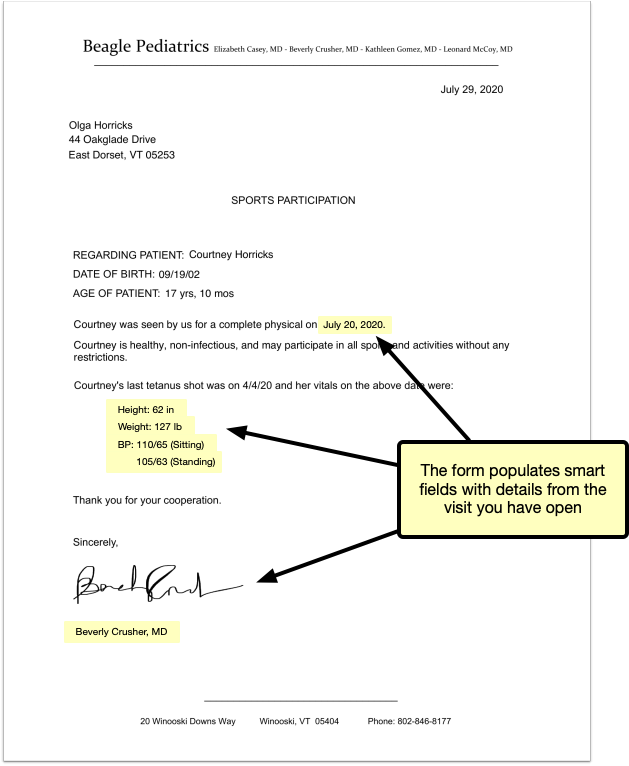
No Forms Component? Add It to the Visit Protocol: You can only include visit-specific information on a form if you generate the form from that visit’s note, but not visit protocols contain a Forms component. You can add a Forms component to your visit protocols in the Protocol Configuration tool.
Save the Form
Review your form to make sure the auto-inserted details are correct. Then, save, print, or share it to the patient portal. You can also create tasks from it, or send it to a provider for signing.
Generate a Form with Details from a Phone Note or Portal Message Encounter
Open the Patient’s Chart
Search for your patient in PCC EHR or open their chart from the schedule screen.
Create a New Phone Note or Portal Message
Create a new phone note or portal message from the Edit menu.
You can also create a new phone note or portal message using the buttons displayed at the bottom of the Medical Summary, Demographics, and History sections of the patient’s chart.

Fill Out the Encounter Details
Choose a provider and location for the encounter, and fill out the encounter details.
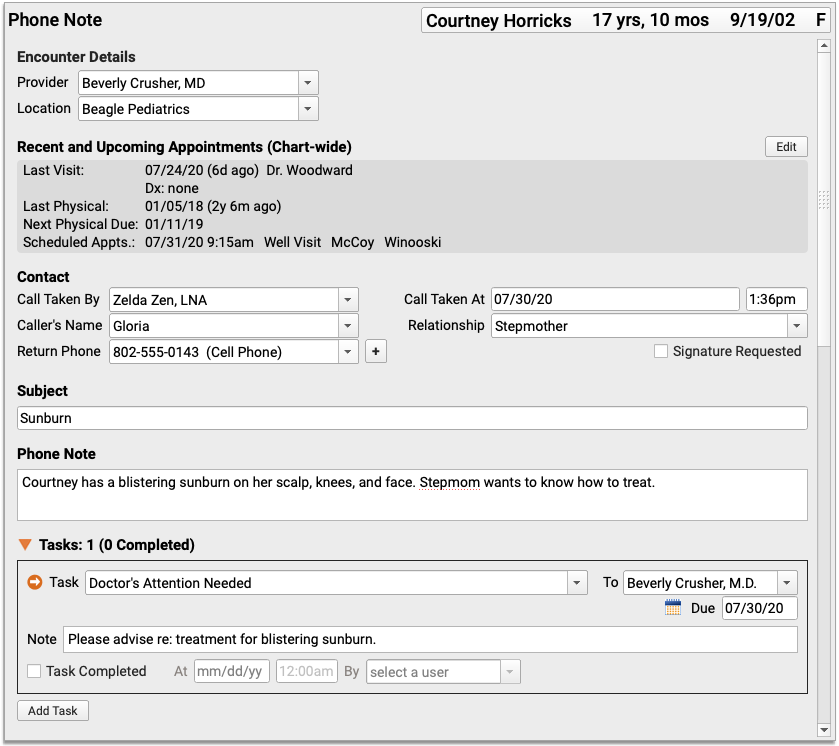
Save the Encounter Details
Click “Save” to save the contents of the phone note or portal message. You must save the encounter details before they can appear on a form with encounter variables.
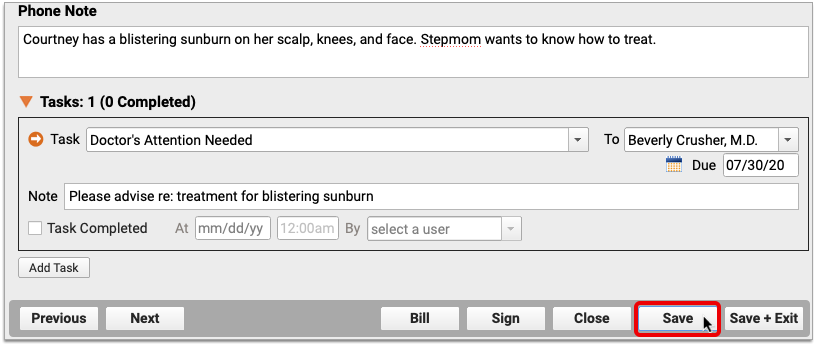
Do Not Exit the Encounter: Do not click “Save + Exit” at this stage. If you exit the phone note or portal message, you will not be able to generate a patient form within the encounter.
Generate a Form
Navigate to the Forms component within the phone note or portal message. Select the form template that includes encounter variables and generate it.

A preview of the form opens in a Document Viewer window.
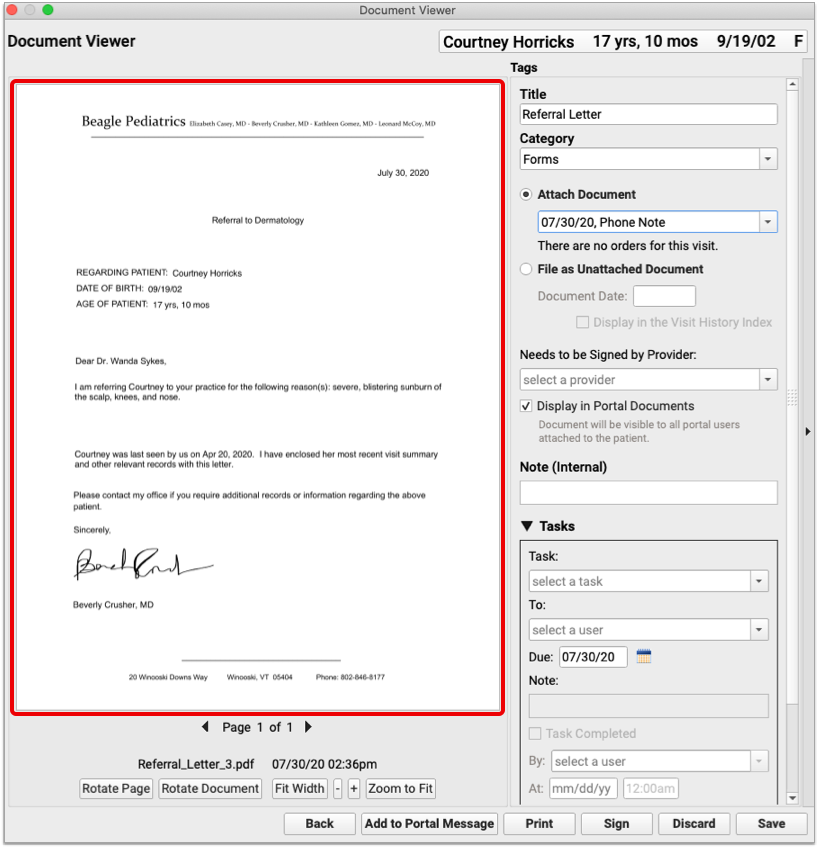
The encounter variables on the form reflect information from the phone note or portal message where it was generated.
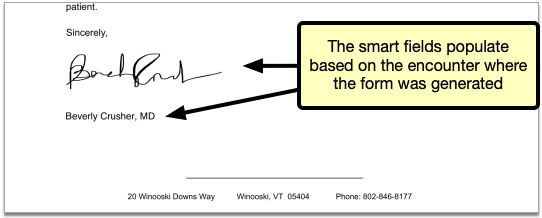
Save the Form
Review your form to make sure the auto-inserted details are correct. Then, save, print, or share it to the patient portal. You can also create tasks from it, or send it to a provider for signing.
Generate a Form With Details From a Patient’s Last Visit
When you generate a form template that includes encounter variables from a generic place in PCC EHR such as a patient’s Medical Summary or during check-in, the encounter variables populate with details from the patient’s last visit.
Learn More About Encounter Variables: For a list of encounter variables and to learn how to incorporate them onto your patient forms, contact PCC Support.
Post Administrative Fees Without an Appointment
When you post charges for an appointment, you can also add fees and payments. You can also collect copays right in the Patient Check-In tool in PCC EHR.
But what if there is no appointment? You may need to collect a fee or post other charges (and payments) that do not have an encounter. To do so, you can create an administrative encounter or “billing encounter”.
Create a Billing Encounter to Bill a Fee
To bill for a fee of any kind, visit the Billing History in the patient’s chart and click Create Encounter to record an administrative encounter.
Follow the procedure below to learn how.
Open a Patient’s Billing History
Open the patient’s chart, click on the History navigation button, and select “Billing History”.
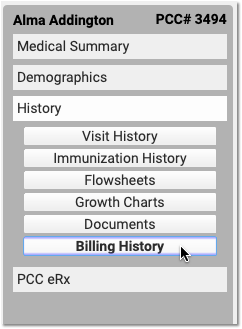
Click “Create Encounter”
After optionally reviewing the patient’s current billing history, click “Create Encounter” to create a new administrative encounter.
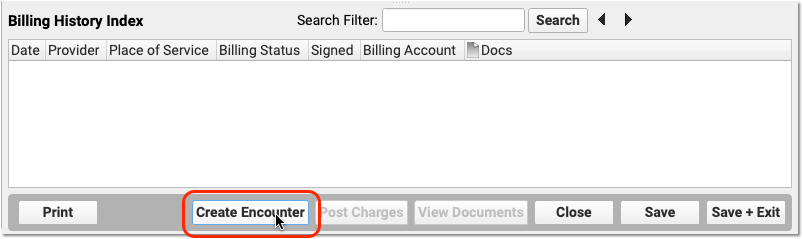
Select a Provider
Select a provider for billing. Charges require a provider.
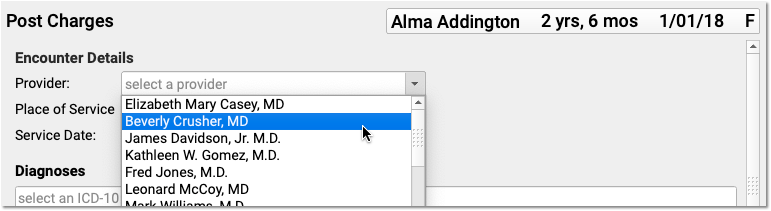
Optionally Adjust the Place of Service or Date
You can optionally change the Place of Service and Service Date for the administrative encounter.
Select the Fee’s Billable Procedure and Adjust the Procedure Details
Find and select a billable procedure in the Procedures component. Your practice keeps a customizable list of administrative fees in your system’s Procedures table.
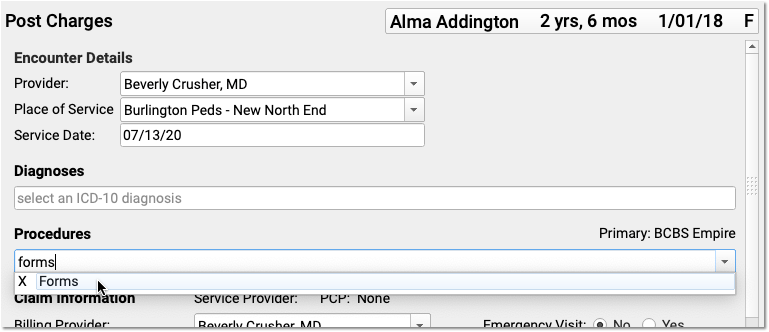
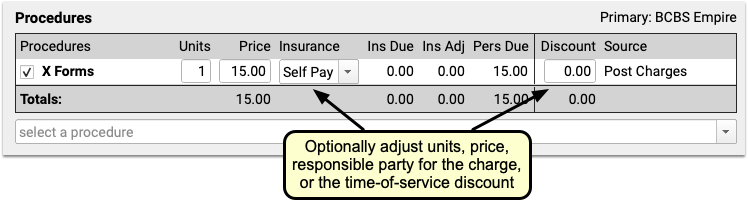
Many practices leave the default price of administrative procedures blank. You can then enter the price as you post the charge. You can also adjust units, the responsible party for the charge (the patient’s insurance policy or “Self Pay”) and enter a time-of-service discount.
What About Diagnoses? Will a Fee Require One?: Normally, a procedure requires a diagnosis. However, you can post an administrative fee without a linked diagnosis. In your practice’s procedures table, you can define all of your various fees and optionally set their default amounts. Any procedure that has a billing code with fewer than five characters will not require a diagnosis when you post charges. For more information, read Edit Your Practice’s Prices and Billing Procedure Codes.
Optionally Enter a Payment
Optionally select a Payment Type and enter a payment. You can adjust the payment to apply toward’s the fee you are entering or past due balances.
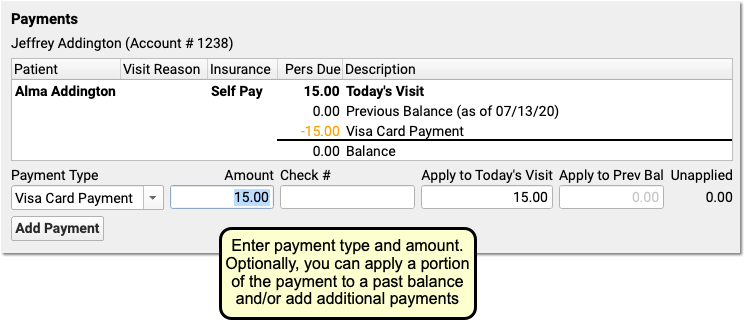
You can optionally click “Add Payment” to add more payments.
Optionally Generate a Receipt
Click the “Generate a Receipt” checkbox to ask PCC EHR to print a receipt as soon as you save the charges.
You can also return to Post Charges for this encounter later and generate a receipt.
Click “Save + Post” and Review the Charges
Click “Save + Post” to save the charges. The new administrative encounter will appear in the Billing History.

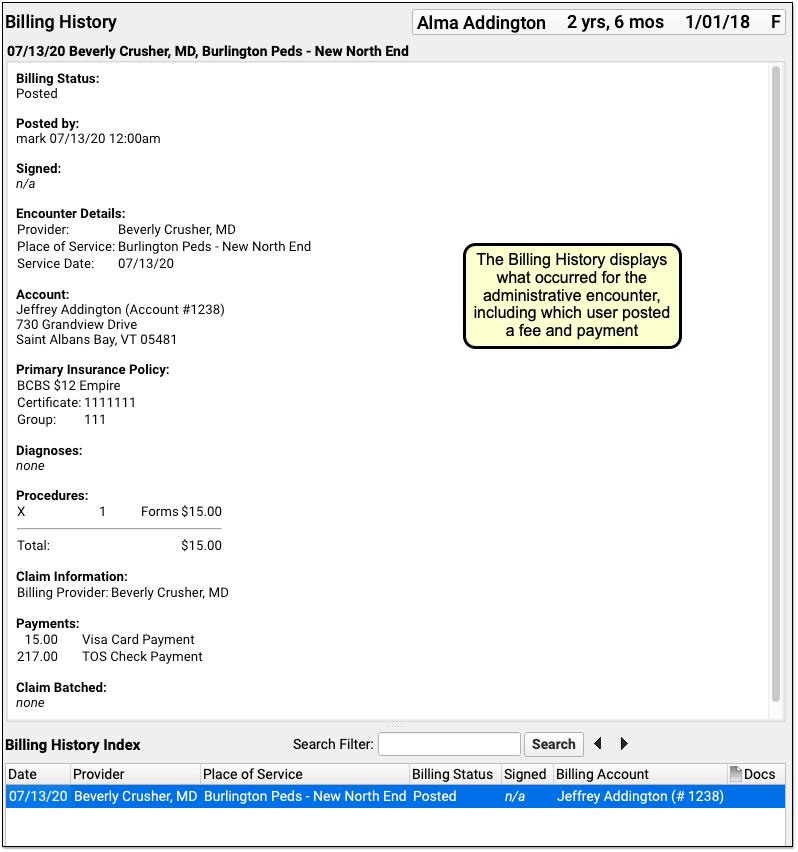
On the Billing History, you can see full details of the encounter, including which user at your practice posted the charge, the fees that were posted, and any payments.
Will Administrative Fees Appear on the Chart's Visit History?: Hospital charges, telemedicine visits, and other clinical encounters appear on the patient’s Visit History. Administrative encounters, such as a forms fee, do not appear on the Visit History and only appear on the Billing History.
Delete an Administrative or Billing Encounter Posted in Error
If you post a fee or other administrative encounter to the wrong patient or need to delete it for another reason, return to the Billing History in the patient’s chart. Select the encounter and then click “Edit Charges”. Deselect all billing procedures (and diagnoses, if any) from the encounter. When you click “Save + Post”, the encounter will be removed from the patient’s billing record.
Post a Payment Without Creating an Encounter
The procedure above shows how to create a billing encounter and optionally post a payment.
You can also post a payment without an encounter.
Read Post Personal Payments and Write Off Charges or watch a tutorial video to learn how to post payments.
Review, Order, and Administer Immunizations
Use PCC EHR to track, review, order, and administer immunizations in PCC EHR. The procedure below will ensure smooth administration of immunizations for you, your staff, and your patients.
Review Patient’s Immunizations
A patient’s immunization history appears two places: on most chart notes and in the Visit History section of the patient’s chart.
Immunization History includes a date for each administered immunization listed in chronological order. When an immunization is administered, the date will appear automatically.
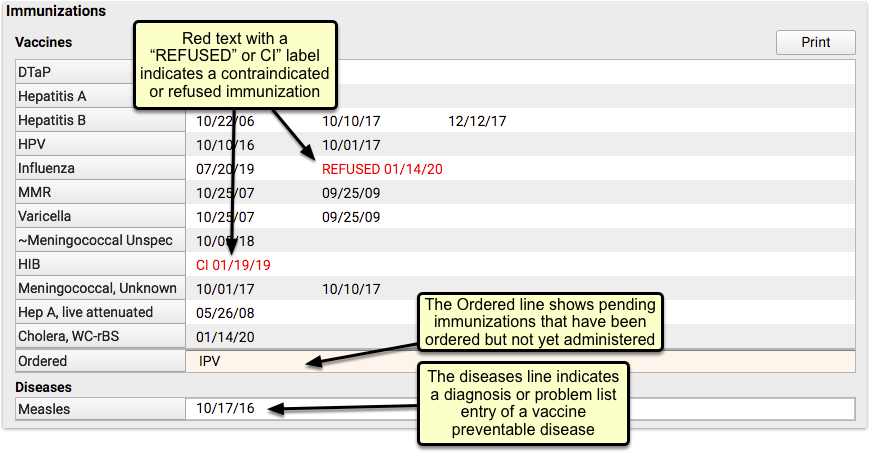
Vaccines are color coded – black text indicates a normal application, red indicates that it was not given. Vaccines not given include a reason: refused, or “CI” for contraindicated. Vaccines that are ordered but not yet administered are listed in the Ordered line. Vaccine preventable diseases are listed with the diagnosis date in the Diseases section.
Review Forecasting and Immunization Recommendations
Next, review the Vaccine Forecasting below. The Forecasting Results compares each patient’s immunization history to the IMMUCAST immunization schedule, and shows a range of dates for each, depending on the patient’s details.
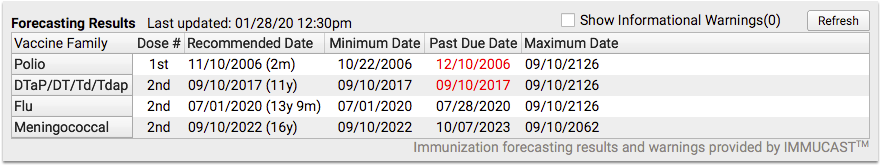
For each vaccine family, from left to right, you can see:
- the next expected dose in the series (1st dose, 2nd, 3rd, etc),
- the recommended date (when it is ideal to receive this immunization) along with the patient’s age on that date,
- the minimum date the immunization could be given early,
- a past due date,
- and a maximum date after which the shot or series would be invalid. (Rotavirus is the only common immunization with a normal Maximum Date.)
This information is intended as a guideline or reference, the ultimate decision on when a vaccine should be given is up to you and your patients, but you may find it helpful when making that decision. To learn more, read Immunization Forecasting.
Check VFC Status
Before you create immunization orders for today’s visit, review the patient’s insurance policy and optionally update their VFC status.
If it’s not already entered from a previous visit, you can select the patient’s VFC status right in the Immunizations component on the chart note.
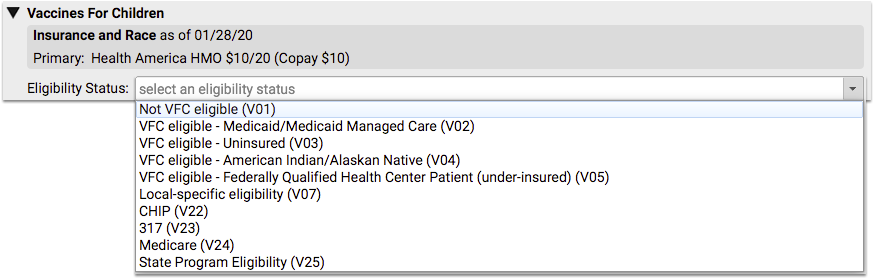
You can also select VFC status in each individual immunization order, but selecting it here will apply the same choice automatically to all future immunizations for this patient.
Order Immunizations and Optionally Assign Tasks
If the visit’s chart note protocol includes pre-selected immunizations appropriate for this visit type, it can be ordered with a single click of the edit button.
If today’s immunization isn’t available in the protocol, start typing the immunization’s name in the text field, or select any immunization from the drop-down menu below and then click order.
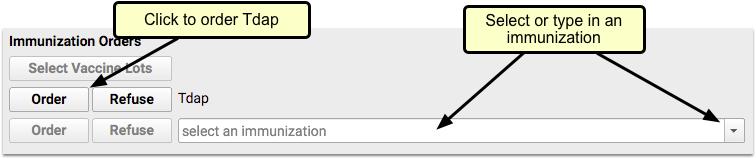
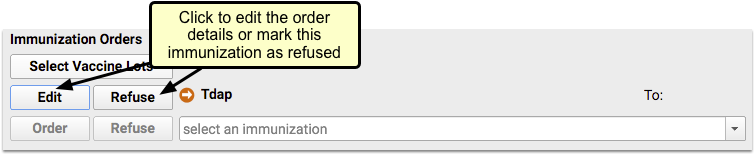
If you aren’t administering the immunization yourself, click edit and assign the task to someone else with the “To” menu.
Answer Memory: The next time you click order, PCC EHR will remember your selection and automatically assign this task to that person. To select someone else, click edit and select again.
If you’re assigning the task to someone else, you’re done. Click save changes and move on with the visit. The immunization task will appear as an orange order indicator on the Schedule in PCC EHR and on the selected user’s Visit Tasks queue.
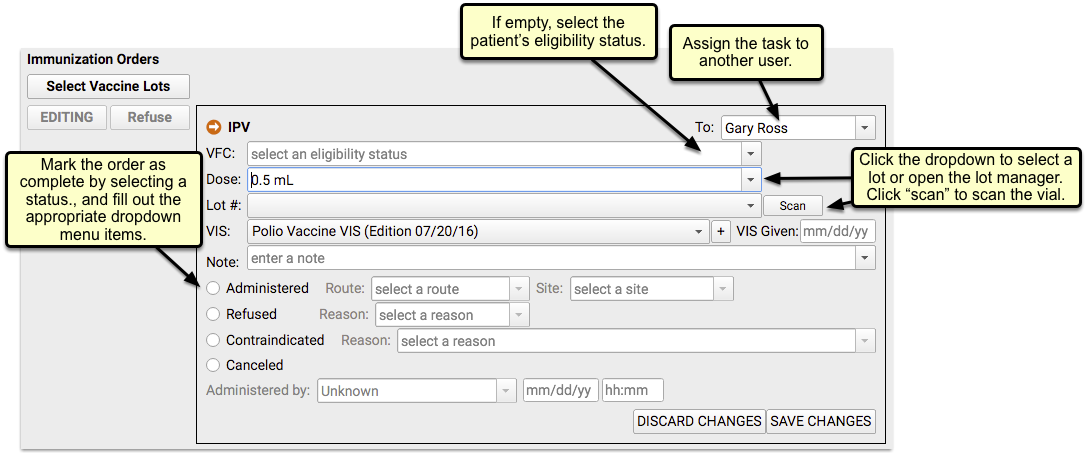
To complete the order, click the orange ball indicator on the schedule or double-click from the Visit Tasks queue.
The order details screen includes everything you need to record to complete the immunization. If you selected the VFC status above, it will be copied here already. You can manually select an appropriate immunization lot from inventory. If you have a barcode scanner, click the scan button to open the scanning window, where you can scan the vial and automatically enter the lot number and dose.
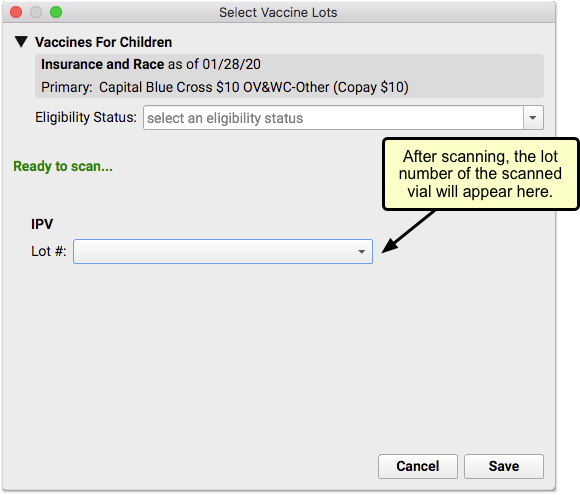
If you don’t use a barcode scanner, you’ll need to select the lot number and dose manually from the drop-down menu, or if needed, launch the Lot Manager to add a new lot.
Enter any notes, and click the result of the order; administered, refused, contraindicated or cancelled.
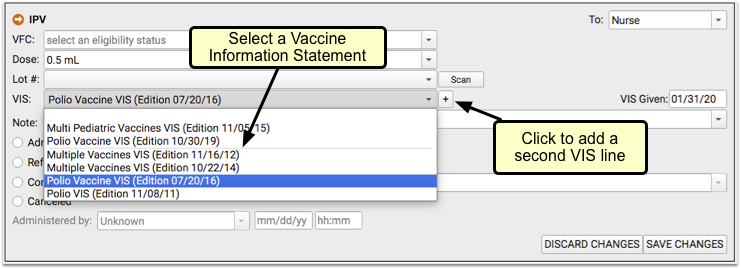
Any selection or note entered in an immunization order can be changed later, even after saving.
Answer Memory: As with the order assignment above, PCC EHR will remember your previous answers and will suggest the same VIS, dose and other details the next time you order this Immunization
With the order details entered, and the vaccine is administered, save your changes and move on to the rest of your visit.
Add Historical Immunizations
In addition to administering current immunizations, you may find it necessary to record historical immunizations, or immunizations administered elsewhere – like a flu shot – without completing the order process.
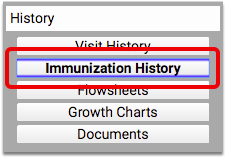
You can edit and update each immunization’s VFC information, dose, lot number, manufacturer, VIS information, note, as well as whether the immunization was administered, refused, contraindicated, or canceled. When selecting certain options, such as Contraindicated, you can add additional details, such as a contraindication reason. All completed immunization orders can also include who completed the order and a date and time.
Historical immunizations or those given elsewhere – a flu shot given outside of your office, for example – can be added manually by clicking Add Imms.
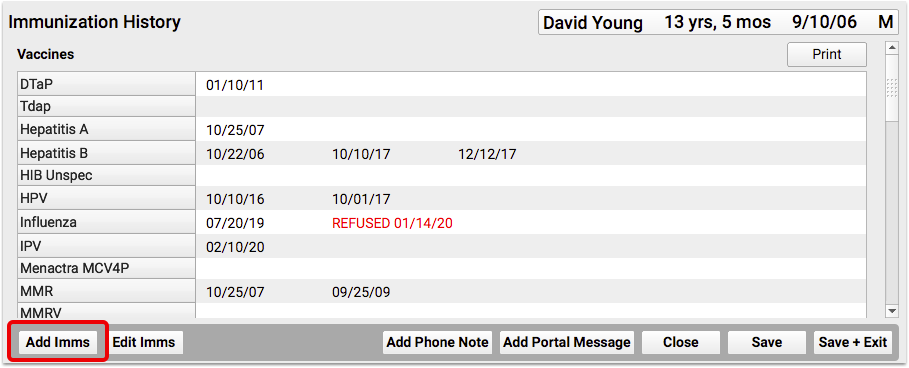

Select an immunization from the drop-down menu, or begin typing to search, and then enter the date or dates of immunization. Clicking save will add the date to the appropriate spot in the patient’s history.
Generate Outbound Lab and Radiology Requisitions
After ordering labs or x-rays during a visit, you can easily generate requisitions with the patient demographic, insurance, diagnostic, and testing information that the lab or radiologist needs.
Generate a Requisition
You can generate lab and radiology requisitions from your patient’s encounter note in PCC EHR. Requisitions can include diagnoses, orders, and other information from the encounter. If the patient needs tests from multiple labs, you can generate multiple requisitions within the visit and include only the specific information each facility needs.
Open the Patient’s Encounter Note
In PCC EHR, open the visit, phone note, or portal message where you plan to order labs or x-rays.
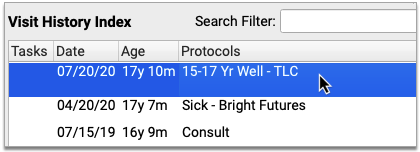
Document Diagnoses
Document the patient’s diagnoses, including those you will need to report on the lab or radiology requisition.
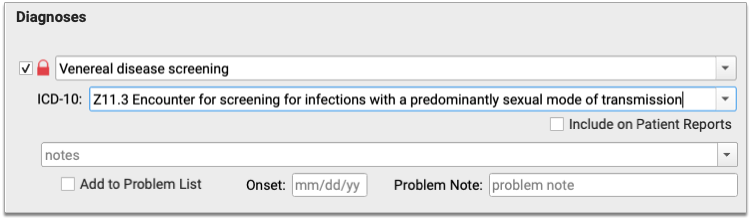
Place Orders
Order the patient’s labs or x-rays.
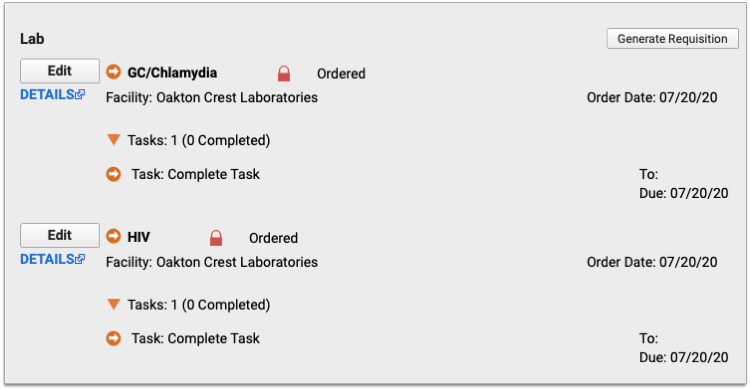
Generate a Requisition
Click the “Generate Requisition” button within the lab or radiology orders component.
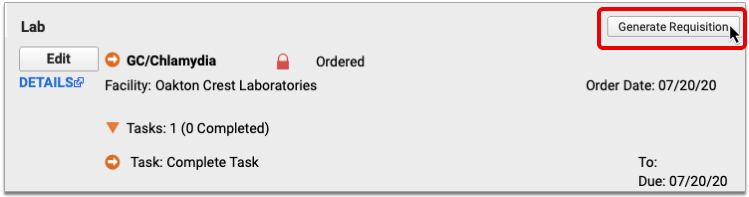
For Lab Requisitions, Select a Facility
If all of the patient’s lab orders list the same facility, that facility will be pre-selected in the Generate Requisition window. Otherwise, select the facility for which you wish to generate a lab requisition.
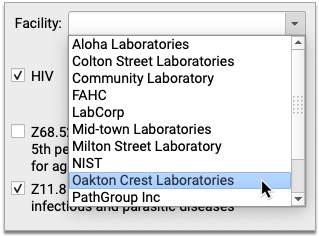
If you leave the Facility drop-down field blank, the requisition will generate without a facility address or phone number.
No In-Office Facilities: In-office laboratories are excluded from the list of facilities.
No Facility Drop-Down for Radiology Requisitions: Because there is no place to record radiology facility information in PCC EHR, the Facility drop-down is never available for radiology requisitions.
Select a Form
Select the form you wish to generate from the Requisition Form drop-down.
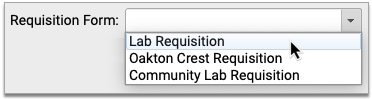
If you do not see a Requisition Form drop-down, it means your practice only has one requisition template configured for use.
Select Orders and Diagnoses
Select the orders and diagnoses you want to include on the requisition.
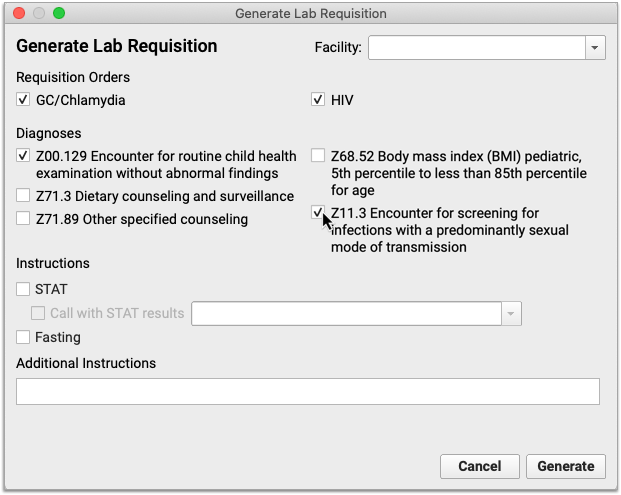
The orders and diagnoses presented in the Generate Requisition window come from the patient’s encounter note and exclude in-office tests.
Fill Out Instructions
Use check boxes to indicate if the requisition is for STAT or fasting orders.
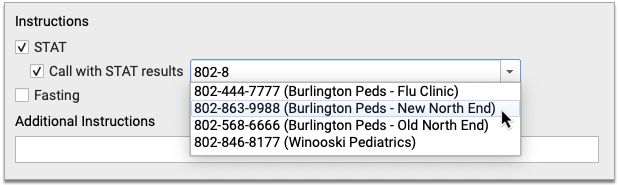
For STAT orders, indicate if you would like a call with results and which phone number to use. Manually type a number or pick one from the drop-down list. The drop-down list comes pre-populated with phone numbers for each of your office locations, and also remembers the most recent numbers entered by the user generating the requisition.
Write additional details or instructions in the Additional Instructions field.
Finish Generating the Requisition
Click the “Generate” button to finish generating the requisition.
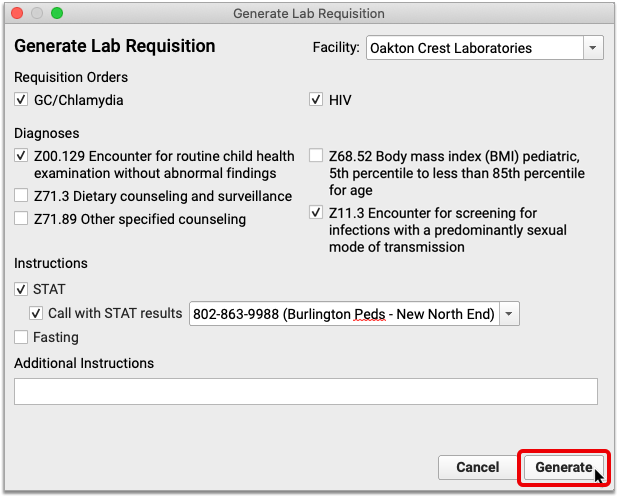
Review and Title the Requisition
When the preview of the requisition opens in a Document Viewer window, give your requisition a title, optionally change the document category and add tasks in the Document Viewer window.
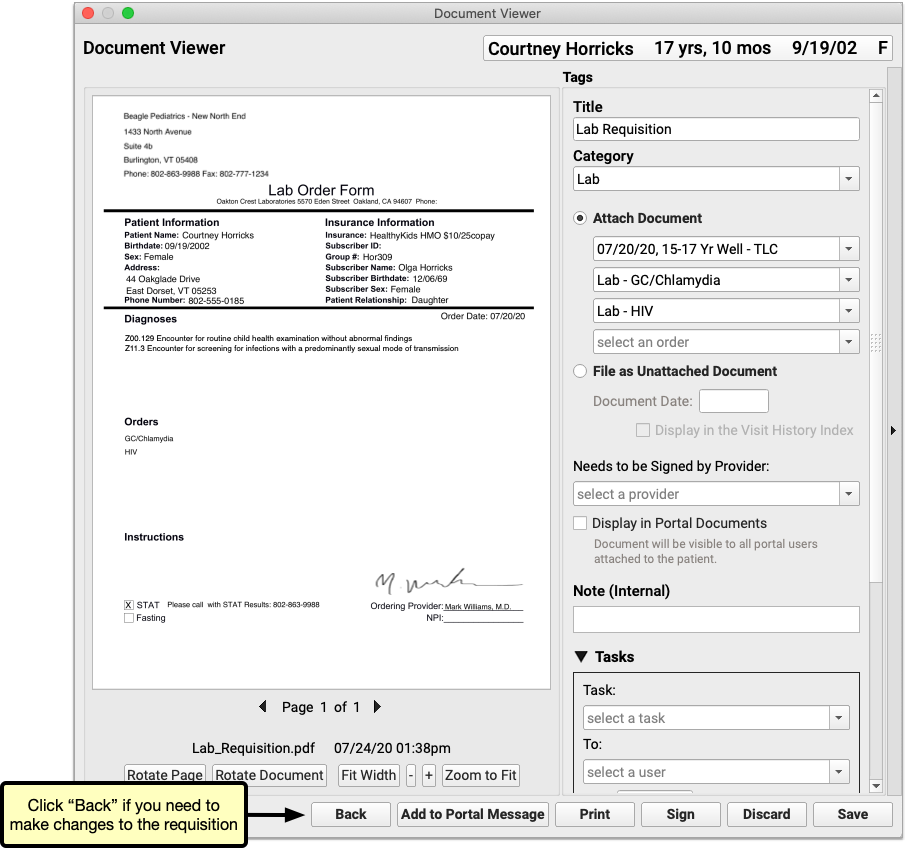
If you need to make changes before saving, printing, or sharing the requisition, click the “Back” button.
Save, Print, and Share Requisitions
Once you generate a requisition, you can edit and manage it like any other document in PCC EHR.
Review and Edit the Document Details
After you generate a requisition, it opens in a Document Viewer window, where you can review and optionally edit its attributes.
Depending upon the type of requisition, the document title defaults to either “Lab Requisition” or “Radiology Requisition”, and the document category defaults to either “Lab” or “Radiology”.
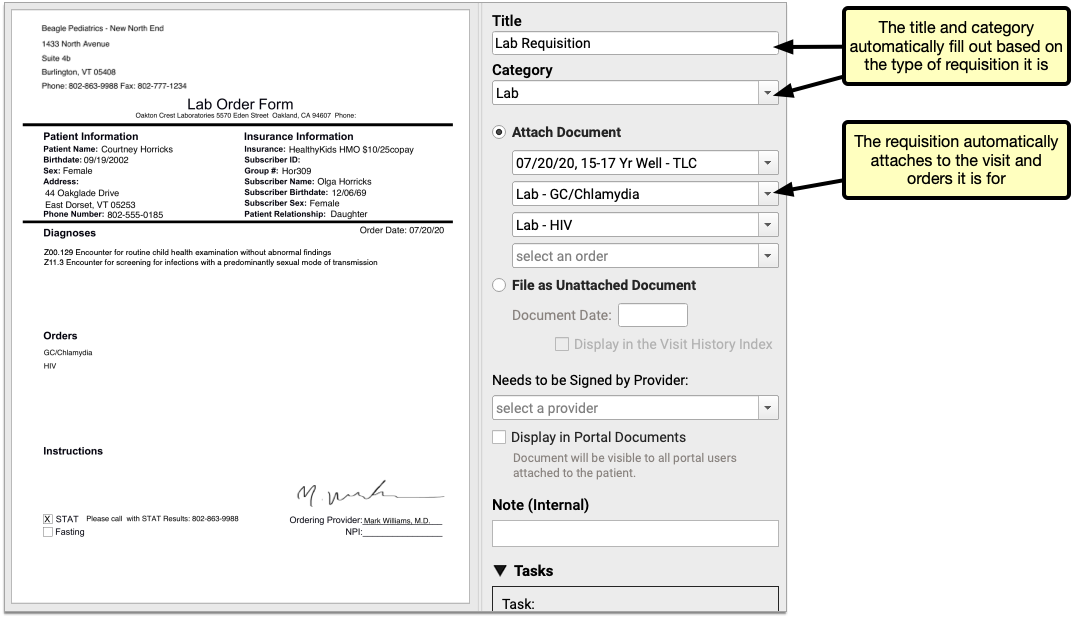
Requisitions get linked by default to the visits from which they originate. They are further linked to whichever orders are on the form.
Create Tasks
Optionally select a task and assign it to a user. You can also include a note and a due date.
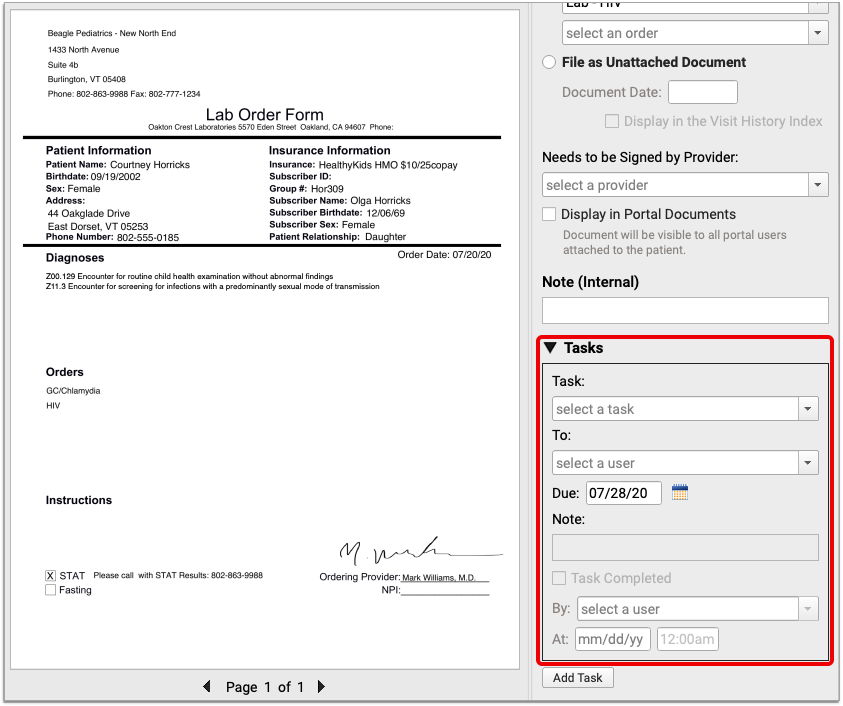
You can use document tasks to inform users at your practice that there are steps to take with the requisition. When the task is done, the assigned user can mark the task complete and create subsequent tasks if needed.
Call PCC Support to Add More Task Options: You might find that you need to add more options to the list of document tasks in PCC EHR. Contact PCC Support for help adding new task types.
Print and Share the Requisition
There are multiple ways to share requisitions with patients and the lab.
You can print out a physical copy and hand it to the patient or fax it to the lab. You can also share a digital copy of the requisition with the patient.
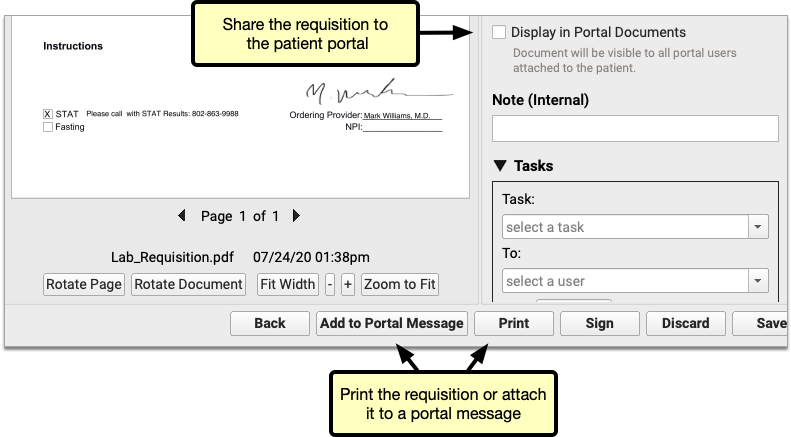
Click “Print” to generate a hard copy of the requisition or check “Display in Portal Documents” to add a digital copy to the patient’s portal documents.
Optionally click “Add to Portal Message” to send the requisition as a portal message attachment.
Save the Requisition
Click the “Save” button to save your settings, close the window, and file the requisition in the Documents section of the patient’s chart.
If you don’t want to save the document, you can click the “Discard” button instead.
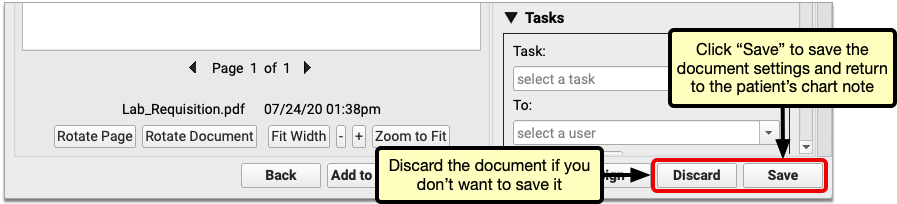
Configure In-Office Lab Orders and Facilities
In-office lab facilities and orders are automatically excluded from outbound lab requisitions in PCC EHR. You can configure in-office lab facilities and orders in the Lab Configuration tool in PCC EHR.
Configure In-Office Lab Facilities
Open Lab Configuration from the Configuration menu in PCC EHR. Click the Lab Facilities tab.
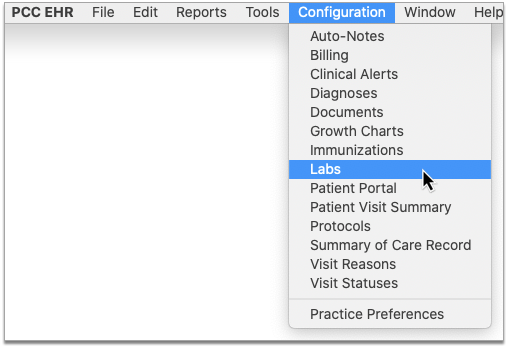
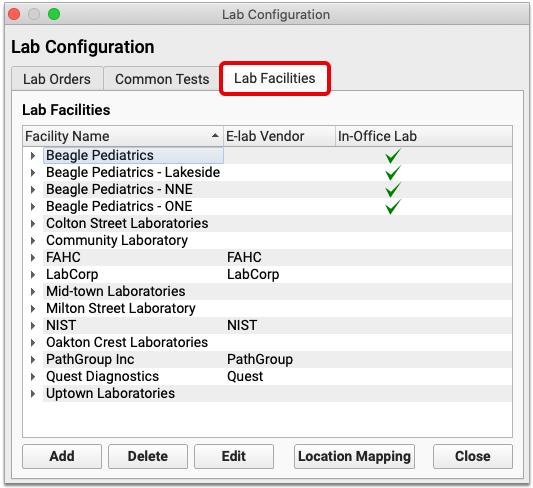
A green check appears in the In-Office column beside lab facilities which are considered to be internal to your practice.
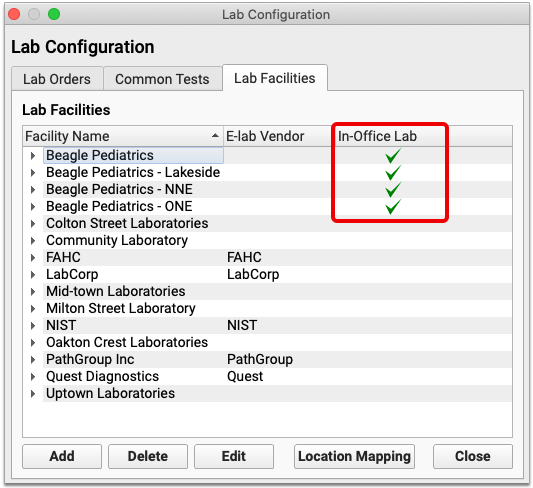
You can edit a facility by double-clicking it, or selecting it and clicking the “Edit” button. Check or uncheck the “In-Office” box within the lab facility settings, then click “Save”.
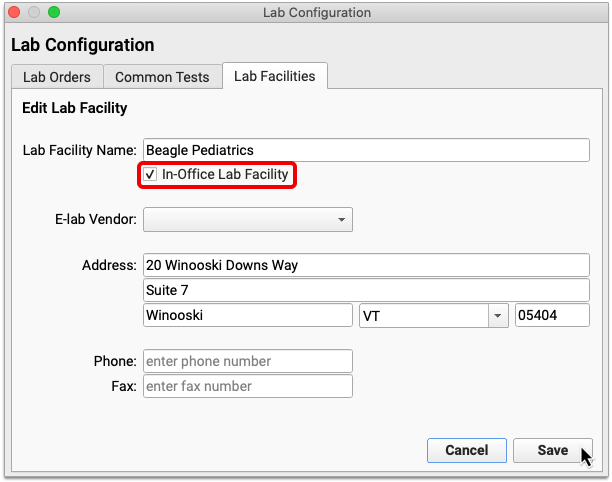
Once you have configured all of your in-office facilities, map them to your appointment locations.
Map In-Office Lab Facilities to Appointment Locations
Within the Lab Facilities tab, click the “Location Mapping” button. Map each of your appointment locations to an in-office lab facility.
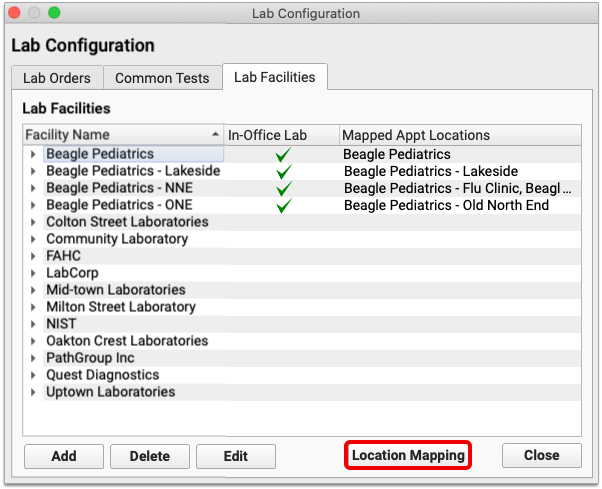
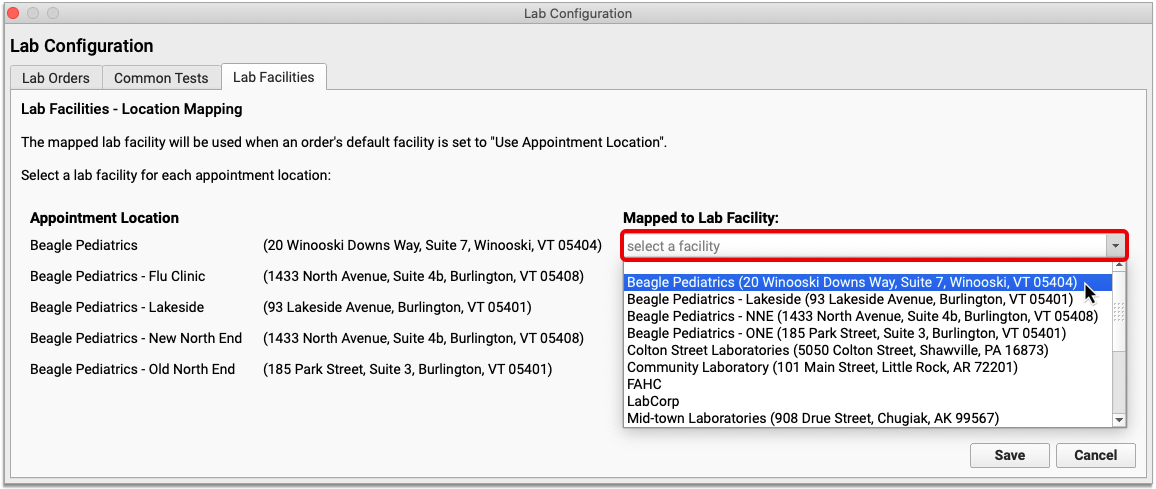
Once all appointment locations are mapped to a lab facility, click “Save”.
Next, check that the lab tests you conduct internally default to using whichever lab facility is linked to the location of the appointment.
Configure a Default Facility for In-Office Lab Tests
Click the Lab Orders tab. If all of your in-office lab orders follow a similar naming convention, use the search box to narrow down the list.
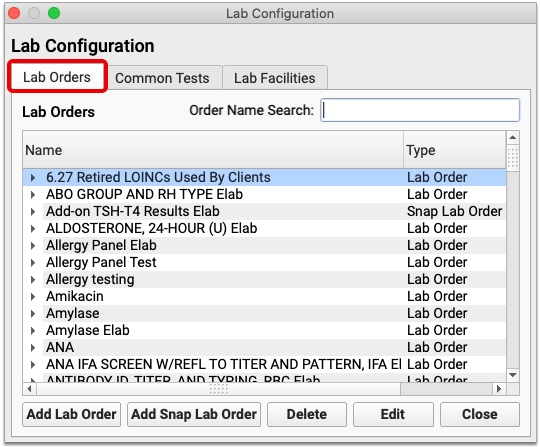
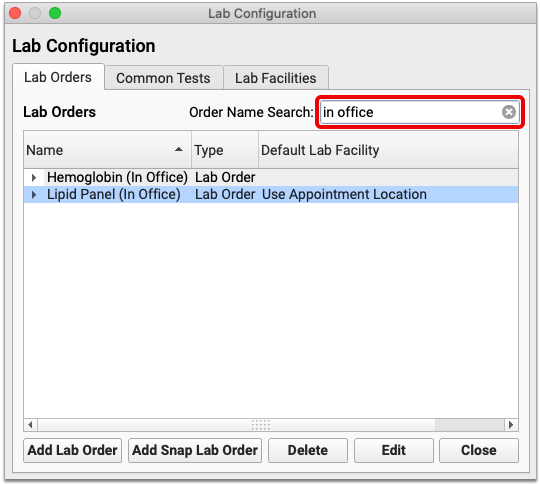
Check that “Use Appointment Location” appears in the Default Lab Facility column beside each in-office lab order.
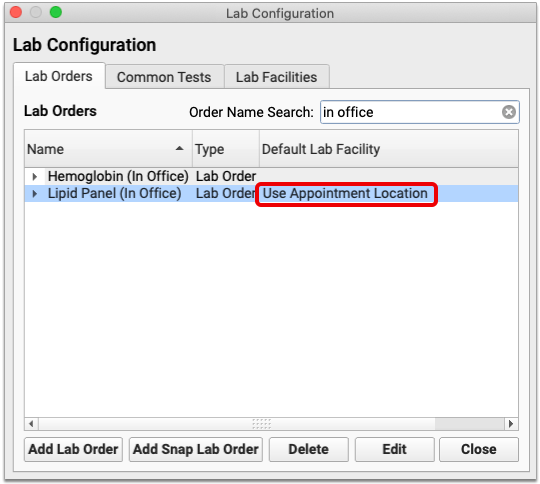
If you need to edit an order’s default lab facility, double-click it, or select it and click the “Edit” button.
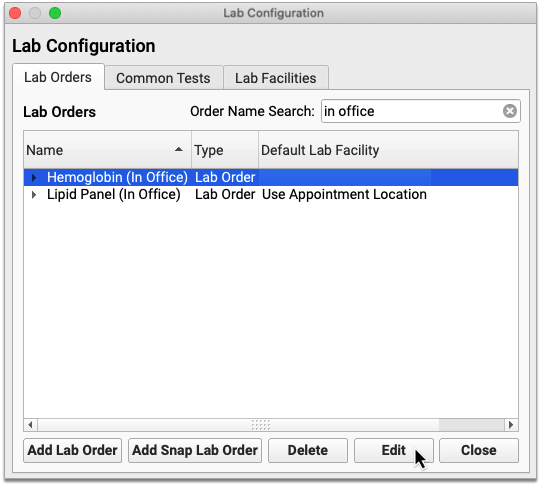
Set the Default Lab Facility field to “Use Appointment Location”, then click “Save”.
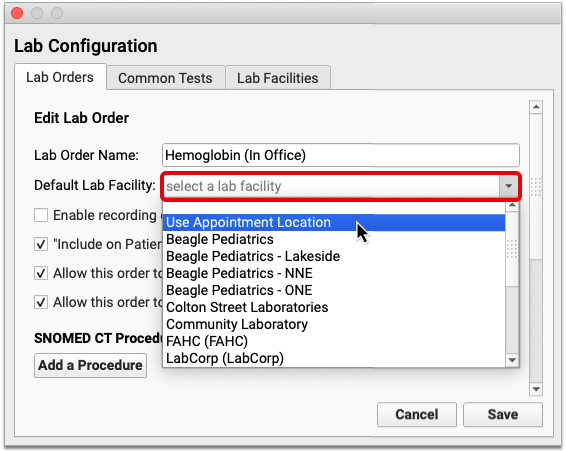
Lab orders which use the appointment location as their default lab facility are prevented from appearing on outbound lab requisitions, provided the appointment location is mapped to an in-office lab facility.
To learn more about how to set up lab orders and facilities, read all about Lab Configuration.
Lab Configuration Changes Take Effect the Next Time Users Log In to PCC EHR: The changes you make to in-office lab facilities and orders will not take effect for users until the next time they log in to PCC EHR.
Set Up Default Document Categories for Lab and Radiology Requisitions
By default, PCC EHR saves lab requisitions in the “Lab” document category, and radiology requisitions in the “Radiology” document category. You can change these defaults in the Document Configuration tool.
Open Document Configuration tool from the Configuration menu in PCC EHR. Click the “Assigned Categories” tab.
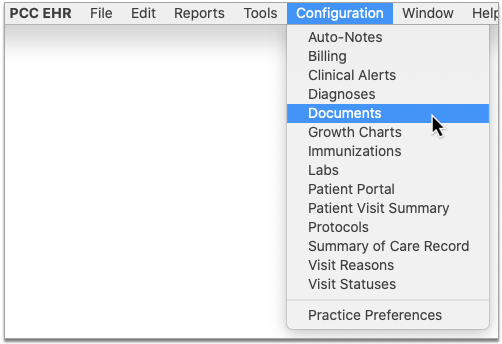
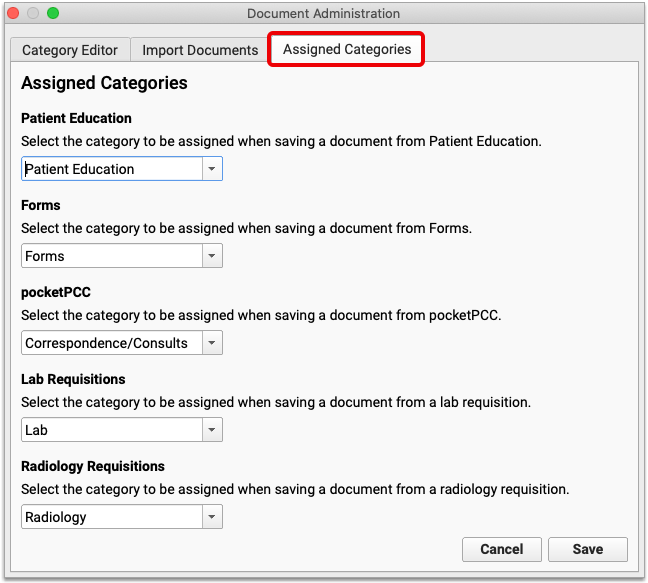
Use the drop-down lists under the Lab Requisition and Radiology Requisition headers to select the document categories where lab and radiology requisitions should be saved by default.
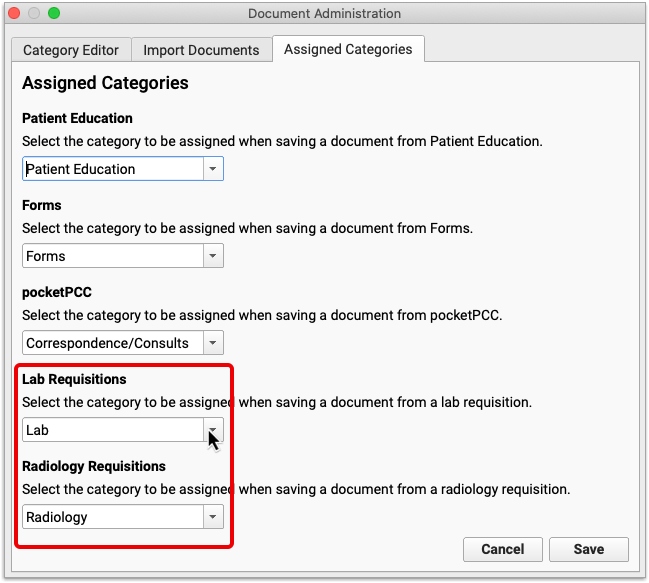
Click “Save” to save your changes.
Configure Provider Signatures to Automatically Appear on Lab and Radiology Requisitions
You can configure lab and radiology requisitions to generate with the signature of the ordering provider. Contact PCC Support for help adding signatures to lab and radiology requisitions.
Configure Custom Requisition Forms
PCC provides a stock lab and radiology requisition template to all practices, but offers the option to upload custom requisition form templates by special request. Please note that PCC cannot configure custom lab and radiology requisition forms containing checkboxes at this time.
Contact PCC Support to learn more about custom requisition form requirements, and to get help adding custom requisitions to your system.
Learn More
To learn more about how to use orders within the patient chart, read Order a Lab, Procedure, Supply, or Other Order. Practice administrators can also learn more about Lab Configuration in PCC EHR.
Securely Retrieve Clinical Documents from Hospitals and Other Providers
Watch a Video: Watch Clinical Document Exchange: The Initiator Role to learn how to configure your PCC system to submit requests and retrieve clinical documents.
Initiate a Query for Patient Records
If a new patient transfers to your practice, or if you know that an existing patient has received care at another healthcare facility, you can request and retrieve their records on demand within PCC EHR.
Open the patient’s chart and navigate to the History component. Click on “Find Clinical Documents”.
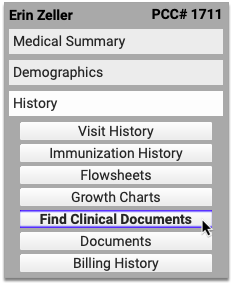
If the patient has default organizations configured, PCC EHR immediately begins querying them for records.
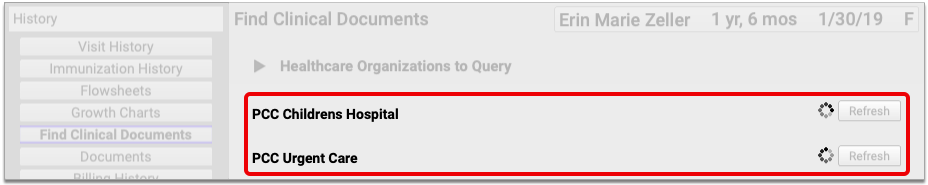
If the patient does not have default organizations configured, or you want to query organizations which are not part of the patient’s defaults, click the triangle beside the Healthcare Organizations to Query header.
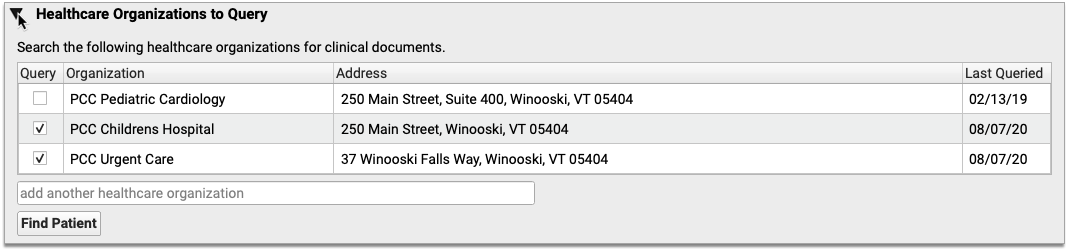
The triangle reveals a list of healthcare organizations that your office has historically queried for the patient. Check marks appear beside the patient’s default organizations.
To query an organization that is on the patient’s list but is not a default, check the box beside it and click the “Find Patient” button.
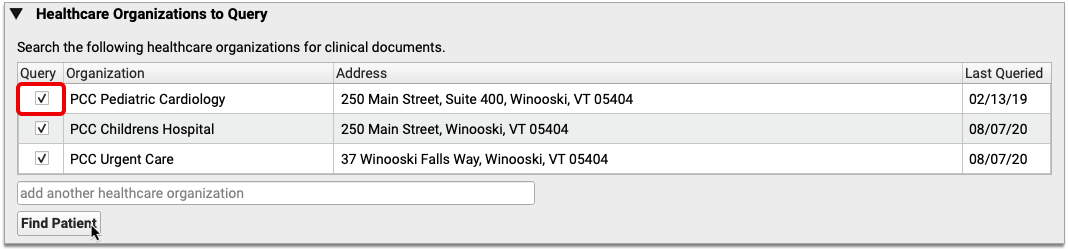
If you want to query an organization that is not on the patient’s list, search for it by name or address and add it to the patient’s list.
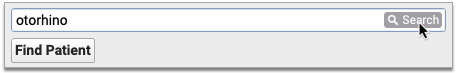
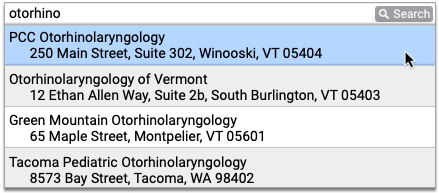
Search Results Only Show Organizations You Can Query: Search results include healthcare organizations that both match your search terms and have adopted the Carequality interoperability framework.
After you add the new organization to the patient’s list, click the “Find Patient” button.
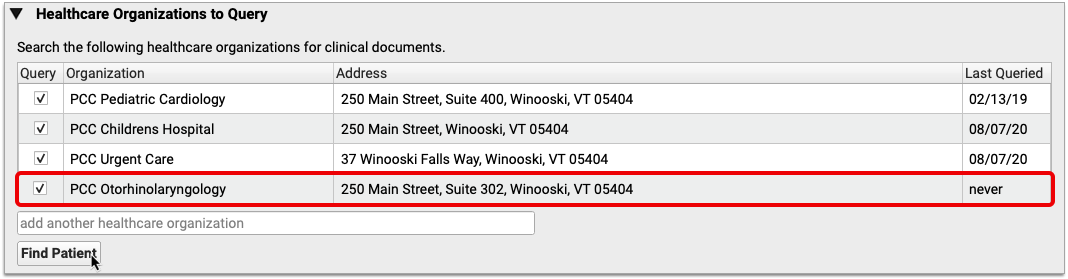
The “Find Patient” button initiates a query to all of the selected organizations for patients whose name, date of birth, and sex match yours. Each organization returns patient match results in its own table.
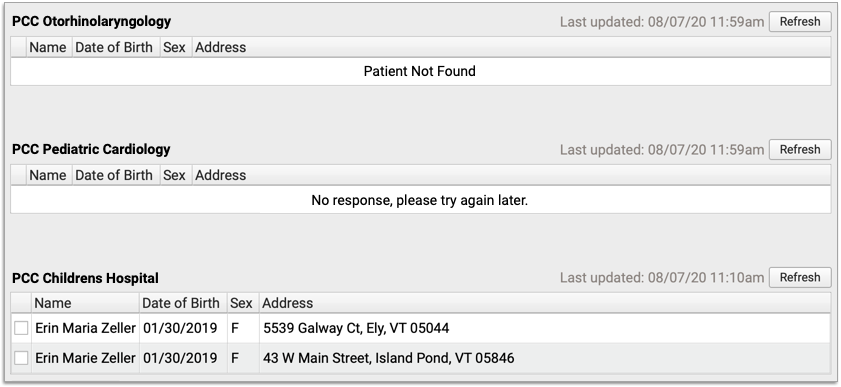
Patient Not Found: If an organization does not have any records that match your patient’s demographic criteria, the query will return a message that says “Patient Not Found”. If the request times out, you will receive a message that says “No response, please try again later.”
Select your patient from the query results, then click “Find Documents”.
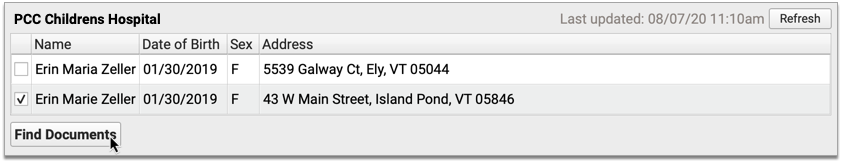
Found documents display in a table beneath the organization and patient they are associated with.
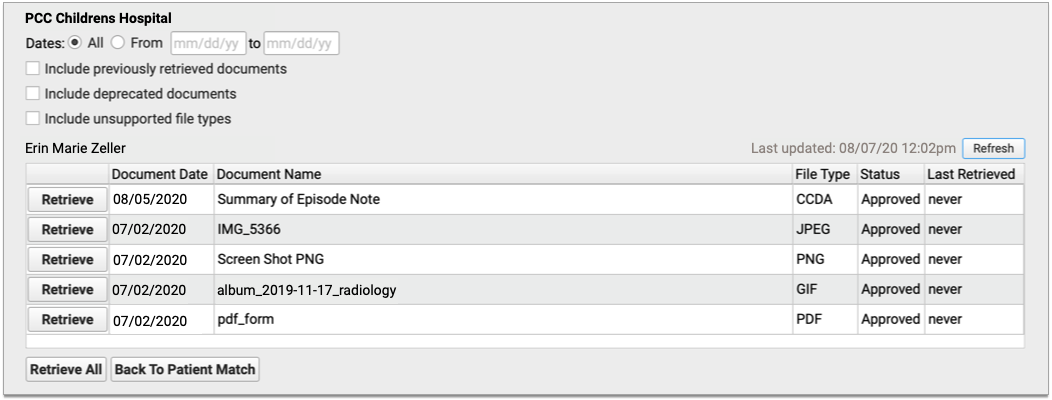
You can filter the list of found documents by date. You can also expand the results to include previously retrieved documents, deprecated documents, and documents are of an unsupported file type.
Deprecated Documents and Unsupported File Types: Deprecated documents are flagged by the source organization for being out of date. Unsupported file types are documents that cannot be retrieved and imported into PCC EHR due to their file format.
If you want to run the query again, click the “Refresh” button in the top-right corner of the results table. The time stamp in the top-right corner of each table shows the last time a query was performed.
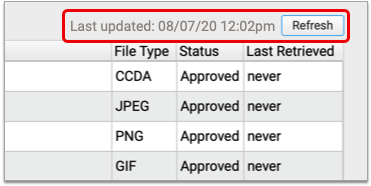
Query Results Remain Visible All Day: Clinical document queries persist on the Find Clinical Documents screen until 11:59 p.m. and can be seen and refreshed by all users who have query permissions. After midnight, the Find Clinical Documents screen clears its queries, leaving a blank slate for users who access it the next day.
View and Manage Retrieved Documents
Once you have determined that there is a document for your patient at a queried healthcare organization, you will need to import it in order to view its contents and save it to PCC EHR.
Click the “Retrieve” button beside the document you wish to import. If there are multiple documents and you want to import all of them, you can click the “Retrieve All” button beneath the table.
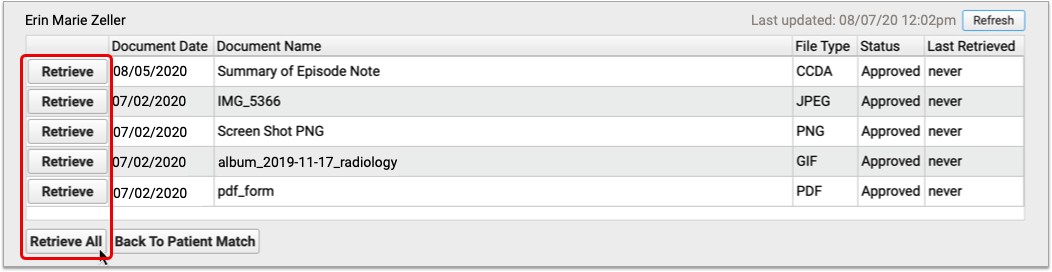
Wrong Patient? Try Again: If you realize at this point that you have requested documents for the wrong patient, you can cancel your search by clicking the “Back to Patient Match” button beneath the table.
Once you retrieve documents, the “Retrieve” button is replaced by “View” and “Reconcile” buttons. The “View” button appears for all document types. The “Reconcile” button only appears for CCDA documents.
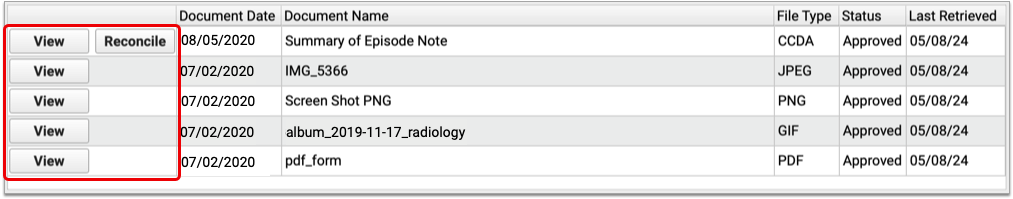
You can open a retrieved document by clicking the “View” button.
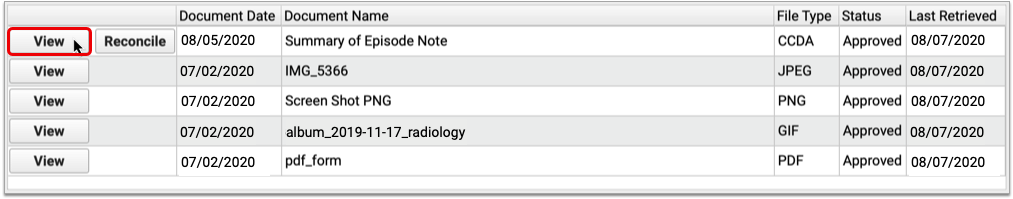
Once open in a Document Viewer window, you can see the document’s contents and other information about it, such as its title and source, the date it was last modified, and the name of the document category under which it is saved in the patient’s chart in PCC EHR. Retrieved documents are always saved into the Retrieved Documents category when you first import them.
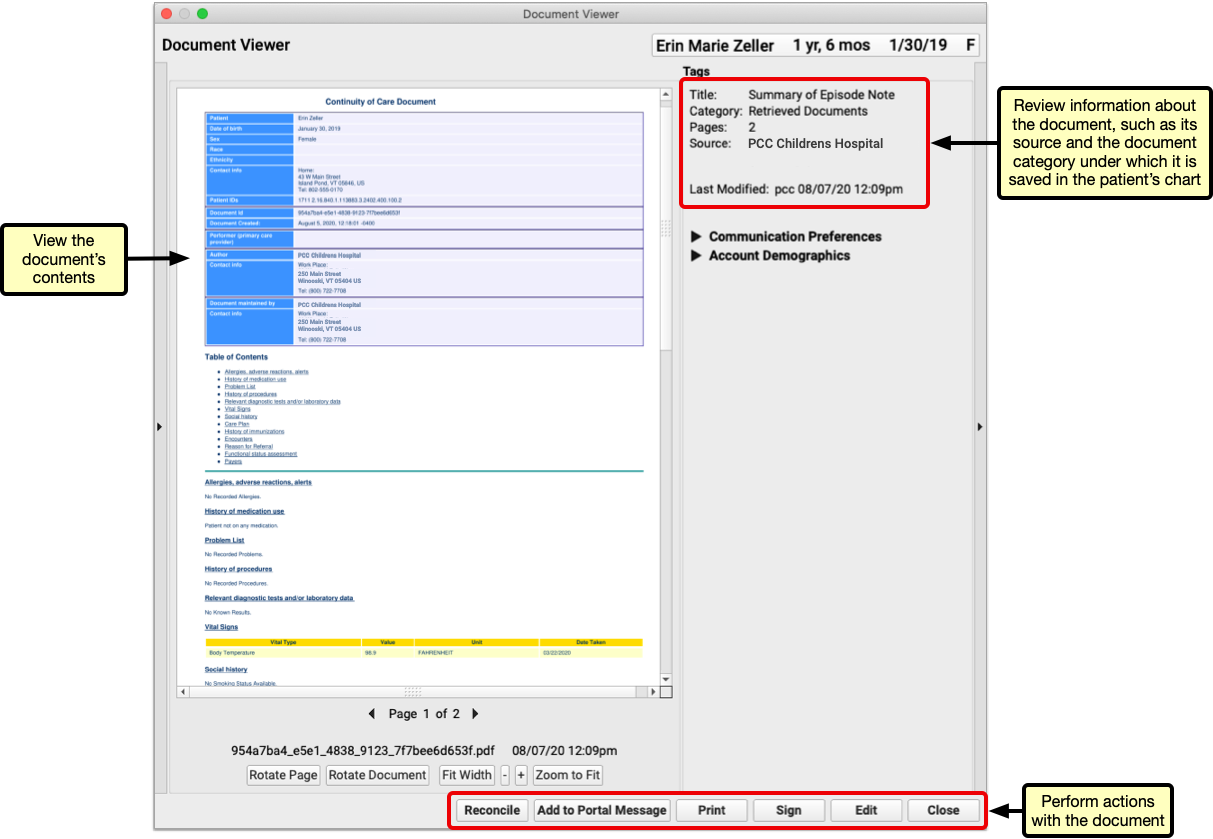
Click the “Edit” button to modify the document’s title, re-assign it to a different category, attach it to a visit, send it to a provider for signing, share it to the patient portal, attach it to a portal message, annotate it, or create messaging tasks from it.

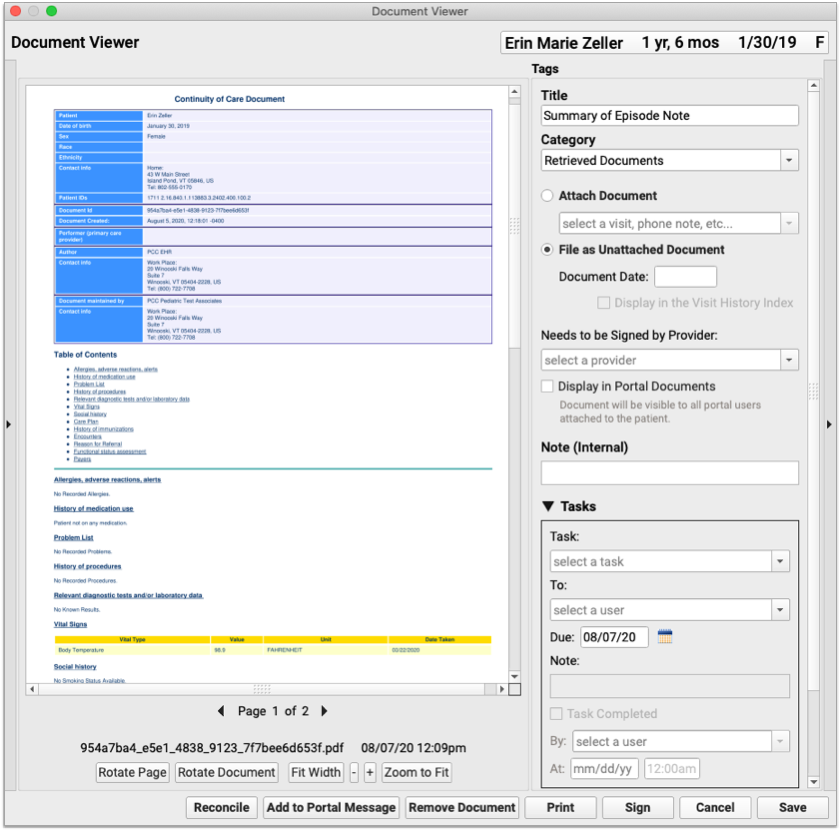
You can remove the document from the patient’s chart by clicking the “Remove Document” button.
Removed Documents Get Deleted Altogether from PCC EHR: Unlike other kinds of documents in PCC EHR which return to the Import Documents screen when you remove them from the patient’s chart, clinical documents retrieved from other healthcare organizations are deleted from your PCC system altogether when you click the “Remove Document” button. Documents deleted in error can usually be retrieved anew from the source organization, as long as the source organization has not deleted them.
You can find and edit retrieved documents anytime in the Documents section of the patient’s chart.
Reconcile Retrieved Documents
You can import Problems, Medication Allergies, and Medications from retrieved documents into your patient’s chart in PCC EHR.
If you already have a retrieved document open in a Document Viewer window, click the “Reconcile” button to review and import its data.
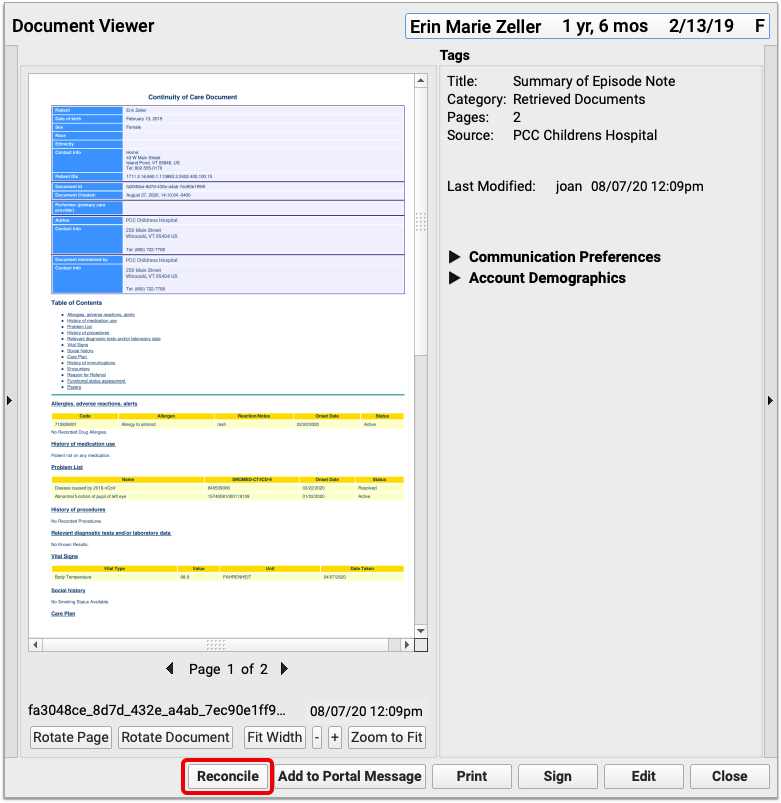
You can also begin reconciling a document from the Find Clinical Documents screen within the History section of the patient’s chart, provided the document was retrieved the same day you are reconciling its contents.
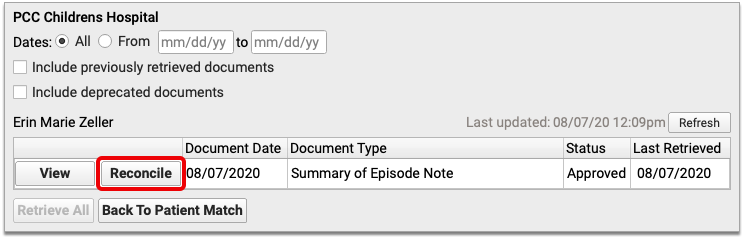
The reconciliation window compares the Problems, Medication Allergies, and Medications in the retrieved document to those already in your patient’s chart. You can select which items, if any, you wish to import from the retrieved document.
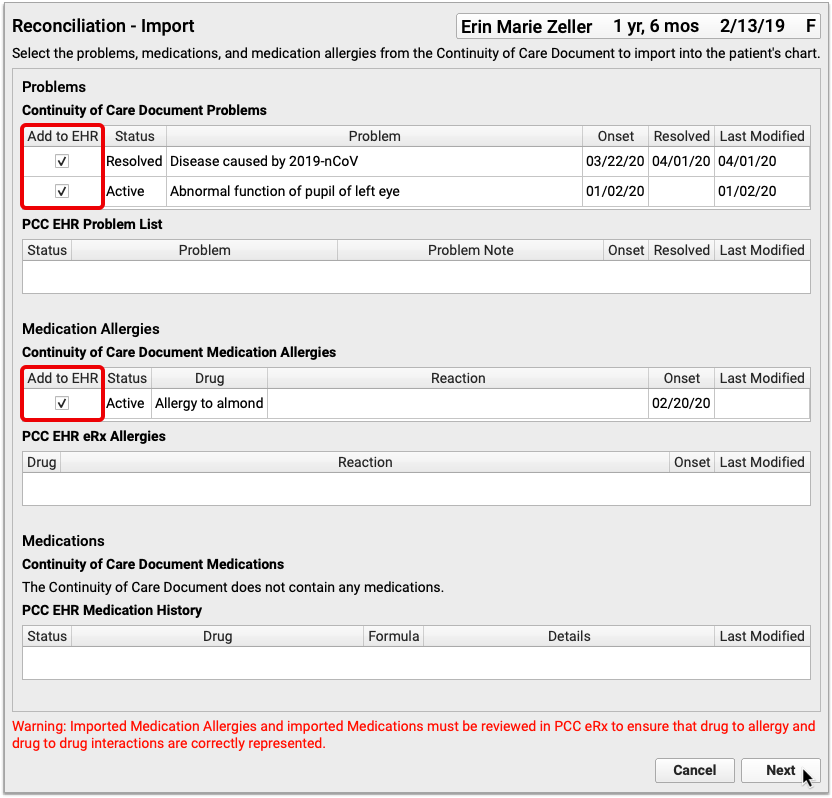
Once you have selected all of the items you wish to import, click the “Next” button.
Review your changes. If you notice duplicate or outdated information in the preview, click “Edit” to make corrections.
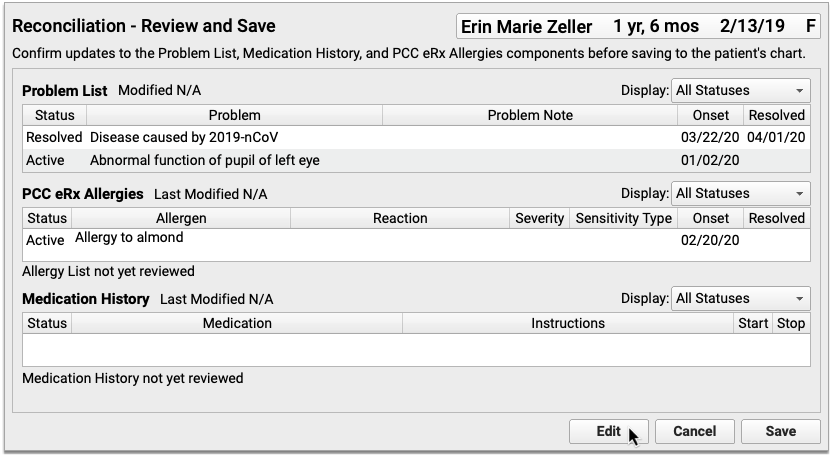
The corrections you make in this window will be reflected in the patient’s chart once you complete the reconciliation.
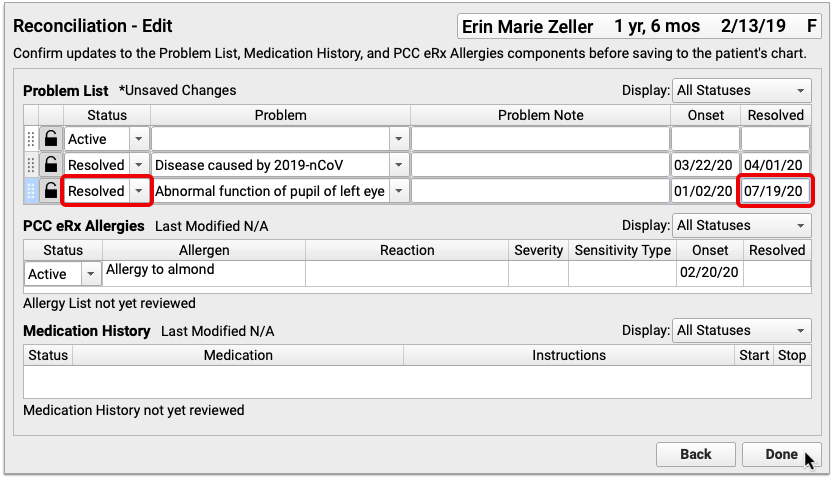
When you have finished making corrections, click “Done” to exit the editor. Then, click “Save” to finish reconciling the retrieved document.
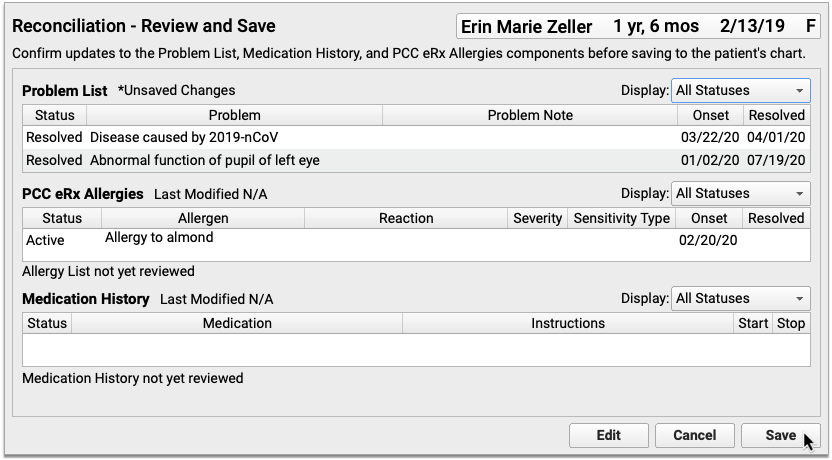
The patient’s Problem List, PCC eRx Allergies, and Medication History in PCC EHR will reflect the choices you made while reconciling the retrieved document.
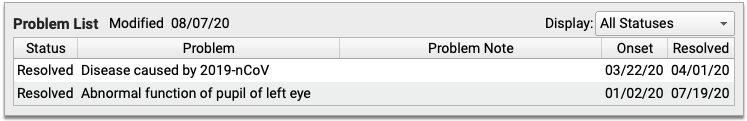
Reconciled documents include a “Last Reconciled” date and user stamp.
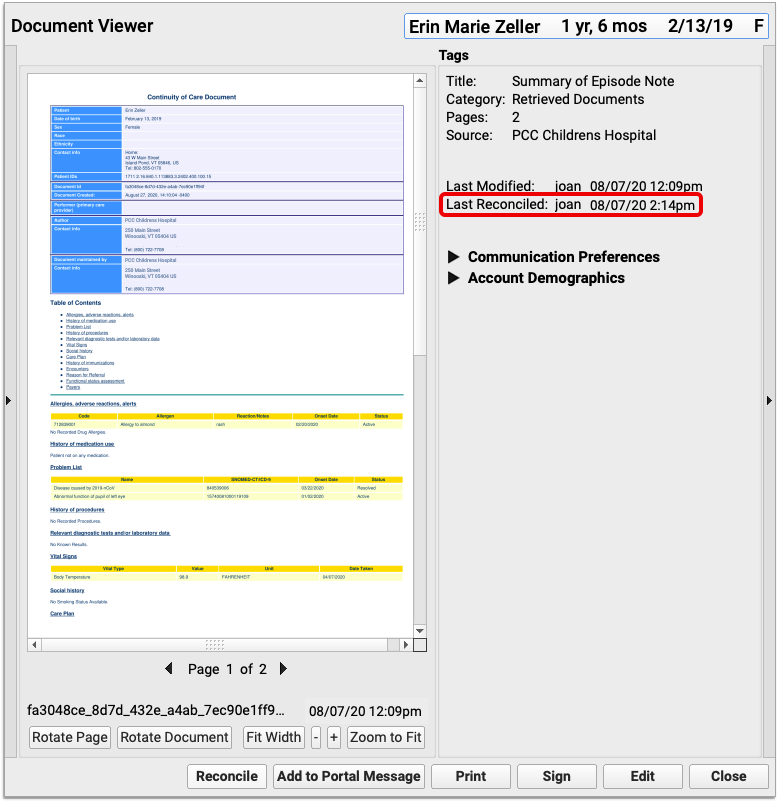
You can reconcile documents as many times as you need. The “Last Reconciled” date and user stamp updates each time a document is reconciled.
Manage Default Healthcare Organizations
You can set up default healthcare organizations for just one patient and for all patients at your practice.
Set Up Default Organizations for One Patient
You can manage a patient’s default healthcare organizations within the Find Clinical Documents section of their chart in PCC EHR.
On the Find Clinical Documents screen, click the triangle beside the Healthcare Organizations to Query header.
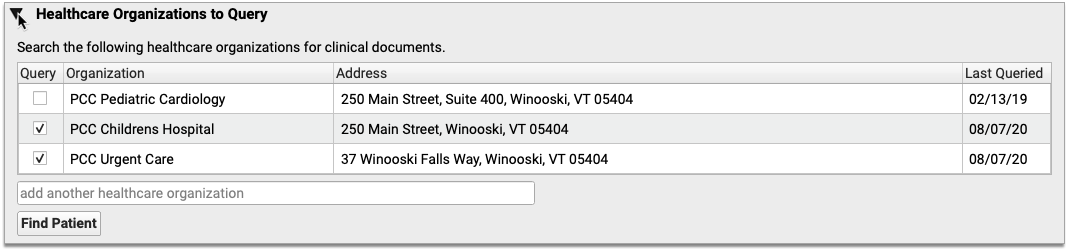
The triangle reveals organizations which have historically been queried for this patient.
Place a check mark beside organizations that should be queried by default for the patient, and uncheck those that should not.
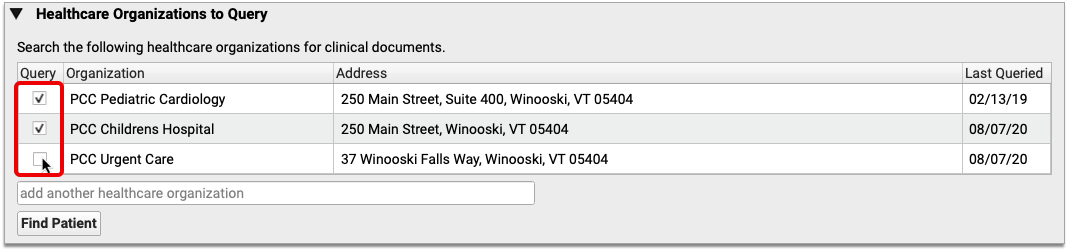
You can add more organizations to the list using the “add another healthcare organization” search field.
As soon as you place a check mark beside an organization, it is considered a default for this patient. Default organizations are automatically queried when users open the Find Clinical Documents section of the patient’s chart.
Set Up Default Organizations for All Patients
If your practice frequently request records from a local hospital or urgent care clinic, and that organization has adopted the Carequality interoperability framework, you can set it up as a default healthcare organization to query for all of your patients.
Click on the PCC EHR Configuration menu and select “Clinical Document Exchange”.
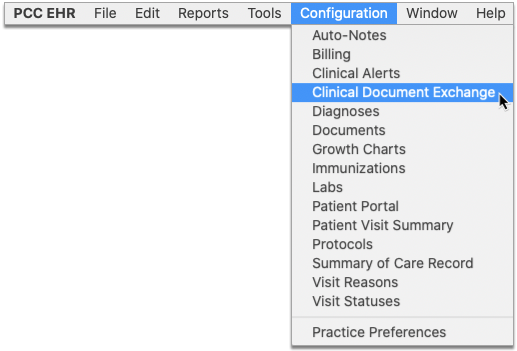
Use the search field to find a healthcare organization that you regularly request patient records from.
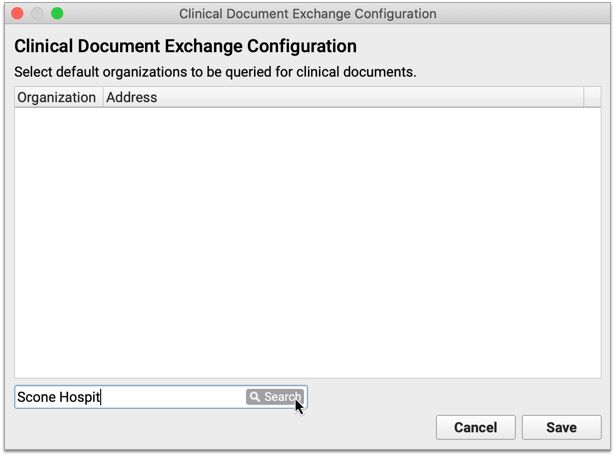
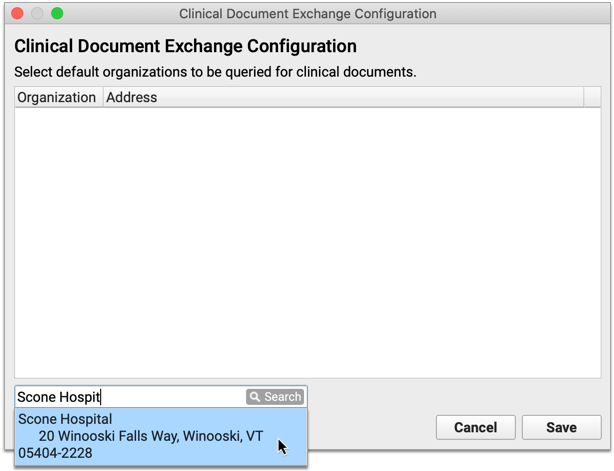
The search results include healthcare organizations that both match your search terms and have adopted the Carequality interoperability framework. Select an organization from the search results to add it to the list of healthcare organizations that should be queried by default for all patients.
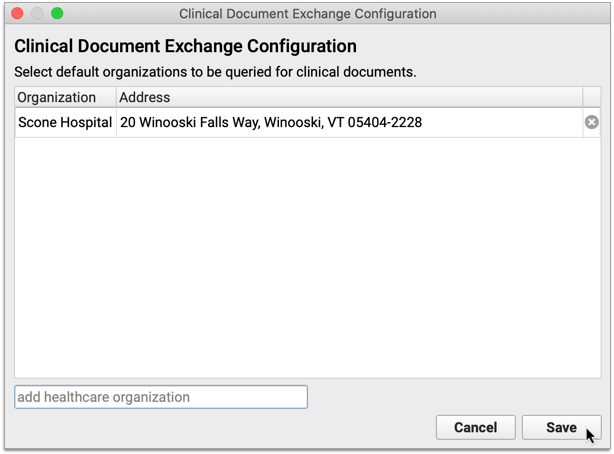
Repeat this process for as many organizations as you want to query by default for all patients. Click “Save” to save the configuration and close the window.
If an organization is no longer active with the Carequality network, an Inactive icon (red triangle with exclamation point) appears beside it in the Clinical Document Exchange configuration window.
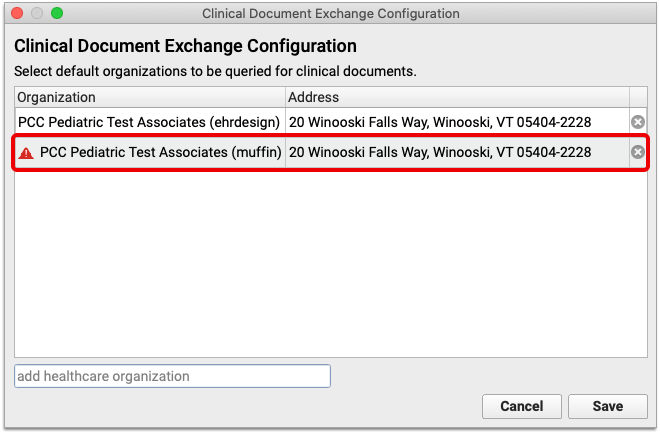
Inactive organizations are automatically hidden from patient charts, but they remain in the Clinical Document Exchange configuration list until you manually remove them by clicking the “x”.
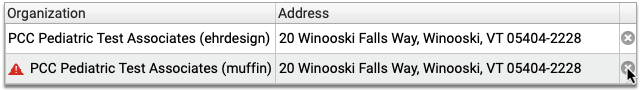
Note: Sometimes organizations are marked inactive in the Carequality directory as the result of a name change or a change in ownership. Search for the new name of the organization to re-add it to your list of default organizations to query.
User Permissions
Allow Users to Retrieve Clinical Documents
Users require special permissions in order to query other healthcare organizations for patients’ clinical documents. Permissions are assigned on a per-user basis in PCC EHR.
Open User Administration from the Tools menu in PCC EHR.
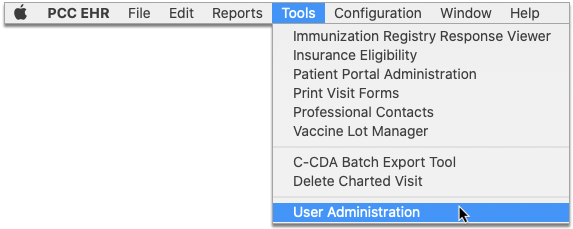
Select a user from the list and click the “Edit” button.
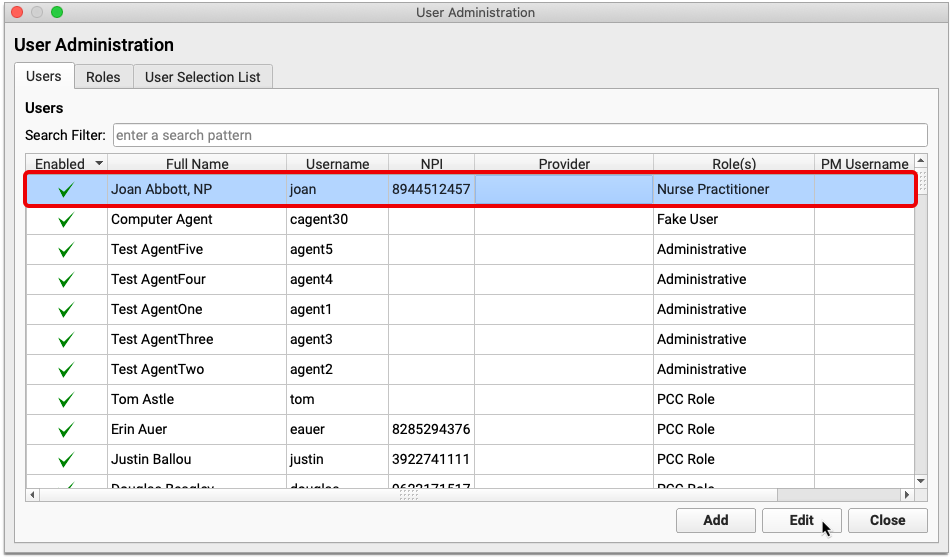
Under the “Clinical Document Exchange” header, check the box labeled “This user is allowed to query for clinical documents.”

Select a role for the user. The list of roles is defined by the Carequality interoperability framework and cannot be modified. Each user at your practice may only be assigned one role. Role assignment is required.
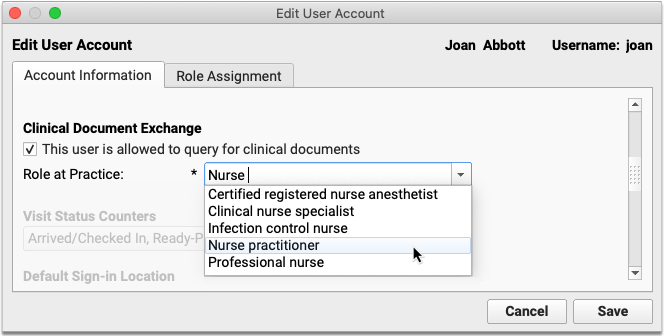
Once you have assigned permissions and a role to the user, click the “Save” button.
Repeat this process for all users at your practice who need to be able to query other healthcare organizations for patients’ clinical documents.
Users with Clinical Document Exchange permissions are able to see the “Find Clinical Documents” button within the History section of patient charts. The “Find Clinical Documents” button is hidden from users who do not have Clinical Document Exchange permissions.
Allow Users to Manage Practice-Wide Clinical Document Exchange Settings
Some users at your practice will require special permissions in order to manage your practice’s default healthcare organizations to query. These permissions are assigned on a per-role basis in PCC EHR.
Open User Administration from the Tools menu in PCC EHR.
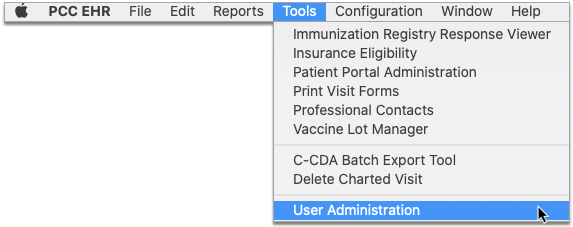
Click the “Roles” tab at the top of the window.
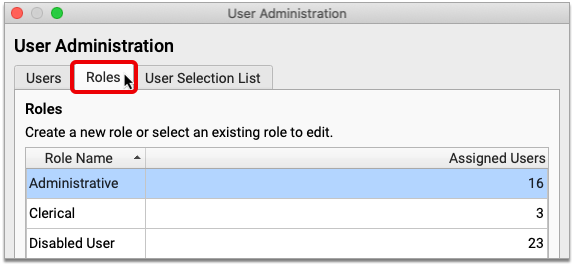
Select an existing role and click the “Edit Role” button.
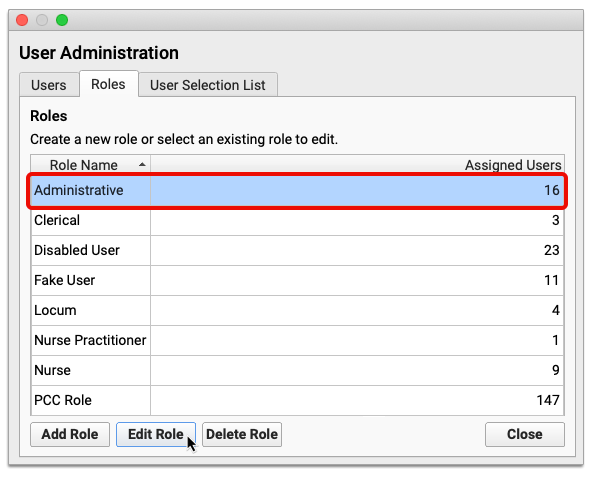
Check the box for “Clinical Document Exchange Configuration”, then click “Save”.
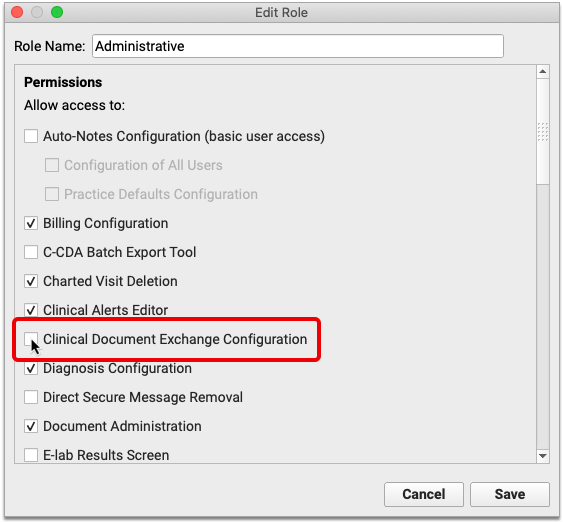
If you would rather create a new role to manage Clinical Document Exchange Configuration permissions, click “Add Role” instead of editing an existing one.
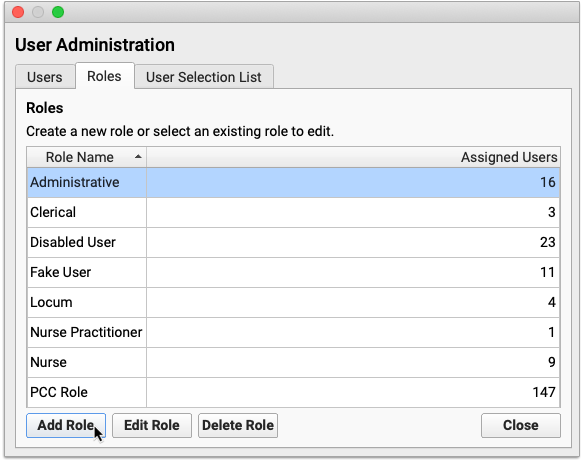
Name the role, check “Clinical Document Exchange Configuration”, then click the “Save” button.
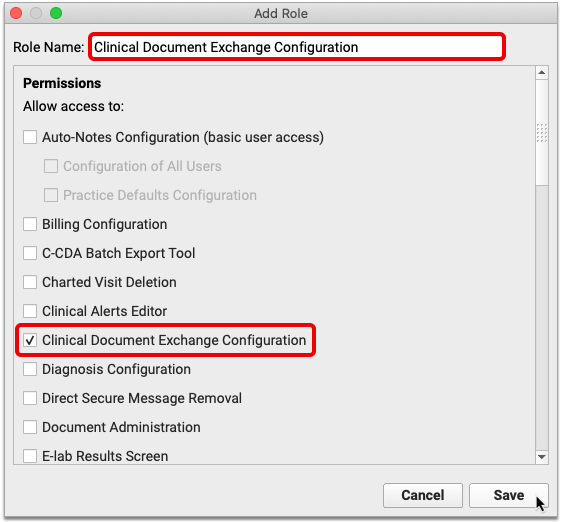
Assign the new role to relevant users in PCC EHR.
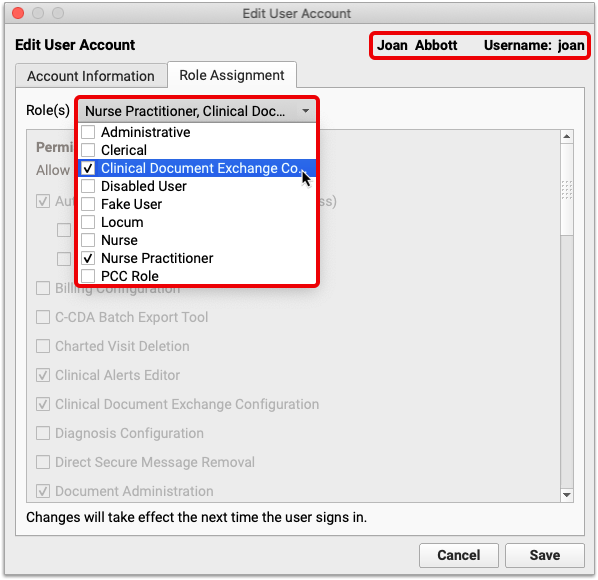
Users with Clinical Document Exchange Configuration permissions are able to manage your practice’s default healthcare organizations to query.
Close User Administration when you have finished assigning permissions. The new permissions will take effect the next time users log in to PCC EHR.
Sign Notes, Visits, and Documents in pocketPCC
PocketPCC includes the option to sign visits, phone notes, and documents, so you can complete your signing tasks conveniently, from anywhere.
Sign in to PocketPCC from your phone or other mobile device. If your PCC EHR user account has permission to sign, even with a co-signer, you’ll have the option to sign under pocketPCC’s menu.
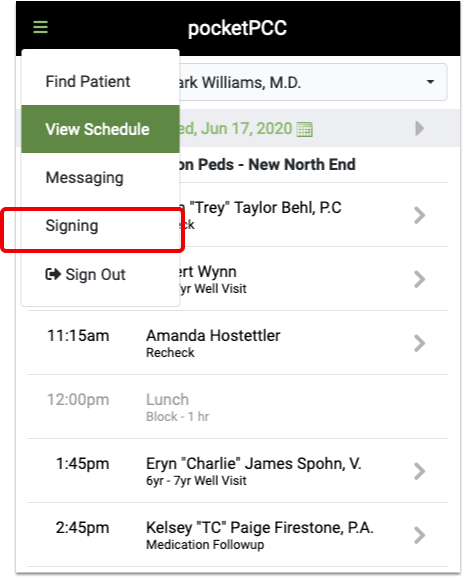
The signing window lists all items in the signing queue. Green checks indicate the item has been signed, and the orange icon indicates that a co-signer is needed.
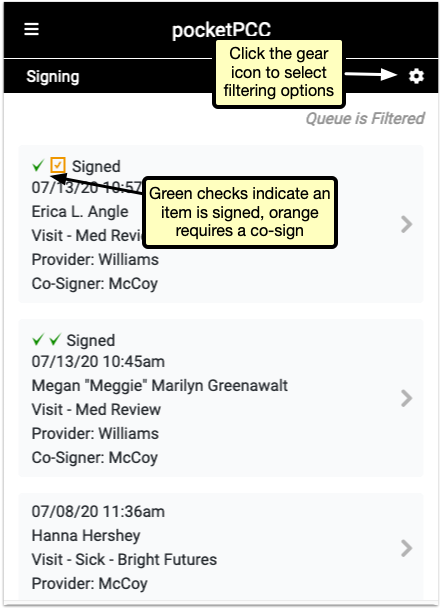
Click the gear icon in the upper right to open the filter options. You can limit by the type of item, the current signed status, or by provider. Select filters and click “Done” to refresh the list to match your selection.
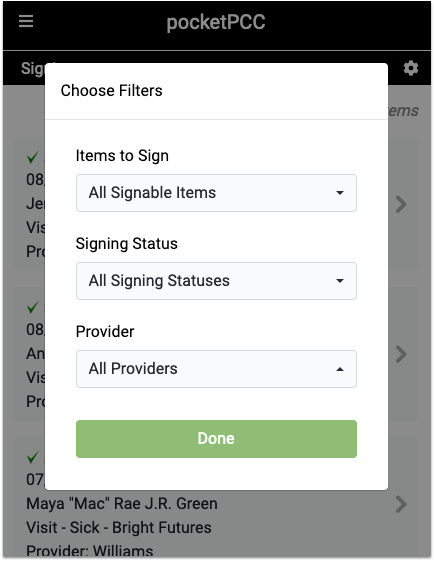
Select a signable item to open the visit, note, or document for you to review. At the bottom of the window, after you’ve reviewed the item, you can sign or co-sign with a single click.
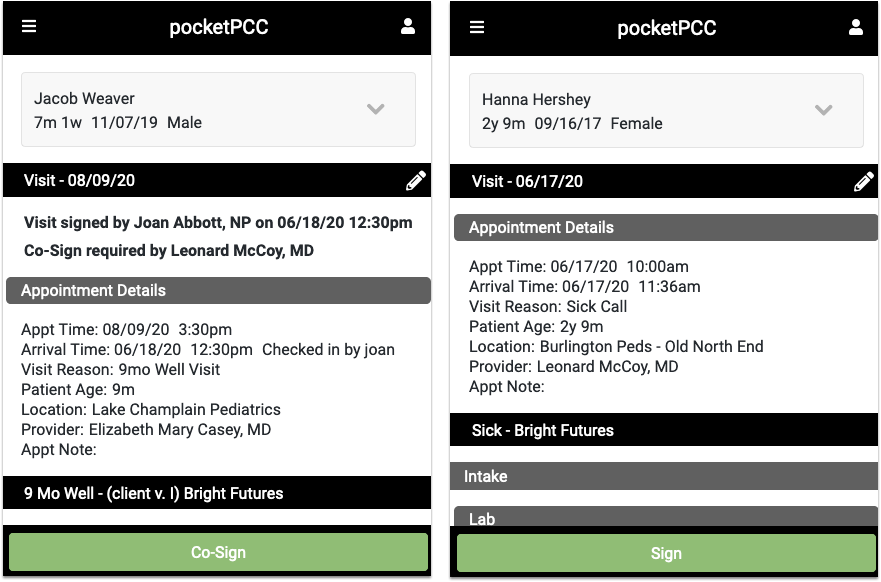
While reviewing a visit, document, or phone note, you can click any of the edit buttons and make additional notes, assign tasks, or any other edit to the item. Then, you’ll have the option to simply save your changes, or both save and sign the item in one click by selecting “Save & Sign”.
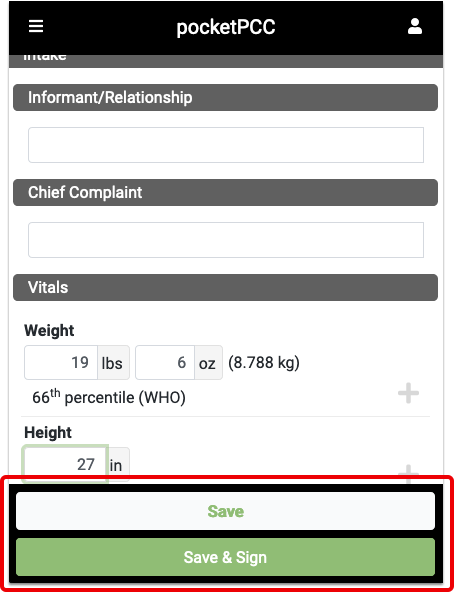
When you’ve saved, or saved and signed, you’ll be returned to the signing queue, where you can select another item to sign.
Best Practices for Pediatrics in the COVID-19 Era
Pediatric practices around the country can continue to see patients, provide great care, and thrive as businesses during and following the COVID-19 pandemic.
PCC worked with practice managers and managing providers to develop this library of recommendations.
Recall Patients
PCC recommends that all practices launch a patient recall initiative. During the initial months of the COVID-19 pandemic, many practices experienced lower visit volume. Children’s developmental needs and other health concerns (diabetes, asthma, depression, and more) did not slow down, and this created an unmet need.
Consider contacting all families who have visited your practice in the past three years and schedule them for telemedicine or in-person appointments. Get your patients caught up on well visits, screenings, shots, and chronic problem and care plan management. As you provide much needed care, you will also be maintaining your practice’s relationships and your ability to help your community.
Read Why and How Pediatric Practices Should Launch a Recall Initiative Today to learn more.
Adjust How You Schedule Patients
When PCC spoke with pediatric practices, they shared changes they’ve made to patient scheduling during the COVID-19 era.
Implement the PCC EHR Appointment Book
The Appointment Book has built in Telemedicine features and can be configured with visit templates to help your schedulers. The close integration between the Appointment Book and the patient’s chart record make everything easier, from connecting to patients, to charting, to billing.
If your practice is not using the PCC EHR Appointment Book, PCC Support can help you get started.
Maximize Portal Communication
Contact your families and make sure they all have patient portal access. This will allow their initial contact with your practice to be asynchronous, which means your staff and clinicians can followup on questions and concerns whenever they are available.
By improving this initial point of contact, you can more efficiently triage issues and schedule appointments as needed.
Implement Appointment Requests in the Patient Portal
Your practice can create a patient portal template for appointment requests. Then, when the family wants an appointment, they can pick “Appointment Request” when they create a portal message.
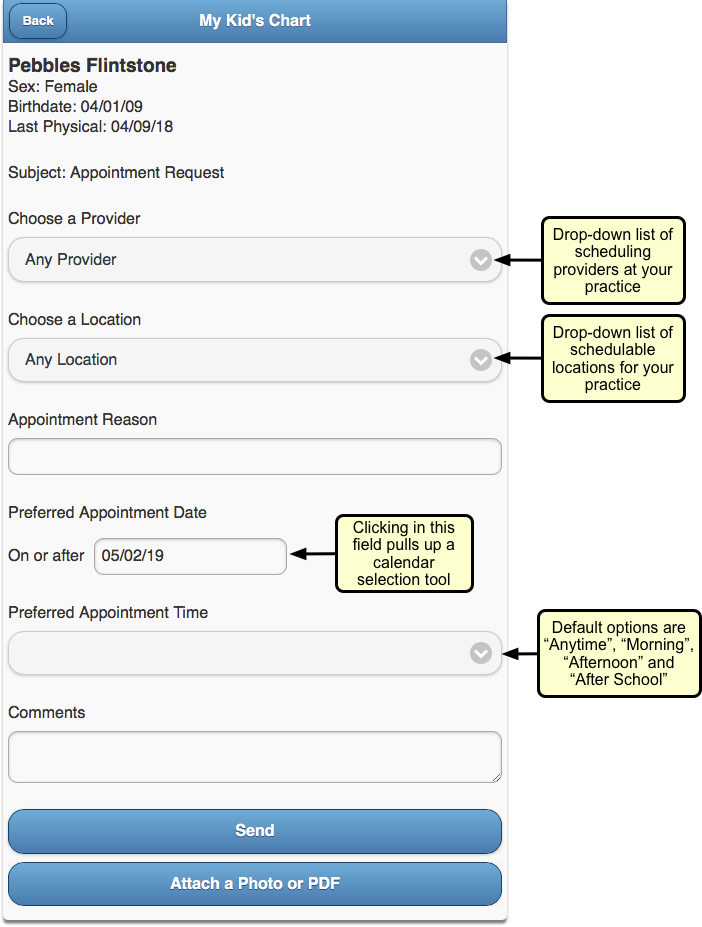
With an Appointment Request template, you can encourage families to provide the information you need to schedule them.
Read Configure Your Patient Portal Message Templates to learn more.
Update How You Handle Scheduling Phone Calls
When your practice schedules an appointment, what do you review and communicate to the family?
Develop a quick script that informs the family what to expect when they visit your practice, and confirm demographic, insurance, and other information when you schedule. For example, if your practice requires masks, no longer uses your waiting room, or performs a phone-based checkin prior to the appointment, set that expectation when you schedule.
If your practice is implementing practice-wide credit card on file for all families, you can collect that information when you schedule. See below for more tips on CCOF implementation.
Adjust When You Schedule, Your Scheduling Blocks, and More
Review when your practice schedules different visit types, and make adjustments that balance what your families need with your practice’s enhanced safety protocols and other changes.
-
Well Visits in the Morning: Some pediatric practices have implemented a “Well Visits in the Morning” schedule. That means all well visits are seen in exam rooms, normal cleaning takes place in between visits, sick visits happen in the afternoon, and the once-a-day more comprehensive cleaning happens after the office has closed.
-
Sick vs. Well Locations: Another pediatric practice has two locations, and they have changed one to a “sick only” location and one to a “well visit only” location.
-
Change Blocks, Stop Using Blocks: Some practices report that in 2020 they “threw out the visit template”, reworked their blocks based on daily trends, or no longer use visit blocks at all.
The above ideas may or may not suit your practice’s goals, but you might make other changes to how you schedule. In the COVID-19 era, pediatric practices need to stay agile as they tweak and adjust schedule blocks, hours, open time slots, and family expectations. As your community and culture rapidly changes in response to COVID-19, patient appointment needs will change too.
Proactively Schedule Followups and Recurring Appointments
When a followup appointment is appropriate, consider scheduling it at the same time as you schedule the initial visit, or during the initial visit. Rather than waiting the weeks or months before you contact a family to schedule, make the appointments when you have the family’s attention.
If your practice normally only schedules out six months, consider expanding that to 13 months so you can schedule annual well visits at the preceding visit.
Ask: “Could This Be a Telemedicine Encounter?”
Many practices schedule telemedicine encounters for sick visits and followup visits. Some are trying out partial well visits over telemedicine as well.
See the Telemedicine section below for ideas on expanding your practice’s telemedicine services.
Improve Your Practice’s Pre-Visit Steps
What does your practice do in advance of each appointment? During the COVID-19 era, you can examine your process and make changes that will make the visit itself easier and more efficient.
Your process might include:
-
Expand When and How You Check Eligibility: Especially if you are increasing telemedicine visits or offering new services, you should review eligibility for all encounters in advance. You can do that with PCC’s built in eligibility tools. Practices report that payers do not respond to eligibility requests until 5 days previous, and anecdotally some Medicaid payers only provide day-of or day-before eligibility information. Regardless, it’s important to check eligibility as employment status, insurance payer rules, and state rules about visit types are rapidly changing.
-
Implement Pre-Visit Questionnaires in the Patient Portal and/or With CHADIS: Since clinician in-person time now has additional constraints and challenges, you may want to implement or expand your pre-visit screenings or questionnaires. You can design your own questionnaires in the patient portal’s templates tool, or you could sign up for CHADIS or a similar service. PCC is working to enhance CHADIS functionality, and a partial CHADIS integration is in pilot test now. As you expand your pre-visit questionnaire use, keep in mind that you will need to adjust your workflow so the front desk or a nurse can send the families these materials or links.
-
Collect Copays in Advance: In order to make in-person and telemedicine encounters as smooth and “touchless” as possible, your practice can implement a policy of collecting copays in advance of an appointment. Since account balances and payments can be done through the patient portal, families will have transparency and can see their credit if the visit ends up not requiring a copay, for example.
Change How You Checkin and See Patients
When it’s time for the encounter, what changes will your practice make to accommodate the additional challenges of COVID-19? This section includes recommendations we heard from pediatric practices across the country.
Eliminate or Reduce Use of Your Waiting Room
Some practices have closed their waiting rooms or greatly reduced any time spent in them. They tell families:
-
Wait In Your Car: Your practice can instruct families to wait in their car until the time of their appointment.
-
Call When You Arrive: When a family pulls in, they can call your front desk to checkin. You can verify insurance, demographics, and collect the copay over the phone.
-
We Will Text You When Your Exam Room is Ready: PCC’s built-in text feature means your staff can quickly select an appointment and text the family when their room is ready.
As they make these transitions in their offices, some practices are changing their long term plans for their layout. For example, could you transition your waiting room into multiple exam rooms or office space?
Virtualize Your Checkin and Precheckin Processes
By using the patient portal, texting, and the phone, some practices have eliminated all parts of the in-person patient checkin.
To facilitate encounter management, some practices create a new Visit Status in PCC EHR, such as “Precheck”, so that everyone can understand when a family has completed their demographic updates, paid their copay, and are ready for the doctor.
At The Door: Take Temperature, Provide PPE
When a family enters the building, a practice can greet them at or near the entrance. They can use this opportunity to take temperatures and to review PPE guidelines for the practice.
If a patient or family member is not wearing a mask, a practice can optionally provide masks for them to wear.
Consider Car Visits and Shot Tents
PCC heard from practices that now see their patients right in their cars.
Instead of an exam room, the clinician visits the patient in the parking lot of the pediatric practice.
When an immunization or other medical procedure is needed, they can use a “shot tent” or station set up for that purpose.
Plan for Flu and Immunization Clinics
If your practice performs annual flu clinics, where you bring in patients en masse for their flu immunization, you can make adjustments to your usual procedures and do the same in 2020 and beyond.
Similarly, if you implement Telemedicine well visits (some practices are trying), you may have a backlog of kids who need to come in for immunizations. When COVID-19 vaccines are developed, pediatric practices may be an important part of distribution and administration.
Practices can work now to improve their “immunization-only” visit workflow and how they might run clinics while maintaining enhanced safety protocols.
Read More Here: Run a Pediatric Drive-Up Flu Shot Clinic
Implement and Expand Your Telemedicine Services
Telemedicine encounters can provide effective care without physical contact. During the COVID-19 era, practices across the country have expanded their use of phone, portal messages, and video telemedicine encounters. When a practice schedules a sick visit or a followup visit, they can stop to ask the both the family and themselves, “Could we do this as a telemedicine encounter?” The answer is often “Yes!”
You can learn how to use PCC EHR’s tools for these encounters here:
- Schedule, Chart, and Bill for a Telemedicine Encounter (Video, Article)
- Bill For Phone Calls and Portal Message Encounters (Video, Article)
Read below for an overview of tips and recommendations we heard from pediatric practices.
Schedule for Telemedicine Appointments
When you schedule a telemedicine encounter:
-
Actually Schedule Telemedicine Encounters: A telemedicine encounter is not just a phone call that you decide to bill for later. Schedule your Telemedicine encounters. Adjust your schedule’s visit reasons, blocks, and more to make telemedicine a real part of your practice’s offerings that you will bill insurance for.
-
Use the PCC EHR Appointment Book: When you schedule a telemedicine encounter in the Appointment Book, a telemedicine icon appears with the encounter for all users, additional fields are available for telemedicine connection information, and PCC EHR can optionally designate a telemedicine billing place of service based on your configuration.
-
Perform Precheckin When You Schedule: As with any encounter in the COVID-19 era, it is important to review and update information as soon as you can, to make the actual encounter run smoothly. Update patient information, verify insurance, and collect credit card information for the copay when you schedule.
-
Set Expectations: When you schedule a telemedicine encounter for a family, tell them exactly what to expect. For example, when will the practice call them for pre-visit questions? How will they receive telemedicine connection information? Let them know during scheduling.
Perform “Precheckin” Calls Before a Telemedicine Encounter
On the day of a telemedicine encounter, or the day before, your practice can call the family. At some practices, this call is made by the MA or nurse. During that call, they:
-
Update Patient and Family Information: Verify demographics, insurance, and other details.
-
Collect Money: Collect copays and payments for any outstanding balances. Since billing and collection for telemedicine visits are rapidly changing, some practices have made it their policy to always collect the copay ahead of time and issue a refund later once the EOB arrives.
-
Tell Them How to Connect: Provide technical instructions on how to connect to the encounter. The caller can provide the telemedicine link verbally, and also send a portal message or followup text message with the URL, using PCC’s direct text message feature.
-
Update Visit Status: When the precheck phone call is complete, the practice updates the Visit Status for the appointment so the practice can see it has been completed and the patient is ready for the telemedicine encounter.
Adjust Encounter Workflow, Charting, and Billing for Telemedicine
You can make changes to your workflow and PCC EHR configuration to help telemedicine encounters be successful.
For example, create additional Visit Reasons, Visit Statuses, and custom chart note protocols that include tools for recording information during a telemedicine encounter.
If some parts of a visit must be done separately, you must decide how you will chart and bill for the two different parts.
To help chart a telemedicine protocol, create one or more telemedicine protocols for your clinicians.
Get Paid and Maintain Practice Revenue
This section collects recommendations and tips for pediatric billing and collections during the COVID-19 era.
Here are some general recommendations:
-
Consider Billing For Other Encounter Types: Prior to 2020, you may not have billed for phone consultations or portal messages. Many practices now do, and PCC has a guide which can help.
-
Adjust Your Electronic Encounter Form: After a clinician is finished with an encounter, they click “Bill” to review diagnoses and procedures and select a visit code. You can customize your practice’s electronic encounter form to include phone consultations and telemedicine-related procedures to make it easier to bill for services.
-
Update Your Chart Note Protocols and Orders: When you click on a procedure or other order on a chart note, PCC EHR can automatically add the appropriate CPTs to your encounter form. Review your lab, radiology, referral, and other orders so that they appear by default on appropriate chart notes and will automatically queue up the correct codes for billing.
Streamline Personal Payment Collection
Across the country, pediatric practices are finding ways to make personal payment of copays and outstanding balances as quick and “touchless” as possible.
-
Implement Portal Payments: Families can pay their copay and outstanding balances in the patient portal. Read Get Started with Portal Payments to learn more. Once you’re set up, work with your schedulers and staff so that they can prompt families to use this service.
-
Implement Credit Card on File (CCOF) for All Families: Your practice can use a third-party service to securely store credit card information, and incorporate CCOF into your practice’s billing policies. When you use portal payments, credit card information is similarly stored by a third party, but by expanding CCOF to all families for other billing needs, you can streamline payment and avoid problems at the time of service. Ask your bank and your merchant services for information about CCOF service. If you are doing portal payments with PCC, you have an existing contract with BluePay, a company which also offers CCOF for other billing needs. You can use a CCOF account flag and clinical alerts in PCC EHR to both drive adoption (by checking if a family has CCOF yet) and inform staff. You can then also create a custom report for the current week’s appointments showing who has CCOF and who still needs it set up.
-
Collect Copays In Advance: As mentioned above, many practices have begun collecting copays during a pre-visit checkin call. For some encounter types, it may not be clear if a copay is needed. A practice can collect the copay for every visit and issue a refund later when the EOB arrives.
-
Set Default Telemedicine Places of Service: Your practice can set default telemedicine billing places of service per scheduling location.
-
Select Billing Place of Service When You Post: Your billers can select or change an encounter’s billing place of service when they post charges.
-
Change Billing Place of Service for Previously Posted Charges: If needed, your biller can even update the billing place of service for charges after they have been posted.
Get Paid By Your Insurance and Medicaid Payers
Are your insurance and medicaid payers paying you for Telemedicine visits in parity with your in-person sick visits? According to regulations in some areas, they should be. You can research this and other topics at the COVID-19 section of your Practice Vitals Dashboard.
For common coding topics during the COVID-19 era, read Code and Bill for a COVID-19 Related Encounter, or take a look at PCC’s quick COVID-19 Coding Guide.
As insurance companies learn to respond properly to changing circumstances, your practice may need to be extra vigilant as you review claim rejections and underpayments and resubmit.
Is Billing Place of Service Still an Issue for Telemedicine?
Early on in the COVID-19 era, some practices encountered challenges with the billing place of service used on claims.
Insurance payers have mostly improved how they handle this. PCC has seen good response in many states to telemedicine billing and other encounter changes that practices have needed to make.
However, just in case, your practice should know about the capabilities in PCC EHR:
Apply for a CARES Grant and Other Available Support
Pediatric practice across the country have participated in the federal government’s CARES program, which includes grants and money for small business loans. As the COVID-19 pandemic continues, every practice should stay abreast of these opportunities, and PCC will help keep you informed.
Find Encounter Charges That Need to Be Posted
Use the Schedule and Messaging queues in PCC EHR, along with the Encounters by Billing Status report, to ensure that your practice has posted all charges for every encounter.
For every patient encounter, a provider needs to indicate billing codes and a biller needs to review and post the charges to queue up a claim. It is easy for a disconnect to occur between these two critical points; your practice renders so many services in a day that some charges, or whole encounters, could be missed. When a provider falls behind in their charting, or a practice loses track of which visits still need to be billed, charges can be missed and revenue lost.
Read below to learn about PCC EHR’s tools to ensure everything is posted in a timely manner.
New Biller Training: This article is part of PCC Learn’s New User Training for Billers guide.
Review the Schedule Screen and Messaging Queue for Billing Status Updates
The billing status buttons on the Schedule screen and Messaging queue in PCC EHR indicate when a visit, phone note, or portal message is ready to be billed.
Watch for “Ready To Post” Encounters
Once a visit, phone note, or portal message has been made ready for billing by the clinician, an orange “Ready To Post” button appears in the Billing Status column beside it.
Visits can be billed right from the Schedule screen in PCC EHR. Phone notes and portal messages can be billed from the Messaging queue.
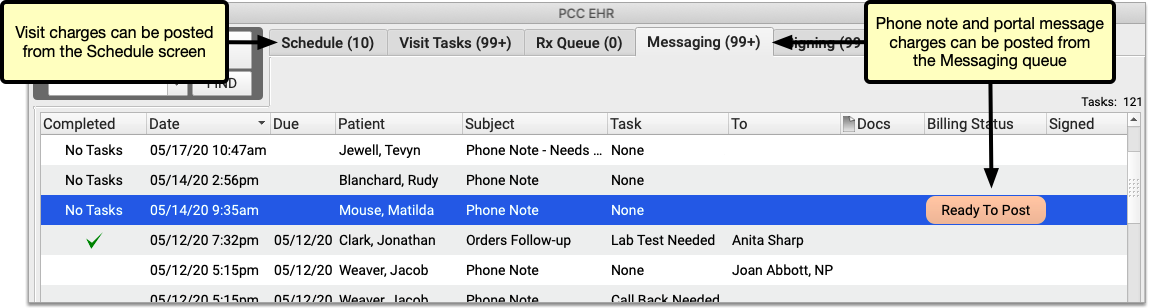
Click the “Ready To Post” button to open the Post Charges screen and bill the encounter.
Watch for “New Items” Encounters
Procedures and diagnoses are sometimes added to visits, phone notes, or portal messages after you post charges for them.
A “New Items” button appears in the Billing Status column beside such encounters, indicating that they require further attention from a biller.
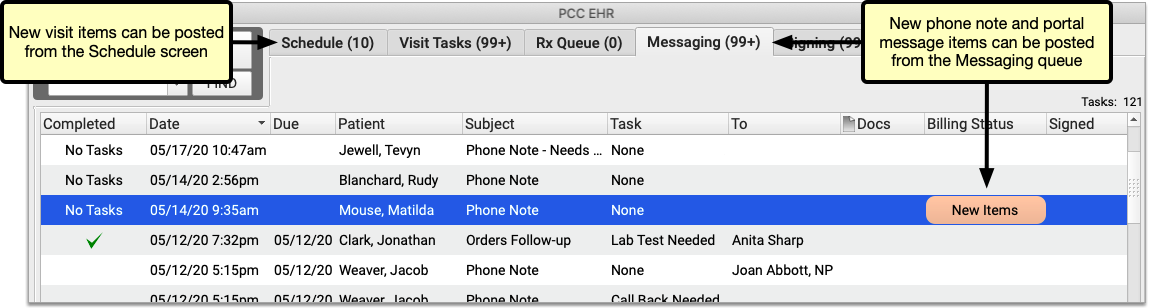
New encounter charges can be billed from the Schedule screen. New phone note and portal message items can be billed from the Messaging queue.
Click “New Items” to open the Post Charges screen and bill the new items that were added to an encounter. You will not be able to edit procedures or diagnoses that were previously posted for the encounter.
Set Your Default Billing Status Filters
You can filter the Schedule screen and Messaging queue by billing status to find visits, phone notes, and portal messages that require a biller’s attention. Furthermore, billing status filter settings can be saved as part of your default view on the Schedule screen and Messaging queue.
In the Schedule screen or Messaging queue, open the “Billing Status” drop-down and select the items you wish to view.
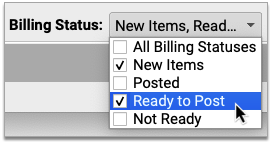
If you decide to save these settings as your default view, click the “Save My Defaults” button.
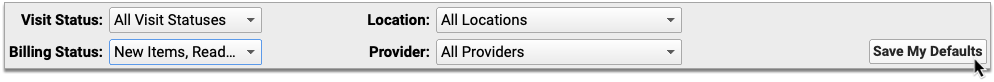
The next time you log in, your window will already be filtered by the billing statuses you set as a default.
Save Separate Defaults for Each Screen or Queue: Each screen or queue in PCC EHR has its own settings and defaults. In order to update your default billing status filters on both the Schedule screen and the Messaging queue, you must set those parameters individually in each screen or queue.
Check Previous Days
As clinicians sometimes finish charting and signing charts later in the day, you may want to build into your workflow a habit of flipping back to the previous day’s schedule and looking for “Ready to Post” or “New Items” that need your attention.
Run the Encounters by Billing Status Report
Use the Encounters by Billing Status report to identify encounters that were not posted and other billing issues so that you can address them. The report can be filtered by provider, billing status, posting status, and location (for multi-location practices). The report can list visits, portal messages, and phone notes that require a biller’s attention. When generated routinely, the Encounters by Billing Status report helps you find and bill outstanding encounters well in advance of insurance carriers’ timely filing deadlines.
Open the Report Library
To generate the Encounters by Billing Status report, open the Report Library from the Reports menu in PCC EHR.
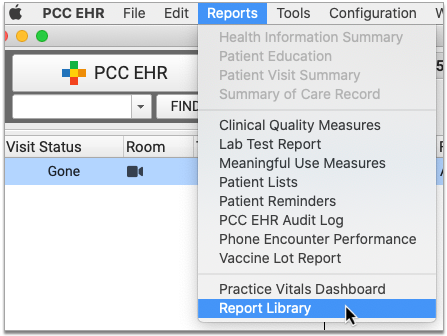
Open Encounters by Billing Status from the Billing Report Category
The Encounters by Billing Status report appears by default under the Billing category in the Report Library. Click on the category title, then click on the report title to open it.
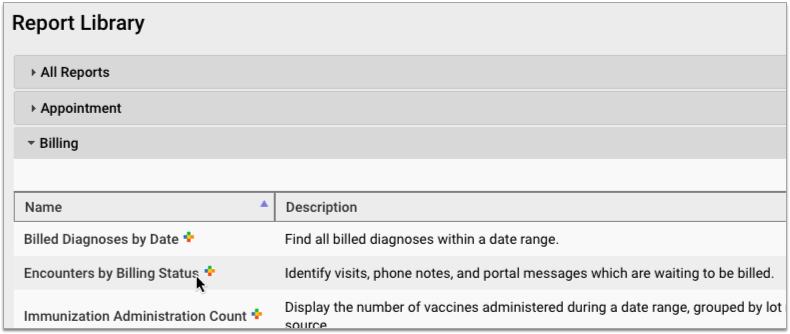
Set a Date Range for the Report, and Optionally Filter by Provider and Location
Set criteria for the report. Choose a date range in the past, and optionally set filters by provider and location.
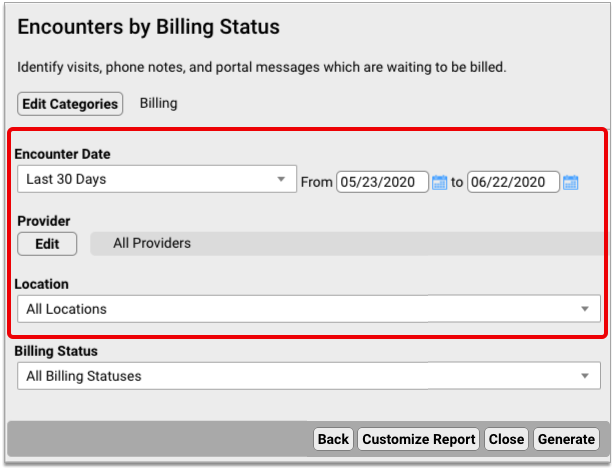
Choose the Billing Statuses for the Report
Which encounters do you want to see? Use the Billing Status filter to indicate the encounter statuses you are searching for.
For example, to generate a list of all encounters that are ready to post or have new, unposted items, select “New Items” and “Ready to Post”.
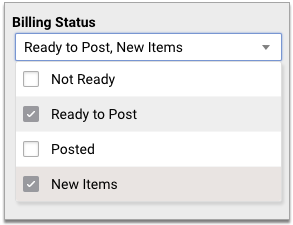
Or, to find old encounters that the clinician hasn’t yet made ready for billing, select “Not Ready”.
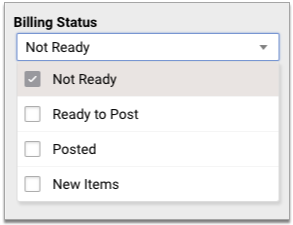
Remind Clinicians to Finish Charting: When you generate a list of encounters that have yet to be made ready for billing, you will likely need to remind the clinicians to wrap up their charting before you are able to post charges.
Generate the Report and Print or Export the Results
Once you have set report criteria, generate the report. Print the resulting list, or export it to your workstation.
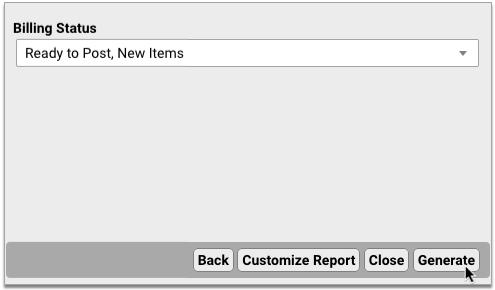
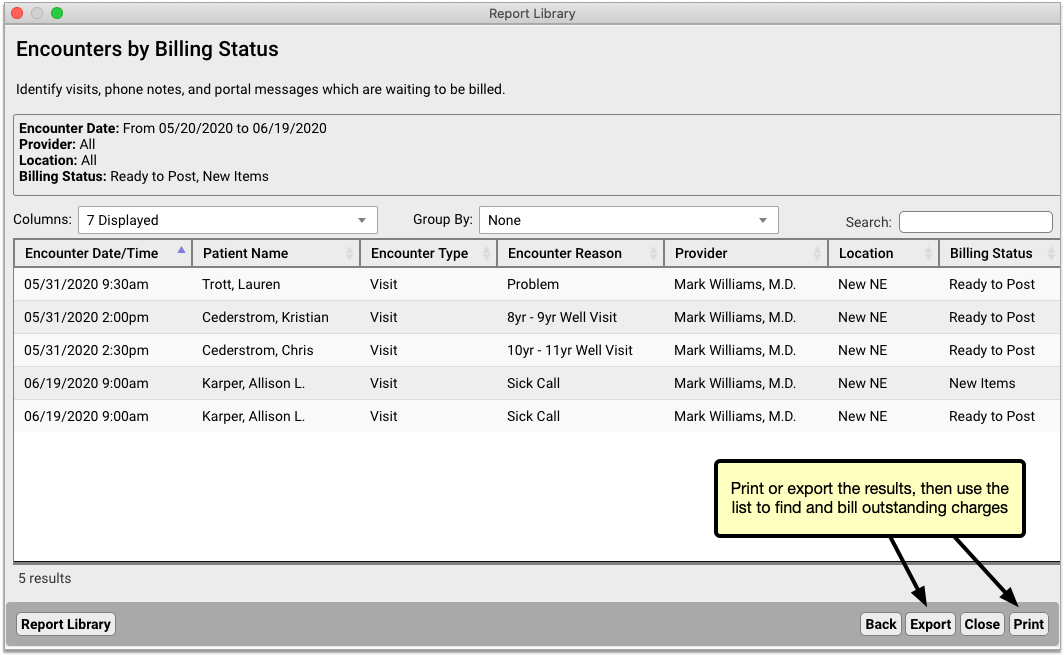
Find and Bill Outstanding Encounter Charges
Use the results of your Encounters by Billing Status report to find and bill all outstanding encounters in PCC EHR.
Outstanding visits can be billed from the Schedule screen by navigating to the date of the encounter. Portal messages and phone notes can be billed from the Messaging queue.
You can also post charges from the Billing History section of the patient chart. Open the chart of a patient who appears on the Encounters by Billing Status report. Navigate to the History section of their chart, then click the “Billing History” anchor. An orange billing status displays beside encounters which have new items or are ready to post. Highlight the encounter you want to post, then click the “Post Charges” button in the bottom right corner of the window.
Encounters by Billing Status Report vs Visits by Billing Status Report: The Visits by Billing Status report only allows you to report on visit encounters. Portal message and phone note encounters are not included in its results. For the most complete information about encounters that need to be billed, use the Encounters by Billing Status Report.
Establish a Billing Routine
The most significant step you can take to ensure that your practice charges for all eligible encounters is to create practice-wide routines around chart note completion and charge posting. As a practice, decide how soon chart notes need to be completed after a visit, and how soon charges need to be posted after that.
By holding clinicians and billers accountable to a common standard, your practice reduces the chance that encounters will be made ready for billing when they shouldn’t, or that charges will be posted before chart notes are truly complete.
If you would like to explore how to improve your practice’s particular workflows, contact PCC Support. To learn more about posting charges in PCC EHR, visit Post Charges.
Send a Text Message Directly to a Patient or Family
Is a family waiting in the car before their appointment? Do you need to send a family a URL link for a telemedicine connection? You can now send a text message directly to a patient’s cell phone number. To watch a video about how to use this feature, click here.
Send a Single Text Message
When you need to send a quick text message, select an appointment on the Schedule screen and then click “Send Text”.
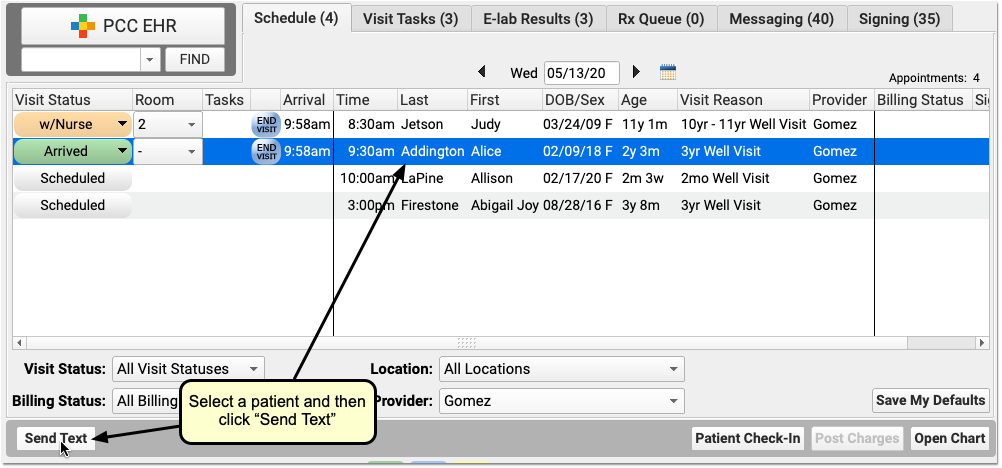
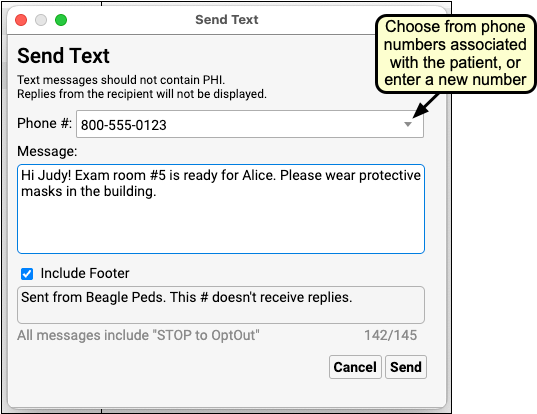
Select a phone number from the patient’s records or enter a new phone number. Then type your message and optionally turn on or off your practice’s default message footer. Messages are limited to a total of 160 characters and should not contain PHI.
Click “Send” to send the message. The family will receive the message in a few seconds.
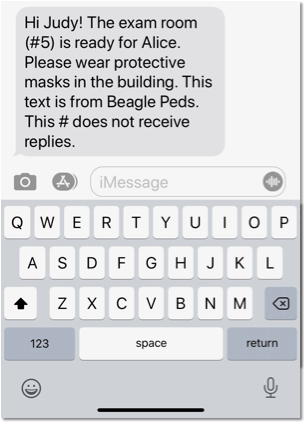
In addition to sending a text from the Schedule screen, you can also open any patient’s chart and choose “Send Text” from the Edit menu.
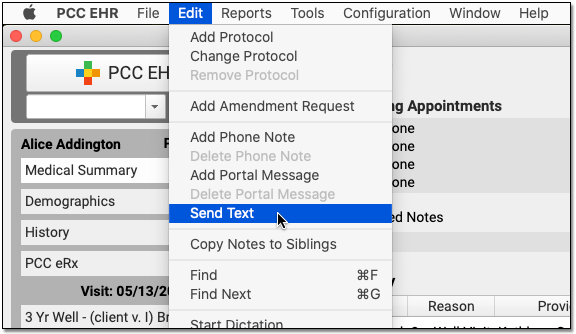
After you click send, PCC EHR will display a brief status window, which will usually tell you that the text was successfully delivered. If the text is stalled for some reason, PCC EHR will close the window to allow you to return to work. Use the Single Text Log report in the PCC EHR Report Library to review what text messages went out (and if any bounced or couldn’t be sent). PCC EHR does not log text messages in patient chart record.
Text Message Workflow Tip--Ask For Their Preferred Number: If you know you’re going to text a family about an appointment, you can ask them what cell number they want to receive the text message update. Enter that number in the Appointment note or in a custom chart note component, and it will be available when your practice needs to text them.
What Phone Numbers Appear in the Drop-Down When I Send a Text?: When you create a text message, you can pick from phone numbers that PCC has linked to the patient, including home account phone numbers, the patient’s confidential communication preference, and patient portal numbers. If instead you enter a number manually, PCC EHR will remember that number for later use. The most recent number used by your practice will appear at the top. Any numbers previously identified as invalid will not appear.
Review Your Practice’s Outbound Single Text Messages to Patients and Families
How can you review what texts were sent, by whom, to whom, and find out if a text was delivered successfully?
Run the Single Text Log report in the PCC EHR Report Library to examine your outbound text records.
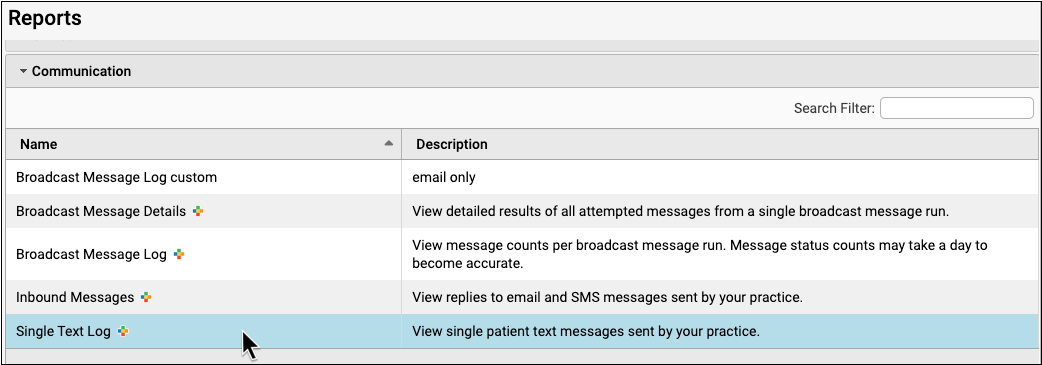
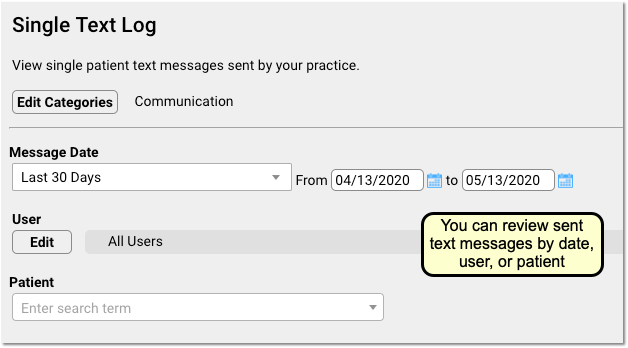
You can filter the report based on date, the user who sent the messages, or by the patient. By adjusting these criteria, you could see all the texts sent by Dr. Crusher, or all the texts sent to any cell phone number listed for patient Abigail Addington.
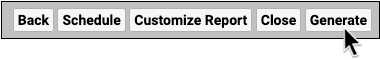
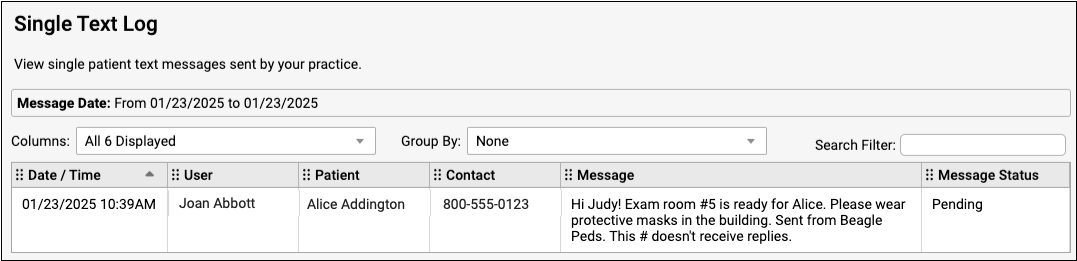
On the report, you can see the date and time, the user at your practice who sent the text, and the patient who the message was sent in regards to. Next, the report displays the phone number that was used. When known, the report will display where the number comes from (i.e., from a parent account). If your practice typed in a number when they sent the text, the number’s origin may not be known.
Finally, the report will display the Message and the Message Status. You can use the Message Status to understand whether a message was successfully delivered, bounced by the cell phone carrier, or if something else happened.
Turn On and Configure Direct Text Messaging
If your practice wants to send direct text messages to patients and families from PCC EHR, you must first turn this feature on. Open Practice Preferences from the Configure menu and select the “Enable Send Text” option.
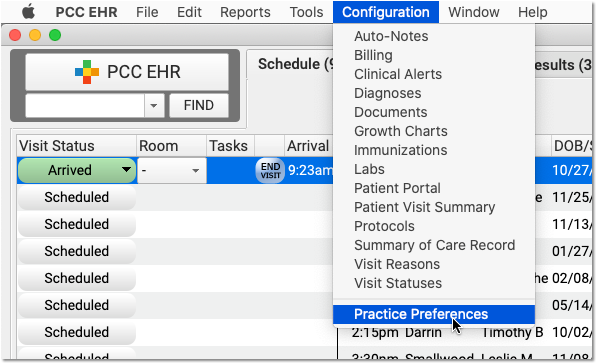
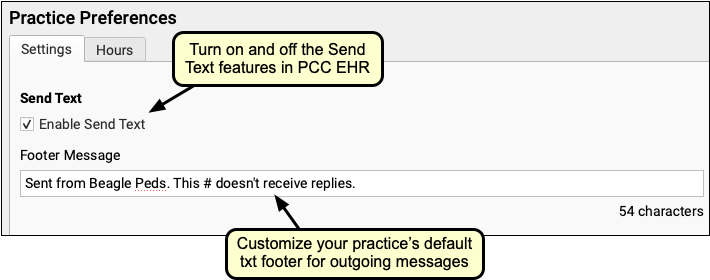
After you have turned on the feature, the next time a user logs in they will see the “Send Text” option on the Schedule queue and in the Edit menu when editing a patient chart.
You can also customize the default footer text that appears on outgoing text messages sent to single recipients. Note that the footer contributes to the overall total limit of 160 characters.
Note that these setting are for the Send Text features only, and they do not affect Broadcast Messaging or patient portal notification text messages.
Who Pays for Single Outgoing Text Messages?: Your practice’s PCC Care Plan contract covers 100% of costs for outgoing, single direct texts to patients and families.
UC 2020 Chat
For UC 2020, PCC is running a chat feature to keep users connected as we attend remote sessions. Presenters and instructors will use the chat as a way to field questions and facilitate discussion, and it can also be used to talk and connect with other session attendees.
The chat will be live for the duration of our virtual UC, and you can access it outside of session hours. For more details about UC 2020, and a session schedule and links, visit the UC 2020 page on pcc.com.
Sign up for UC Chat
Use the link you received from PCC Marketing to reach the registration page.
Enter your email address, and select a username and password. The chat tool will then send you a verification email.
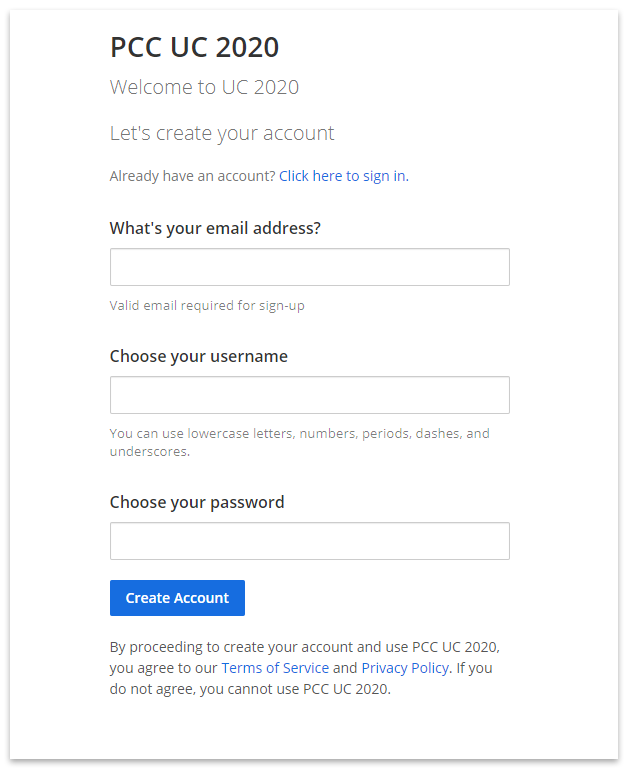
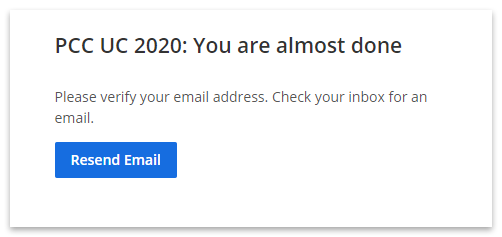
When you receive the verification email, simply click on the Verify Email button to complete the process.
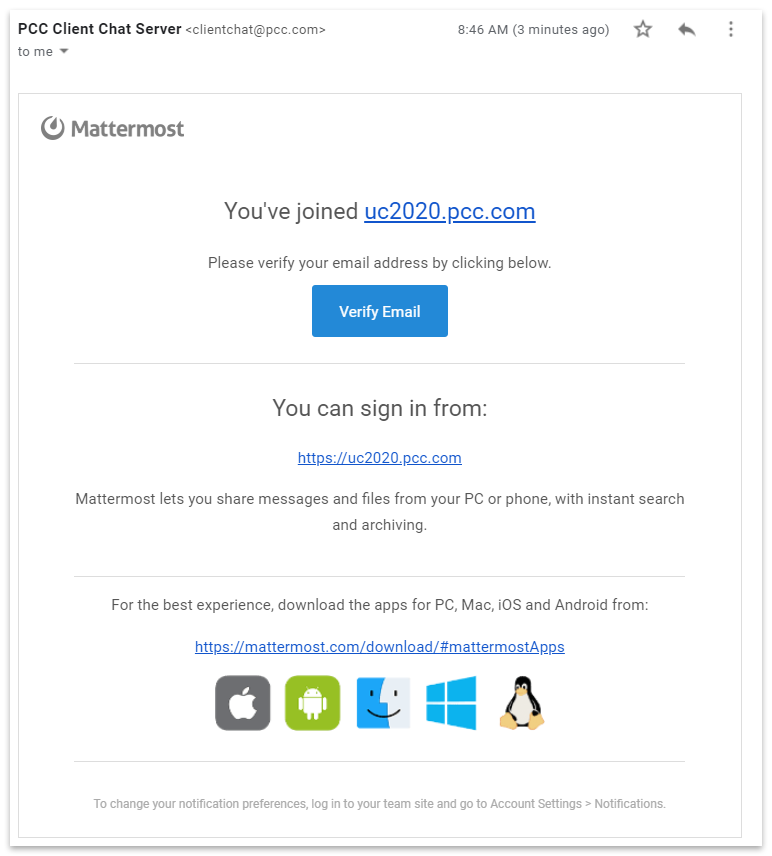
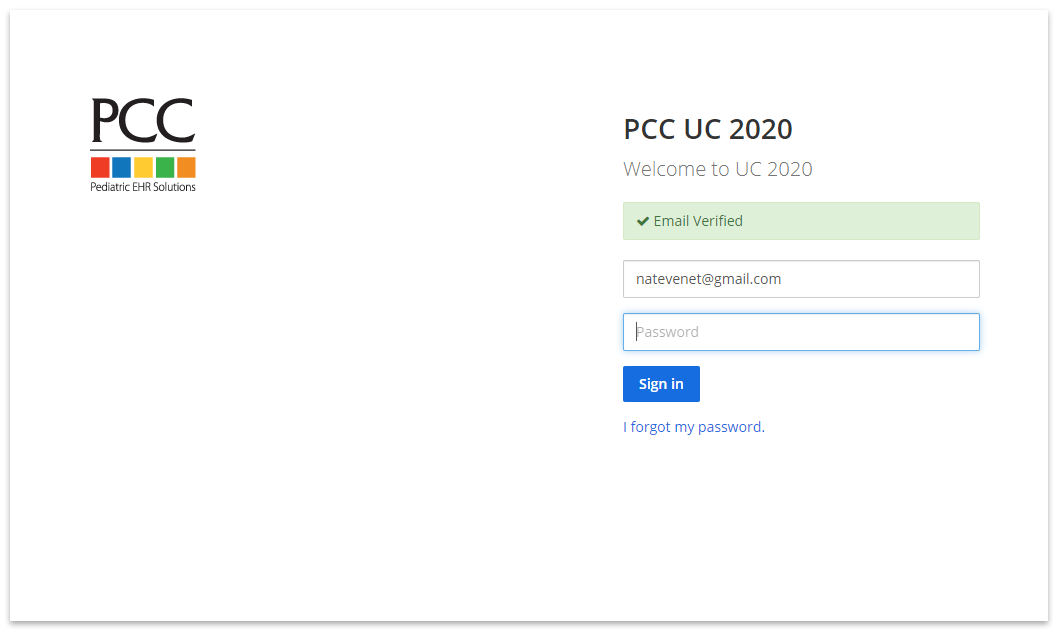
Now you’re ready to log in!
Logging in to UC Chat
Follow the link from PCC’s UC2020 page, or manually enter the URL for chat in your browser: https://uc2020.pcc.com/uc2020
Enter your email and password to log in to UC Chat.
How to Use UC Chat
On the right is the main message window, and on the left you can select from different channels, or message threads.
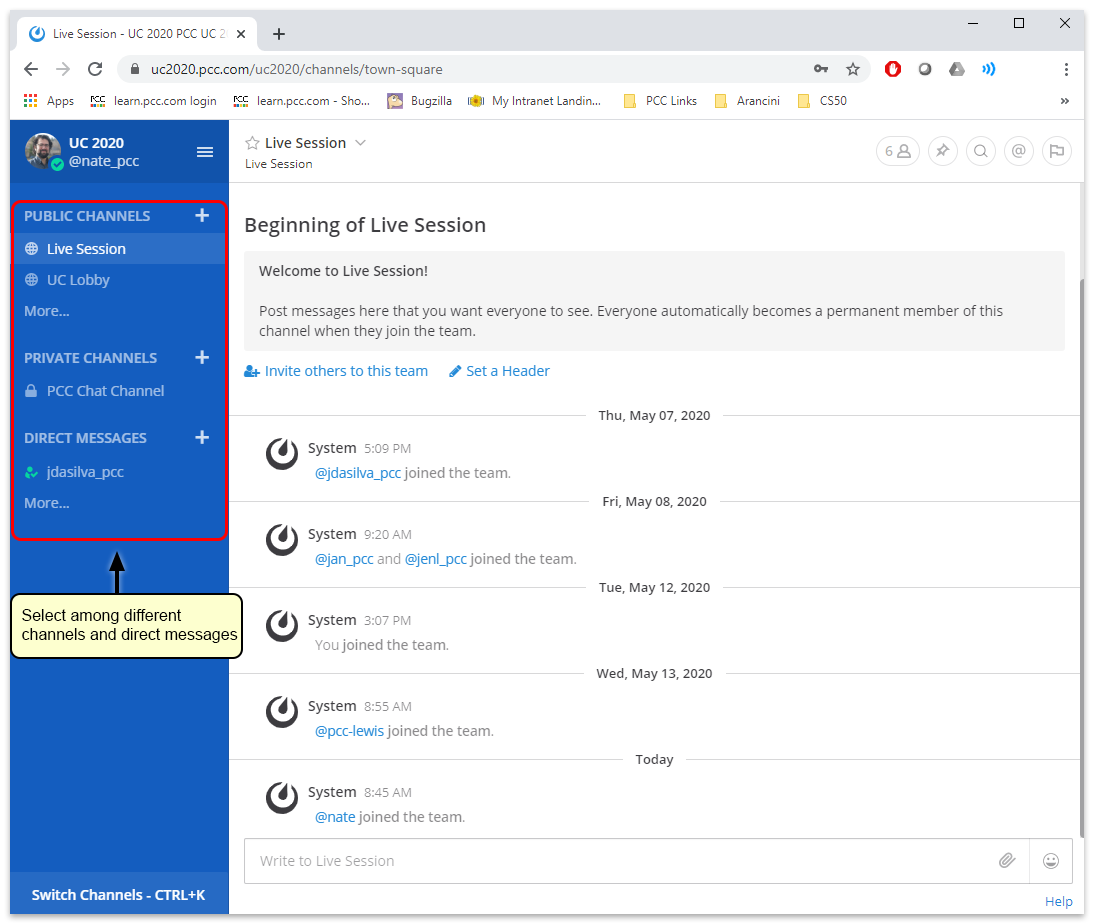
Discussion Channels
There are two main channels:
- UC Lobby: This is for general chat and conversation. Talk and connect with other Virtual UC attendees.
- Live Session: This channel is for questions and discussion about UC sessions as they are happening. During sessions, this channel will be moderated and monitored by a PCC staff member, and is where you can ask presenters questions.
Other Channels
There are other channels that provide opportunity to connect directly with other practices who are similar in size and scope. To add them to your ribbon, Click on “More…”
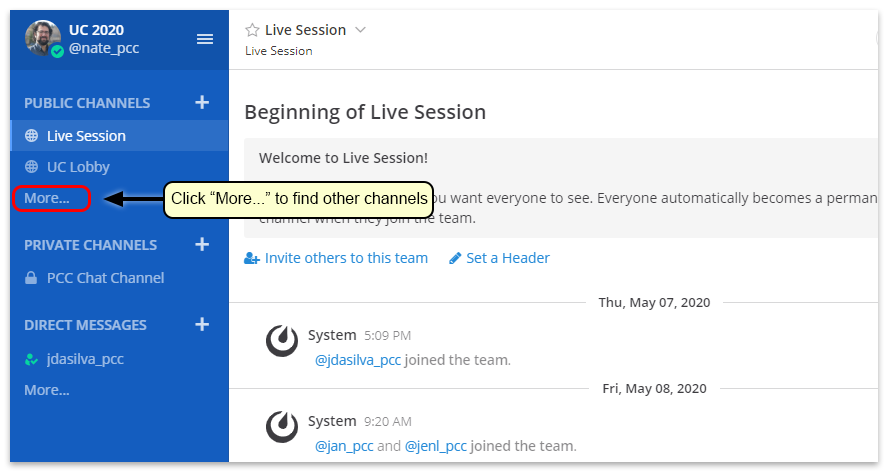
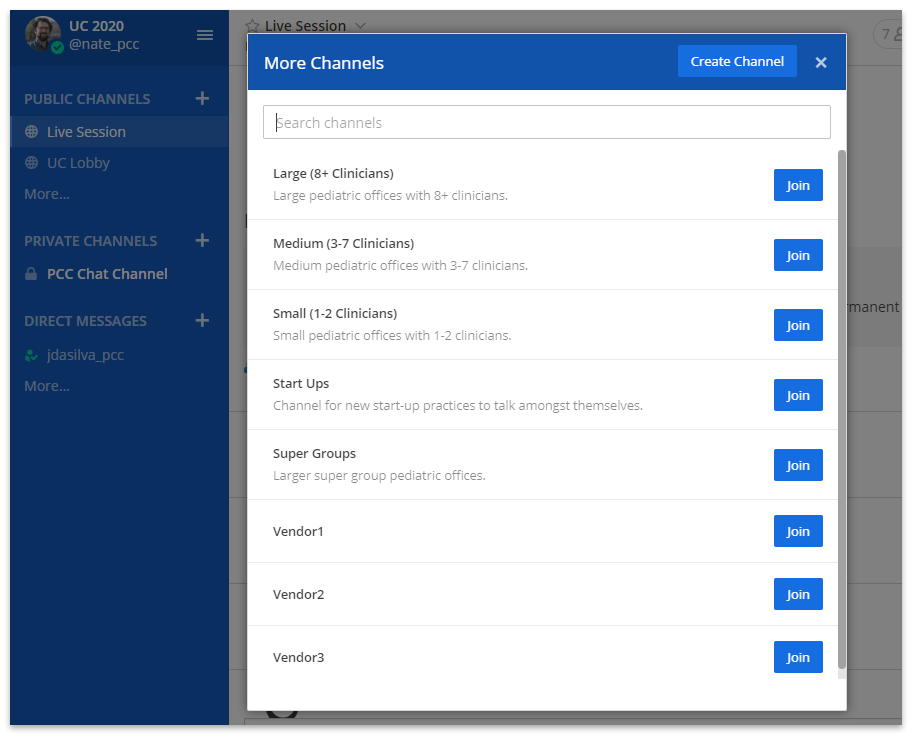
There are channels specific to different sizes of practices, as well as a channel specifically for start up practices. Join one or more of these channels if you want.
There are also channels here for virtual vendors. If you would like to connect directly with one of the vendors, you can do so here.
Direct Messages
If you want to chat with one or more people directly, you can do so by sending a direct message. First, click on the plus next to Direct Messages.
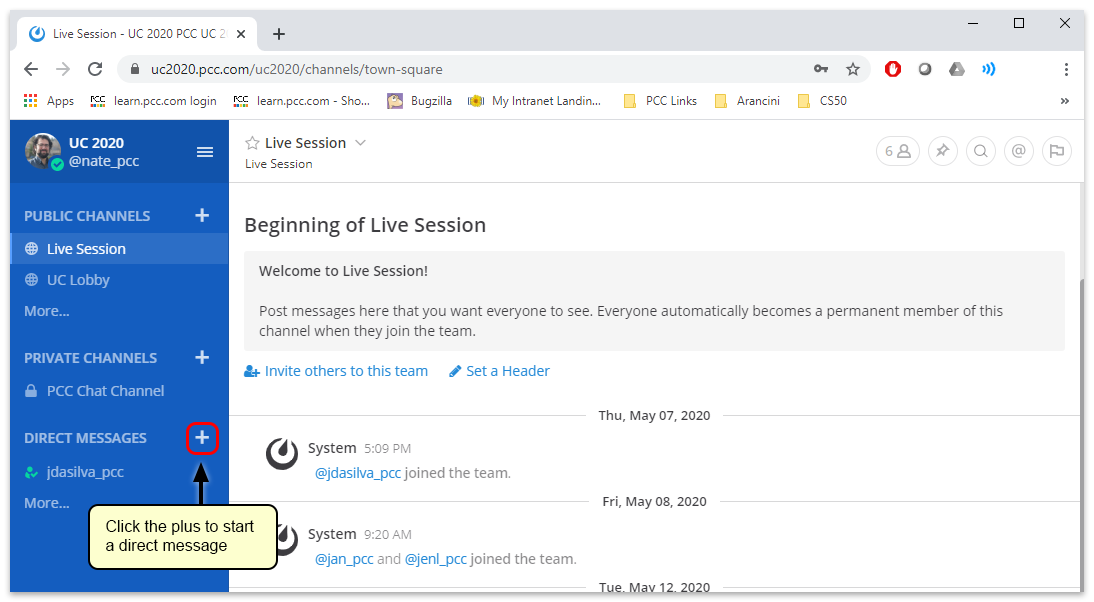
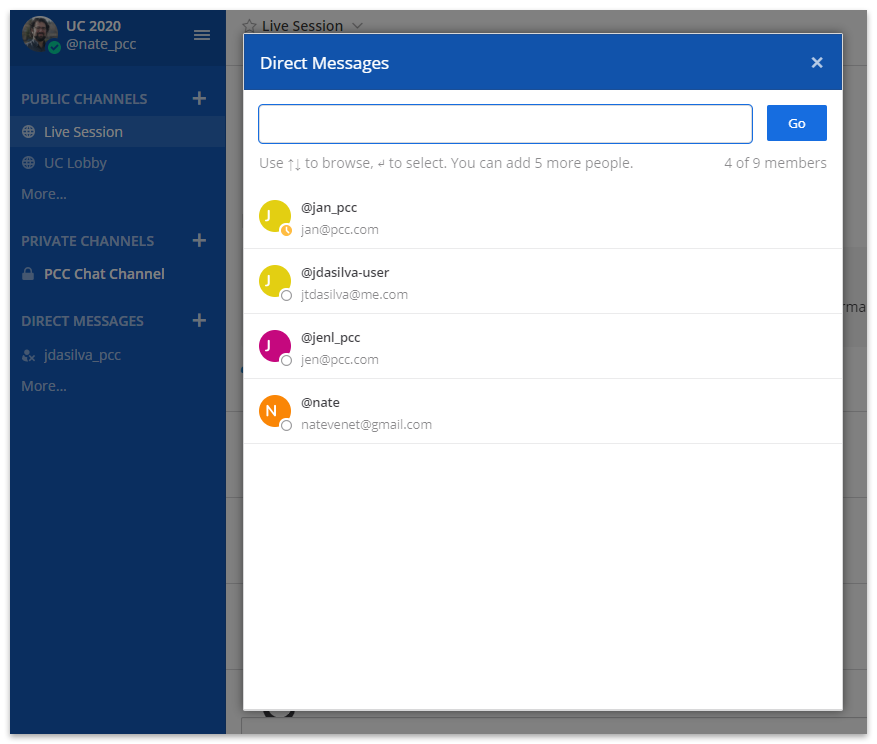
Find and select the person or people you want to message, and then click the “Go” button.
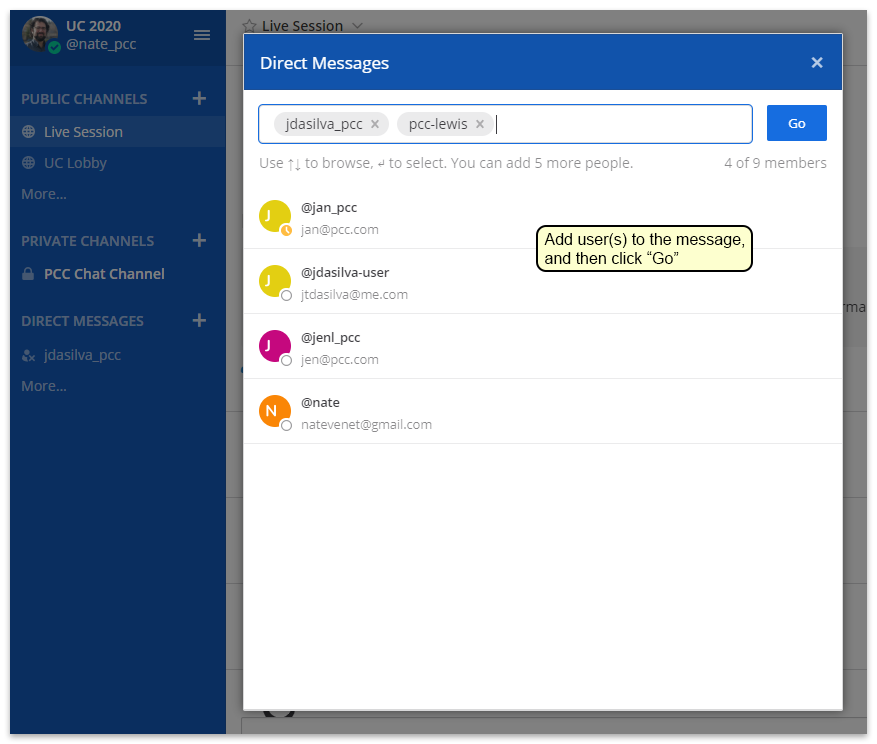
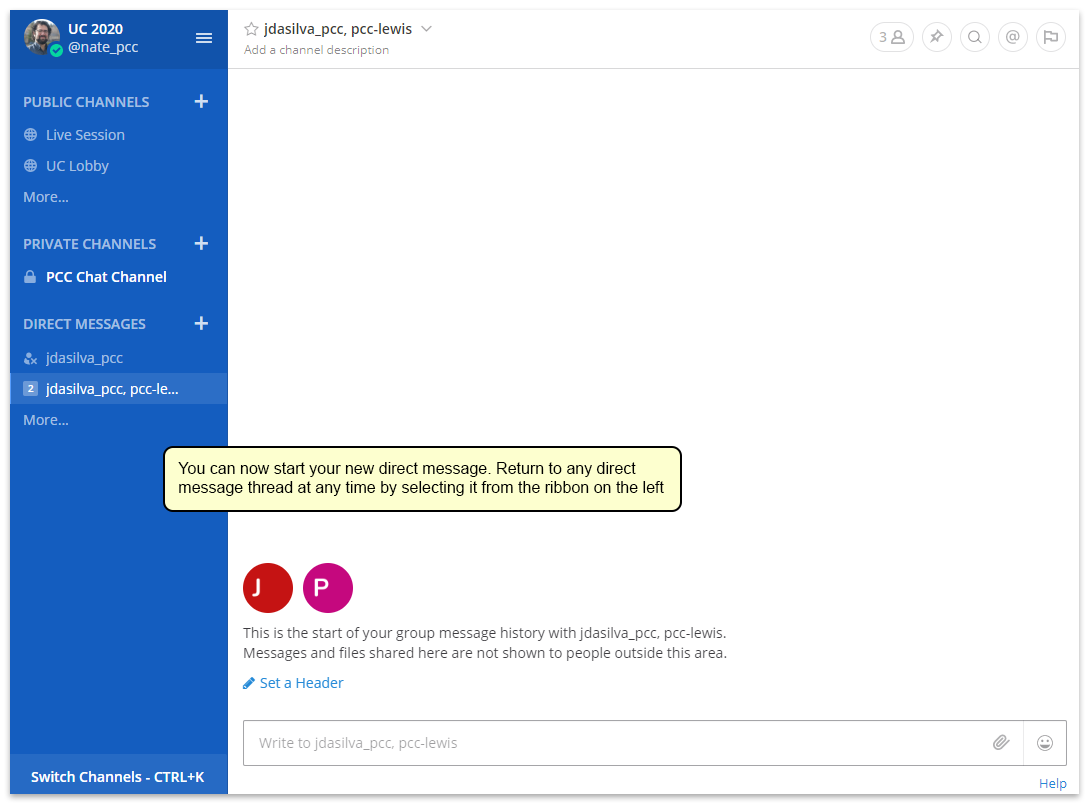
You can now begin messaging these people. Your recent direct messages will appear in the ribbon on the left for easy navigation.
Preferences and Settings
You can change your username, notification settings, avatar, and other details in the Account Settings menu.
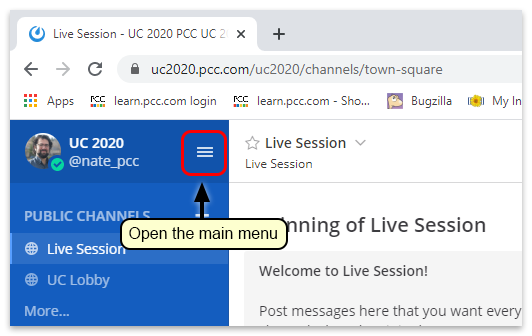
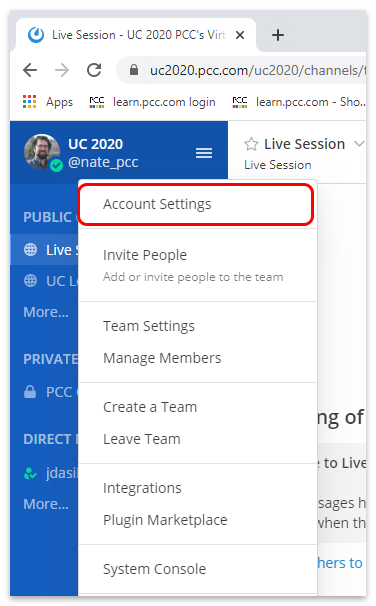
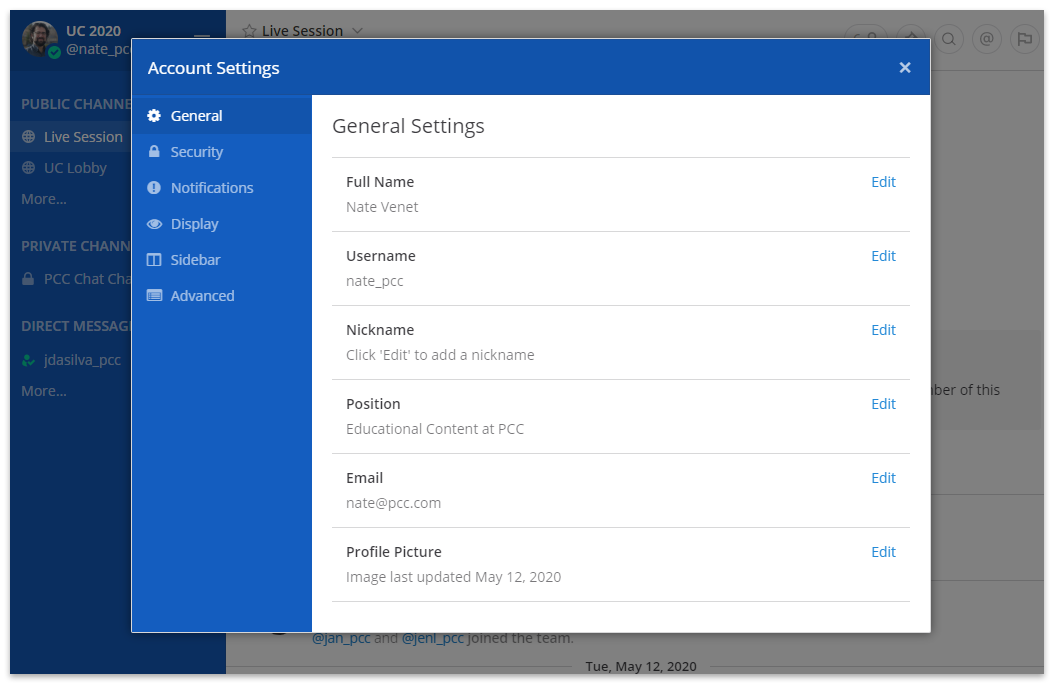
The first screen here, “General Settings” gives you options to change your user name and email. You can fill out the “Position” field to let people know more about who you are; it can be helpful to include your position and the name of your practice. You can also add a profile picture here.
Notifications
You can also change your Notification preferences in Account Settings, under the “Notifications” tab.
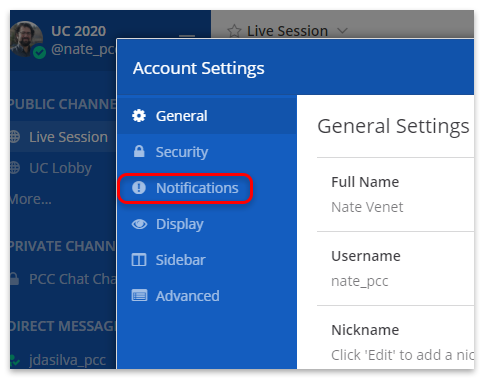
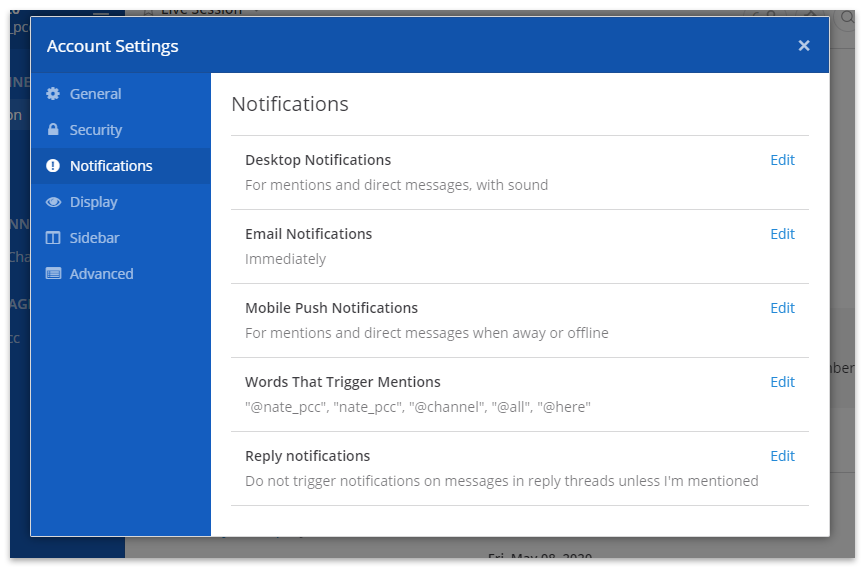
Print from PCC SecureConnect to Your Home Printer
If you connect remotely to your PCC system using SecureConnect, you can print out of PCC EHR and the Practice Management window wherever you are working.
For more information about getting set up with SecureConnect, read Connect to Your PCC System from Home.
Print out of PCC EHR in SecureConnect
Learn how to print out of PCC EHR while working in SecureConnect.
In PCC EHR, Click “Print”
While working in PCC EHR in SecureConnect, navigate to the item you wish to print and click the Print button.
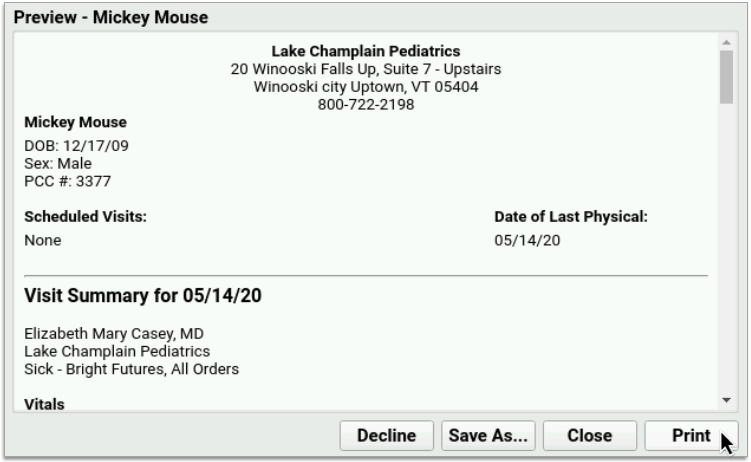
Select the Printer Named “Print_to_SecureConnect”
In the print options, select the printer named “Print_to_SecureConnect”.
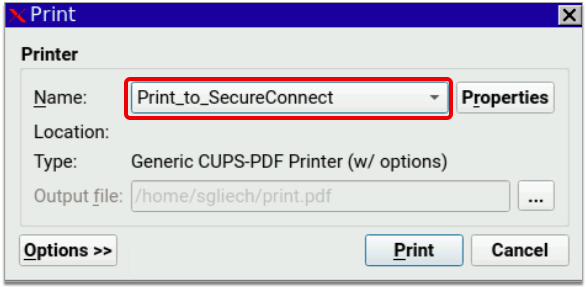
Finish Printing out of PCC EHR
In the PCC EHR print dialogue, click “Print”. The print file will automatically download to your workstation.
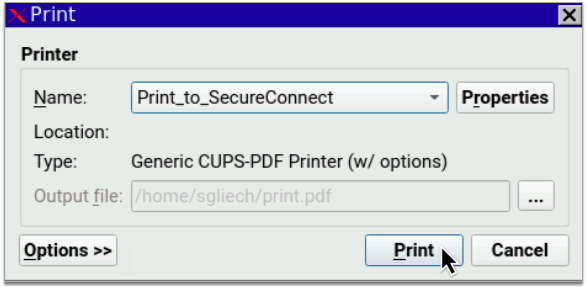
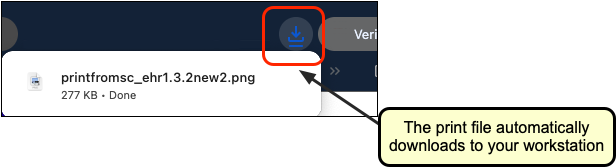
Unsuccessful? Try Again: The very first time you try printing out of SecureConnect, your web browser might not be successful in printing the document. Don’t panic! Exit SecureConnect, sign back in, and try again. If you continue to experience issues printing out of SecureConnect, contact PCC Support.
Open the Print File in a Document Viewer Window
Find the print file in your internet browser or computer’s downloads folder. Double-click the file to open it in a document viewer on your local workstation.
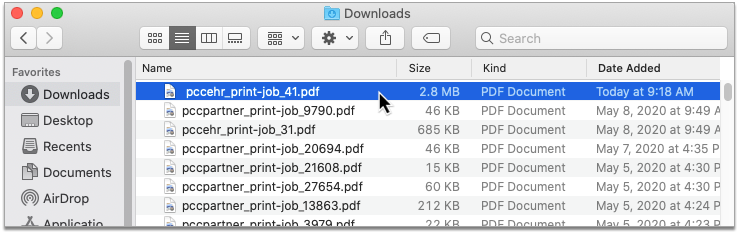
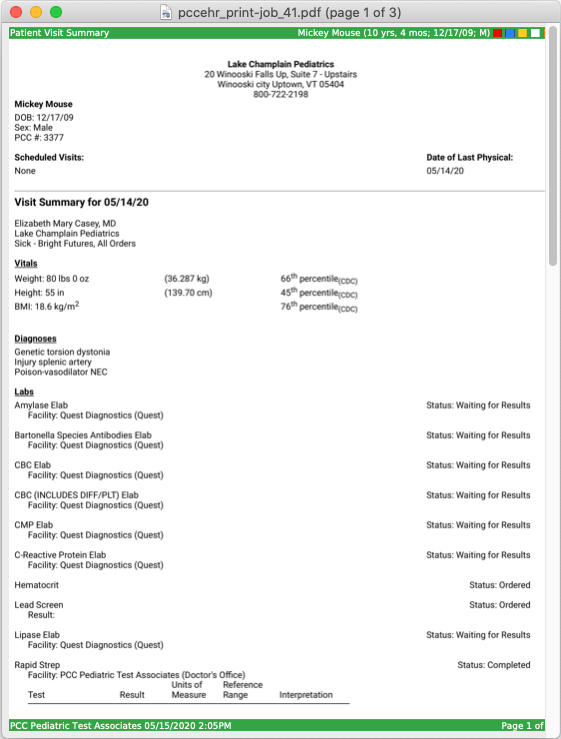
Files Might Open Automatically: Some workstations and web browsers are configured to open files automatically upon download, saving you the step of having to find the documents in your downloads folder.
Print the File to Your Local Printer
In the document viewer window, open the File menu and click “Print”. Select your local printer as the destination and print the file.
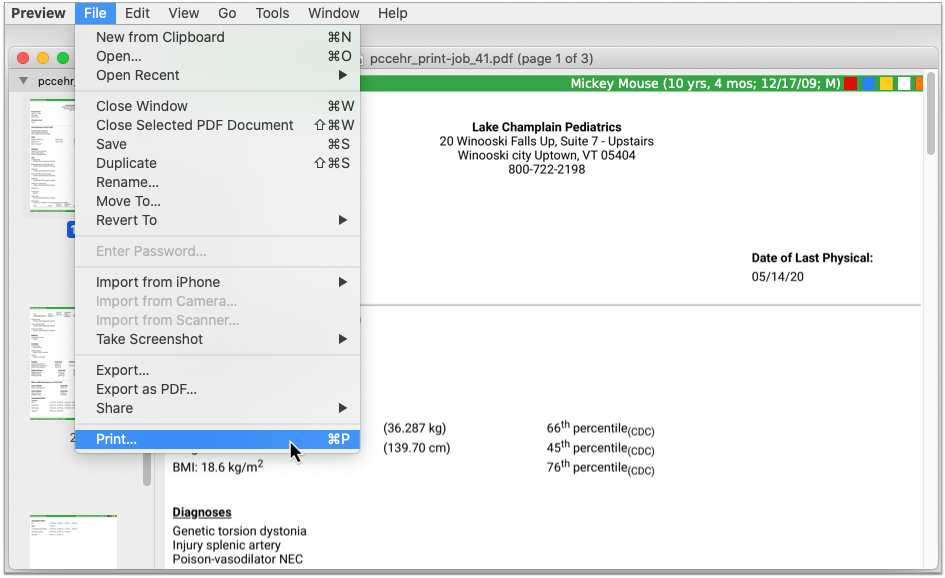
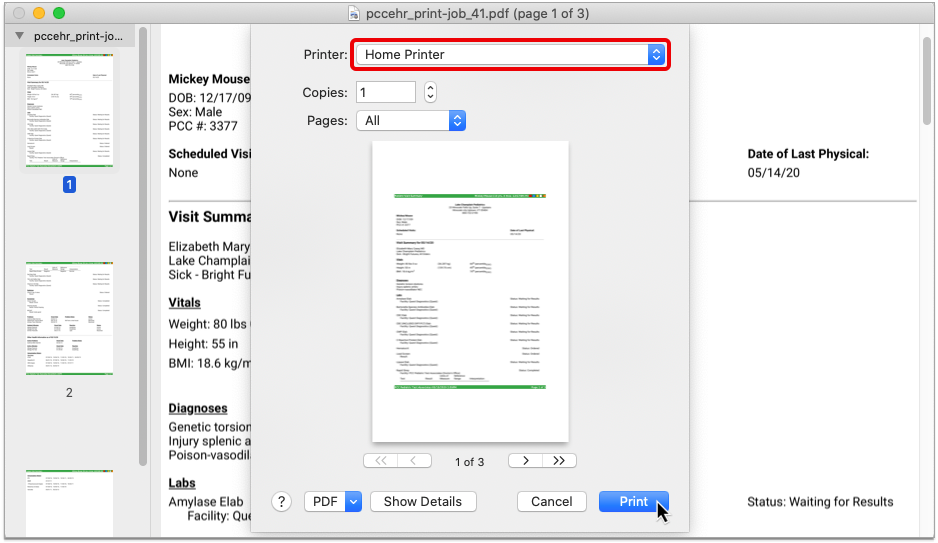
Log Out of PCC EHR Every Time You Use SecureConnect: Please make sure to sign out of PCC EHR before closing your Secure Connect tab or window to avoid multiple login instances.
Print out of Practice Management in SecureConnect
Learn how to print out of Practice Management while working in SecureConnect.
Open a Practice Management Window
In SecureConnect, open a new Practice Management window.
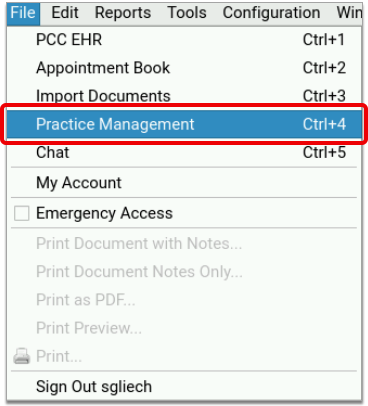
Set Your Default Printer
Most users will automatically be prompted to choose a default printer when they open Practice Management. In this case, type ‘X’ next to the printer named “Print_to_SecureConnect”, then press F1 to save your selection.

Some users will not be prompted to choose a default printer when they open Practice Management and will instead be directed to the main menu screen.
To set your default printer from the main menu screen in Practice Management, select Pick a Default Printer (pickaprinter), then choose “Print_to_SecureConnect” as your default.
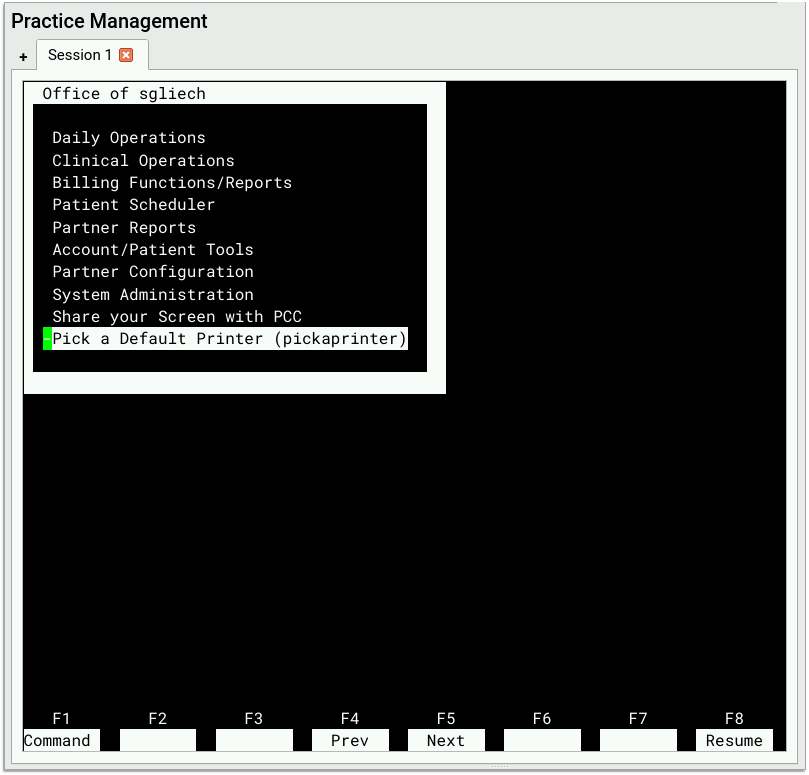
If you do not see Pick a Default Printer (pickaprinter) in your main menu in Practice Management, call PCC Support to have the option added.
Find Something to Print and Set a Destination Printer
Navigate to the item you wish to print. Follow the screen prompts to print the file. If you are given the option to define a destination printer, use your default or type in “Print_to_SecureConnect”.
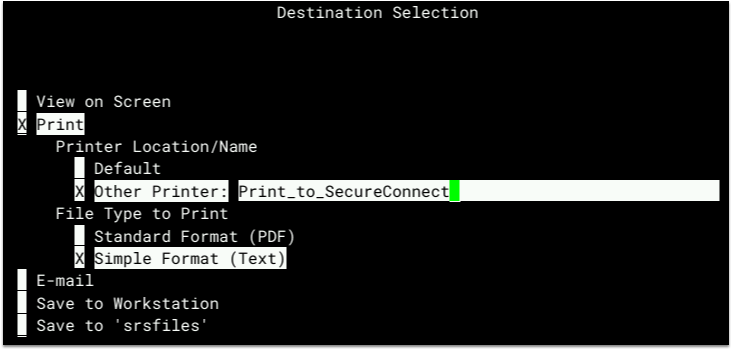
If you are not given the option to define a destination printer, Practice Management will automatically use your default printer setting, which is now “Print_to_SecureConnect”.
Not All Practice Management Jobs Can Be Printed from SecureConnect: Certain kinds of print jobs, such as paper HCFA forms, are configured at the practice level and do not pay attention to users’ personal printer settings. Contact PCC Support if you are having difficulty printing one particular type of job while working in SecureConnect.
Finish Printing out of Practice Management
After you set the destination printer, follow the screen prompts wherever you are working to finish printing the file. The print file will automatically download to your workstation.

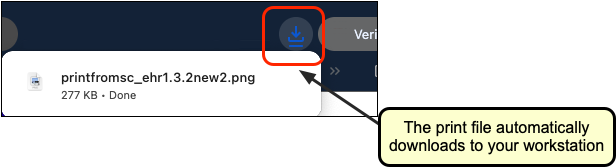
Unsuccessful? Try Again: The very first time you try printing out of SecureConnect, your web browser might not be successful in printing the document. Don’t panic! Exit SecureConnect, sign back in, and try again. If you continue to experience issues printing out of SecureConnect, contact PCC Support.
Open the File in a Document Viewer Window
Find the print file in your internet browser or computer’s downloads folder. Double-click the file to open it in a document viewer on your local workstation.
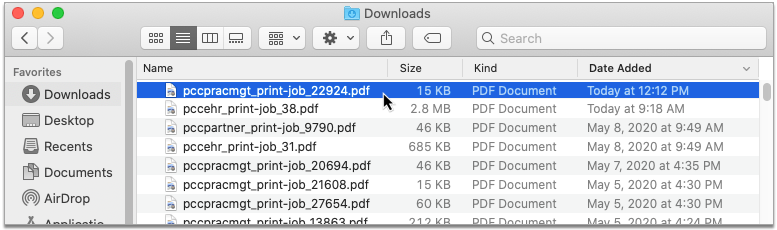
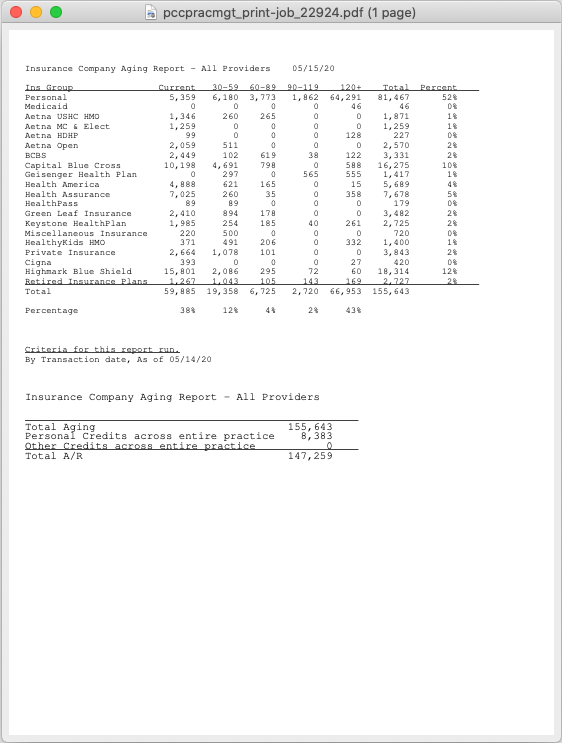
Files Might Open Automatically: Some workstations and web browsers are configured to open files automatically upon download, saving you the step of having to find the documents in your downloads folder.
Print the File to Your Local Printer
In the document viewer window, open the File menu and click “Print”. Select your local printer as the destination and print the file.
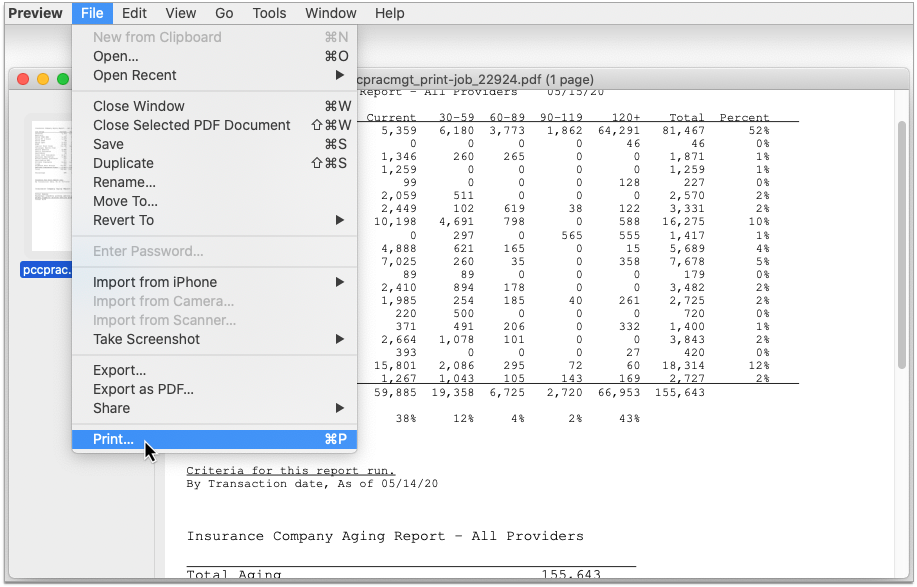
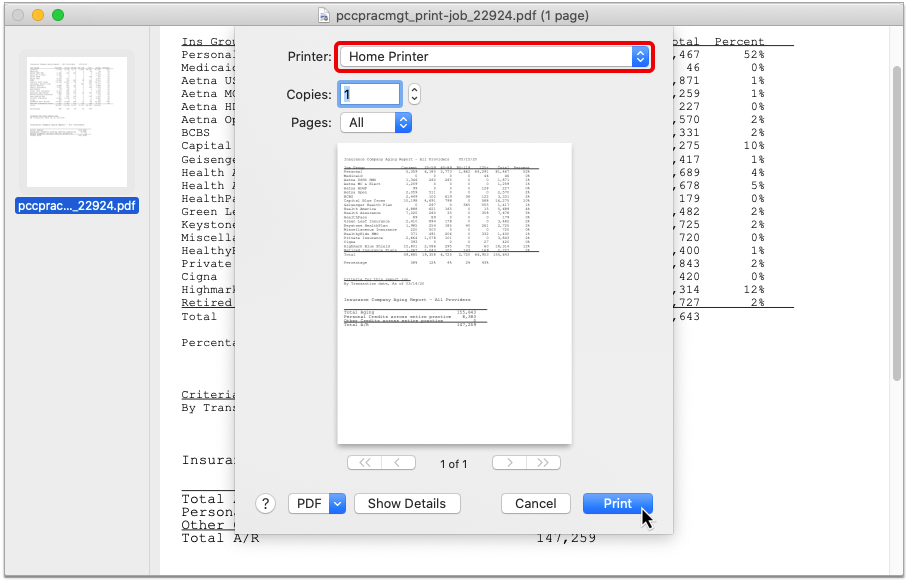
Log Out of PCC EHR Every Time You Use SecureConnect: Please make sure to sign out of PCC EHR before closing your Secure Connect tab or window to avoid multiple login instances.
For information about how to call up your local workstation’s printer options from Practice Management while working at the office, read Choose Your Practice Management Printer.
Configure Post Charges
Read the sections below to learn about configuration options and implementation recommendations for the Post Charges features in PCC EHR.
Turn Post Charges Off/On for Appropriate Users
Before your practice can post charges in PCC EHR, you must grant permissions to a user role. You should review your user roles and decide which users can post charges and queue up an insurance claim.
Open the User Administration tool and visit the Roles tab.
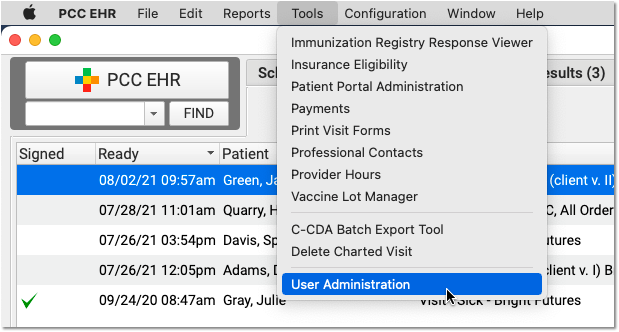
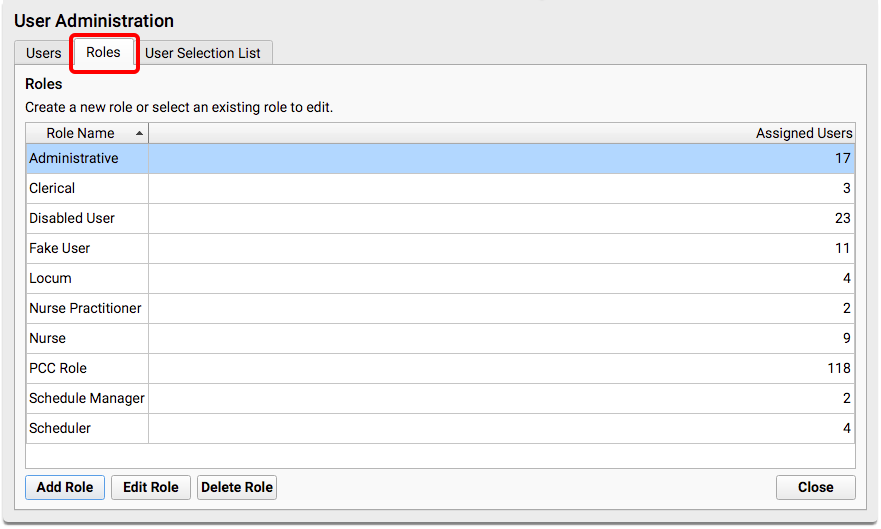
You can create a new “Biller” role, or use an existing role.
When you edit the role, add the new “Post Charges” permission.
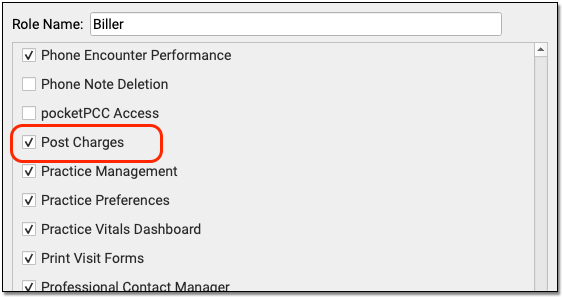
Next, review each user at your practice who will post charges and add the role.
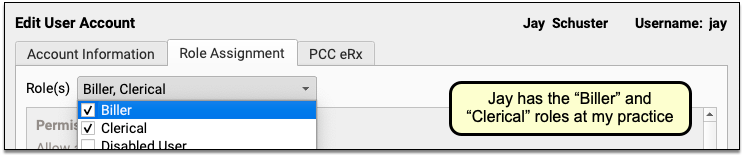
For a more detailed guide to setting up roles and configuring user permissions, read Set User Roles for Permissions and Security.
Set a Default Billing Place-of-Service for Telemedicine Encounters
It can be cumbersome to manually switch the billing place of service each time you post telemedicine visit charges. To make posting easier, set a default billing place of service for telemedicine visits in PCC EHR Practice Preferences.
To learn more, read Set a Default Billing Place of Service for Telemedicine Visits.
Configure Billing Behaviors for Each Payer
As you work in Post Charges, PCC EHR can automatically adjust due amounts and what appears on a claim based on your selection and your practice’s configuration.
PCC supports configurations for price schedules, copay rules, capitated plans that adjust off charges immediately, and Medicaid plans (where nothing reverts to personal due). Your practice can customize the billing behavior of any procedure for any insurance plan.
For example, PCC EHR can automatically calculate copays based on procedure codes or percentages. Your staff should rarely have to manually change the copay amount due. The correct amounts will appear in the Procedures component automatically.
For help customizing billing behavior of insurance plans, contact PCC Support.
Create Alerts for Post Charges
Would you like to alert your staff when they open Post Charges? You might have specific reminders you want to deliver when a patient has a certain insurance policy, has an account flag, or when other criteria apply.
You can use Clinical Alerts in PCC EHR to automatically alert your staff when they open Post Charges. To learn how to create a Clinical Alert, read Clinical Alerts.
Configure Your Practice’s Patient Details Protocol for Post Charges
As you post charges in PCC EHR, you can review a customizable Patient Details ribbon.
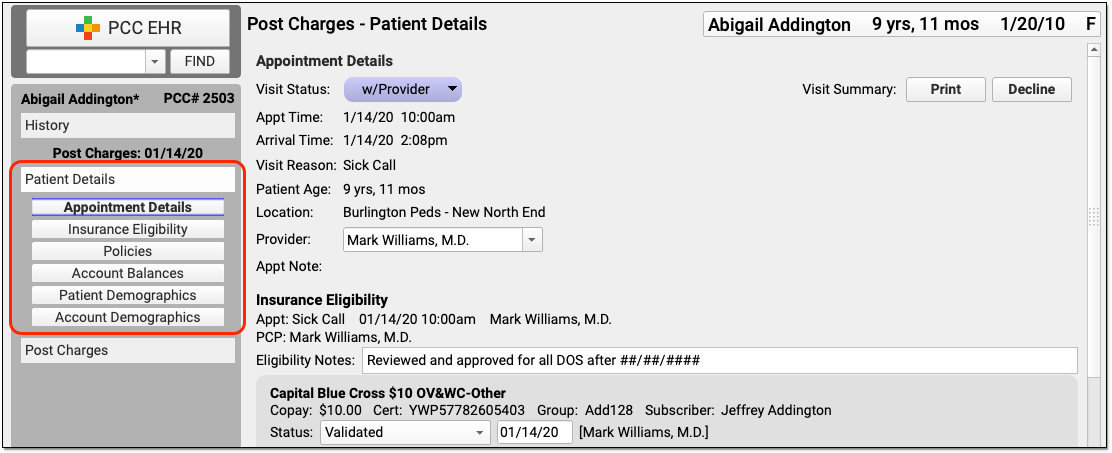
You can customize the Patient Details protocol to include any components your practice will need when they post charges.
Select “Protocols” from the Configuration menu to open the Protocols Configuration window.
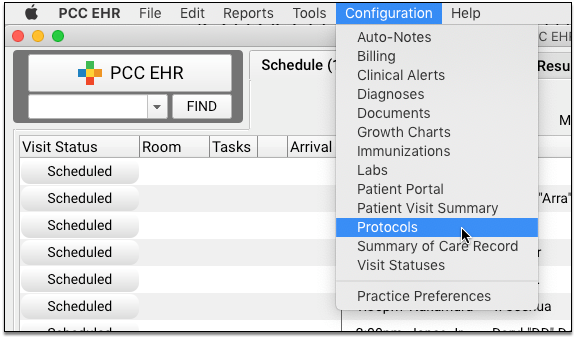
Click “Post Charges – Patient Details” to customize the protocol.
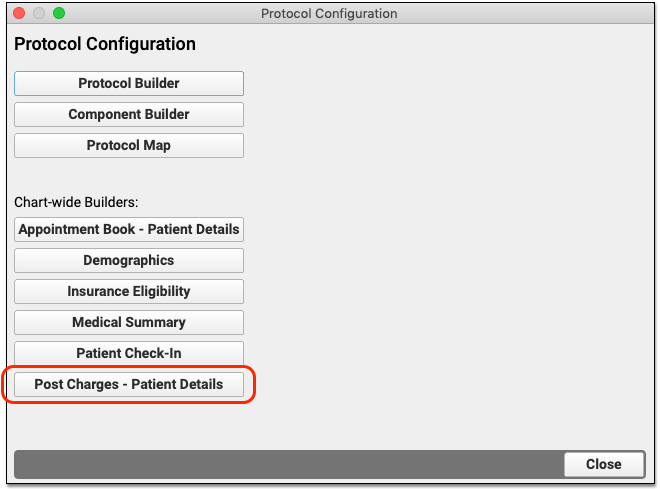
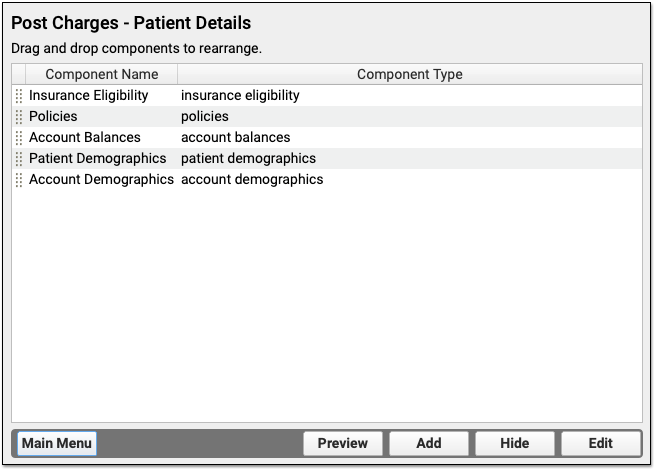
To learn more about how to add and customize components on a protocol, visit the Configure Chart Notes and PCC EHR Components section of learn.pcc.com.
Configure Clinicians, Locations, Procedures and Prices, Claim Behavior, and More
In addition to the items above, there are many aspects of your PCC system that relate to charge posting. For help with any configuration option or maintenance need, talk to PCC Support.
Configure Clinicians
Contact PCC Support for help configuring which clinicians are selected automatically as the billing provider and to set up per-payor claim configuration for clinicians.
Update Your Practices Procedures and Prices
Read Edit Your Practice’s Procedures, Codes, Adjustments, and Prices to learn how to manage your practices codes and prices.
Configure Locations as Subparts of a Main Billing Location
If your practice bills for several facilities, such as when you have a multiple locations across town, you can designate that a location is a subpart of your main billing location.
To make the change, contact PCC Support and ask them to configure one of your locations as a subpart of a main billing location for claim purposes.
Your PCC system will then automatically use the correct logic to include (or leave out) service facility location information based on electronic claim standards and your practice’s configuration.
Why and How Pediatric Practices Should Launch a Recall Initiative Today
Pediatric practices are navigating a new and urgent challenge: massive shifts in federal Medicaid and vaccine policy. With the conclusion of continuous enrollment protections, millions of children are at risk of losing Medicaid coverage, while new recommendations for COVID-19, RSV, and flu vaccines require clear communication with families.
These changes threaten to disrupt continuity of care and lower immunization rates across the country. To counteract this, practices must be more proactive than ever. PCC recommends that all practices launch a strategic patient recall initiative now to ensure families are informed, their coverage is active, and their children remain up to date on essential preventative care.
Why Should My Practice Increase Patient Recall Efforts Now?
If you are concerned about Medicaid cuts and vaccine policy changes, chances are that some of your patients and families are too. You can use this opportunity to support and guide the families that you serve, and get your patients treated while they are still covered.
Here’s why PCC recommends that every practice perform patient recalls:
-
Respond to Medicaid Changes: Upcoming changes to Medicaid may affect your patients and families. See your Medicaid patients while they still have coverage.
-
Respond to Vaccine Policy Changes: Upcoming changes to vaccine policies will affect the overall health of the community that your practice serves. Protect your patients and community by keeping your patients up to date on their immunizations.
-
Vaccines Protect Herd Immunity: Vaccination of the majority of the population prevents outbreaks of vaccine-preventable diseases and protects the most vulnerable members of our communities.
-
Preventative Care is Always Beneficial: AAP strongly encourages pediatricians to continue with their preventive care services. Every missed Bright Futures guideline is an evidence-based lost opportunity to address important developmental issues with children. Pediatric practices are on the front lines for issues around vision, hearing, height, weight, dental health, depression, ADHD, lead, and more.
-
Pediatricians Identify Abuse and Neglect: Pediatricians, teachers, and other mandated reporters who provide direct care are on the front line of identifying abuse and neglect.
-
Your Performance-Based Measures Are Still In Play: Practices receiving performance-based payments nearly always depend on the services performed during preventive care visits.
Inform Patients of the Value of Vaccines
Make sure that your vaccine policy is up-to-date and written in a way that is accessible to the population that you serve. When you share your policy with families, consider referencing recommendations from the AAP and your state’s health department that support preventive care and chronic disease management visits.
Does your practice use ShotBlocker, Buzzy, or colorful ice packs for fearful patients? When you reach out about vaccine clinics, share what makes your practice special, and emphasize how you’re going to take care of your patients and families during their visit.
Adjust Your Workflows to Accommodate Patient Recall Efforts
As you plan for a patient recall initiative, your practice should decide which kinds of visits you are prioritizing, and make adjustments to your workflows accordingly.
- When patients are in for a sick visit, make sure they have their next well visit scheduled before they leave your office.
- “Supersize” your well visits: When your well check patients are behind on their med checks or immunizations, take the time to get your patients caught up.
- Consider the time of year when you are planning your recall efforts. For example, in the fall you can run a report of patients who are due for asthma rechecks and give them their flu shot while they’re in the office.
- Schedule your well visit recall reports to run monthly. You can filter these these reports further and send batch notifications at your practice’s convenience.
- If your looking for a smaller grouping of patients to recall, consider filtering by patient age. These can be individual reports that are saved and scheduled.
- Check that you are using up-to-date charting protocols that support your conversations with families about vaccine-preventable diseases. Make sure that you have prepared talking points and handouts ahead of your visits.
- Decide which visits you can perform using telemedicine and which will require a vaccine clinic or a longer in-person visit. Your decision may be impacted by payment and resources available to you. Your state’s payment rules and individual practice resources will dictate what is appropriate and possible.
- If your community is struggling with vaccine-preventable diseases, such as Measles, consider how you will screen patients to avoid spreading disease within your office. Plan how you will manage patients with vaccine-preventable diseases who do enter your office.
- Give your recall efforts a personal touch with postcards, birthday cards, or personalized phone calls.
- If you use a third party patient outreach service, set it up to automatically reach out to patients who are overdue for a visit or immunizations.
After evaluating your workflows and making adjustments, you’ll be able to integrate your recall routine into your regular practice administration tasks.
Clean Up Your Patient List Before Doing a Large Recall
Before you contact large groups of your patients, your practice should do a quick review of your active patient lists.
You can run a patient list report in the PCC EHR Report Library and review a list of your active patients (those who have visited your practice in the past 3 years, for example).
Flag any patients that you know should be marked as “inactive”, “transferred”, or “hospital only” (e.g., you saw them as a newborn but they never came to your practice). When you perform your patient recall, you can exclude patients with those flags.
PCC can configure your practice’s system to automatically “autoflag” patients and families based on criteria, such as visit frequency. Contact PCC Support for assistance.
Perform Recalls For Specific Patients and Needs
Which patients should you identify and recall for appointments, and when?
Consider the following groups of patients for your recall:
-
-
Respond to Medicaid Changes: Upcoming changes to Medicaid and vaccine policy may affect your patient population. Get your Medicaid patients seen now, before they lose coverage.
-
Overdue Well: Recall patients who are overdue (or are about to become overdue) for regular well visits. The screening and guidance directed by Bright Futures are vitally important. For a well visit recall walkthrough, read Recall Overdue Patients for Well or Chronic Conditions. Or watch our Recall Patients for Preventative Well Visits video.
-
Overdue Vaccines (Under 2): Recall patients who are overdue (or are about to become overdue) for any of the vaccines recommended by age 2. Preventing a measles outbreak is just as vital and important as ever. For a vaccine recall walkthrough, read Recall Overdue Patients for Vaccines.
-
Overdue Vaccines (Adolescent): Recall patients who are overdue (or are about to become overdue) for any of the adolescent vaccine series (HPV, Meningococcal, TdaP). For a vaccine recall walkthrough, read Recall Overdue Patients for Vaccines.
-
Overdue Vaccines (School/Daycare Required): Recall patients who are overdue (or are about to become overdue) for any of the vaccines needed for daycare or school. Families struggling to manage daycare coverage do not want to be held up by an overdue vaccine. For a vaccine recall walkthrough, read Recall Overdue Patients for Vaccines.
-
High BMI and Obesity Management: Recall patients who have a high BMI % or known obesity concerns. Follow up on nutrition plans and weight management, and provide additional resources these patients may need (for example, how to get healthy meals from school).*
-
Depression and Anxiety: Recall patients who have active depression or anxiety diagnoses (or active meds for these conditions) or other behavioral or developmental concerns.*
-
ADHD: Recall patients who are on ADHD medications who need a followup.*
-
Asthma: Recall patients with asthma diagnoses who need a medication followup or who need an adjustment to their Asthma Action Plans.*
-
Care Plans: Recall patients with active Care Plans that may need review or adjustment.*
-
Referrals: Follow up on open referrals and other incomplete orders. This work is a vital Care Management service.*
-
*Telemedicine-Friendly Visits: These encounters may work well as a telemedicine encounter or phone/portal message encounter. They may not require an in-person visit, and yet they are particularly valuable during a time of high stress and anxiety. If your practice provides integrated mental health services, you can work with your clinicians to develop a patient recall focus in that area.
How to Code and Bill For These Visits
If you have questions about coding and billing for telemedicine or any type of visit, join one of PCC’s billing drop-in weblabs where we discuss coding, billing, and practice management topics. Looking for a reliable coding resource? Check out the AAP’s 2025 Coding for Pediatric Preventative Care handout.
Create a Library of Resources and Links for Your Patients and Families
When you recall and see patients, what additional resources can you provide? PCC recommends you review your standard links, handouts, and materials and expand them to address current topics.
Your practice’s library of resources will engage your patients before and after visits, make your in-person time more efficient and effective, and promote the value of pediatric work.
Use PCC’s Reports and Other Tools to Perform Your Recall
Which tools will you use to recall patients? PCC offers a variety of patient communication tools, summarized in this article.
How will you create a list of patients, filter it based on criteria, and then contact your patients and families?
PCC EHR’s Report Library, which has customizable reports with a wide range of criteria for performing a recall. Patient-based reports also include PCC’s built-in Broadcast Messaging feature, which will allow you to send emails and text messages to your patients and families.
The following reports in the PCC EHR Report Library will help you identify and contact appropriate patients:
-
-
- Preventive Care Recall report
- Chronic Condition Recall report
- Care Plans by Date report
- Vaccine Recall report
- Orders By Visit report (for referrals or other incomplete long-term orders)
-
If you run a patient-based report, you can then click “Export” to send a custom email and/or text message to patients and families. If you use order and procedure based reports (like the Vaccine Recall report and Orders By Visit), you can customize the output to include contact information and export the list.
Learn More By Seeing Examples: To learn how to run recall reports, you can watch the Recall Patients for Preventive Well Visits video, or read example procedures in Recall Overdue Patients for Well or Chronic Condition Visits or Find and Recall Patients Who Are Overdue for Vaccines.
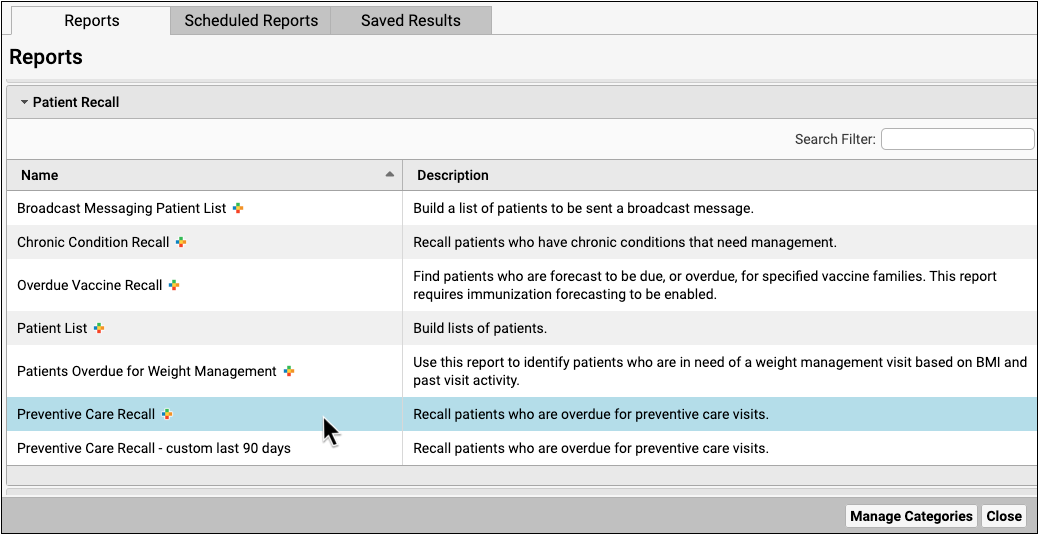
Customize Report Criteria and Output: Want to learn how to customize a PCC EHR report? Watch or read Create a Custom Report (video, article).
If you need help finding, running, or customizing your recall reports to your practice’s specific need, contact PCC Support.
Review Responses and Mass Messaging Details
Did messages go out, and are you reaching patients? If you use PCC’s built-in broadcast messaging features, you can later run the Broadcast Messaging Log report to examine your recall activity. In addition to tracking down missing contact information, your practice can use PCC’s reporting tools to evaluate the visit volume impact of performing a recall.
Read Send Broadcast Messages to Patients and Families or watch the accompanying video to learn more.
Send Chat Messages to Colleagues
PCC EHR includes a chat/instant messaging tool that lets you chat and send messages to other PCC EHR users.
Chat allows you to communicate quickly with the rest of the staff and clinicians at your office without having to log in to another program.
To watch a video about Chat, click here.
Send a New Message
To send a message, click on the “Chat” icon at the bottom of the EHR window.
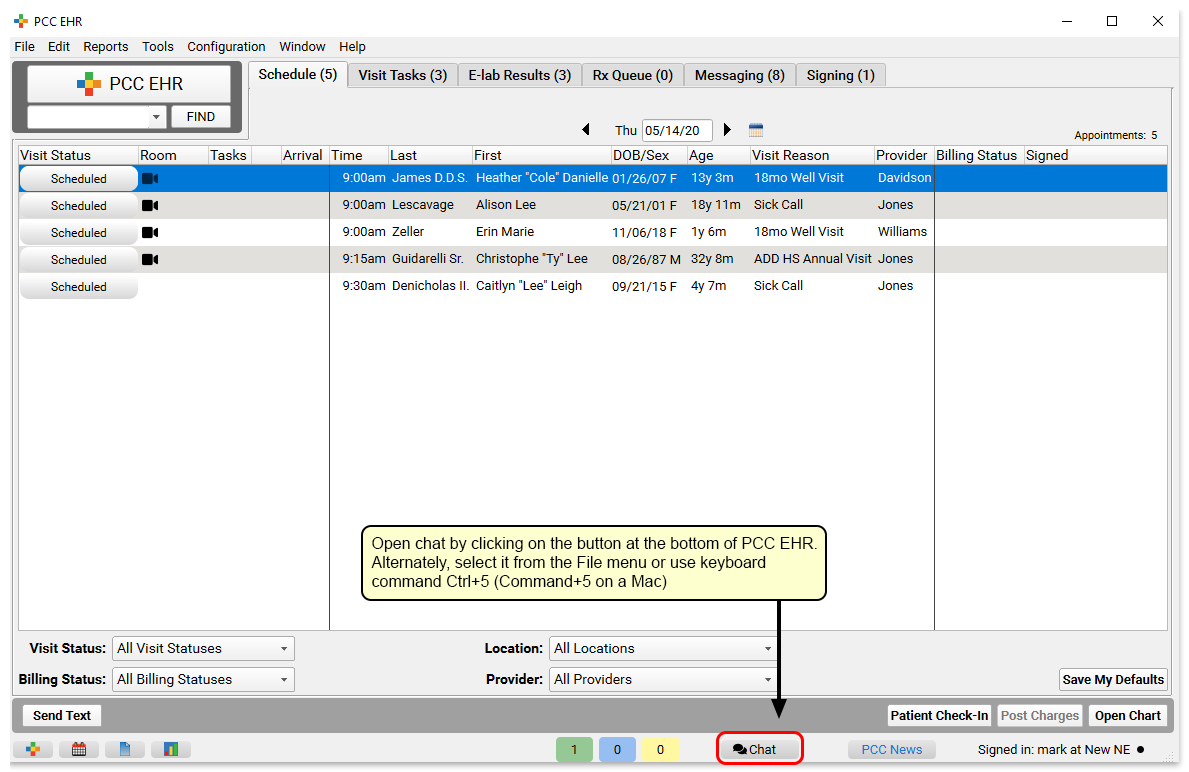
If you have any existing message threads you can find and open them here. Or, simply click on the “New” button to find any PCC EHR user at your practice.
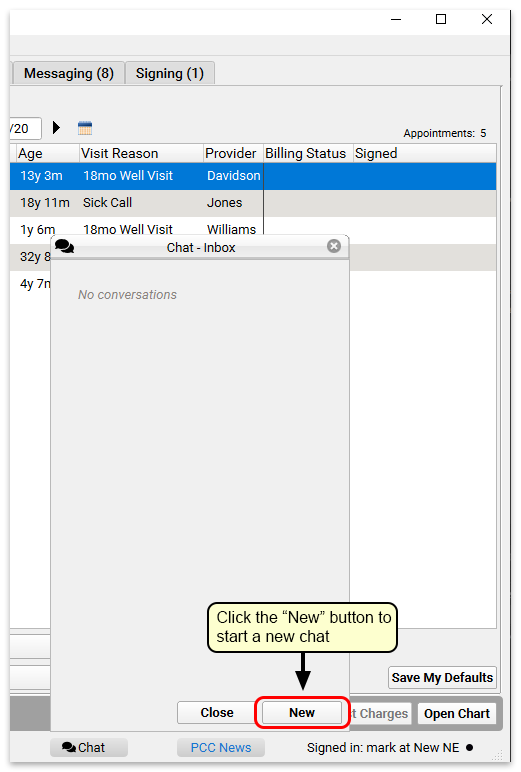
Use the “To:” field to search for the user you want, or select a user using the drop-down menu.
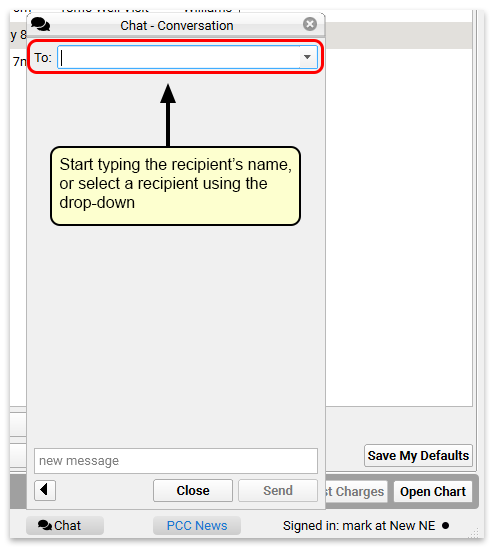
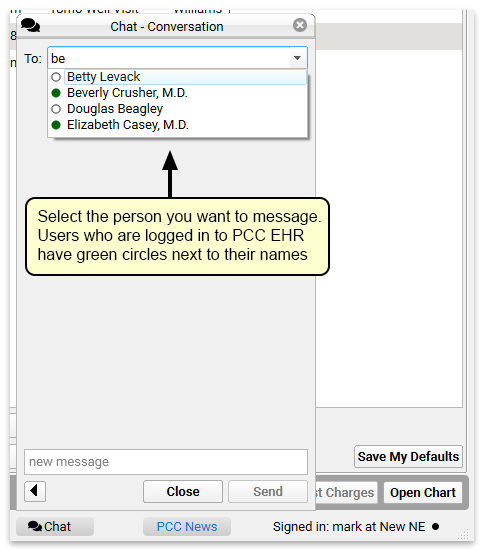
Who is on Chat?: The user list in Chat includes all active PCC EHR users. The order in which they appear is controlled by the settings in the User Selection List in the User Administration tool. If your practice uses Care Center functionality, users from your Care Center will always appear at the top of the list.
Then simply begin typing. Other users will be notified that they have a new chat message, and can respond. If you have the chat window open, it will automatically refresh as the conversation continues.
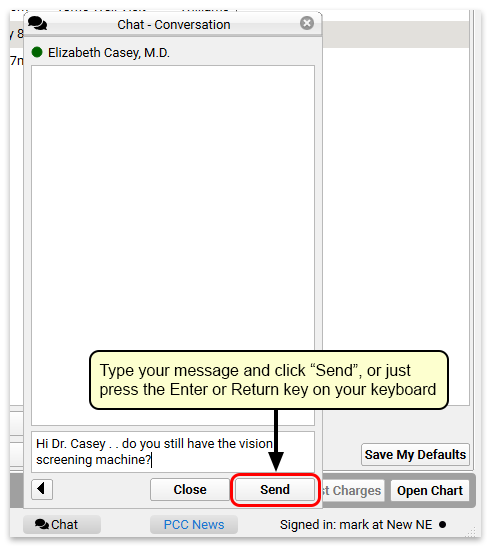
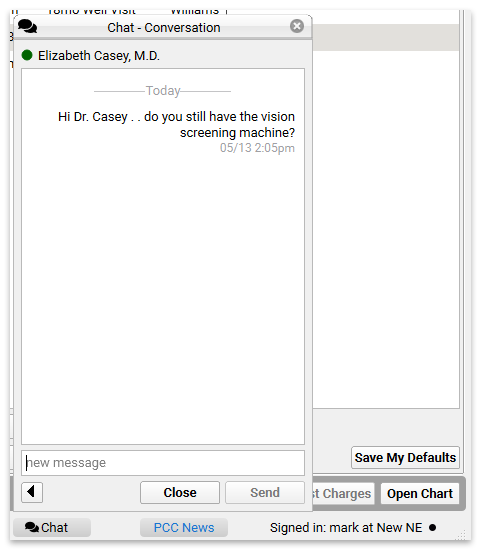
When you get a reply, it will appear instantly in the chat window. All chat messages are time stamped, so you can see exactly when they arrived.
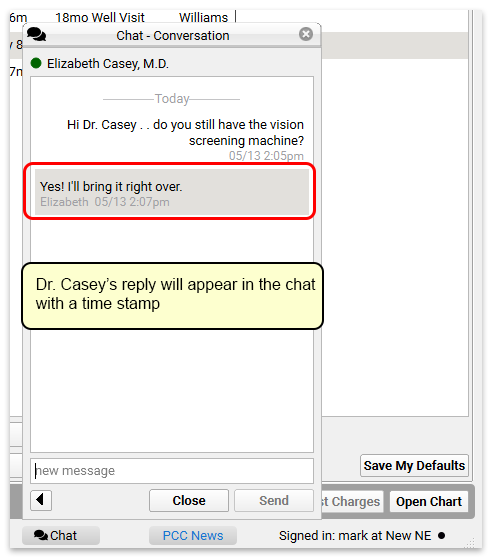
Close the chat using the “Close” button, or use the back arrow to return to the Chat inbox.
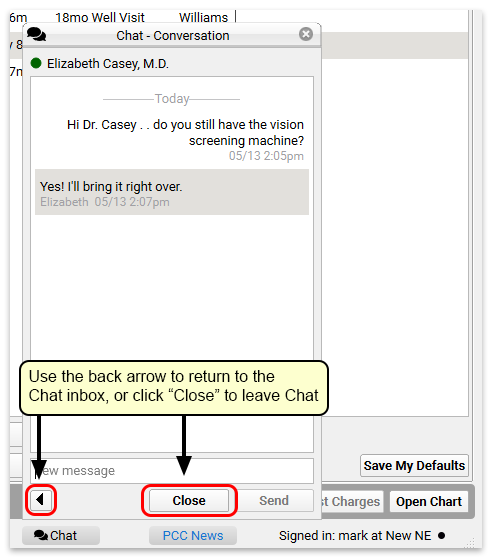
Receiving Messages and Message Notifications
When you have new messages, the Chat icon at the bottom of the PCC EHR window will indicate that you have messages waiting with a red circle.
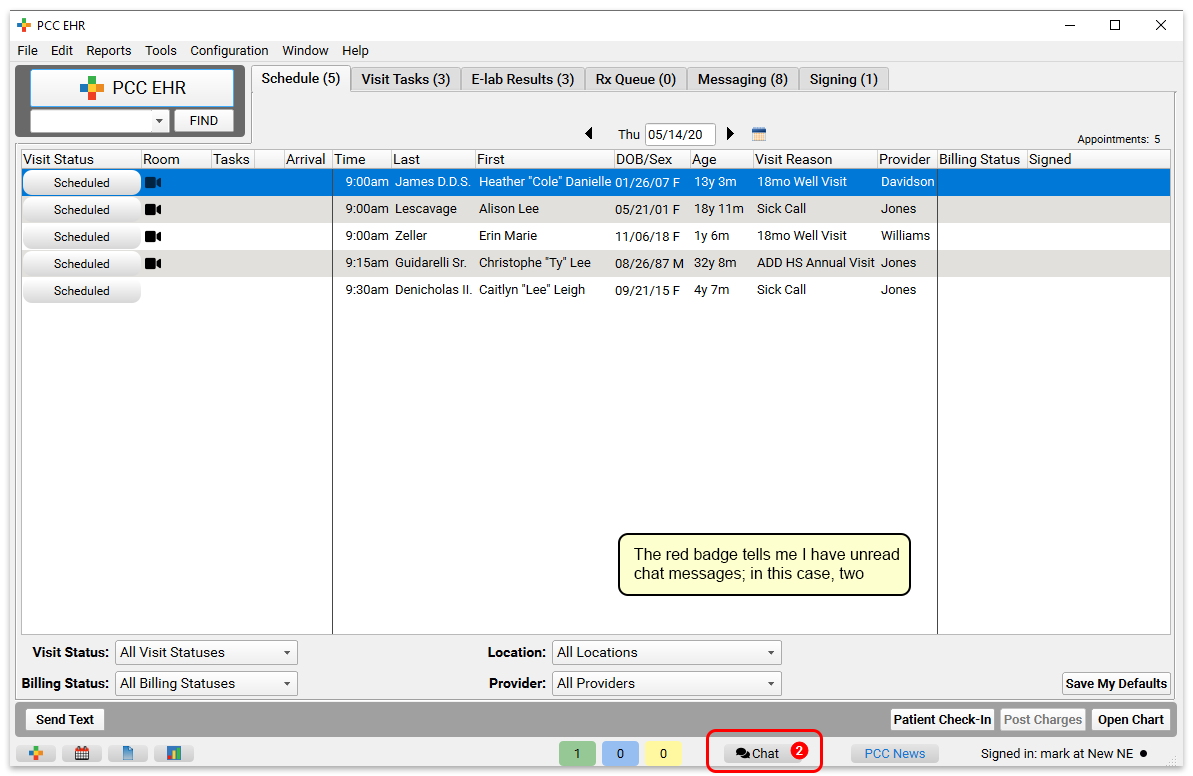
When you open Chat, you will see unread messages at the top of the of your Chat inbox in bold. Click a message to open the conversation and reply.
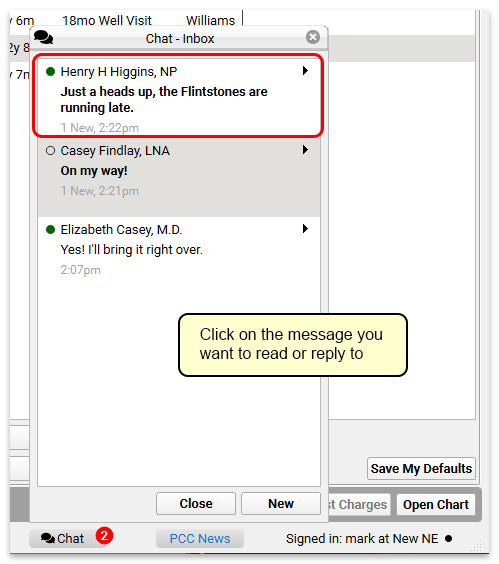
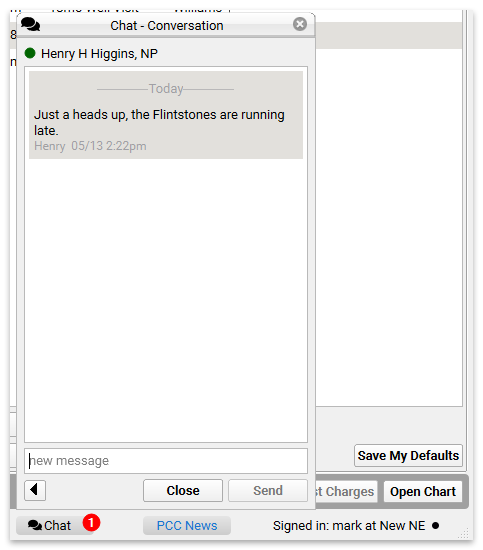
Reply to the message, and then either return to the Chat inbox, or close Chat and continue with your work.
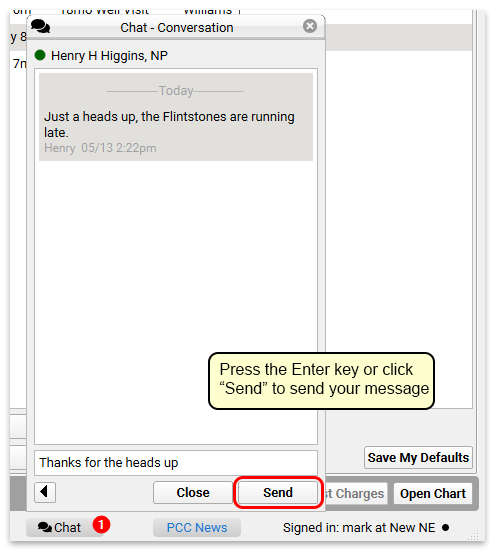
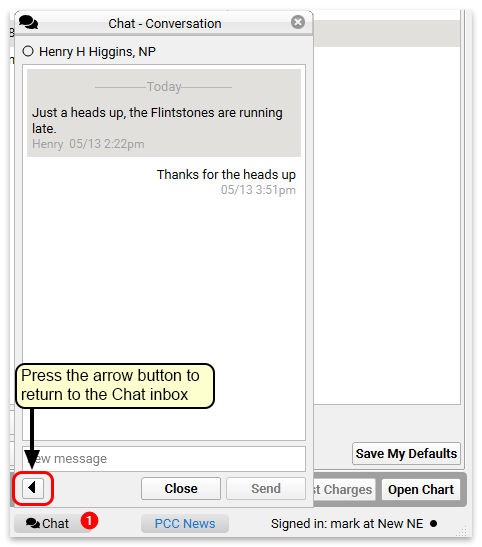
Chat History is saved in PCC EHR: All chat messages are saved in PCC EHR. Scrolling back through a conversation will reveal the entire chat history between two users.
Chat with Groups of Users
You can create groups of users to send messages and converse with the full group of users, all at once.
Create, manage and edit groups through the User Administration tool’s Chat Groups tab. Click “Add Group” to create a new group of users.
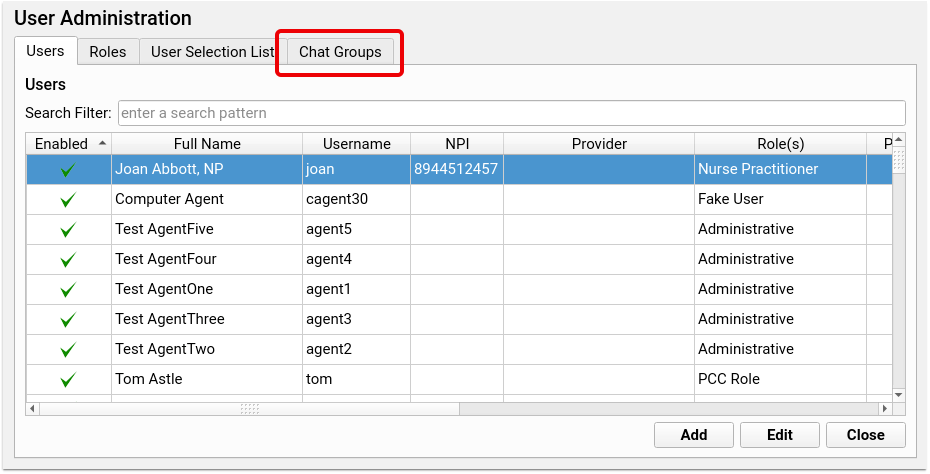
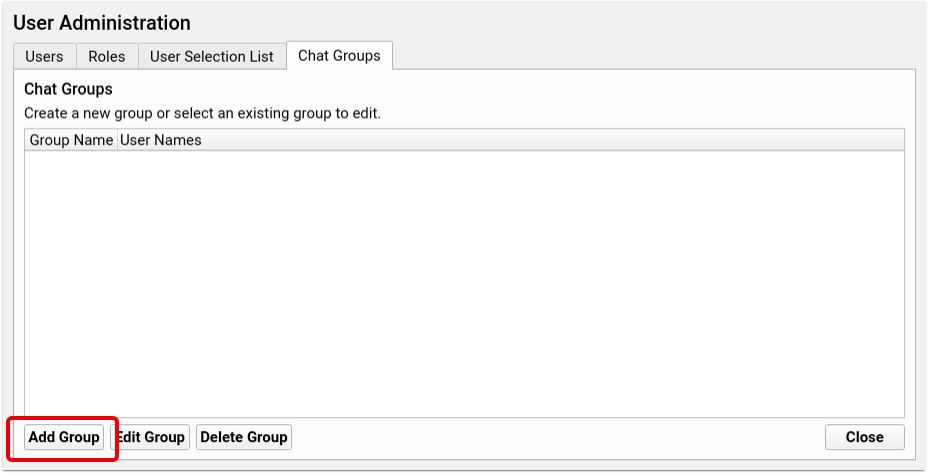
Check the box alongside each user’s name to add that user to the new group. Name the group at the top of the window and click save. Each group name can only be used once, so you won’t be able to duplicate group names, but to avoid confusion, be sure that your group names don’t match existing users. For example, if you have a user called “Nurse” make sure to name your group of nurses something like “Nurse Group” to differentiate the group from the individual.
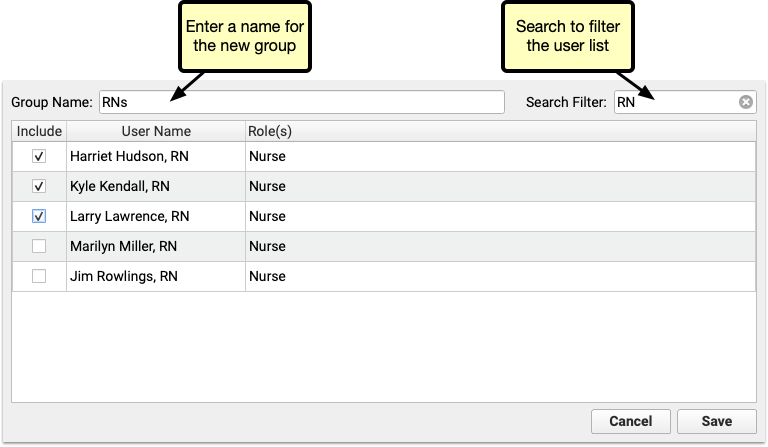
When you’ve created one or more groups, they’re available in the chat window’s “To” menu, at the bottom of the list of users.
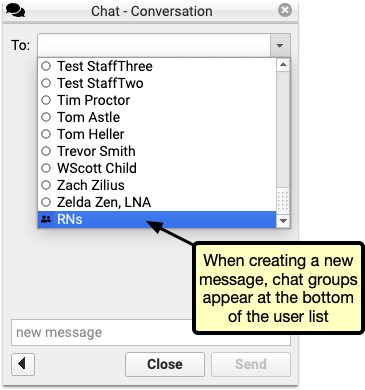
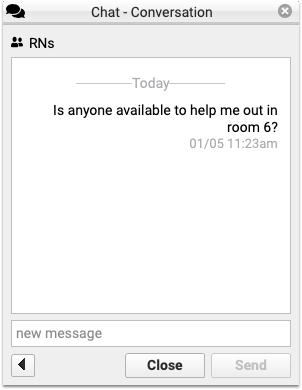
The message appears to the whole group, and any replies will be marked with the replying user’s name.
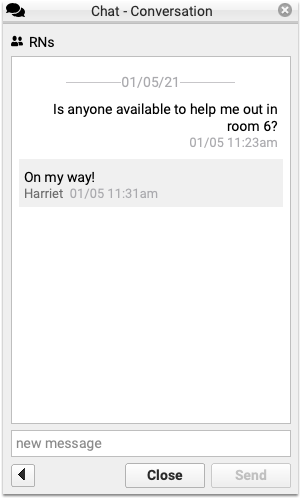
You can edit or delete groups at any time in the User Administration tool. To add or remove users, or rename a group, select the group in the Chat Groups tab and click Edit.
Check or uncheck the box to add or remove a user, then click Save.
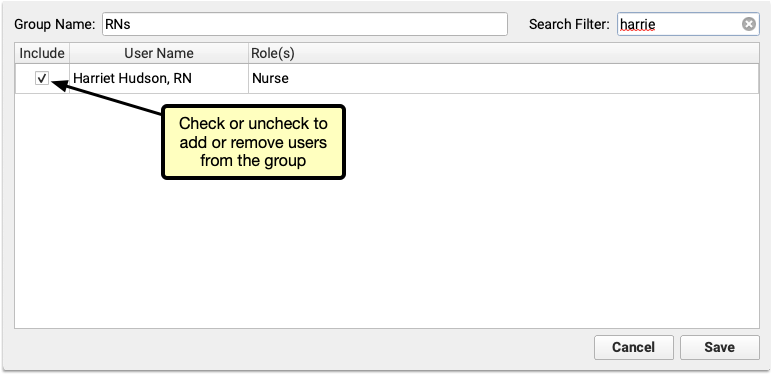
When a user is removed from the group, they’ll still be able to see the message history, but will no longer see any new messages or have the option to send messages to the group.

If your practice deletes a group, the same is true. Each user will be able to see the history of the conversation, but the option to send a message will be removed, and replaced with “This conversation is closed.”
Expand Short Text into Common Phrases in PCC EHR
Use PCC EHR’s Snap Text to enter commonly used words, phrases, or longer texts with just a few keystrokes.
To watch a video about Snap Text in PCC EHR, click here.
Each user can customize their own personal Snap Text and your office can set practice-wide entries for all users.
Set User Permissions
Creating and managing the practice-wide Snap Text list is accessible via the User Administration tool. To add permission to user role, open the User Administration tool and visit the Roles tab, select a role, and check the Snap Text Configuration box.
Open the User Administration tool and visit the Roles tab, select a role, and check the Snap Text Configuration box.
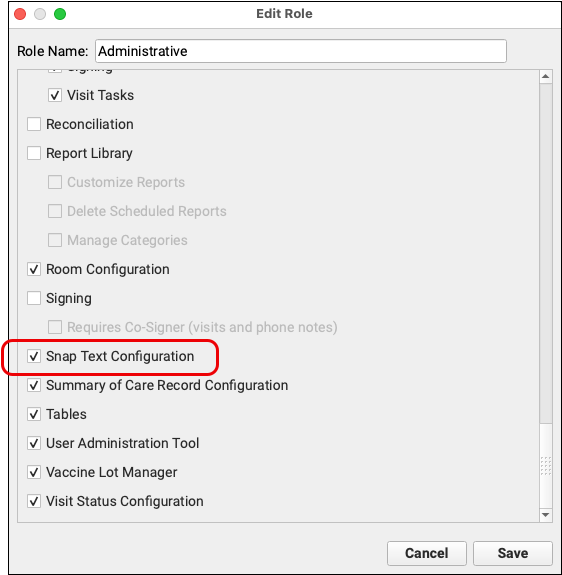
For a more detailed guide to setting up roles and configuring user permissions, read Set User Roles for Permissions and Security.
Create Snap Texts
Open My Account within PCC EHR’s File menu and select the Snap Text tab.
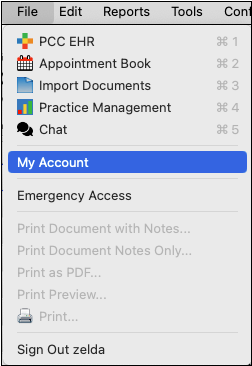
Each user is listed in the drop down menu on the upper right. By default your PCC EHR account is selected.
Here, you’ll find two columns, one for the typed text and one for the expanded text.
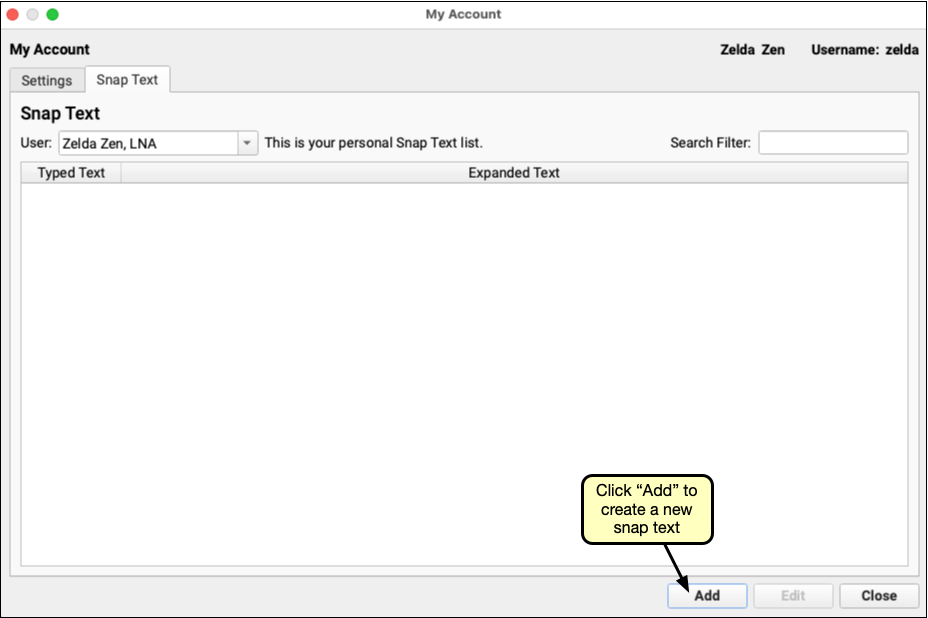
To add a new Snap Text, click “Add.” Enter the typed text in the first field, and the full, expanded, text in the second. The short text should be a few characters long, and the expanded text can be as long as you need.
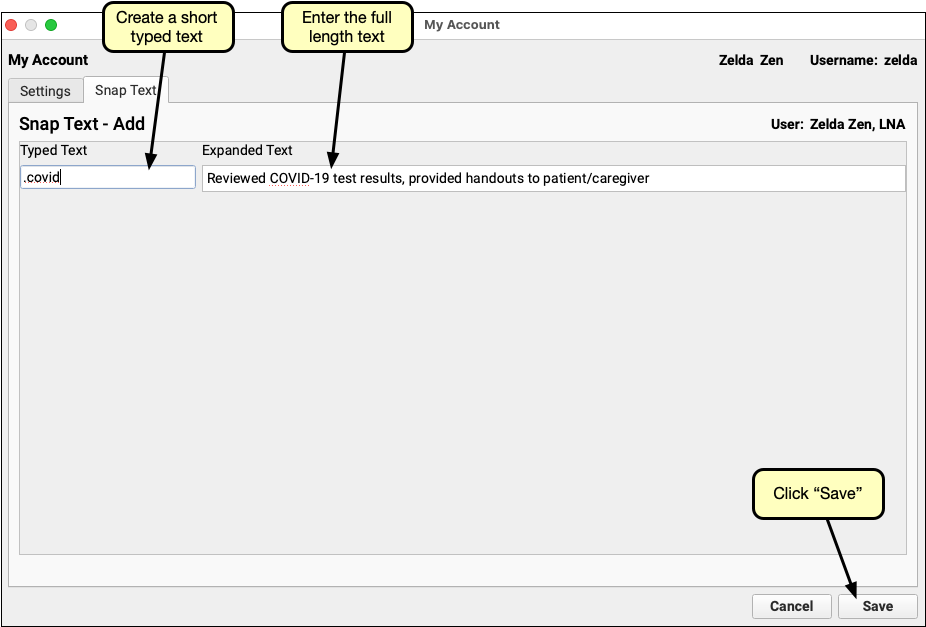
Typed text can be any combination of characters. It is case sensitive, so the expanded text will only be triggered if the letter case matches. That also means that “ABC” and “abc” can both be used to trigger different expanded texts.
Avoid Common Words, Use a Prefix Character: Whatever short codes you enter will be automatically replaced by the expanded text. Avoid using real words that might be used in a different context. Consider using a special character prefix before your code. For example, “.adhd” to expand to “Attention Deficit Hyperactivity Disorder” while still leaving “adhd” available to be used without being expanded.
Click Save, and you’ll be returned to the Snap Text tab, where you can add another or Save and Exit.
The Practice Defaults list, managed by users with permission, as described above, are available to all users automatically. If a user creates a Snap Text in their own list that matches a practice default typed text, the user’s snap text will take precedence over the practice default for that user.
Copy And Edit Snap Texts
Each user can view, but not edit, the snap texts of other users.
When reviewing another user’s entries, any user can copy entries to their own list by using the copy button at the bottom of the tab.
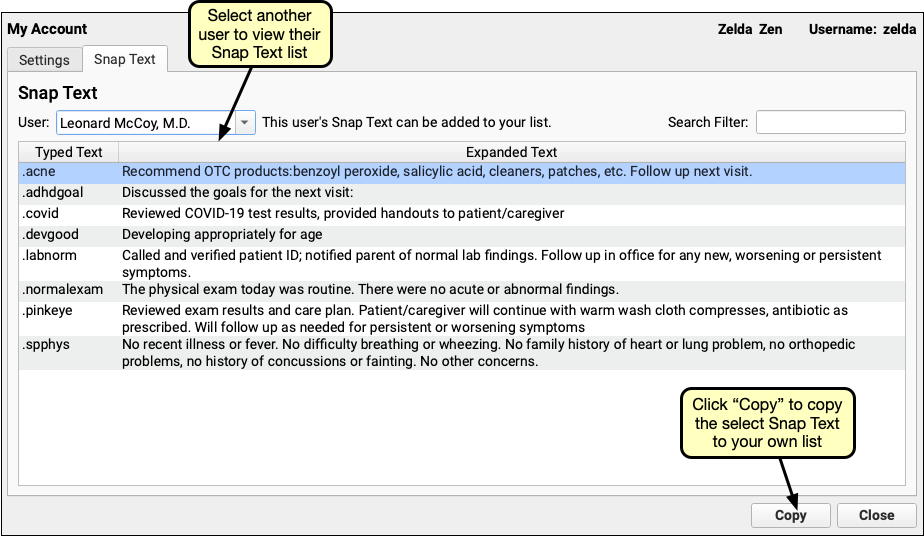
Any of your own snap texts, even those copied from other users, can be edited by selecting it from your list, and clicking the edit button. Simply change the text, or if it’s no longer needed, click the delete button to delete it from your list.
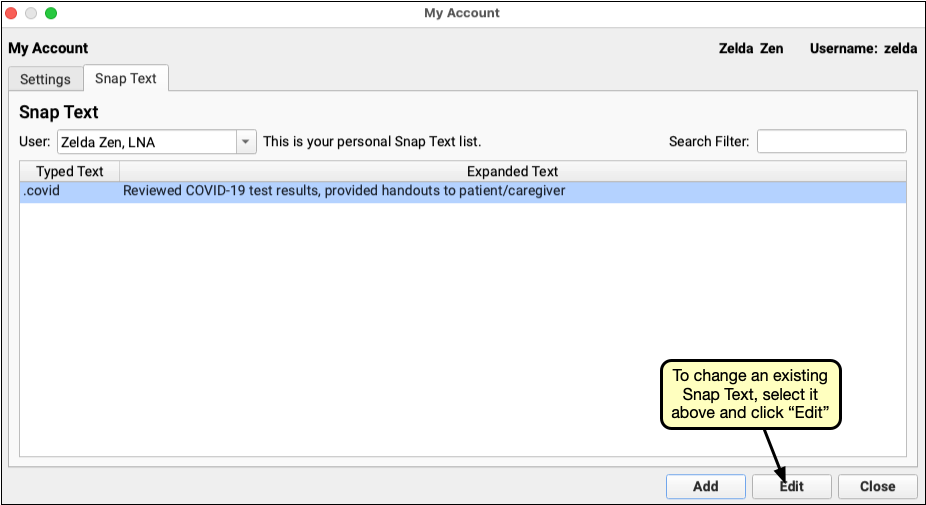
To find and edit or copy specific texts, use the Search Filter to find all texts, both typed and expanded, containing a word or phrase.
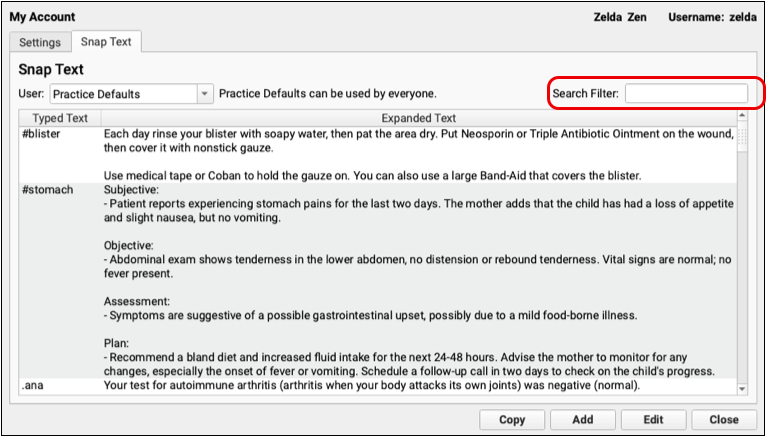
Using Snap Texts
Type any of your short typed texts into a PCC EHR text field, and the expanded text will automatically replace the short text when you type a space, or in the case of multi-line text fields, enter or return. After text is expanded, you can use ctrl.+z or select “Undo” from the Edit menu, to remove the expanded text and return to the short typed text.
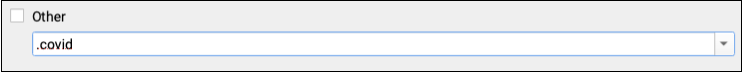
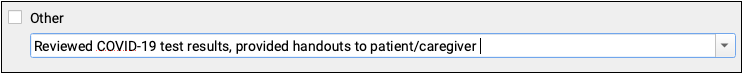
Alternately, instead of memorizing and typing your short texts, you can open a list of your Snap Texts by typing Ctrl+Shift+. or, on a Mac, command+Shift+..
You can also right-click or control-click and select “Insert Snap Text” to open the list of snap texts. Select one, or begin typing to search both the short and expanded text columns.
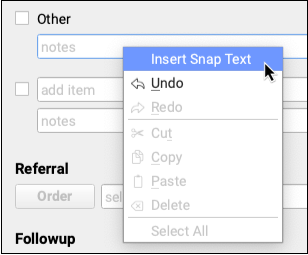
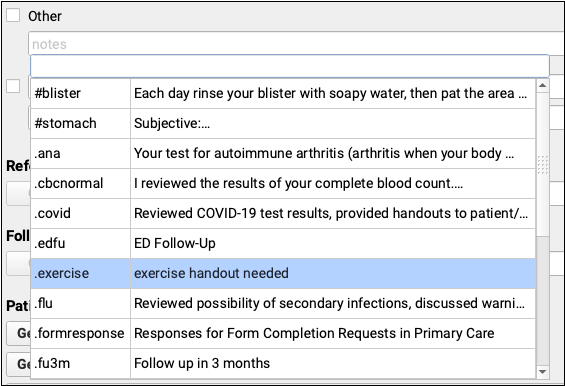
Change an Encounter’s Billing Place of Service After Posting Charges
You can adjust an encounter’s place of service when you post charges.
Sometimes you need to change the place of service of an encounter after the charges have already been posted.
Select the encounter in the Billing History in the patient’s chart. Then click “Edit Charges”.
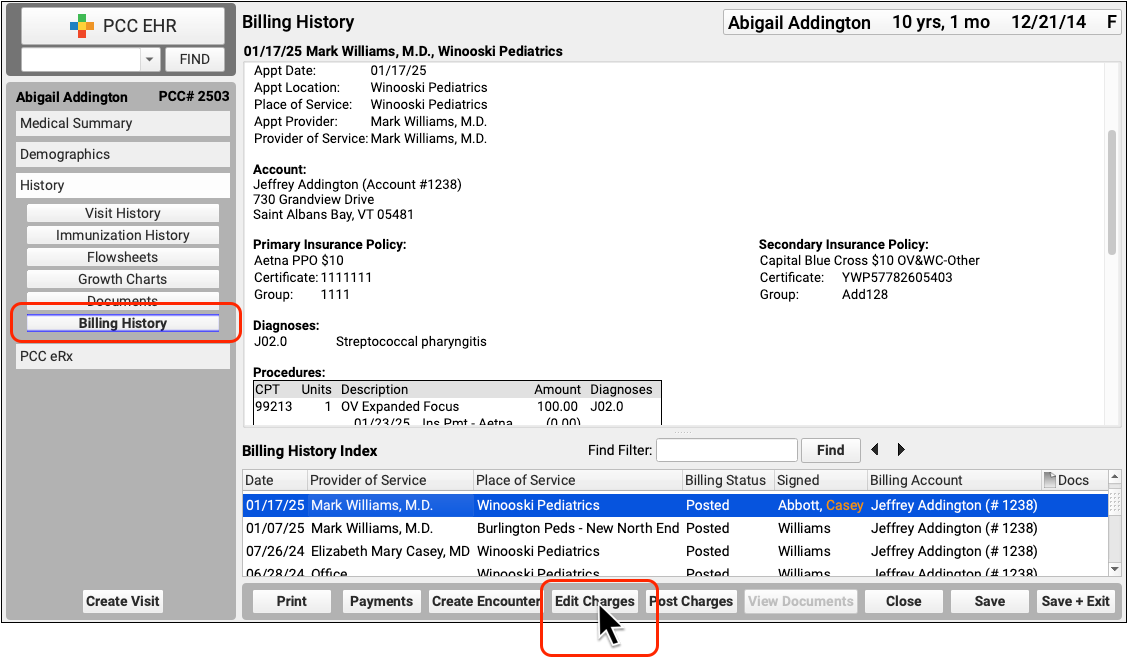
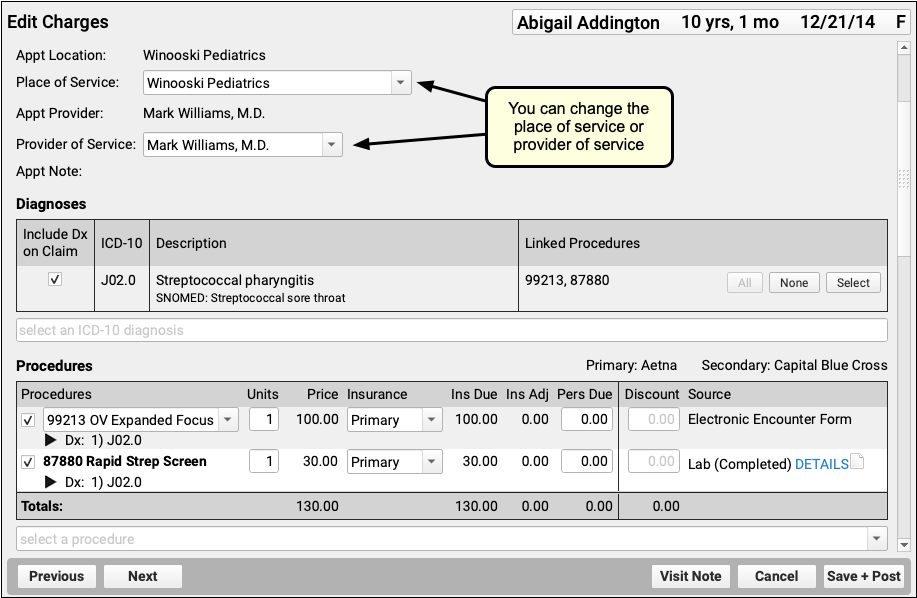
Next, edit the encounter’s location, or any other information about the encounter. Then click “Save + Post”.
For more information, including how to make other changes and queue up a claim, see Edit Encounter Charges and Other Claim Information.
Analyze and Respond to COVID-19’s Impact in Your Dashboard
Use the COVID-19 section of your Practice Vitals Dashboard to see how the crisis is impacting your practice and what you can do to respond.
Open the Dashboard and Review COVID-19 Impacts
To log into your Practice Vitals Dashboard, select “Practice Vitals Dashboard” from the Reports menu.
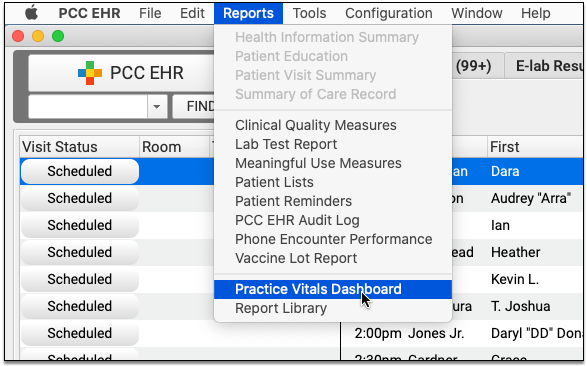
Click on the new COVID-19 tab to review trends and metrics specific to your practice.
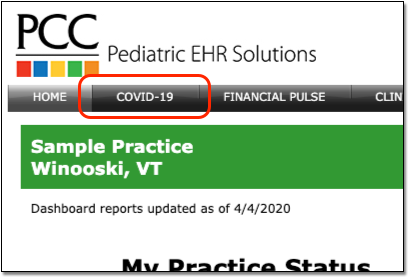
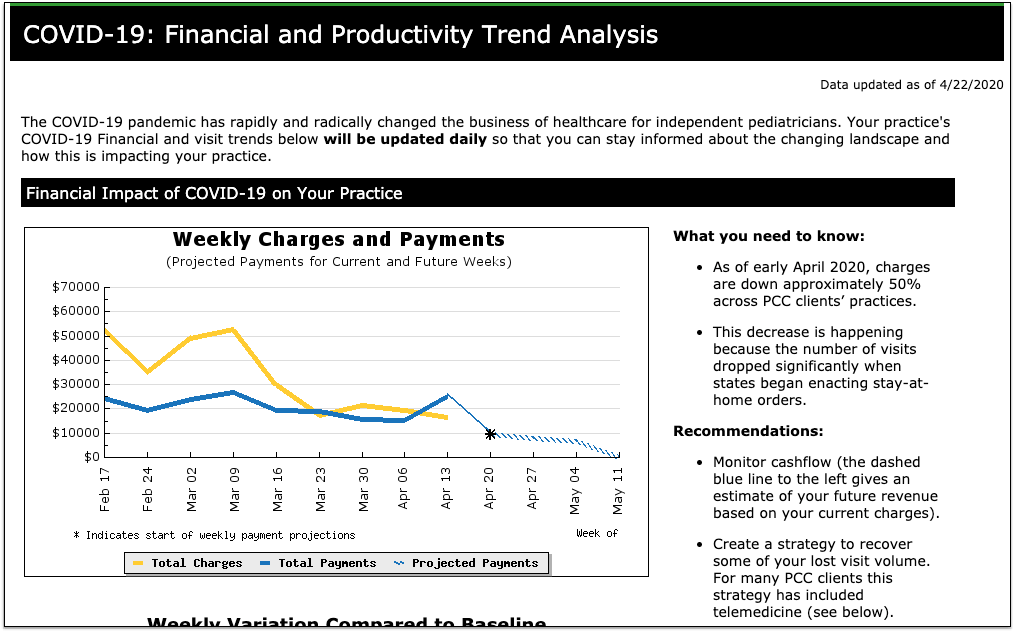
Graphs are based on weeks, going back to 2/17 as a pre-coronavirus baseline. Data points are updated live from your practice every morning.
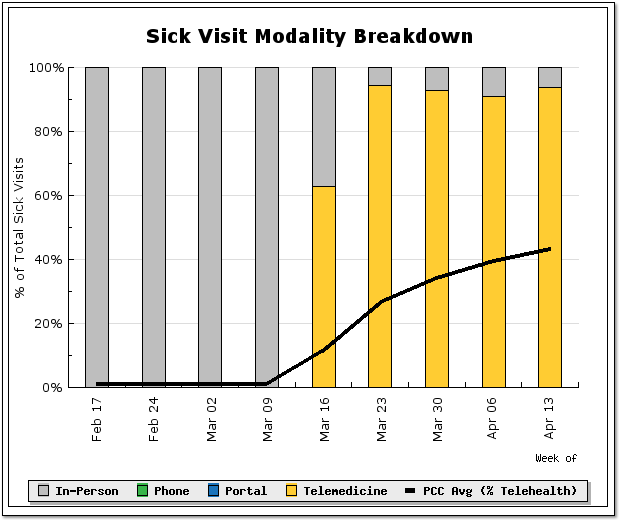
COVID-19 has an effect on your practice’s charges and payments (cashflow), your visit volume, and how you see patients. The new dashboard section visualizes those impacts based on data from your PCC system, and it also provides explanations and ways to take action.
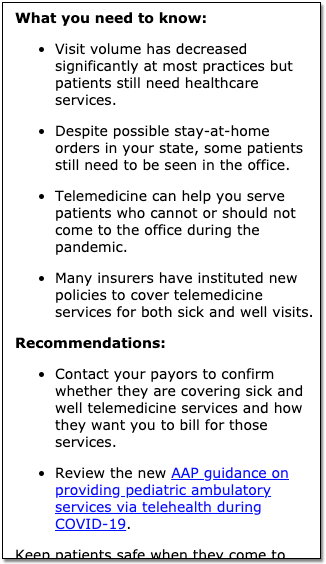
To see graphs and analysis based on data from pediatric practices around the country, visit The Business Impact of COVID-19 on Pediatric Practices.
How Often Does COVID-19 Dashboard Data Update?: Your PCC system automatically updates your COVID-19 Dashboard numbers every night. Since many data points are based on weekly totals, you may not notice changes every day.
See How Well Your Payors are Paying for Telemedicine Sick Visits
Do your payers pay you for telemedicine sick visits, and do they do so on par with payment for in-person sick visits? Use the new Telemedicine Payment Parity section of your Practice Vitals Dashboard to find out. This section was added to all practice dashboards during the 8.13 release cycle, in June of 2020.
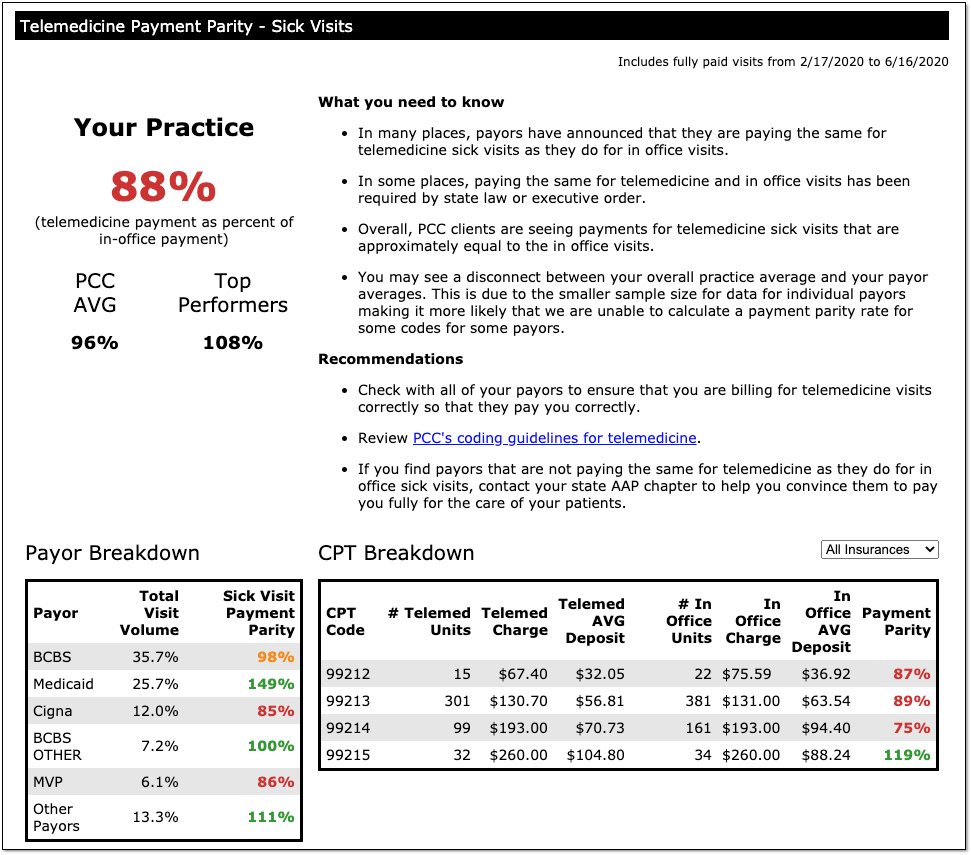
The overall practice percentage summarizes how well you are being paid for telemedicine sick visits versus in-person visits, and compares your payment parity rate to other PCC practices.
The Dashboard also displays a breakdown of your top five payors: You can see what their percentage is of your total visit volume, and then see how well they are paying for telemedicine sick visits versus in-person sick visits.
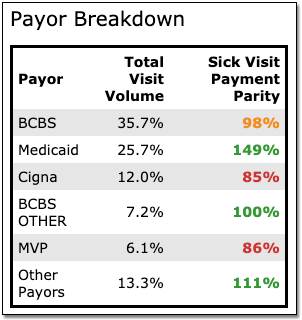
Is a specific payor paying you on par for 99214s, but paying you less for 99213s? The CPT Breakdown section shows which visit codes are being paid on par and which are falling short. You can choose to look at all insurances or just one specific payor.
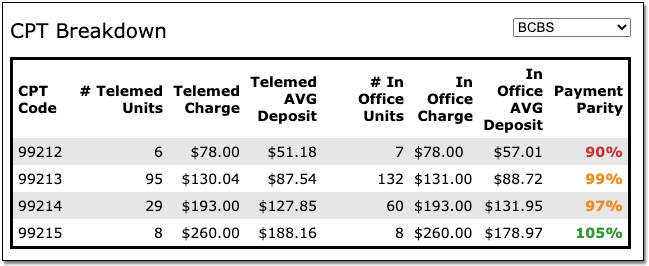
PCC updates the Telemedicine Payment Parity numbers, along with the rest of the data on the COVID-19 dashboard, every day. For questions or help interpreting your numbers, contact PCC.
100% Parity or Greater Doesn't Always Mean Telemedicine Pays Better: You might notice that your overall score, or that of a certain payor, exceeds 100%. This usually does not indicate that telemedicine sick visits pay better than those conducted in-person. It is more commonly a reflection of how many telemedicine visits you are billing to each payor, and what proportion of your overall visit volume they represent. If you have questions about your payment parity score, please contact PCC.
Payment Projections for Your Practice
The COVID-19 dashboard includes short-term payment projections for your practice in the “Weekly Charges and Payments” graph.
The dashboard creates these projections based on your daily charges, your average collection rate (a ratio between payments and charges), and your typical A/R days (an approximation of how long it takes you to get paid for a charge).
Your actual collection rate may not match its historical value. As practices shift to more telemedicine visits, collection ratio may drop.
Note also that these projections only include charges your practice has posted for billing. If current circumstances lead to a delay in posting, your A/R days will climb. PCC recommends you post all charges and submit claims daily, and your practice can use the new Post Charges workflow in PCC EHR to speed up that process.
Visit Categorization Update
PCC recently adjusted the default categorization of visits for many reports. Just as you can now see data on your Telemedicine and Phone visit rates in your Practice Vitals Dashboard, you may also see those categories in financial and charge-based reports in the Smart Report Suite in Practice Management.
If your practice previously used a custom visit category configuration (in order to break out mental health visits, for example), we did not adjust your configuration for Practice Management reports. Contact PCC Support to make changes to report configuration for visit categories or any other configuration needs.
Configure PCC EHR for Telemedicine Encounters
Read the sections below to learn how to configure PCC EHR for telemedicine encounters.
Read or Watch a Telemedicine Procedure in PCC EHR: How will your front desk, clinicians, and billers perform telemedicine in PCC EHR? Before you dive into the configuration options below, read or watch Schedule, Chart, or Bill a Telemedicine Encounter in PCC EHR (watch video, read article).
Create Telemedicine Visit Reasons for Scheduling
When you schedule, perform, or bill a telemedicine visit, it should be clear to everyone at your practice that the encounter is happening remotely.
Open the Visit Reasons Editor from the Configuration menu and create one or more visit reasons for telemedicine.
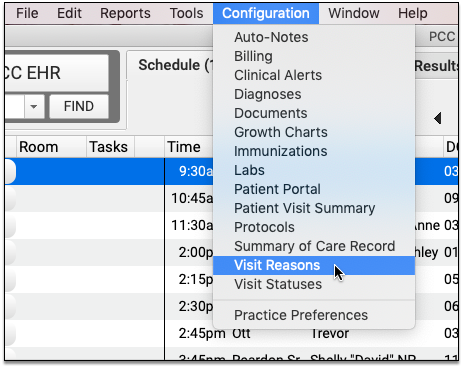
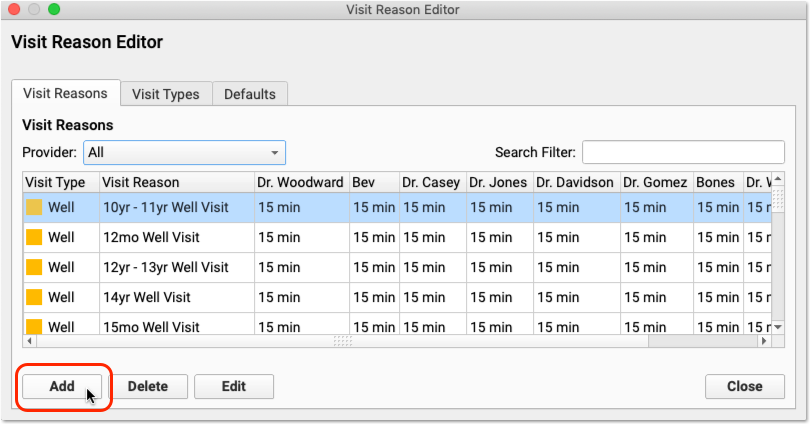
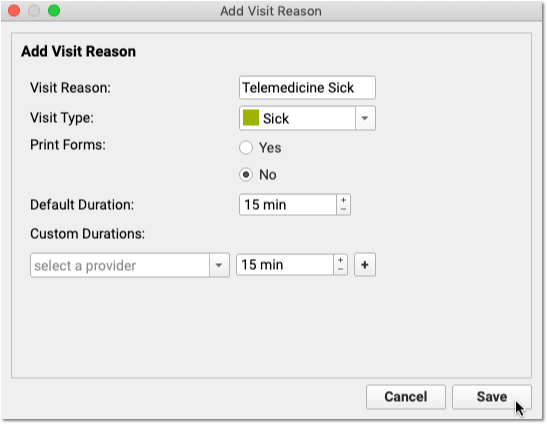
Click “Add” to create a new visit reason. You can name the visit reason, indicate the Visit Type (for helping schedulers pick appropriate times), set whether your practice should print paper forms for the visit, and set both a default duration and optional specific default durations for each clinician.
If your practice commonly performs sick visit and ADHD telemedicine visits, you could create a visit reason (and an accompanying chart note protocol) for each type of visit.
Select Your Telemedicine Vendor
Your practice can choose from a wide range of telemedicine vendors.
PCC has done some research and developed a list of telemedicine vendor options that we believe can provide efficient, safe, and reliable interactions with your patients and families.
Once you’ve chosen a vendor, your practice will need to figure out your workflow for connecting to visits.
Configure Telemedicine Links for Your Providers and Patients
If everyone in your practice is using the same tool, and the vendor supports it, you may have a persistent set of URL web addresses that patients and providers can use to connect.
You can enter those addresses in Practice Preferences.
If you have persistent links for patients, you can enter them in the Patient Access fields
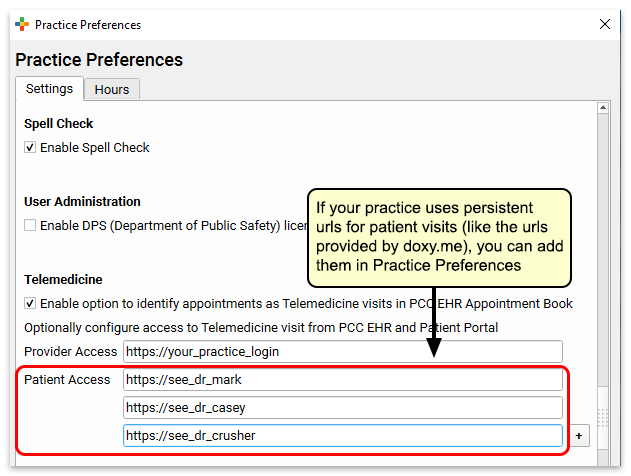
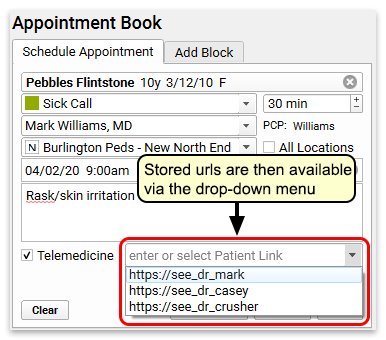
Your practice can then quickly select a link when they schedule or edit appointments.
If you have a persistent link for provider access, you can enter it in the Provider Access field.
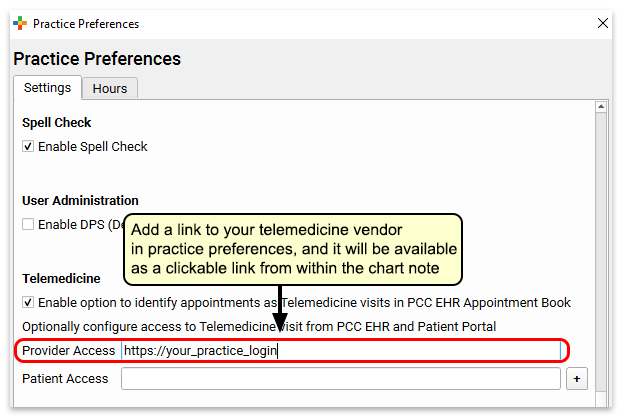
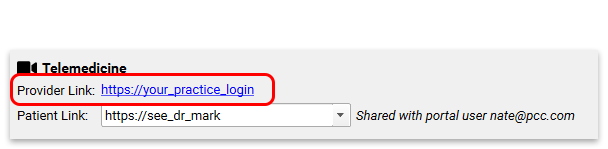
Both the provider and patient links will appear at the top of the chart note protocol for a telemedicine visit.
Add New Visit Statuses to Help Manage Telemedicine Visits
The Visit Status on the Schedule screen (and the Visit Status counters in the lower-right corner of your screen) help your practice track what’s going on with all of today’s encounters.
Your practice can create one or more custom Visit Statuses to help understand the status of telemedicine encounters.
Open Visit Status Configuration from the Configuration menu and create one or more visit statuses for telemedicine.
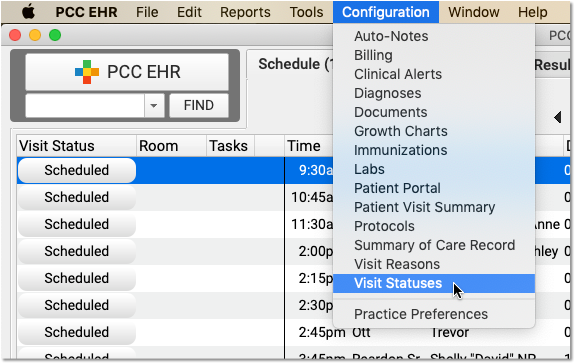
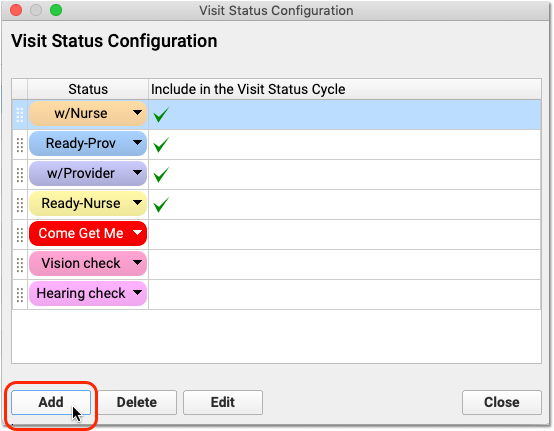
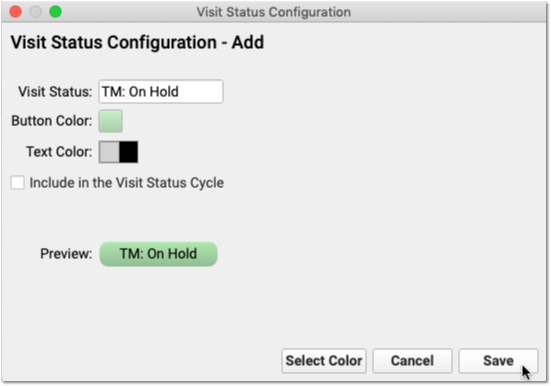
Your practice can use visit statuses so everyone at your practice can know who is on hold, who’s connected, and who is waiting for the provider to join the video chat.
Create a Telemedicine Visit Protocol
In PCC EHR, you can create and customize chart note protocols for different visit types. PCC recommends you create a “Telemedicine Sick” protocol, along with other telemedicine-based protocols you expect to schedule. You can then have that protocol appear automatically for Telemedicine visits.
You can include any typical component in your chart note protocol, and you may want to create custom components or new orders that relate specifically to the types of services that will occur as a result of a telemedicine visit.
To learn how to create and customize a Telemedicine protocol, and find out what other pediatricians are making, read Create a Telemedicine Chart Note Protocol.
Add Telemedicine Procedure Codes and Prices to Your PCC System
Before you can code and bill for telemedicine procedures, you need to add those procedures to your PCC system, along with codes and your practice’s prices.
Create a Telemedicine Procedure Group
If you create a telehealth or telemedicine procedure group, you can easily report on telemedicine A/R and income. You should perform this step first so you can select the group when you create new procedures.
Open the Tables Tool and Select Procedure Groups
Open the Tables tool from the Configuration menu. Then select the Procedure Groups table.
Click “Add”
Enter Procedure Group Information
Give the new procedure group a name and an abbreviation, determine the order it should appear on screen, and indicate “Yes” to display totals for the new group in PCC reports.
Save the New Procedure Group
For more help in setting up new procedure groups, contact PCC Support.
Add Telemedicine Procedures, Codes, and Prices
Next, add new telemedicine procedures to your PCC system. Include codes (with modifiers, if appropriate) and prices.
What procedures are currently in use? Your practice may need to consult with insurance payers to understand how to code for telemedicine procedures. You should refer to your CPT manual for up-to-date coding information.
During the pandemic, PCC published a Guide to COVID-19 Billing Codes, which includes descriptions of different types of telemedicine visits and how to code for them. PCC also created a Telemedicine Timing reference sheet.
Other Examples:
-
Telephone Service Codes: Use the time-based 99441-99443 for Telephone E&M performed by a MD, DO, NP, or PA. Use 98966-98968 for A&M performed by a RN or MA.
-
Realtime Audio/Video Visit Codes: Use 99211-95 through 99215-95 for live or “synchronous” telemedicine services with realtime audio and video. Note that some payers use a -GT modifier instead of -95 for asynchronous communication (sending and receiving video messages).
As always, these codes are provided only as examples and are not recommendations. Refer to the AMA’s CPT guide to select the correct codes.
Read Edit Your Practices Codes and Prices to learn how to add new billing procedures to your PCC system.
Update Your Electronic Encounter Form w/ Telemedicine Billing Codes
When your clinician is ready to make a visit “Ready for Billing”, they’ll need the right visit codes easily available for a telemedicine visit.
Open Billing Configuration under the Configuration menu and add procedures (and optionally diagnoses) to your practice’s Electronic Encounter Form.
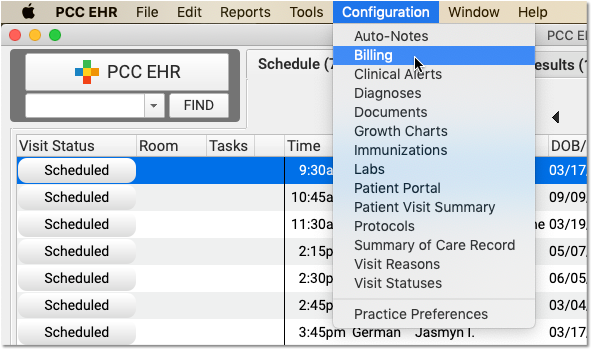
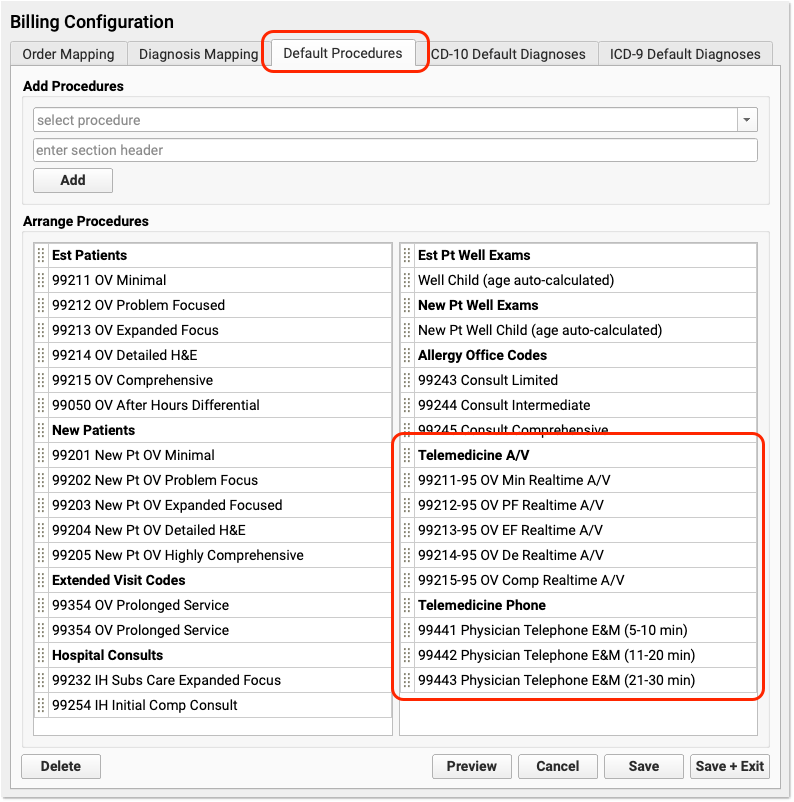
Configure Your Practice’s Telemedicine Places of Service
When you submit a claim for a telemedicine encounter, you need to include a different Place of Service code than for a standard office visit. For example, an “in-office” visit appears on claims with a place of service code of 11, and telemedicine encounters typically need an 02 or a 10.
In PCC EHR, you can schedule all of a provider’s time in your real-world, office locations. You can configure your system with additional telemedicine places of service and automatically select them when billing for telemedicine encounters. When needed, your biller can change the place of service as they post charges or later in the patient’s Billing History.
Which POS Codes Are Used for Telemedicine Encounters?
CMS defines these two telemedicine place of service (POS) codes:
- POS 02: Telehealth Provided Other than in Patient’s Home
Descriptor: The location where health services and health related services are provided or received, through telecommunication technology. Patient is not located in their home when receiving health services or health related services through telecommunication technology.
- POS 10: Telehealth Provided in Patient’s Home
Descriptor: The location where health services and health related services are provided or received through telecommunication technology. Patient is located in their home (which is a location other than a hospital or other facility where the patient receives care in a private residence) when receiving health services or health related services through telecommunication technology.
For more details, you can review the full CMS Place of Service Code Set.
Create Telemedicine Places of Service for Your Physical Locations
To ensure that the correct location codes appear on your claims, your practice should schedule telemedicine encounters to a telemedicine location. Contact PCC Support for help setting up places of service on your PCC system.
For example, PCC Support can create a “Main Office Telehealth (Home)” place of service with the POS 10 code for claims. If you perform telemedicine encounters when the patient is at another medical facility, PCC Support can create another location for POS 02 encounters.
As with other claim requirements, check with your carriers to determine billing requirements. For example, some payers may require an 11, 10, or 02 place of service code for telemedicine visits, depending on circumstances. PCC can also help you configure schedules so the correct place of service always appear on every claims.
Set Default Billing Places of Service for Telemedicine Encounters
When you schedule a telemedicine visit, use your real-world physical office location in the Appointment Book. Then your doctors can see their whole schedule, and your practice can see what’s happening that day at a glance.
When it’s time to bill, as noted above, payers typically require a special telemedicine place of service on the claim. It’s cumbersome to manually switch the place service each time you post telemedicine visit charges. To make posting easier, you can set a default billing place of service for telemedicine encounters for each of your scheduling locations. Follow the procedure below to learn how.
Open Practice Preferences
Click on the Configuration menu and select “Practice Preferences”.
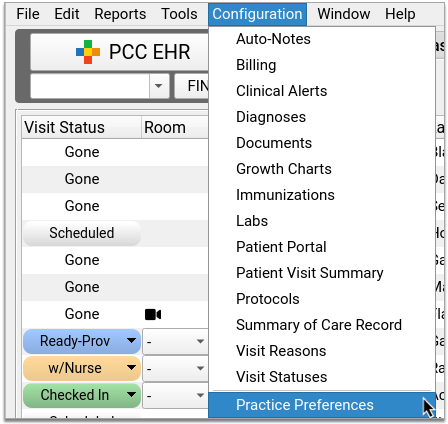
Find Telemedicine Place of Service Mapping
Scroll down the page until you find Telemedicine Place of Service Mapping.
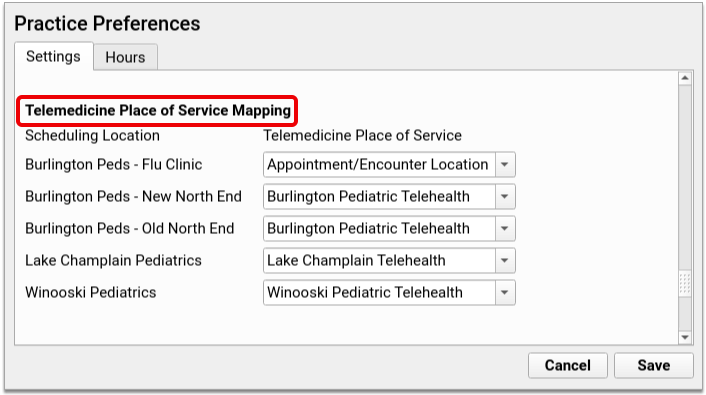
Link Your Scheduling Locations to a Telemedicine Place of Service
Open the Telemedicine Place of Service drop-down next to each of your Scheduling Locations. For each location, pick a default billing place of service for telemedicine visits.
If you don’t want to bill telemedicine visits using a special place of service, use “Appointment/Encounter Location” as the Telemedicine Place of Service default.
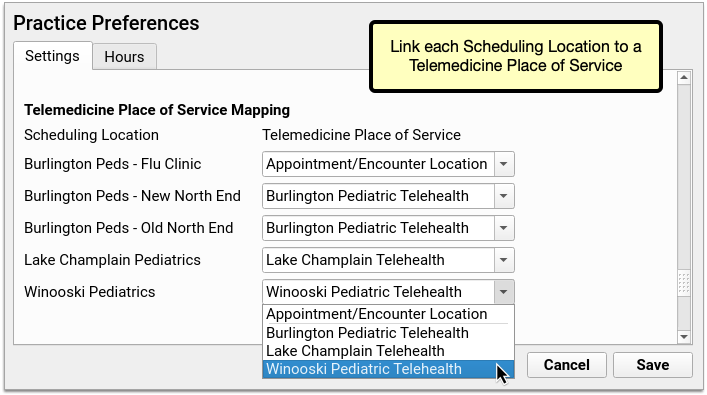
The drop-down will show you all of the places of service in your PCC system configured with a HIPAA claim code of either “02” or “10”, which are telemedicine place of service codes.
Log Out and Back In
Log out and back into PCC EHR to load the new settings.
Post Telemedicine Visit Charges in PCC EHR
When you post telemedicine visit charges in PCC EHR, the billing place of service will default to the Telemedicine Place of Service you set in Practice Preferences for that scheduling location.
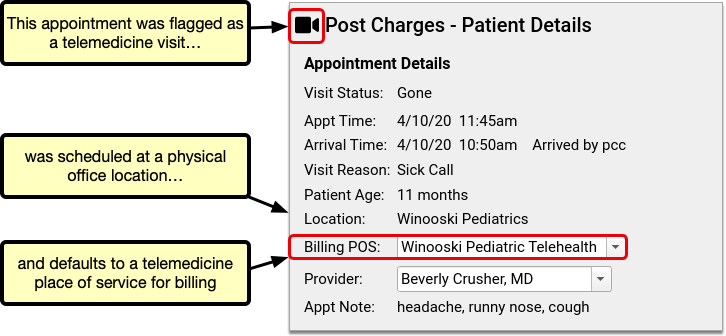
Use the Billing POS drop-down if you need to change the billing place of service on the fly for a particular visit.
If you encounter a billing problem with a telemedicine encounter, you can also change the place of service later and queue up a new claim using the Edit Charges feature of the Billing History in the patient’s chart.
Create a Telemedicine Visit Protocol
In PCC EHR, you can create and customize chart note protocols for different visit types. PCC recommends you create a “Telemedicine Sick” protocol, along with other telemedicine-based protocols you expect to schedule. Those protocols can then be configured to appear automatically for telemedicine visits.
Sample Telemedicine Protocol: Take a look at a sample telemedicine protocol, shared by a pediatric practice that uses it every day: Telemedicine Sick Protocol was created by Dr. Seth Bokser at Tamalpais Pediatrics in Larkspur, California.
Watch the Video: For a video walk-through of this procedure, watch Create a Telemedicine Visit Protocol.
Create a Telemedicine Protocol for Sick Visits
Open Protocol Builder
In the Configuration menu, select “Protocols” to open the Protocol Configuration tool. Then open the Protocol Builder.
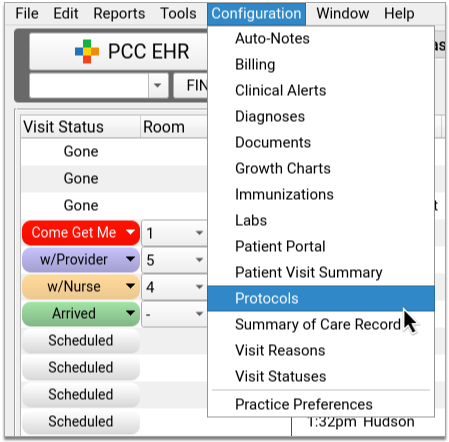
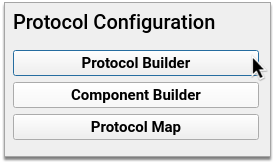
Clone an Existing Sick Visit Protocol
In the Protocol Builder, pick a sick visit protocol to use as a template for your new Telemedicine Sick protocol. Highlight your choice, then click “Clone”.
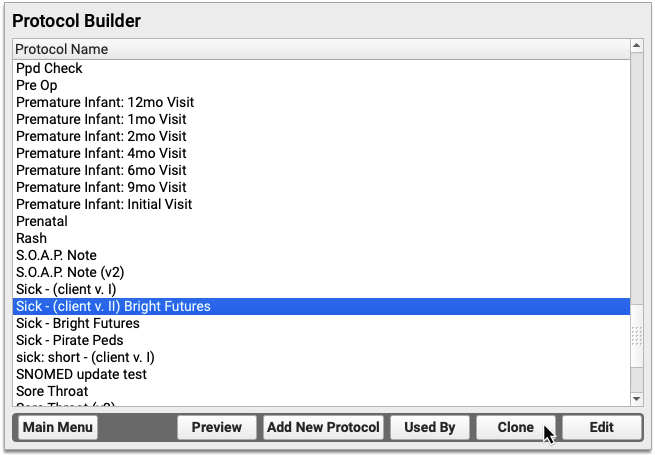
Choosing the Right Sick Protocol: If your practice has several sick visit protocols and you aren’t sure which one to choose, the Protocol Map tool can help you decide. The Protocol Map tool shows you how protocols are linked to the visit reasons your practice uses for scheduling. Use it to see which protocol most providers use to chart sick visits. Learn how to use the Protocol Map.
Name and Save Your New Protocol
Name your new protocol. Then click “Clone” to begin customizing its settings.
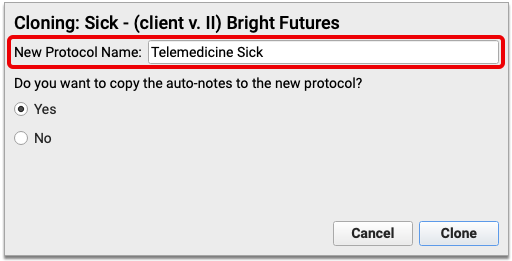
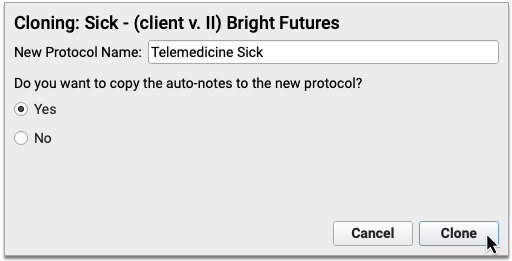
What About Auto-Notes?: If your practice relies on clinician auto-notes to chart sick visits, you can copy those auto-notes into your new protocol now. If you choose not to copy them now, they can also be added later. Choose “Yes” to copy auto-notes now, or “No” to skip this step. Any auto-notes you copy now will likely need to be adjusted later so that they are accurate in the context of a telemedicine encounter.
Remove Unwanted Components from Your New Protocol
Some components in your new protocol will not be useful for telemedicine encounters (e.g., Medical Procedure Orders). Highlight unwanted components and click “Delete” to remove them.
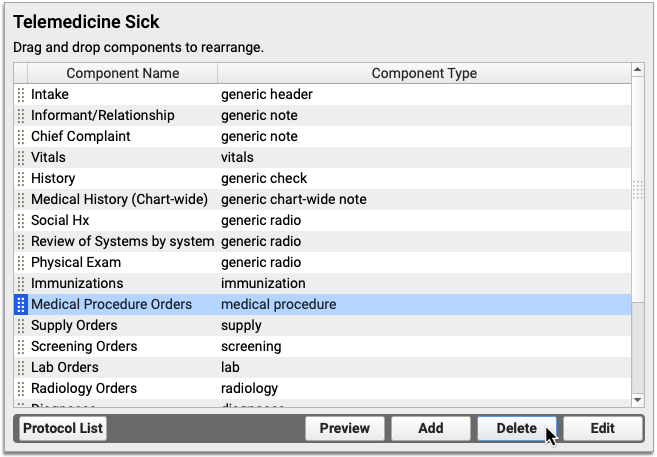
Will I Use Orders Components During Telemedicine Visits?
Yes! You might need to issue orders even though the patient you are seeing isn’t physically in your office. Here are a few components you might want to keep in your Telemedicine Sick protocol:
-
Immunizations: Keep the Immunizations component in your protocol for quick reference to your patient’s Immunization History and Immunization Forecasting details.
-
Lab Orders: Keep the Lab Orders component in case you want to order external lab tests during a telemedicine visit.
-
Radiology Orders: Keep the Radiology Orders component in case you decide to send a telemedicine patient to get an x-ray.
-
Follow-Up Orders: Use Follow-Up Orders to keep track of your what your patients need after their telemedicine visits.
-
Referral Orders: You might decide during a telemedicine visit that your patient needs to be seen by another provider. Use Referral Orders to document this decision in the patient’s chart.
Customize the Remaining Components for Telemedicine
The components you kept in your new protocol will need to be customized for telemedicine.
Review each component by selecting it from the list and clicking the “Edit” button. Delete unwanted items or add new ones, then save your changes. The items you save into each component will become available for one-click charting once the protocol is live.
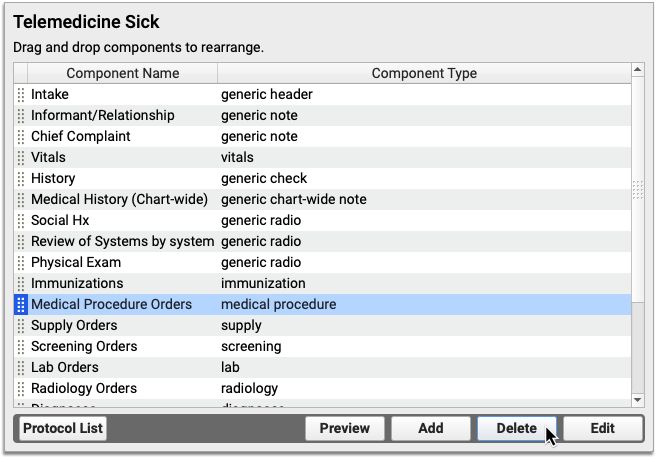
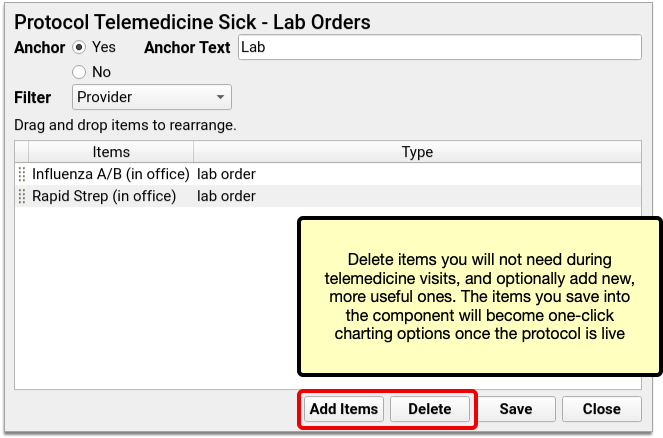
To learn more about customizing components inside a protocol, read Create and Edit a Protocol.
Open the Component Builder to Begin Creating Custom Telemedicine Components
Use the Component Builder to create custom components for your new telemedicine protocol.
Open the Component Builder from the main Protocol Configuration menu.
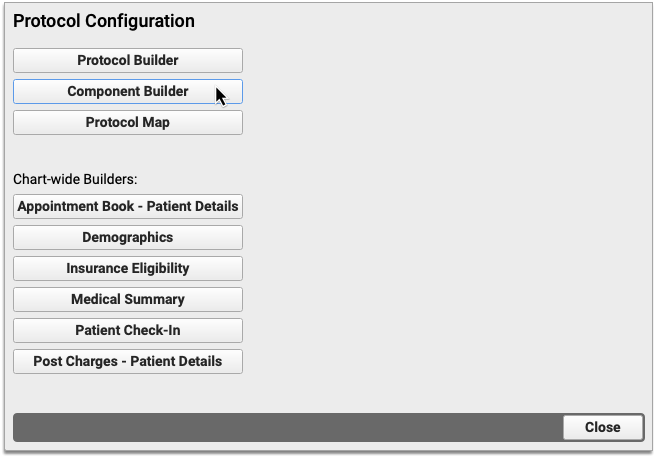
Create a Telemedicine Consent Component
Create a custom check box component to chart patient and caregivers’ consent to telemedicine services.
On the Visit Components tab of the Component Builder, click “Create” to create a new component. Pick a name for your component (e.g., Telemedicine Consent) and set the component type to Generic Check. Click “Save”.
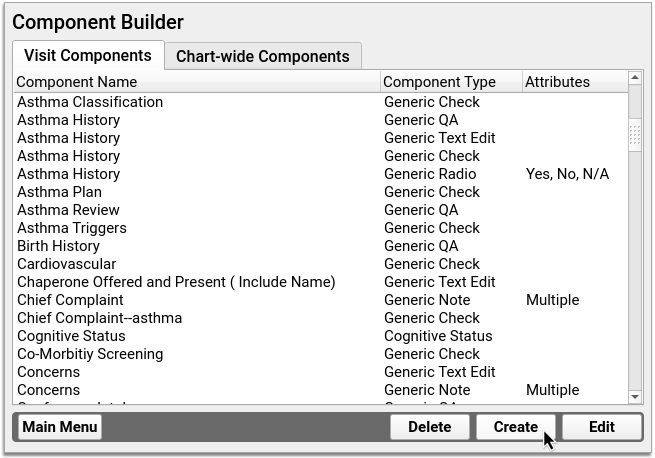
Create telemedicine consent statements in the fields under “Add New Items”. Each field becomes a unique check box once you save the component.
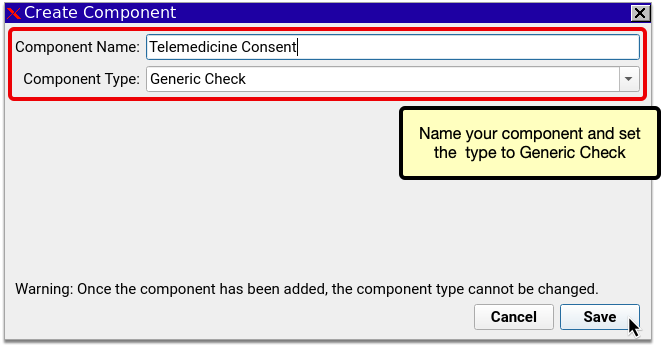
Click “Save” to finish creating your Telemedicine Consent component.
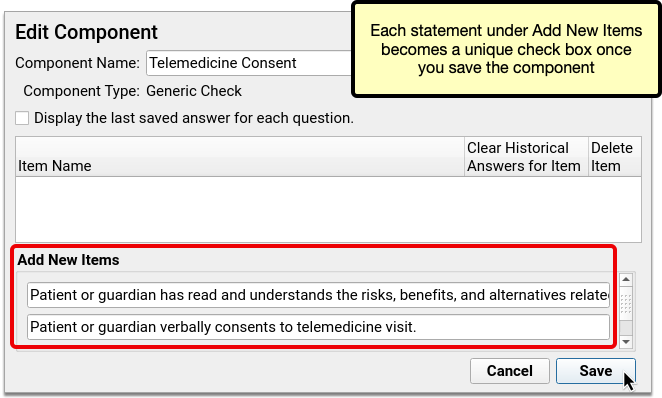
Sample Telemedicine Consent Statements
Your practice should share a telemedicine consent form with patients and families, and solicit verbal consent to telemedicine services during each visit. You should chart that at the top of the chart note.
Here are two sample telemedicine consent statements your practice could use as part of a consent form.
-
Acknowledgment of Telemedicine Consent Policy: “Patient or guardian has read and understands the risks, benefits, and alternatives related to a telemedicine visit at the time of booking appointment.”
-
Consent to Telemedicine Visit: “Patient or guardian verbally consents to telemedicine visit.”
State and Payer Requirements: Your state and insurance payers might require you to document certain kinds of consent information during telemedicine visits. Check with these entities to make sure you understand whether you are required to obtain special consent for telemedicine care, and how to document it in chart notes.
Create a Vitals Notes Component
Vitals might be reported by patients or caregivers during telemedicine visits. Create a Vitals Notes component to document how telemedicine vitals were collected, and by whom. The vitals themselves can be charted the usual way in PCC EHR’s built-in Vitals component.
In Component Builder, make sure you are in the Visit Components tab. Click “Create”. Pick a name for your new component (e.g., Vitals Notes). Set the component type to Generic Note and the input field to Single. Click “Save”.
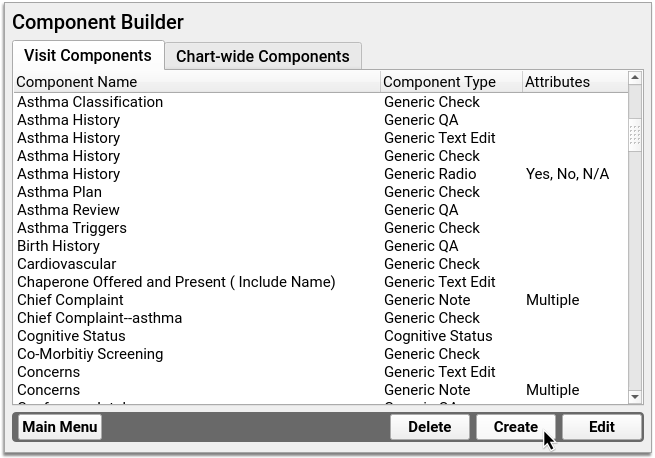
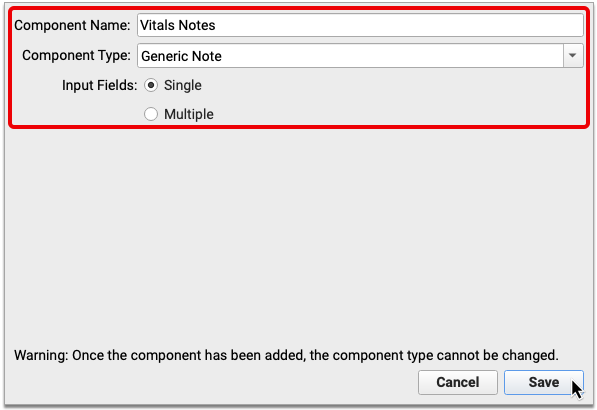
I Already Have a Vitals Notes Component: If your practice already has a Vitals Notes component, there is no need to create a new one from scratch. Repurpose the existing one for your Telemedicine Sick protocol.
Should I Chart Telemedicine Vitals in PCC EHR's Built-In Vitals Component?: If you want to calculate BMI and percentages, and see telemedicine vitals in Growth Charts and Flowsheets, chart them in PCC EHR’s built-in Vitals component. If you are concerned that telemedicine vitals are too inaccurate to be included in Growth Charts and Flowsheets, consider recording them in the Vitals Notes box instead. Vitals recorded in the notes box will appear in the final chart note, but will not be included in Growth Charts and Flowsheets.
Add New Telemedicine Components to Your Protocol
Return to the Protocol Builder and edit your Telemedicine Sick protocol.
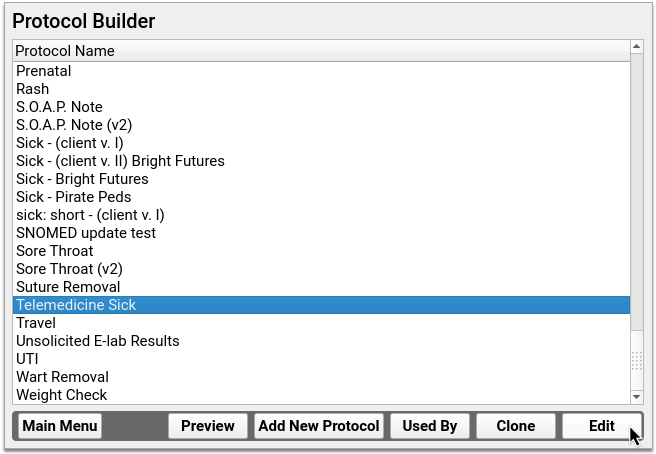
Click “Add” to begin adding your new components to the protocol.
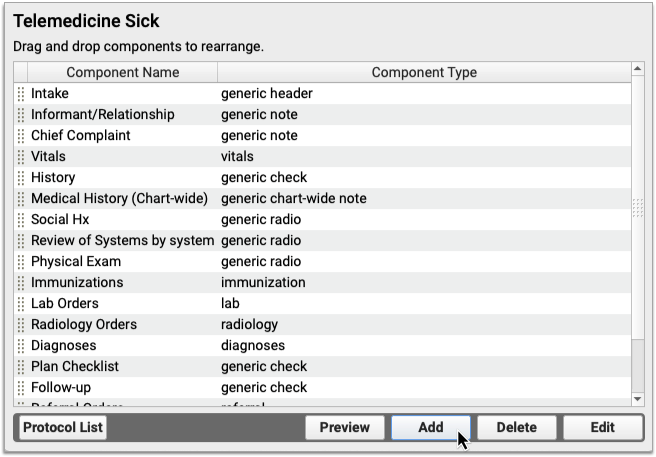
Select your telemedicine consent component from the drop-down. Once you do, a second, blank drop-down field will appear. Use that second drop-down to select your Vitals Notes component. If there is already a Vitals Notes component in your protocol, you will not be able to add it a second time.
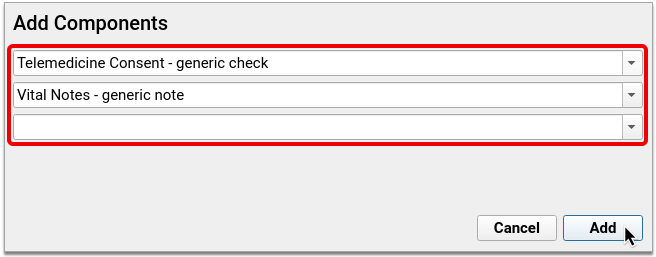
Click “Add” to finish adding the components to the protocol.
Once they have been added, click and drag the components to rearrange their sequence in the protocol.
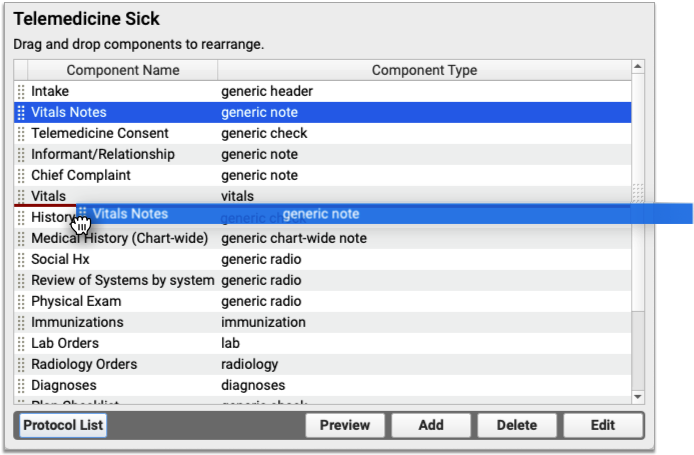
Display Telemedicine Consent Check Boxes in Your New Protocol
In the Telemedicine Sick protocol, highlight the Telemedicine Consent component and click “Edit”.
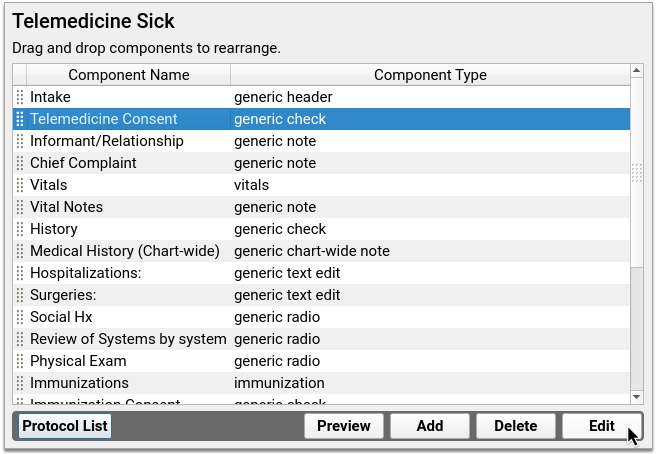
Click “Add Items”.
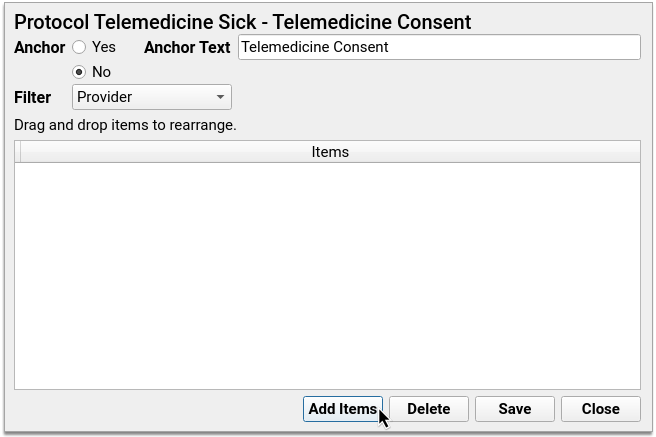
Click the drop-down arrow and select a consent statement. Once you do, another, blank drop-down field will appear. Use that blank field to select another consent statement. Repeat this until all consent statements have been added to the list.
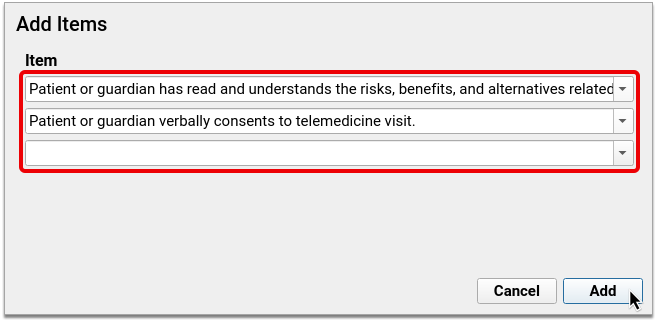
Click “Save” to finish adding the items to the component, then save again to close the component.
Preview Your Finished Protocol
Click “Preview” to see what your protocol will look like once it is live.
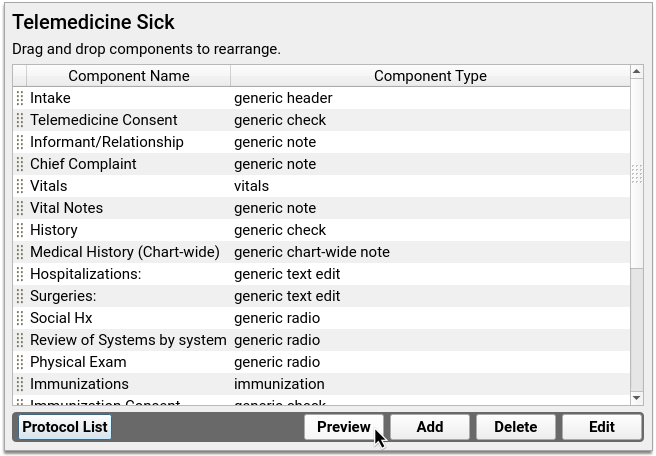
Test the look, flow, and function of components by clicking buttons, checking off boxes, and typing inside text fields. When you are done, click “Close” to exit the preview.
If you want to make more changes, do so now. Otherwise, close Protocol Configuration.
Adjust Clinician Auto-Notes for Your Telemedicine Sick Protocol
If you copied clinician auto-notes into your new protocol, you might need to adjust the statements so that they are accurate in the context of a telemedicine encounter.
Open Auto-Notes from the Configuration menu.
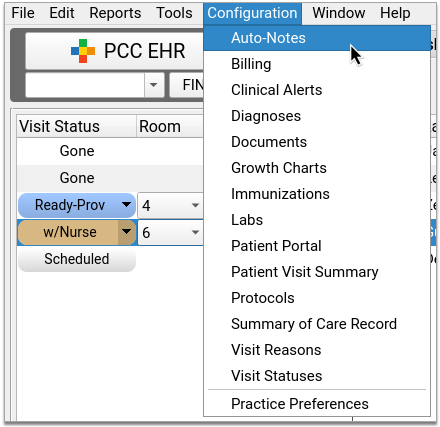
Select “Telemedicine Sick” from the Protocol drop-down and select “Practice Defaults” from the User drop-down.
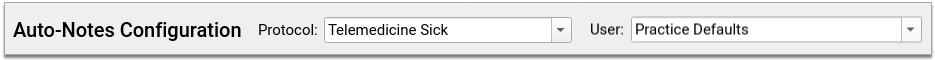
Review and edit the statements to make them accurate for telemedicine encounters. If an individual user at your practice has custom auto-notes set up for sick visits, switch the User drop-down to their name and adjust those statements too.
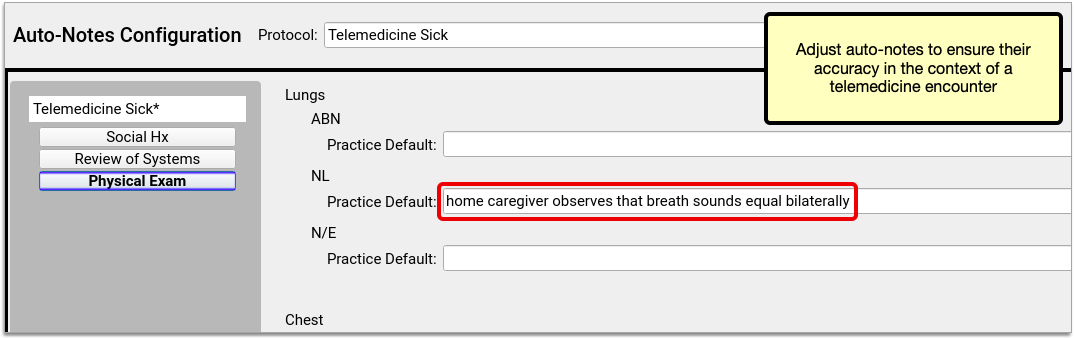
For an in-depth look at how to use and configure auto-notes, read Use Auto-Notes to Insert Your Standard Text in a Chart Note Field.
Map Your Telemedicine Sick Protocol to a Visit Reason
Use the Protocol Map tool inside Protocol Configuration to link your Telemedicine Sick protocol to telemedicine sick visit reason(s). Once linked, your new protocol will become the default chart note for appointments scheduled as telemedicine sick visits.
Learn how to use the Protocol Map.
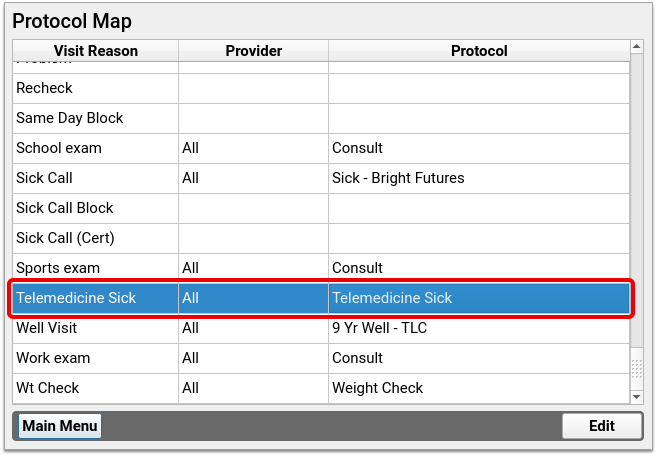
Customize Other Chart Note Protocols for Telemedicine
Sick visits aren’t the only kind of appointment you see via telemedicine. Use the tips in this article to customize other types of chart note protocols for telemedicine too, such as ADHD follow-up protocols, well visit protocols, and more!
Create a COVID-19 Test Lab Order
You can use the Lab Configuration tool to create and track lab orders for COVID-19 tests. Your PCC EHR system includes codes and descriptions for SARS-CoV-2, including the newer 95209-3 SARS-CoV+SARS-CoV-2 Ag test.
Watch a Video: Watch a video walk-through of creating a COVID-19 lab order.
CMS Guide to Becoming Certified for Lab Testing: On 2020-09-25, CMS released new tools for laboratories seeking Clinical Laboratory Improvement Amendments (CLIA) certification to test for coronavirus disease 2019 (COVID-19).
Procedure Code Guidance: The procedure codes discussed in this article are intended only as examples. You should consult the AMA’s current CPT Coding Guide and work with your insurance payers to verify what codes you should report on claims. Your practice updates and maintains your billable procedure list, codes, and prices in the Procedures table in the Tables configuration tool on your PCC system.
Open Lab Configuration
Open the Lab Configuration window from PCC EHR’s Configuration menu.
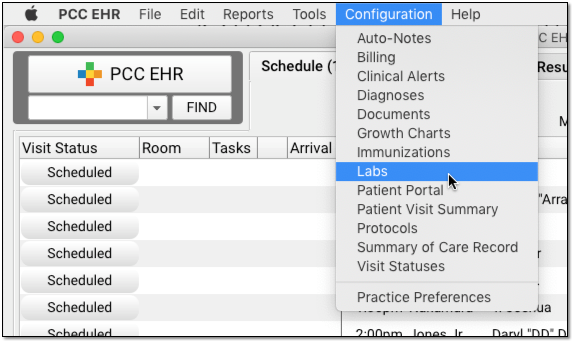
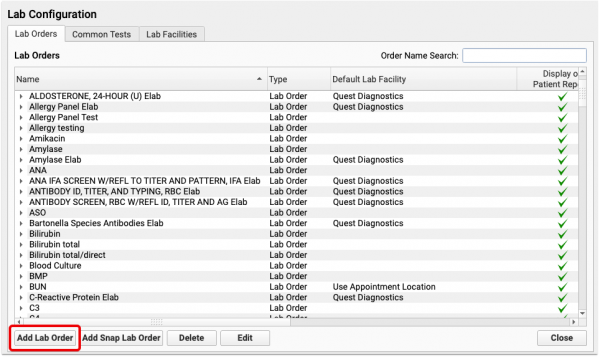
Add a New Lab and Configure Details
Click into the Lab Orders tab, and click the “Add Lab Order” button to create a new lab.
Enter the lab’s name, default lab facility, and other details.
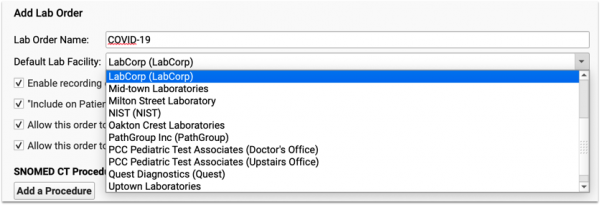
Set Default Lab Behaviors
Next, review and edit the settings and default behaviors for this lab order.
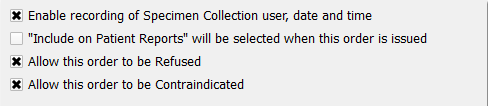
-
Specimen Collection: If you wish to record specimen collection information for this lab order, click “Enable recording of Specimen Collection user, date, and time”.
-
Appear on Patient Reports and My Kid's Chart: If you wish this lab to be visible by default on patient reports, including the Patient Visit Summary and My Kid’s Chart (the patient portal), select “‘Include on Patient Reports’ will be selected when this order is issued”. Clinicians can determine whether or not a lab order is visible at any time for any order by selecting the check box on the specific order for a patient.
-
Refusal and Contraindication: If a lab order can be refused or contraindicated, select the appropriate options to enable those checkboxes on the order.
Add COVID-19 Lab Tests for Third-Party Vendors
If your practice receives results for this lab order electronically from LabCorp or Quest you can add their specific lab test to this lab order. Both LabCorp and Quest have provided lab codes for COVID-19 tests. Enter those into the E-lab Vendor Order Mapping:
- Labcorp COVID-19 Test: 139900
- Quest SARS-CoV-2 RNA, Qual Real-Time Test: 39433
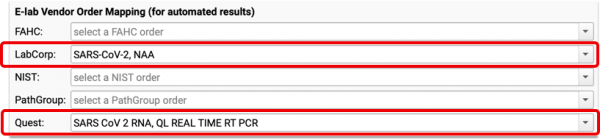
PCC EHR will be able to correctly associate and track the lab results with the order in the patient’s record. For more information about e-labs, read the Import E-lab Test Results article.
Optional: Add Specific LOINC Lab Tests for Manual Results
Type a LOINC code or test name in the “Tests to Include” section to add a LOINC test’s fields for manual entry to your lab order.
For example, you could add the 95209-3 SARS-CoV+SARS-CoV-2 Ag test.
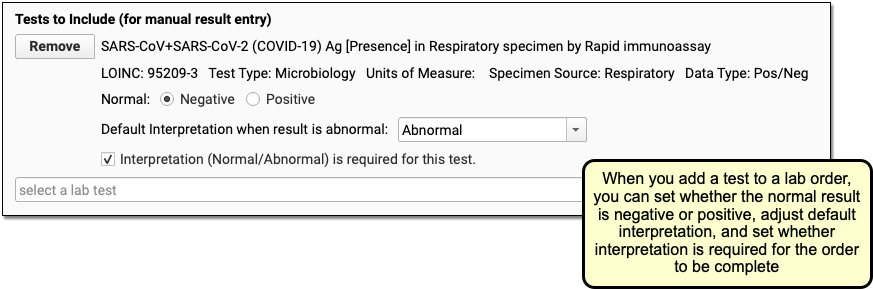
Click “Save”
Click Save to save your lab order changes.
Configure Billing
Open Billing from the Configuration menu. Search for your new lab order, select it, and click “Edit”.
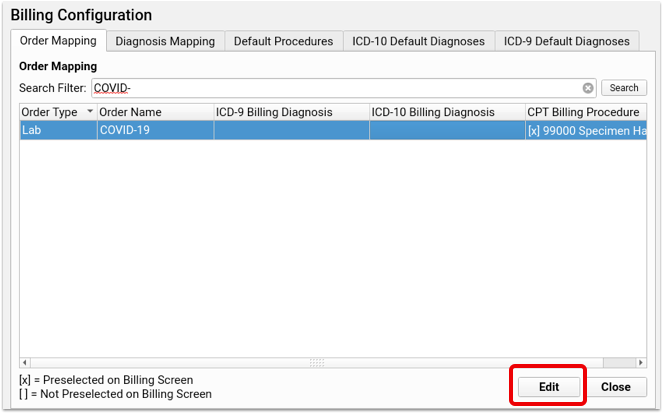
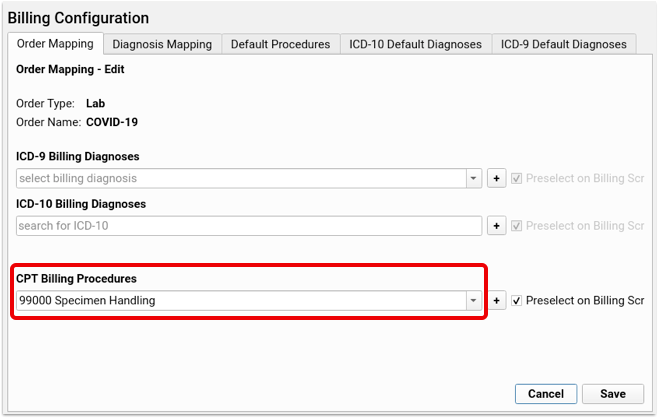
If you’re collecting and preparing the specimen for analysis by an outside laboratory, enter the specimen collection procedure, 99000 Handling and/or conveyance of specimen for transfer from the office to a laboratory, in the CPT Billing Procedure field. Additional procedures can be linked by clicking the plus button to add a new line. Click save and the selected procedures will be included in the visit’s bill.
Depending on whether or not your practice is actually performing a lab, you might add one or more of the following procedures to the lab order:
- 87426 Infectious agent antigen detection by immunoassay technique
- 87635 Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
- 86328 Immunoassay for infectious agent antibody(ies), qualitative or semiquantitative, single step method (eg, reagent strip); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19])
- G2023 Specimen collection for severe acute respiratory syndrome coronavirus 2 (sars-cov-2) (coronavirus disease [covid-19]), any specimen source.
Note: This code is for use by independent labs, not private offices.
- U0002 2019-ncov coronavirus, sars-cov-2/2019-ncov (covid-19), any technique, multiple types or subtypes (includes all targets), non-cdc
For more information, read Code and Bill for a COVID-19 Related Encounter.
Optional: Add Labs to Protocols
You can order any lab from the Labs component, which is already available on most of your chart protocols. Specific labs can be added to each protocol- if you’re creating a visit type just for these tests, use the PCC EHR Configuration Tool to add the labto your chart note protocols. Contact PCC Support for assistance.
Test Your New Lab Order
Create a sample visit for a test patient and order your new COVID-19 lab. You should see appropriate tests inside the order, and if you added the Specimen Collection (or other CPT), it should appear on the Electronic Encounter Form.
For additional help setting up your labs or adding them to your protocols, please contact PCC Support.
Code and Bill for COVID-19 Related Encounters
How does a pediatric practice code and bill for COVID-19 related encounters? Read below to learn about the SNOMED-CT, ICD-10, and CPT codes available for tests, diagnoses, and more. PCC Support can help you customize your chart note protocols, diagnoses, orders, and billing tools.
New Codes On Your System: Throughout 2020 and into 2021, PCC regularly updated your system to add vendor lab identifiers, SNOMED-CT descriptions, ICD-10 codes, and LOINC codes to help with COVID-19-related orders, charting and billing. Contact PCC Support if you have any questions or can’t find the code you need.
Procedure Code Guidance: The procedure codes discussed in this article are intended only as examples. You should consult the AMA’s current CPT Coding Guide and work with your insurance payers to verify what codes you should report on claims. Your practice updates and maintains your billable procedure list, codes, and prices in the Procedures table in the Tables configuration tool on your PCC system.
Code for Exposure or Other COVID-19 Related Symptoms
How do you code for exposure to COVID-19? What other diagnoses are used for a COVID-19 encounter, and how might you map those to SNOMED descriptions for use on a chart note?
Exposure
When you diagnose exposure to COVID-19, you can use:
- Z20.822 Contact with and (suspected) exposure to COVID-19
- SNOMED-CT Mapping Option: Exposure to SARS-CoV-2 (alternate title: Exposure to 2019 novel coronavirus)
History, Associated Symptoms, and More
What other ICD-10 billing codes, and corresponding SNOMED descriptions, are available for COVID-19 related encounters?
- B97.21 SARS-associated coronavirus as the cause of diseases classified elsewhere
- SNOMED-CT Mapping Option(s): Suspected disease caused by severe acute respiratory coronavirus
- Z86.16 Personal history of COVID-19
- SNOMED-CT Mapping Option(s): H/O: viral illness, H/O: infectious disease
- Z86.19 Personal history of other infectious and parasitic diseases
- SNOMED-CT Mapping Option(s): History of disease caused by Severe acute respiratory syndrome coronavirus
- Z03.89 Encounter for observation for other suspected diseases and conditions ruled out
- SNOMED-CT Mapping Option(s): Disease caused by Severe acute respiratory syndrome coronavirus 2 absent
- M35.81 Multisystem inflammatory syndrome (MIS)
- SNOMED-CT Mapping Option(s): Acute organ dysfunction due to systemic inflammatory response syndrome, Systemic inflammatory response syndrome, Systemic inflammatory response syndrome associated with organ dysfunction, Systemic inflammatory response syndrome without organ dysfunction
- M35.89 Other specified systemic involvement of connective tissue
- SNOMED-CT Mapping Option(s): Disorder of connective tissue co-occurrent and due to systemic disease
- J12.82 Pneumonia due to coronavirus disease 2019
- SNOMED-CT Mapping Option(s): (pneumonia diagnosis descriptions)
You might also use other diagnoses for common signs and symptoms:
- R051-R059 Cough
- R06.02 Shortness of breath
- R50.9 Fever, unspecified
Code for a Screening Encounter?: In December of 2020, the WHO added another related ICD-10: Encounter for screening for COVID-19 (Z11.52). During the COVID-19 pandemic, a screening encounter code is generally not appropriate. For encounters for COVID-19 testing, including preoperative testing, code instead as exposure to COVID-19.
Adjust Your PCC EHR Chart Note Protocols to Display COVID-19 Related Diagnoses
To make them easier to select, you can use the Protocol Configuration tool to add diagnoses directly to your practice’s chart note protocols.
When clinicians select a SNOMED diagnosis description, the mapped ICD-10 billing code appears on the Bill screen.
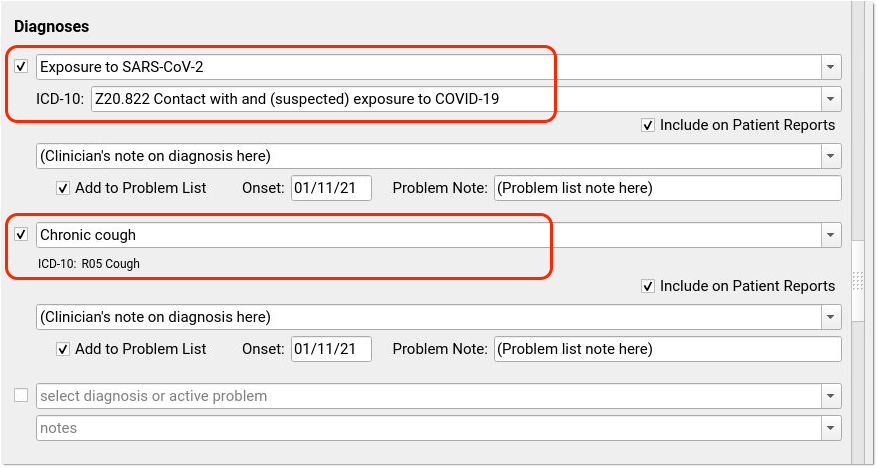
Many codes include pre-defined mapping. Use the Billing Configuration tool to adjust the mapping of SNOMED-CT descriptions to ICD-10 codes. Possible SNOMED to ICD-10 mappings are listed in the section above with each billing code.
Order and Code for COVID-19 Lab Tests
During an encounter, you may decide to order a COVID-19 test. When you order a COVID-19 test, your practice might collect the specimen and relay the test to a lab vendor for processing. Increasingly, pediatric practices are also completing tests in-house.
In PCC EHR, when you click “Order” next to a lab order, the appropriate LOINC will be part of the order, appropriate diagnoses and procedures can be queued up for billing, and optionally the lab test information can automatically be added to the chart note for incoming electronic results.
Set Up Your COVID-19 Lab Test Orders: You can learn how to create a COVID-19 lab test order on your system, add it to chart note protocols, and configure billing behavior by reading: Create a COVID-19 Test Lab Order. For additional details about Lab Configuration in PCC EHR, you can read Lab Configuration.
Billing Codes for COVID-19 Tests and Orders
When you gather the specimen for a COVID-19 test, you can bill:
- 99000: Handling and/or conveyance of specimen for transfer from the office to a laboratory
Depending on your lab configuration, and whether or not you perform the test in-house, you may use additional procedures for a COVID-19 test:
- 87635: Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
- 87426: Infectious agent antigen detection by immunoassay technique
- 86328: Immunoassay for infectious agent antibody(ies), qualitative or semiquantitative, single step method (eg, reagent strip); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19])
- U0002: 2019-ncov coronavirus, sars-cov-2/2019-ncov (covid-19), any technique, multiple types or subtypes (includes all targets), non-cdc
- G2023: Specimen collection for severe acute respiratory syndrome coronavirus 2 (sars-cov-2) (coronavirus disease [covid-19]), any specimen source. Note: This code is for use by independent labs, not private offices.
In PCC EHR, you can map your orders directly to the procedures you bill so they will automatically appear on your electronic encounter form automatically.
E-Lab Configuration Identifiers
You can configure lab orders so results will be sent back to your practice electronically, if your lab vendor supports e-lab integration.
Labcorp and Quest have provided the following vendor-specific identifiers, which PCC added to all practice systems:
- Labcorp COVID-19 Test: 139900
- Quest SARS-CoV-2 RNA, Qual Real-Time Test: 39433
Code and Bill a COVID-19 Diagnosis
During an in-person or telemedicine visit for a patient with a COVID-19 diagnosis, you would code both the COVID-19 diagnosis and related conditions.
When you indicate a COVID-19 diagnosis with a SNOMED description, use:
-
840539006 Disease caused by 2019-nCoV: This diagnosis has alternate, searchable names of “Disease caused by 2019 novel coronavirus” and “Disease caused by Wuhan coronavirus”.
In PCC EHR, you can select this diagnosis on a chart note and/or add it to a patient’s Problem List.
For all encounters that occured after April 1st, 2020, use this code when you bill for a visit with a patient with a positive COVID-19 diagnosis:
- U07.1 COVID-19
This code was added to all PCC systems with a 2020-03-23 update. By default in PCC EHR, when you select the SNOMED COVID-19 description, the ICD-10 COVID-19 code will appear:
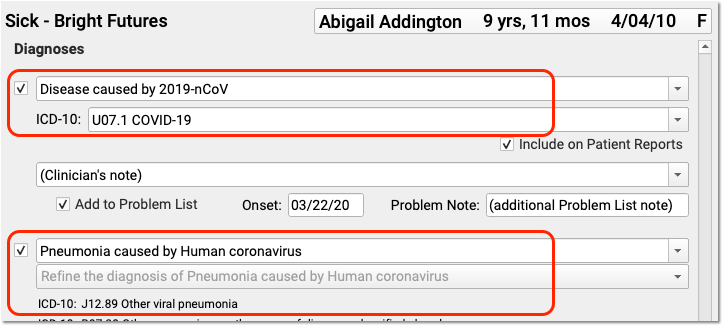
For services rendered prior to the April 1st effective date of U07.1 COVID-19, the CDC recommends you chart and code for the conditions of Pneumonia, Bronchitis, Lower Respiratory Infection, Respiratory Infection NOS, and ARDS, and then adding B97.29 Other coronavirus as the cause of diseases classified elsewhere. Before the specific COVID-19 ICD-10 diagnosis code is in effect, use the less specific B97.29 secondary to the manifestation code to indicate the patient has COVID-19.
Details May Change: The above scenarios and COVID-19 codes are new and payer response may vary. PCC keeps an up-to-date handout with COVID-19 coding and billing recommendations here: 2020 COVID-19 Coding Guide. We will update that PDF and this article as the situation changes and we learn more.
Use Other Procedure CPTs for COVID-19 Related Visits
In addition to the codes mentioned above, here are some other CPT codes you might use in relation to a COVID-19 related encounter.
Code for Telemedicine, Phone Calls, Portal, Email and Other Remote Services: What CPT visit code should your practice use for a video telemedicine encounter, a telephone call, a portal message consultation, or other remote service? PCC is maintaining a COVID-19 Coding Guide with descriptions of appropriate codes for different circumstances. You can also read PCC’s Schedule, Chart, Code, and Bill for Telemedicine Encounters.
Bill for COVID-19 Risk Counseling
Your practice may talk with a patient or parent at length about COVID-19 risk. You could use:
- 99401: Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual (separate procedure) approximately 15 minutes
- 99402: …approximately 30 minutes
- 99403: …approximately 45 minutes
- 99404: …approximately 60 minutes
You may use these codes for COVID-19 risk reduction and prevention counseling. You can add these codes onto a claim with other office visit codes, or they can stand alone.
Are These Codes Okay for Telemedicine?: Although these codes do not appear in Appendix P of the CPT manual, which lists telehealth or telemedicine codes, many states are currently mandating that all services, including the 99401-99403 codes, be billable in a telemedicine encounter.
Add-On CPTs for Urgent and Unusual Circumstances
If an emergency appointment disrupts your office’s schedule, such as the sudden arrival of a patient with Acute Respiratory Distress, you can use this additional code on the claim:
- 99058: Service(s) provided on an emergency basis in the office, which disrupts other scheduled office services, in addition to basic service
If you have to leave the office for an emergency visit that disrupts your schedule:
- 99060: Service(s) provided on an emergency basis, out of the office, which disrupts other scheduled office services, in addition to basic service
If you leave the office for an encounter at the request of the patient or family, you might add:
- 99056: Service(s) typically provided in the office, provided out of the office at request of patient, in addition to basic service
We're Seeing Kids in the Parking Lot. Is That a 99056?: If the patient or family makes a special request for you to come out to the parking lot to perform a visit, you may add this code. If your practice sees patients in your parking lot as your general office policy during the COVID-19 epidemic, this code may not apply.
Vaccine, Administration, and Counseling Codes
Payment for administration of COVID-19 vaccine varies among payers and states. You should consult your CPT resource for guidance, and speak with your payers.
Guide to COVID-19 Vaccines in PCC EHR: Read COVID-19 Vaccines: Plan, Configure, Order, Administer, and Track to learn about the MVX, CDX, NDC, and CPT codes needed for COVID-19 vaccine encounters.
How to code for COVID-19 vaccine-related encounters has continued to evolve and change during 2021. For example, in June of 2021, North Carolina Medicaid changed their payment policy for CPT 99401 (Preventative medicine counseling and/or risk factor reduction intervention) to allow for an additional 15 minutes to counsel about the benefits of receiving COVID-19 vaccine. They require a CR modifier on the code. When this change occurred, PCC reached out to North Carolina clients.
If you learn of similar updates to policy, please reach out to PCC and/or PCC Community to share!
Installing Your Firewall
PCC uses a Fortinet Fortigate 60F (or related model) as a firewall in our clients’ offices to protect their networks.
Follow the instructions on this page to install your Fortigate firewall.
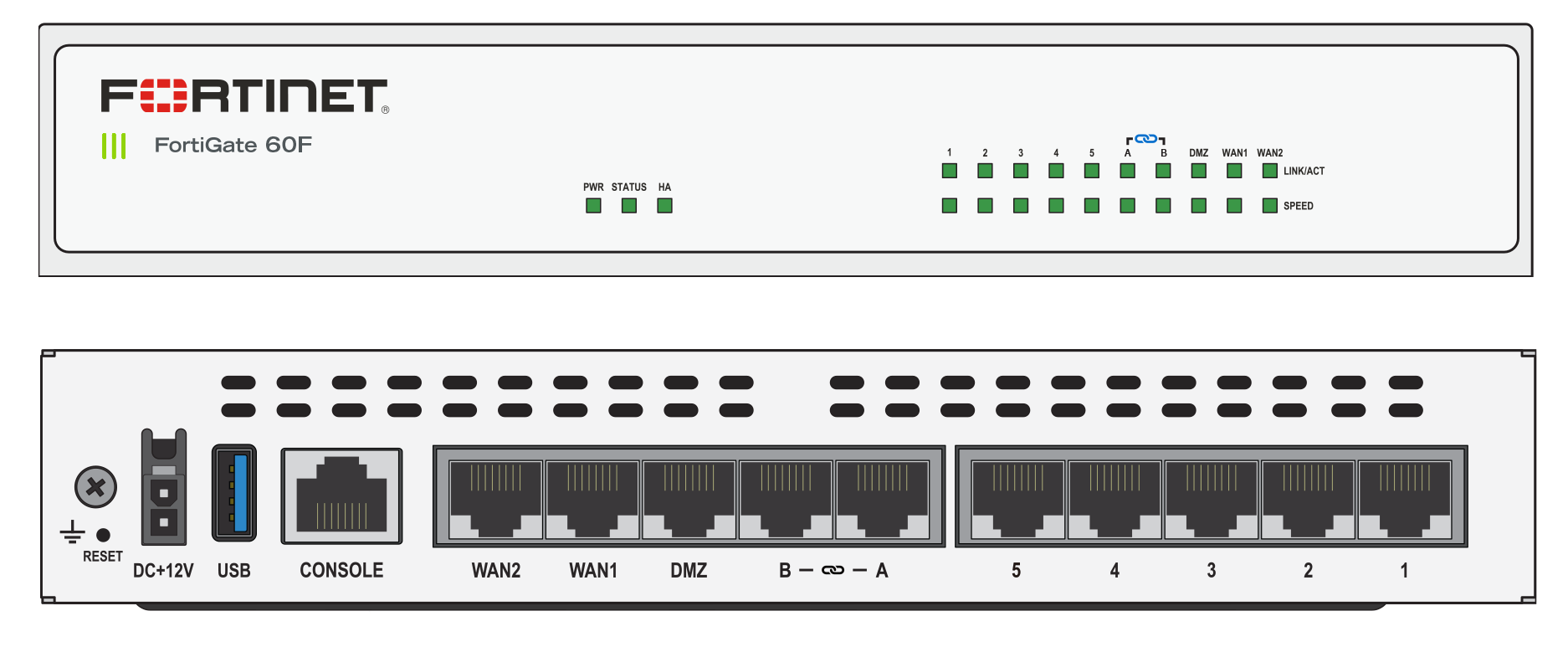
Follow the instructions on this page to install your Fortigate firewall.
Connect Your Modem
With the ethernet cable that came with your Fortigate firewall, connect your ISP’s modem to the “WAN1” port on the Fortigate.
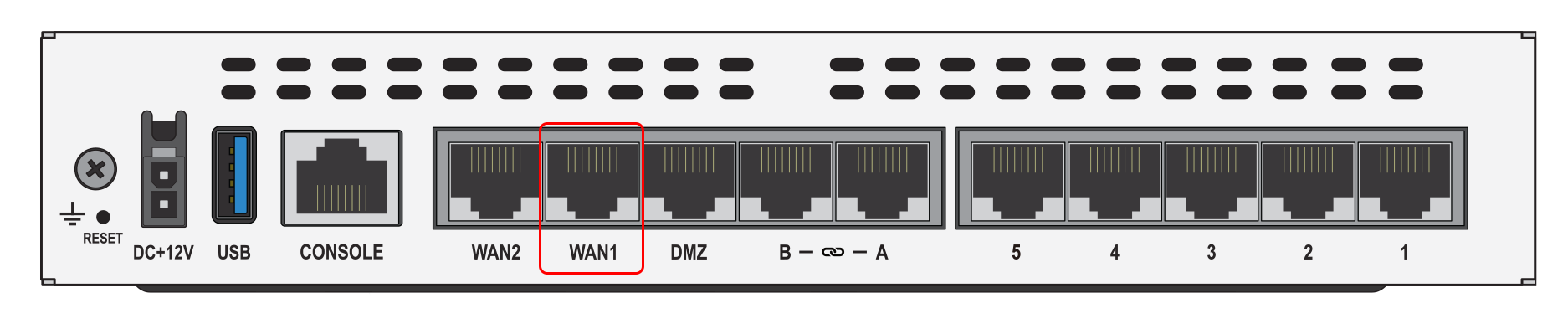
The ethernet ports on most modems are usually clearly labeled, but if you are unsure which port to use, contact your ISP.
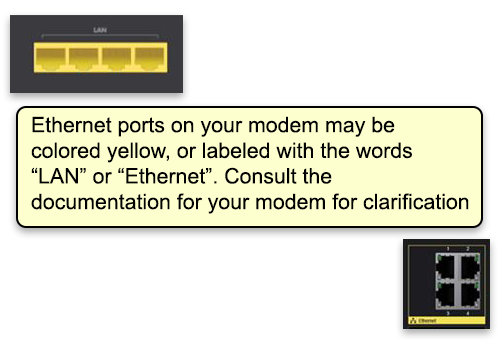
Add Other Devices to Your Network
Now connect other networking equipment to the LAN ports on the back of the Fortigate. Use the ports labeled 1-5. All 5 of these ports are identical.
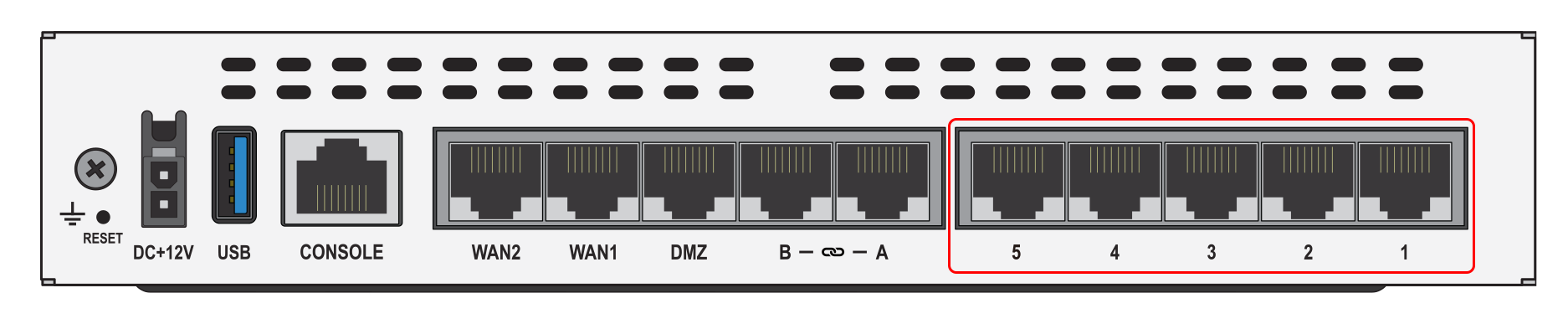
Ports A and B: Depending on your needs, PCC may have configured your router to also allow ports A and B to be used. Use these ports only if instructed to do so by PCC.
Connect Your Network Switch (optional)
Depending on the needs of your office, you may or may not use a network switch. If you use a switch, plug all devices, including the Fortigate, into the ports on the front of the switch. All ports work the same, and all ports communicate in both directions; you can plug any device into any port.

Connecting network devices via your network switch: If you are using a network switch, all the instructions below still apply. However, instead of plugging your other devices into your Fortigate firewall, plug them into your switch. The switch and your modem will be the only two devices connected to the Fortigate.
Connect Your Network Attached Storage
A Network attached storage (NAS) device is a RAID array of hard drives connected to your network that is used to store backups.
PCC is currently equipping our clients with the FreeNAS Mini E. To connect the Mini E to your firewall (or switch), use the lower-left ethernet port on the back of the Mini E.
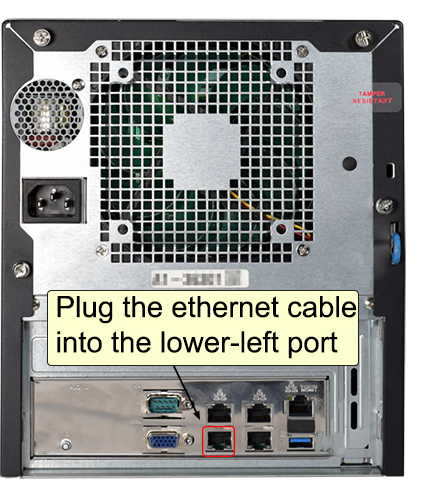
Connect Your Server
Your Dell server will need to be connected to your firewall (or switch) using two ethernet cables. Connect one using the “GB1” port, and the other using the “iDRAC” port.
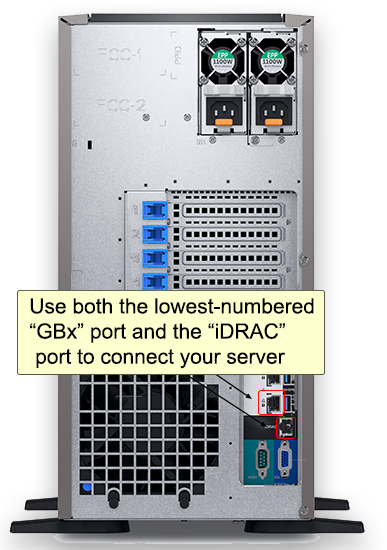
Connect Wireless Access Points
Your wireless access points should already have been installed around your office by your local IT support. Connect them to free ports in your firewall (or switch).
Connect Your Fortigate Firewall to Power
Turn on your modem first: Your modem should be powered on before you plug in your firewall.
Connect the power supply to the back of the device and plug it into a UPS battery device.
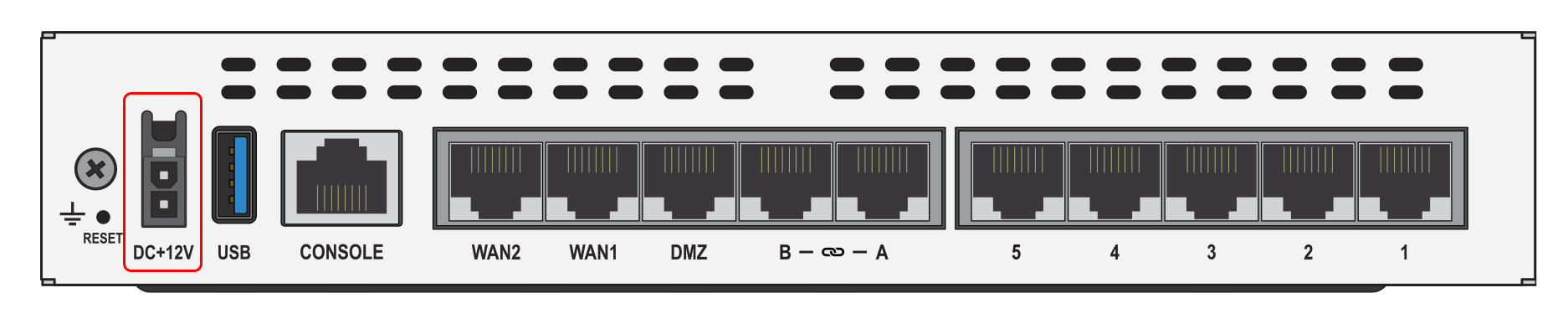
Your UPS looks like this:

The “PWR” and “STATUS” indicators on the front of your Fortigate firewall should light up green if the cable is pluged in correctly.
Power cable clicks into place: The power supply connector has a locking tab that will click into place. You must press the tab if you want to remove the cable from the firewall for any reason.
Wait for Your Devices to Connect
Depending on how quickly you plugged everything in, the Fortigate firewall may still need time to start up before you can connect to the network. If after 5 minutes you are unable to connect, please contact PCC for assistance.
Call PCC for assistance: If you need assistance at any point in this process, PCC is here to help! Call PCC Support at 800.722.7708. If possible, have a photo of the back of your Internet modem and the back of the Fortigate firewall available.
Send Broadcast Messages to Patients and Families
Use Broadcast Messaging in PCC EHR to send batches of messages to patients and families. You can use PCC’s Broadcast Messaging report, or customize any patient-based report, to create a patient list. PCC EHR will collect all contact information for the patient (emails and cellphones) and send the message to all of them.
Broadcast Messaging requires some initial setup before you can begin sending messages. Contact PCC Support to get started using Broadcast Messaging.
Watch a Video: You can learn how to use Broadcast Messaging in PCC EHR by watching the Send Broadcast Messages to Patients and Families video.
Send a Broadcast Message
Open the Report Library
Open the PCC EHR Report Library from the Reports menu.
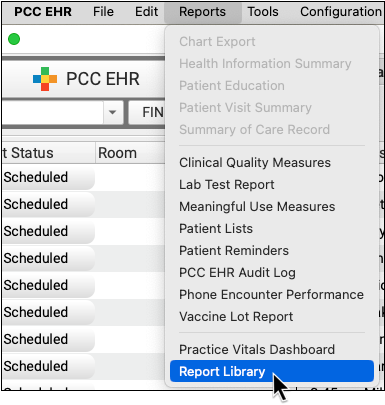
Select a Report
Select a report to begin building a patient list.
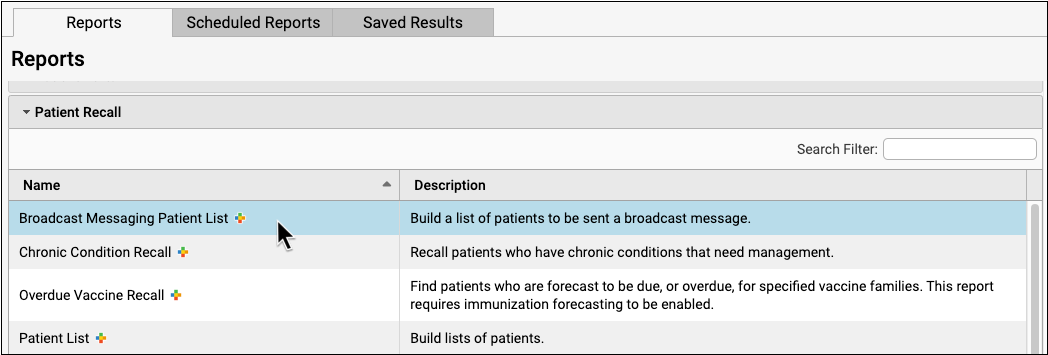
You can use the Broadcast Messaging Patient List or another report in the library.
Most EHR reports work with the broadcast messaging feature, including (but not limited to) those in the Appointment, Clinical, Immunization, and Patient Recall categories.
Select Report Criteria
Adjust the report criteria to create a list of patients and families you wish to contact.

The Broadcast Messaging Patient List includes a range of criteria for narrowing down the list of patients included in your report. For example, exclude by patient or account flag to ensure that inactive or deceased patients aren’t contacted, or select by care center flag to limit the results to patients of one care center.
By default, the Broadcast Messaging report includes all patients who have been seen in the past three years, are not marked as deceased, and who are under 21 years old.
Run the Report and Review the Patient List
Once you have adjusted the criteria to meet your needs, run the report, and check that the resulting list includes the patients or number of patients you expect.
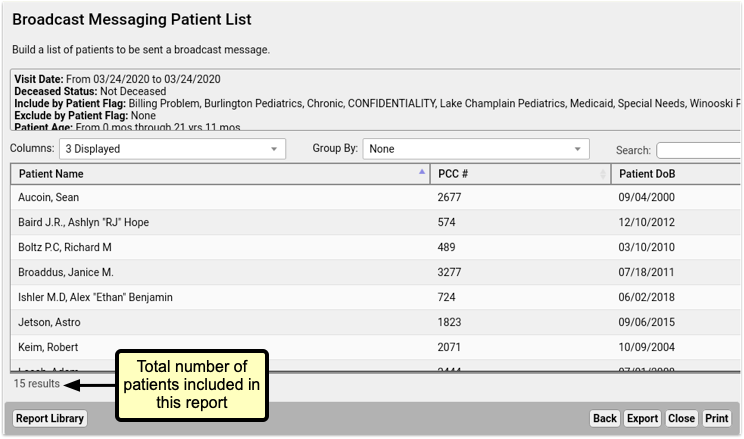
Export Your Results
Click the “Export” button at the bottom right of the results window.
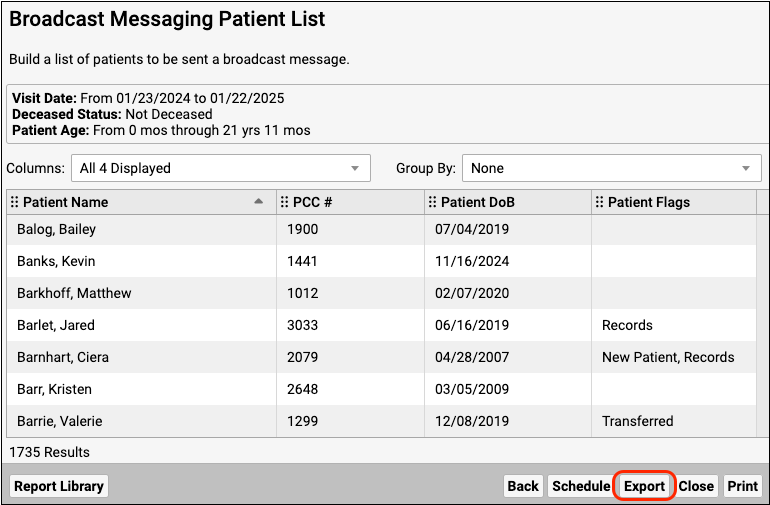
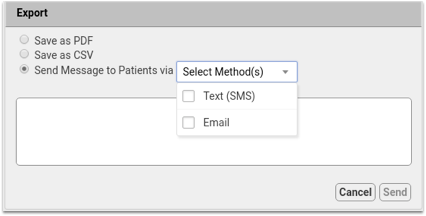
Select One or More Sending Methods
You’ll see three options, PDF, CSV, or “Send message to patients via” with the option to choose a sending method.
Select one or both of the sending methods, SMS or Email.
Compose a Message
Write your message.
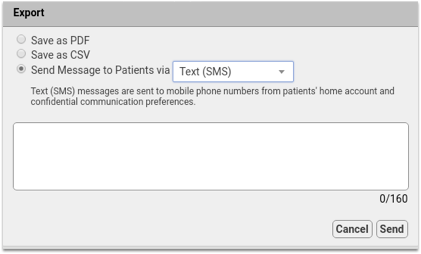
Text (SMS) messages are limited to 160 characters per message. The character count in the bottom right of the window shows how many characters you’ve used out of the 160.
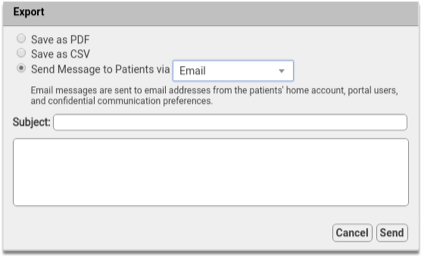
If you select the email option, you will see a subject line for the email. There’s no character limit to emails, so you can write as much as you need.
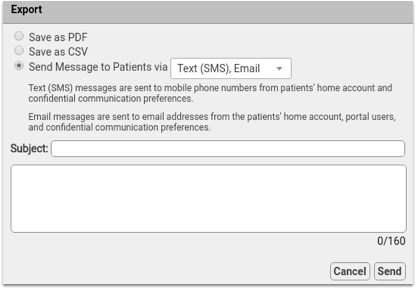
If you select both the Text (SMS) and Email options, you will see both the Subject field and and character count. When you send both message types, you’re limited to 160 characters. Anything in the Subject field will appear as the subject line of the email and the first line of the text message.
Include Your Practice Information: Broadcast Messages are plain text, and include nothing more than what you type. Be sure to include your practice name, and, if necessary, contact information, so the recipients will know who the message is from.
Send Your Message
When your message is complete, be sure to double check it, since there’s no going back after sending. When you’re happy with it, click send.
If you’ve chosen to send a message via text and email, the message will go out by both methods to the phone numbers and email addresses you selected in Practice Preferences to all accounts in your report result. Accounts may receive both an email and a text message.
Duplicate Email Address or Phone Numbers: If siblings or patients with shared custodian accounts appear in your search results, duplicate messages will not be sent. Only one message will be sent to each email address and phone number.
You’ll see a confirmation message, and you’ll be returned to the report results.
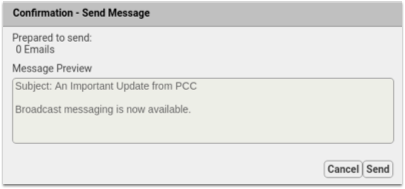
How Do I Get Started With Broadcast Messaging?
Begin by assigning permissions for broadcast messaging. Who at your practice will compose and send these messages? Broadcast Messaging is extremely powerful, and can send thousands of messages with just a few clicks.
Use the User Administration tool to add a new Role for Broadcast Messaging, and then assign that role to particular users at your practice.
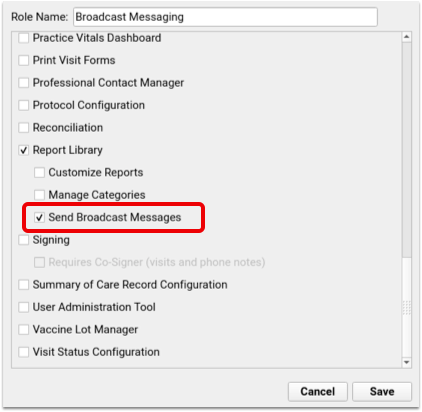
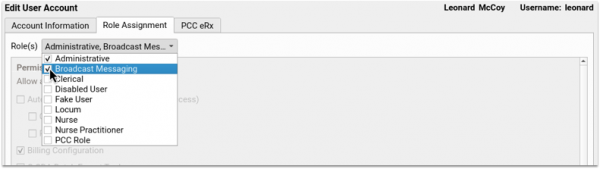
Select Which Phone Numbers To Use For Broadcast Messaging
By default, Broadcast Messaging sends text (SMS) messages to all available phone numbers and email addresses in the patient’s home account, confidential communication preference, and patient portal information. If you prefer to limit which contact methods Broadcast Messaging uses, you can now select which fields should be included in the Practice Preferences menu.
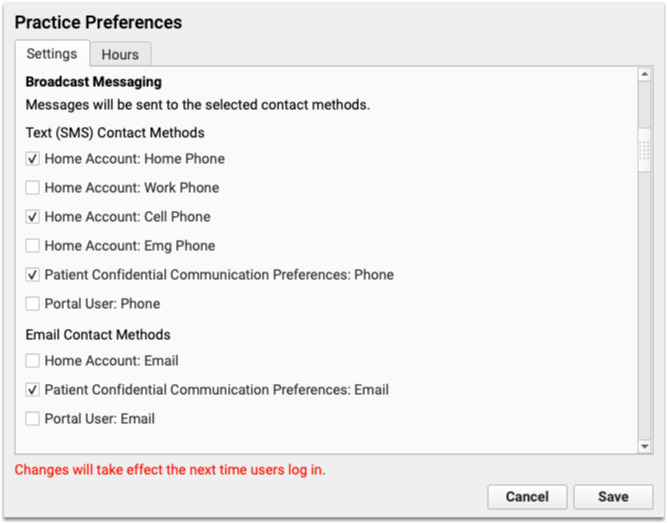
Who Will a Broadcast Message Be “From”? What If The Family Replies to the Message?
When a patient or family member receives an email from Broadcast Messaging, the message will be from your practice, with an email address noreply@CLIENT.pcc.com, where “CLIENT” will be replaced with your acronym.
If they reply to that email, it will go to a “noreply” email account on your PCC system, in order to filter bounced emails.
Your practice can configure who will receive a copy of these noreply emails. For example, families might reply to your message with a request to be seen, even though it says “noreply”.
PCC Support can configure what email address will receive copies of email replies from parents and families.
Text (SMS) Messages
When a patient or family receives a Text (SMS) message, it will appear to be from a phone number with your practice’s local area code. PCC provisions these lines, creating one number per-practice or multi-practice group.
You can ask PCC Support for details about this phone number, and optionally share it with your patients and families so they can know the number the messages will come from.
If a family responds to that text message, the Broadcast Messaging service will ignore that text.
Unsubscribing
If a patient or family does not wish to receive Text (SMS) messages from your practice, responding “stop” or “unsubscribe” will prevent that number from receiving texts in the future. Likewise, each email sent via Broadcast Messaging includes an unsubscribe link, that will remove the recipient’s email address from future mailings. These addresses and numbers will be moved to your blacklist, and appear there in the Broadcast Messaging Log Report
Unsubscribing Stops Patient Portal Messages and Direct Texts: Unsubscribing prevents the user’s phone number from being used for any reason by PCC. In addition to broadcast messages, unsubscribing will prevent a user from receiving Patient Portal notifications or direct messages via SMS.
If a patient or account has unsubscribed from Broadcast Messaging, and would like to receive your practice’s broadcast messages again, responding to a previous message with “unstop” will remove their number from the blacklist, and they’ll begin receiving your messages again.
To learn more about how you can help patients and families resubscribe to broadcast messages, read the article Help Families Resubscribe to Broadcast Emails and Text Messages From Your Practice.
Bounced Messages and Dead Phone Lines
PCC’s Broadcast Messaging service will automatically recognize when an email address fails, or a cell phone number fails. When that happens, PCC will automatically add that cell phone number or email address to a black out list so your practice does not send messages to disconnected numbers or emails.
Repeated messages to dead emails or cell phones can lead to your system being identified as a spam service. PCC has set up the blacklist feature to avoid this.
Spam and Invalid Email Address
If the email address is not unsubscribed but still not receiving emails, then either the email address itself is incorrect, or the recipient has marked messages from Patient Portal or Broadcast Messaging as spam or junk. Broadcast Messaging and Patient Portal messages will not be sent to any addresses that have marked a previous messages as spam. The recipient must resolve the invalid spam complaint then use the resubscribe link from a previous PCC email.
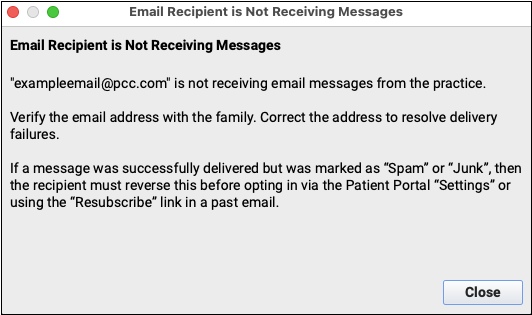
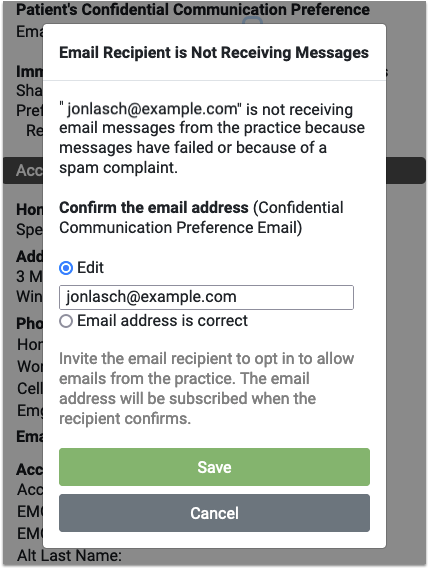
If the email address is not unsubscribed but still not receiving emails, you’ll find the option to correct any typo in the email address, or mark the email address as correct. Marking the address as correct does not guarantee the next message will send, but it clears the error and attempts to send future messages
Broadcast Messaging Log
PCC EHR’s Report Library includes a Broadcast Messaging Log, which tracks all Broadcast Messages sent. You can review historical messages and see results of each batch of messages.
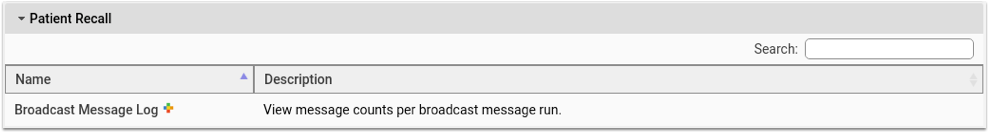
Broadcast Message Log is found in the Communication category and the Patient Recall category in the Report Library, and can be run for a range of dates and limited by user.
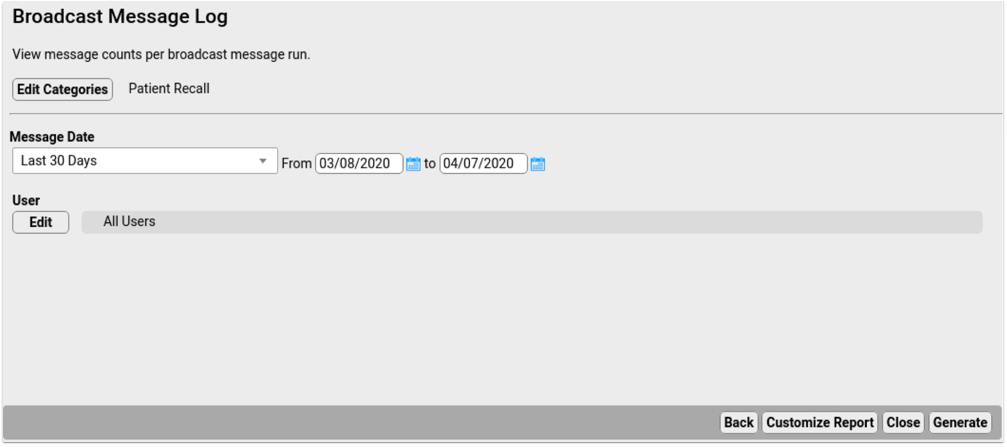
Results include the date and time of each message run, the user who sent the message, the message content, type and count of messages, both email and SMS, were attempted, how many were sent successfully, and how many failed.
Broadcast Messaging Details Report
The Broadcast Message Details report provides detailed results of a single broadcast message run. You’ll find it in the Patient Recall category.
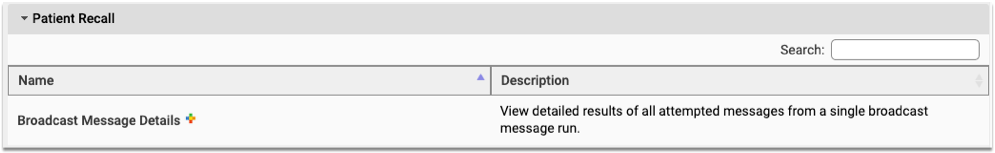
The communication log criteria lists all previous Broadcast Message runs. Select one from the drop-down menu and click Generate to run the report and see the results of that run.
The results show the date and time of the run, each recipient, the patients associated with each email address or phone number, the status, and a blacklist column.
If an email or phone number is added to the blacklist, the Excluded from Future Broadcasts column indicates a reason why a contact method has been added. If a text message is sent to a landline, that number is added to the blacklist with the reason “Not Text Enabled”. “Validation Failed” indicates an email address that is invalid or no longer exists.
Review Replies with the Inbound Messages Report
When a recipient of a Broadcast Message replies via email or text, you can review those replies in the Inbound Message report in the Report Library’s Communication category.
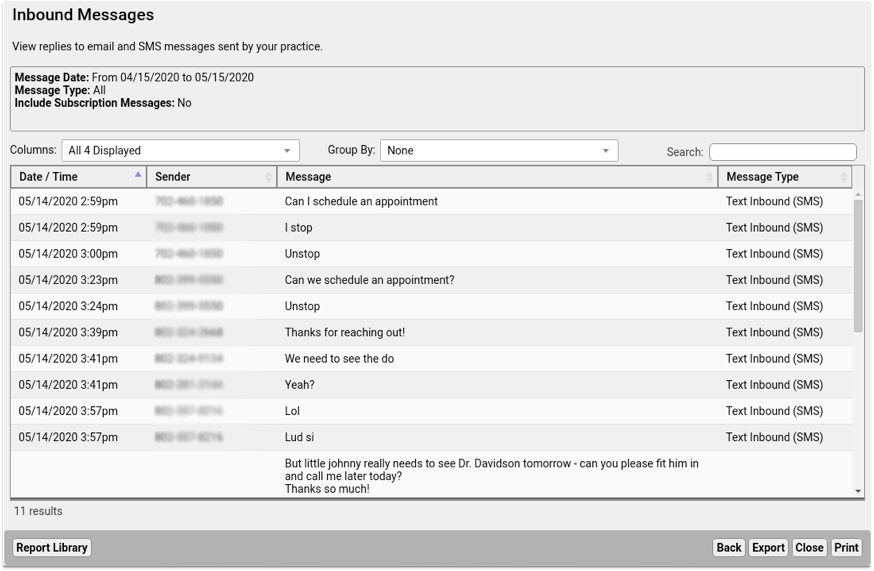
Here you’ll see all replies, including automatic responses from emails, and direct replies from users. You can use these results to keep your user’s contact information updated, or follow-up with users who need additional help or answers.
COVID-19 Links and Resources
This page was created in 2020 and updated throughout the first few years of the COVID-19 pandemic. Follow the links below to find content, services, and features collected by PCC to help pediatric practices during the COVID-19 Coronavirus crisis.
Rapid Development of COVID-19 Related Features: PCC launched a series of rapid updates in response to the COVID-19 pandemic. In 2020, we beta tested and rolled out new functionality, and then released six major updates to all clients with new features for telemedicine, office communication, COVID-19 vaccine support, and more. To review these new features, visit the Updates page.
COVID-19 Vaccines
PCC EHR supports tracking the administration, charting, and billing of the new COVID-19 vaccines. Whether or not your practice administers a COVID-19 vaccine, you can configure PCC EHR to display the vaccination on chart immunization records when patients are vaccinated.
-
Continuous Updates to Your System: During 2021, PCC continually patched and updated client systems with new CVX, MVX, VIS listings, billing code validation, and corresponding information as new vaccines were approved and new codes announced.
-
Read the Latest News: PCC tracked the development of COVID-19 vaccines. We published several blog posts, including: Pediatric COVID Vaccinations: How to Prepare Your Practice and Discussing Benefits of COVID-19 Vaccination with Families.
Get Started With COVID-19 Vaccines in PCC EHR: For a guide to available vaccines, how to set them up in your PCC system, and how to order, administer, bill, and track a COVID-19 vaccine, read COVID-19 Vaccines in PCC EHR: Configure, Order, Administer, and Track.
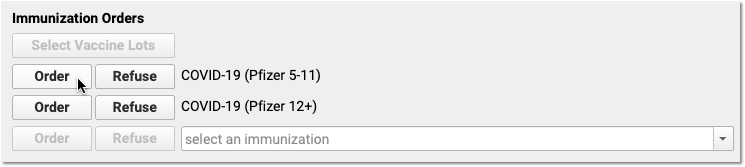
Connect With Patients and Families During the COVID-19 Pandemic
- Why and How Pediatric Practices Should Launch a Recall Initiative Today
- Run a Pediatric Drive-Thru Flu Shot Clinic
- Schedule, Chart, and Bill for a Telemedicine Encounter (Video, Article)
- Send Broadcast Messages to Patients and Families (Video, Article)
- Bill For Phone Calls and Portal Message Encounters (Video, Article)
- Create a Telemedicine Visit Protocol (Video, Article, Sample Protocol)
- Send a Single Text Message Directly to a Family Waiting in Their Car (Video Coming Soon, Article)
- Connect to Your PCC System From Home
- Telemedicine Billing Code Time Table
- Telemedicine Vendors for Pediatric Practices
- Video: Dr Hagan On Performing Well Visits via Telemedicine
- What Are the Current Telemedicine Rules in Your State? The Center for Connected Health Policy is regularly updating a state-by-state chart of Telemedicine guidelines. Visit their COVID-19 RELATED STATE ACTIONS page, and then click the “View a Quick Reference Chart” link for the most up-to-date information.
Code and Bill During the COVID-19 Pandemic
- Code and Bill for a COVID-19 Related Encounter
- Create COVID-19 Lab Orders in PCC EHR (Video, Article)
- Change an Encounter’s Billing Place of Service After Posting Charges
- PCC’s COVID-19 Coding Guide (PDF)
- Web Lab: March 2020 Pediatric Coding Web Lab featuring COVID-19 coding issues
- Webinar: Telemedicine Services – Usage, Billing, & Coding During COVID-19 with PCC’s Jan Blanchard (SOAPM 2020 ‘Fireside’ Series)
- Password: soapm_COVID-19
- March 2020 SNOMED-CT Update Adds COVID-19 Diagnosis and More
Other PCC COVID-19 Information Resources
- Best Practices for Pediatrics in the COVID-19 Era
- Apply to the CARES Act Provider Relief Fund for Medicaid
- Analyze and Respond to COVID-19’s Impact in Your PCC Dashboard
- See the The Business Impact of COVID-19 on Pediatric Practices across all PCC practices
- COVID-19 Community Forum for Pediatricians
- The PCC Blog
- Chip’s Blog
- Webinar Series: The Business Impact Of COVID-19 On Pediatric Practices
- Watch The Business Impact Of COVID-19 On Pediatric Practice part 5 recorded Thursday, April 16th
- Read PMI’s white paper The Uncertain Future Of Pediatric Practices As The COVID19 Pandemic Evolves by Paul D.Vanchiere, MBA
Useful Information From Other Sources
American Academy of Pediatrics
Center for Disease Control
World Health Organization
Other
Schedule, Chart, and Bill a Telemedicine Visit
Read the procedure and recommendations below to learn how to schedule, chart and bill a telemedicine visit with PCC.
Watch a Video: You can watch an overview of a telemedicine workflow in PCC EHR by viewing Schedule, Chart, and Bill a Telemedicine Encounter.
Configuration: To learn how to configure PCC EHR for telemedicine, read Configure PCC EHR for Telemedicine Encounters.
Perform a Telemedicine Visit
Read the procedure below for an overview of how to schedule, chart, and bill a telemedicine encounter in PCC EHR.
Schedule the Patient’s Appointment
Use the Appointment Book to schedule a patient, just as you would any other encounter.
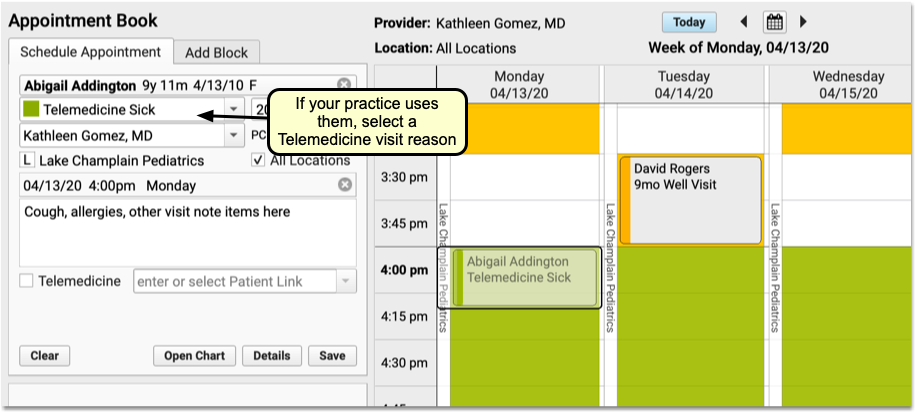
If your practice uses telemedicine visit reasons, mapped to specific telemedicine chart protocols, be sure to select one. As you schedule, you can review telemedicine consent, insurance information, and any additional details you normally confirm with the patient or family.
To learn more about the Appointment Book, visit Schedule Patients in the Appointment Book.
Unplanned Telemedicine Encounters: Even if you are recording a telemedicine encounter that happened yesterday or are created on-the-fly during a phone call, PCC recommends you schedule Telemedicine appointments so they appear in the clinician’s schedule and are ready to chart and bill.
Click “Telemedicine” and Optionally Enter a URL For Connecting
When you create the appointment, check the “Telemedicine” option near the bottom of the Schedule Appointment tab.
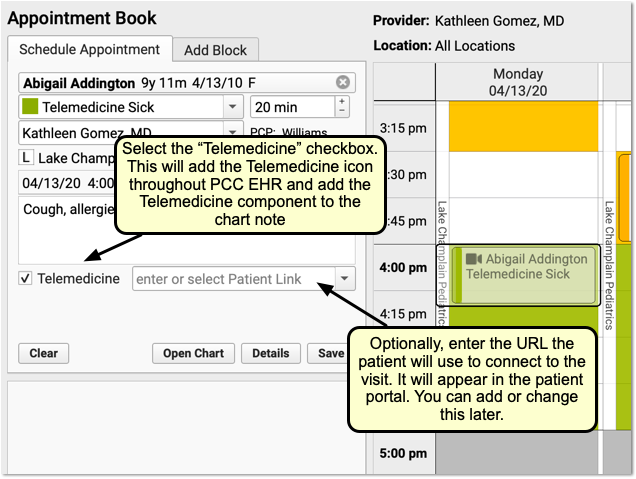
If available, enter the URL web address that the patient or family will use to connect to the visit. If your practice has a set of persistent URLs, you can select from a drop-down menu.
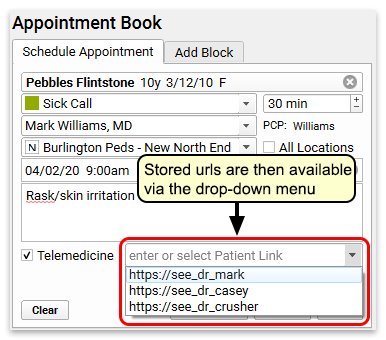
The URL link will appear in the patient portal for the family.
I Don't Have the URL Yet!: Depending on the video telemedicine tool you use, you may not know this URL at the time you schedule the appointment. That’s ok! You can leave this blank and fill it out later, either here in the Appointment Book or directly on the patient’s chart.
Create and Share Telemedicine Connection Information
After you schedule the appointment in PCC EHR, you may need to also create an appointment with your third-party telemedicine vendor. You may need to share the connection address with the family at a later date. Incorporate these needs into your practice’s scheduling procedure so that when it is time for the visit, both the clinician and family know what to do.
Your practice can store and retrieve telemedicine connection information on the appointment, as shown above, as well as in the Telemedicine component that appears at the top of all telemedicine visits.
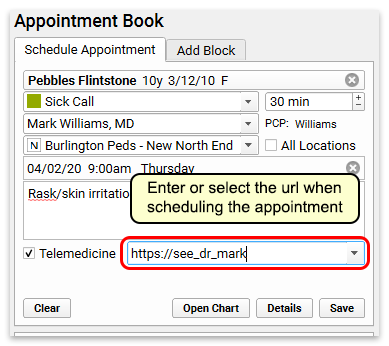
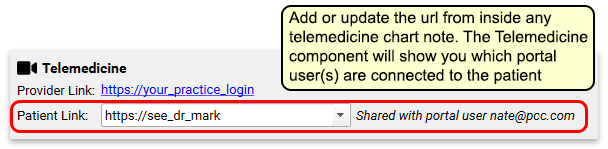
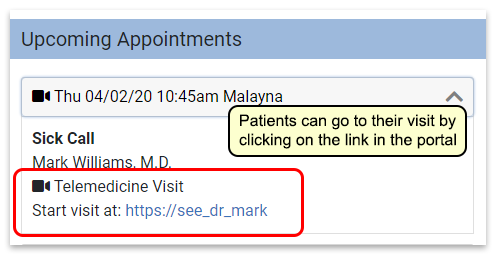
You can add the URL to this field at any time, and it will appear in the patient’s portal. You can also email or text the link to the patient or family.
Check Eligibility, Send Reminders
As you would for any other appointment, your practice can use PCC’s tools to check patient insurance eligibility and send appointment reminders.
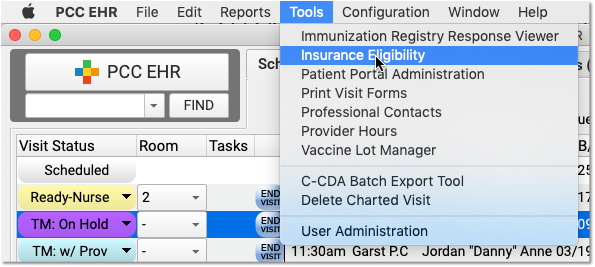
Is This Telemedicine Visit Billable?: Insurance requirements and payment differ for every payer, and often on a state-by-state basis. PCC recommends that you contact major payers and learn what they require for telemedicine visits. While the COVID-19 crisis improved payer responsiveness to telemedicine services, historically there has been a wide range of support and payment from payer to payer. PCC discusses trends such as this at our monthly Billing Drop-In.
Manage Your Schedule in PCC EHR
You can easily see which visits on the schedule are telemedicine visits thanks to the telemedicine video camera icon.
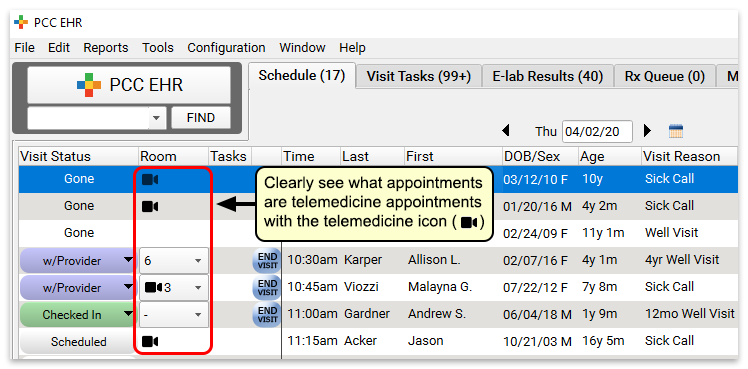
Do We Check In Patients?: Depending on your telemedicine workflow and the tools you use, your practice may have to adjust your check in procedures for telemedicine visits. Your front desk might connect with the patient first via phone to go over insurance and other check-in details, or the clinician might start the visit. Your practice can create custom telemedicine Visit Statuses to track these steps and help coordinate patient flow.
Connect to Your Telemedicine Platform
When it’s time for the visit, connect to your telemedicine platform. Typically, your clinicians can do this from the link at the top of the chart note.
If your practice works with multiple vendors or uses a different method to open a connection, you will need to share that with each clinician.
Some clinicians have told PCC that they prefer to connect on one computer monitor and use another monitor to chart and take notes during the encounter.
Why Isn't My Link Clickable?: If you connect to PCC EHR through a remote client, such as by using remote desktop protocol, then the link will not be clickable. Instead, you can copy and paste that link into your browser.
Open the Chart, Set Status, and Begin Telemedicine
Next, the clinician double-clicks on the patient’s name to open the chart and begin the visit.
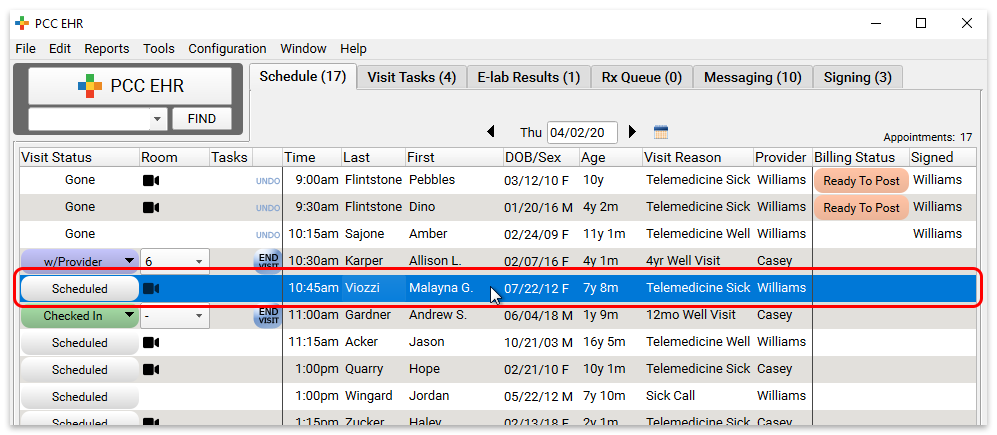
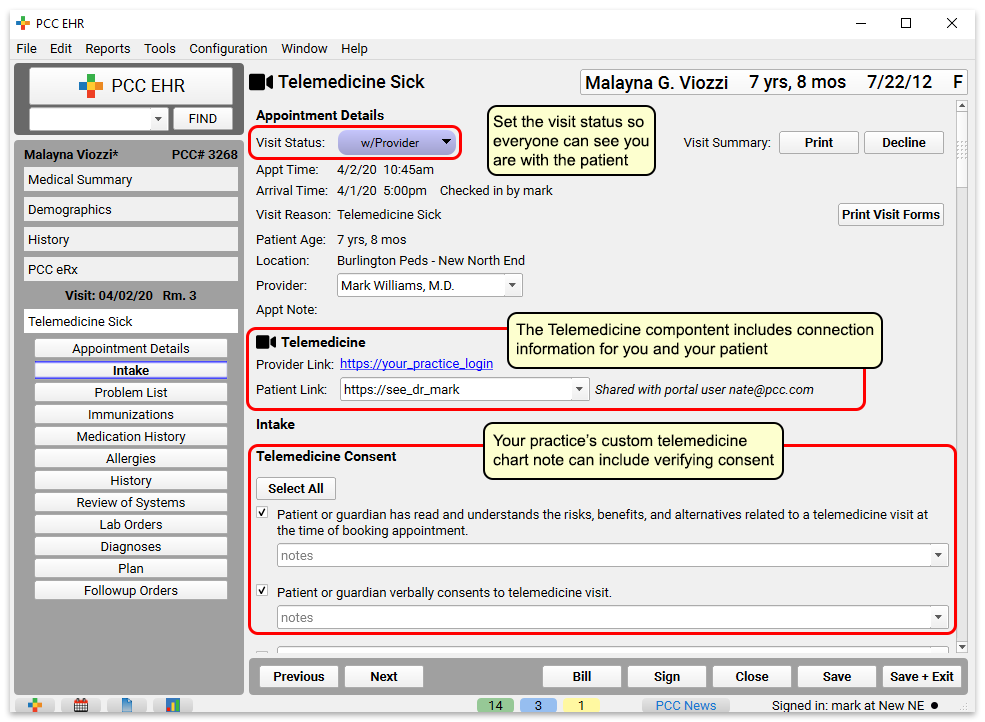
The clinician can set their status to inform the practice the visit has begun. Connection links will appear in the Telemedicine component at the top of the chart note.
Your practice could include a “Telemedicine Consent” component at the top, as illustrated above.
Chart the Encounter
Clinicians can use your practice’s customizable telemedicine chart note protocol to review vitals, history, and perform other steps.
Collect and Record Vitals During a Telemedicine Visit?: Your practice may want to collect vitals as reported by the parent or patient, and indicate the source of that information. You could use PCC’s standard Vitals component and indicate they were reported and not measured, or you could create custom components to indicate the source of information.
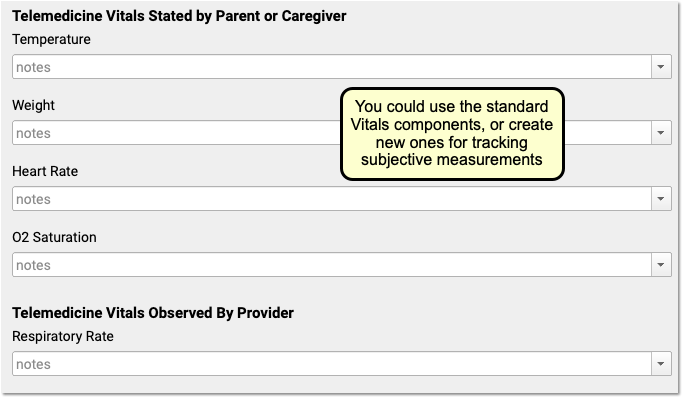
For more tips on designing a great telemedicine chart note protocol, read Create a Telemedicine Chart Note Protocol.
Select Diagnoses, Orders, and Indicate Other Procedures
After a visit is complete, the clinician should double-check diagnoses along with procedures and other orders on the chart note.
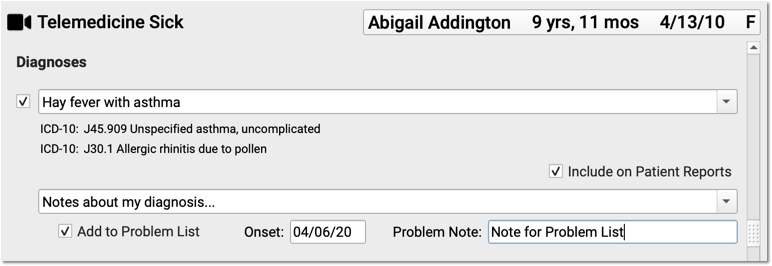
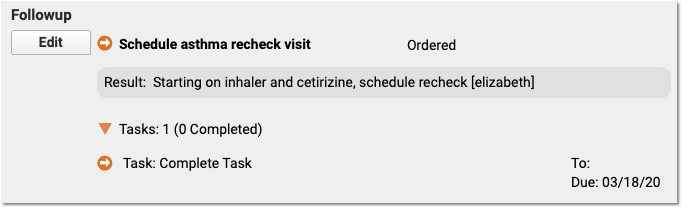
You can also click “PCC eRx” to create prescriptions. New and renewed prescriptions will automatically append to the bottom of the chart note.
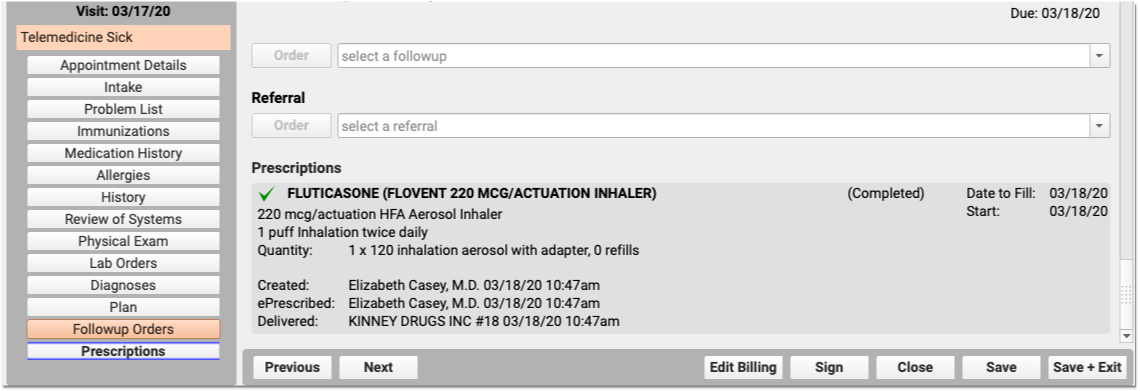
Click “Bill” and Select a Visit Code
Next, click “Bill” to review and select codes on the Electronic Encounter Form.
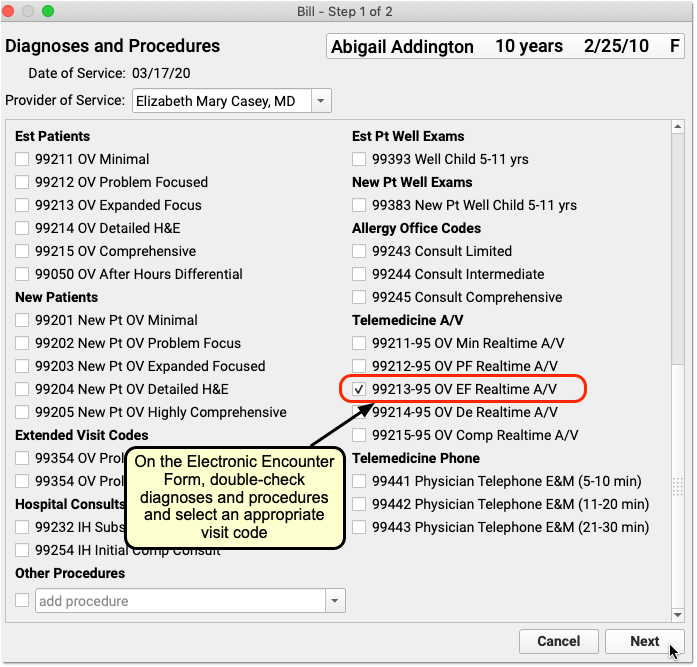
The Electronic Encounter Form displays all diagnoses and procedure codes from items the clinician selected on the chart note. They will typically select a visit code manually.
For a telemedicine visit, you might select a -95 code for a live audio and video E&M visit. For a phone-only visit, you might use time based codes 99441-99443. Check out the configuration article to learn about other telemedicine visit codes. PCC also created a Telemedicine Timing reference sheet.
Update Units and Linking, and “Make Ready for Billing”
After you review and add codes, you can review units and which diagnosis is linked to each procedure. Next, make the visit ready for billing.
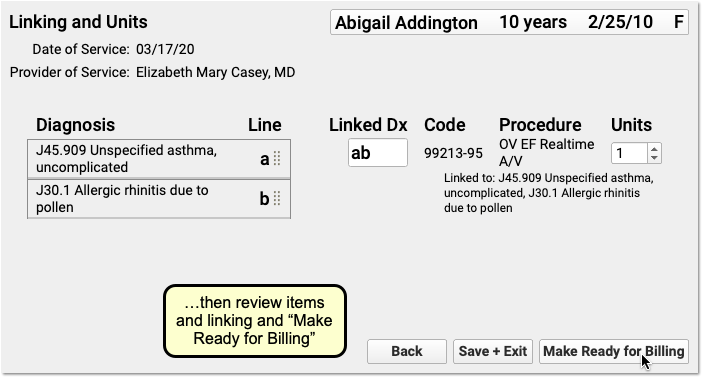
Sign the Chart Note
Complete charting and sign the chart note just as you would for other encounters.

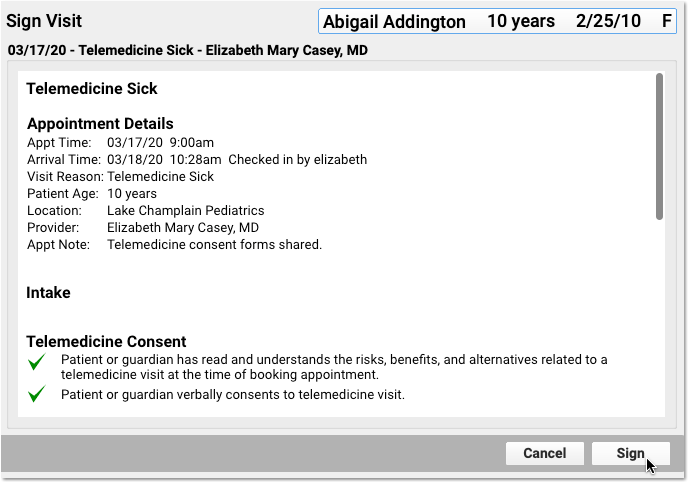
PCC EHR supports cosigning providers if needed.
Click “Ready to Post” and Review the Billing Place of Service
After the clinician has made the encounter ready for billing, your practice can click “Ready to Post” to post charges.
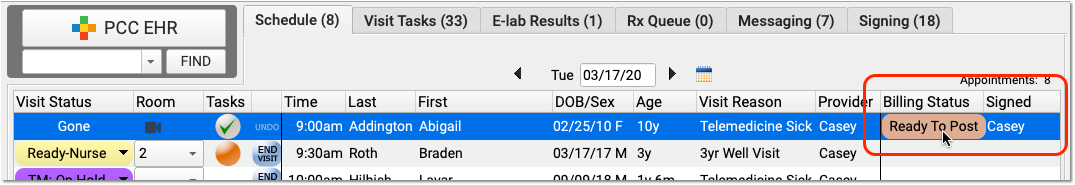
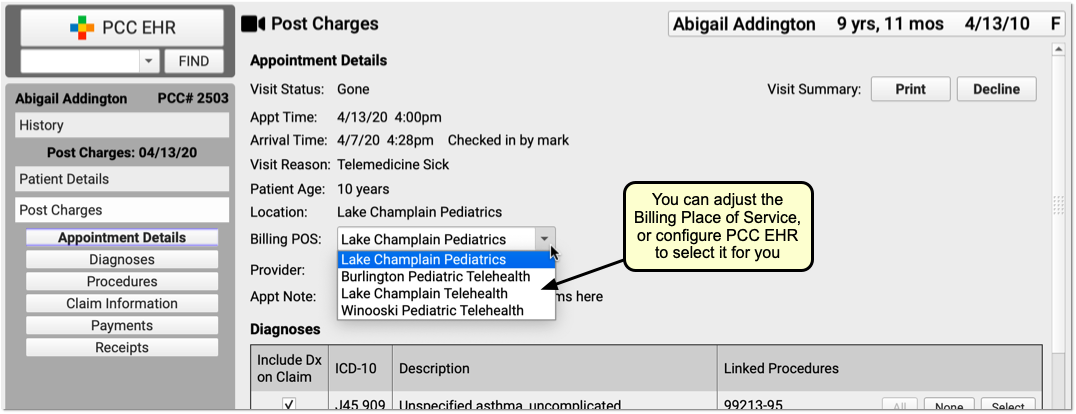
Review the appointment details and optionally select a new Billing Place of Service.
Automatic Telehealth Place of Service: PCC EHR can automatically select an appropriate telemedicine place of service based on your practice’s configuration. Alternatively, you can select a Billing Place of Service manually when you post charges. If a patient is seen for both a telemedicine and an in-person encounter on the same date, with the same clinician, charges with different places of service will result in two separate claims (as of PCC 9.4).
Update Diagnoses, Procedures, Claim Information, and Payments
Next, the biller can make any required adjustments to diagnoses, procedures, claim information, or payments.
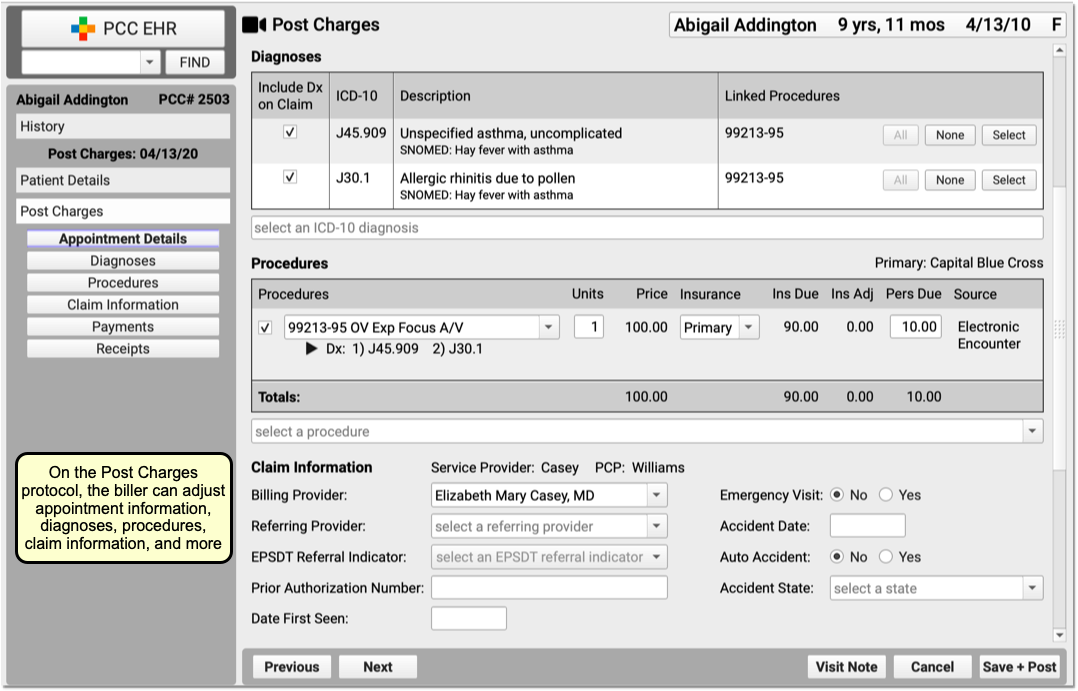
Billing for telemedicine is a rapidly evolving issue. Contact your payers to review their requirements.
Click “Save + Post” to Queue Up a Claim
Finally, the biller clicks “Save + Post” to post the charges and queue up a claim.
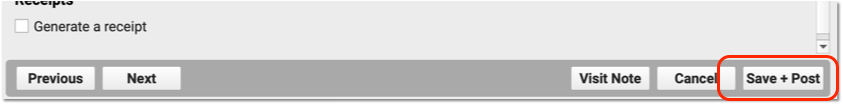
Later, the biller can come back to Post Charges if they need to add additional items.
Optional: Post Charges in Practice Management Instead
If your billers prefer the older Post Charges (checkout, chuck) charge posting tool, they can use it instead.
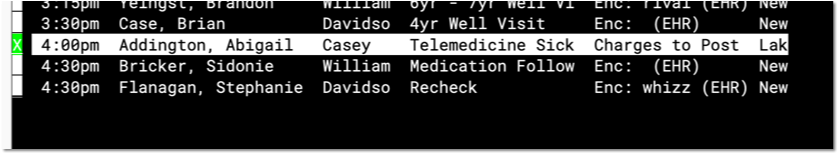
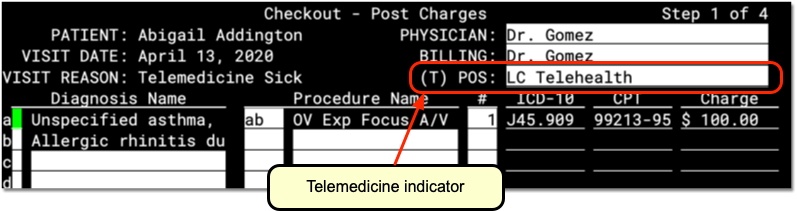
While the Practice Management interface does not include all functionality found in PCC EHR, some billers prefer it.
Just as they can in PCC EHR, the biller can review details and make any adjustments needed to diagnoses, procedures, or claim information. Then they can post the charges and payments and queue up a claim.
Bill for a Phone Call as a Telemedicine Encounter
By using the above procedure, you can schedule, chart, and bill for a telemedicine encounter.
You can also turn phone calls that a clinician charted on a PCC EHR phone note into a billable telemedicine encounter.
Read Bill for Phone Calls and Portal Messages to learn more.
Bill for Patient Portal Messages as a Telemedicine Encounter
Your practice may help patients by exchanging secure portal messages, email, or other asynchronous text communication. You can bill for those encounters as a telemedicine visit, though many conditions apply.
You can bill for portal messages in PCC EHR using the same tools and workflow you would use for phone encounters. Read Bill for Phone Calls and Portal Messages to learn more.
Other Telemedicine Resources
As you research tools and procedures for telemedicine in your practice, you may find these helpful:
New User Training for Front Desk Staff
Use the new user training outline below to learn how to complete front desk tasks in PCC.
For personalized training, help with configuration, or other needs, contact PCC Support.
Get Started
Learn how to log in, navigate in PCC EHR, and use chat.
Log In to PCC EHR
- Log In and Navigate PCC EHR
- Log In to PCC EHR
- Change Passwords and Other User Account Settings
- Connect to Your PCC System from Home
Navigate PCC EHR
Chat with Colleagues
Schedule Appointments
Find open slots on the schedule by provider and location, then book appointments for patients and their siblings.
- Schedule a Patient in the Appointment Book
- Schedule for Providers Across Multiple Locations
- Schedule Multiple Appointments in the Appointment Book
- Schedule a Patient
Update Demographics and Insurance Policy Information
Work with patient and family account records and update a patient's insurance policies.
- Review and Update Patient and Family Demographics
- Update a Patient’s Insurance Policies
- Review and Update Patient and Family Demographics
- Review and Update Patient Insurance Policies
- Find Patients and Accounts
- Add New Patients and Accounts
Verify Insurance Eligibility for Encounters
You can review insurance eligibility en masse for all upcoming encounters, or for a single patient's encounter.
Check In a Patient
Update demographic information, verify insurance policy details, and collect copays when patients arrive for their appointments.
Work with Account Notes and Encounter Billing Notes
Whenever you work with a family on a billing issue, you may want to take notes on the account. You may also have encounter-specific billing notes as you work on a rejected claim.
- Account Notes and Encounter Billing Notes
- Enter and Review Account Notes
- Enter and Review Encounter Billing Notes
Communicate with Patients and Take Messages
Learn how to take notes during patient phone calls, send text messages to patients and families, and communicate with patients and families through the patient portal.
Work with Phone Notes
- Work With Phone Notes and Tasks
- Create Referrals, Labs, and Orders on Phone Notes (and Other Messages)
- Create a Phone Note
Send Text Messages to Patients and Families
- Send a Text Message Directly to a Patient or Family
- Send a Text Message Directly to a Patient or Family
Communicate with Patients and Families through the Patient Portal
- Reach Patients and Families with the Patient Portal
- Receive and Respond to Patient Portal Messages from My Kid’s Chart
- Adding and Managing Patient Portal User Accounts
Import, Work With, and Share Patient Documents and Forms
Learn how to get documents into PCC EHR, attach them to patient charts, and generate forms for patients and families.
- Import and Work With Documents
- Scan, Fax, or Print a Document into PCC EHR
- Import and Attach a Document to a Patient’s Chart
- Work with Documents in a Patient’s Chart
- Make Documents Available to Patients and Families in My Kid’s Chart
- Generate Forms in PCC EHR
- Print Visit Forms
Manage the Schedule and Complete Tasks
Ensure the schedule remains accurate throughout the day and complete tasks assigned to the front desk.
- Use Visit Status Counters to Know Where You’re Needed
- Work with Today’s Patients on the PCC EHR Schedule Screen
- Mark an Appointment As Missed or Canceled
- Work on Messaging Tasks, Document Tasks, Call Backs, and More
Reconcile Payments at the End of the Day
Make sure the money you collected was entered correctly into PCC EHR.
Recall, Remind, and Notify Patients
Send one-time or recurring notifications to patients and families.
Send Routine Appointment Reminders
Send Broadcast Messages
Recall Patients Who Are Due for a Visit
Front Desk Essentials and Best Practices
Perform Telemedicine Encounters
Schedule, check-in, and manage the flow of telemedicine visits like a pro in PCC EHR.
New User Training for Clinicians
Use the new user training outline below to learn how to complete clinical tasks in PCC.
For personalized training, help with configuration, or other needs, contact PCC Support.
Get Started
Learn how to log in, navigate in PCC EHR, and use chat.
Log In to PCC EHR
- Log In and Navigate PCC EHR
- Log In to PCC EHR
- Change Passwords and Other User Account Settings
- Connect to Your PCC System from Home
Navigate PCC EHR
Chat with Colleagues
Review a Patient Chart
- Review a Patient Chart in PCC EHR
- Navigate a Patient’s Chart
- Clinical Alerts
- The Medical Summary
- The Visit History Screen
- Growth Charts
- Flowsheets
- Allergies
- Immunization Forecasting
- Review and Edit Sibling Charts
- Search the Patient Visit History or within a Charted Encounter
Chart a Patient Visit
Patient Intake
Room the patient, review and update patient information, and begin collecting clinical data.
- Patient Intake
- Review and Update Patient and Family Demographics
- Review and Update Patient and Family Demographics
- Review and Update a Patient’s Immunization Record
During patient intake, you can also:
- Record the Patient’s Chief Complaint
- Record Multiple Measurements of Patient Vitals
- Update the Patient’s Preferred Pharmacy Information
- Review and Update the Patient’s Medication History
- Check if the Patient Needs a Prescription Refill
Chart an Encounter
- Chart a Visit in PCC EHR
- Chart with Multiple Protocols
- Chart with Answer Memory, Last Answer, and Your Custom Auto-Notes
- Expand Short Text into Common Phrases in PCC EHR
- Chart a Visit in PCC EHR
- Chart Note Protocols
- Chart with Answer Memory, Last Answer, and Your Custom Auto-Notes
- Expand Short Text into Common Phrases in PCC EHR
- Spell Check in PCC EHR
Record Diagnoses
- Find and Refine Diagnoses as You Chart
- Hide Sensitive Diagnoses from the Patient Portal and Patient Reports
Create and Complete Medical Procedure, Screening, Lab, and Other Orders
Learn how to order discrete tests, procedures, labs, handouts, and more, create tasks from those orders and assign them to your coworkers, and mark orders as complete when all the tasks are done.
- Create and Complete Orders in PCC EHR
- Create Referrals, Labs, and Orders on Phone Notes (and Other Messages)
- Orders Overview (Labs, Procedures, Supplies, Immunizations, and More)
- Order a Lab, Procedure, Supply, or Other Order
- Fulfill Orders and Complete Tasks
- Find Incomplete Orders by Date Range and Order Type
- Use Orders to Track Clinical Measures for Reporting, Mandates, and Incentive Programs
Order and Administer Immunizations
- Review, Order and Administer Immunizations
- Manage Immunization Lots and Track Vaccine Inventory
- Review, Order, and Administer Immunizations
- Manage Immunization Lots and Track Vaccine Inventory
- Use a Barcode Scanner to Manage Immunization Lot Inventory
Send Out for Labs and X-Rays
- Generate Outbound Lab and Radiology Requisitions in PCC EHR
- Add E-Lab Users and Import E-Lab Results
- Generate Outbound Lab and Radiology Requisitions
- Manage Incoming E-lab Test Results
Find and Share Handouts with Patients
Complete Visit Tasks and Order Follow-Ups
Prescribe Medications
Record patient medications and allergies, prepare or renew prescriptions, automatically check for patient safety before printing or electronically sending prescriptions to the pharmacy, and customize PCC eRx to your preferences.
- Prescribe Medications
- Manage Prescription Activity on the Rx Queue
- Prescribe in pocketPCC
- Prescribing 101: PCC eRx Essentials for New Users
- Prescribing 201: Beyond the Basics of PCC eRx
- PCC eRx – EPCS Enrollment
- Check Prescription Pricing and Insurance Coverage While You Prescribe
- Resend a Prescription
- Prescribe Medications
- Manage Prescription Activity on the Rx Queue
- Allergies
- Review and Update Medication History
- PCC eRx Prescription Favorites
- Create Custom Medications and Sentences in PCC eRx
- Register for EPCS
- Prescribe Controlled Substances (EPCS)
- Manage Your EPCS Account, Tokens, and Password
- Work with Pharmacies
- Check Prescription Pricing and Insurance Coverage While You Prescribe
- Resend a Prescription
- Prescribe in pocketPCC
Prepare an Encounter for Billing
When a visit, phone call, or other billable encounter is finished, prepare it for billing.
Sign Encounters, Orders, and Results
Ensure that providers review and sign chart notes and results.
- Review and Sign Visits, Orders, and Other Items in PCC EHR
- Sign Visit Chart Notes
- Sign Phone Notes
- Sign Orders
- Signing Documents
- Co-Sign Visit Chart Notes
Communicate with Patients and Take Messages
Learn how to take notes during patient phone calls, send text messages to patients and families, and communicate with patients and families through the patient portal.
Work with Phone Notes
- Work With Phone Notes and Tasks
- Create Referrals, Labs, and Orders on Phone Notes (and Other Messages)
- Create a Phone Note
Send Text Messages to Patients and Families
- Send a Text Message Directly to a Patient or Family
- Send a Text Message Directly to a Patient or Family
Communicate with Patients and Families through the Patient Portal
- Reach Patients and Families with the Patient Portal
- Receive and Respond to Patient Portal Messages from My Kid’s Chart
- Adding and Managing Patient Portal User Accounts
Exchange Clinical Records
Electronically exchange patient records with other healthcare providers.
- Get Started with Direct Secure Messaging
- Send, Receive, and Reconcile Direct Secure Messages
- Clinical Document Exchange: Initiator Role
- Clinical Document Exchange: The Responder Role
- How to Respond to Record Requests with PCC EHR
- Send and Receive Direct Secure Messages
- Securely Retrieve Clinical Documents from Hospitals and Other Providers
Import, Work With, and Share Patient Documents and Forms
Learn how to get documents into PCC EHR, attach them to patient charts, and generate forms for patients and families.
- Import and Work With Documents
- Scan, Fax, or Print a Document into PCC EHR
- Import and Attach a Document to a Patient’s Chart
- Work with Documents in a Patient’s Chart
- Make Documents Available to Patients and Families in My Kid’s Chart
- Generate Forms in PCC EHR
- Print Visit Forms
Perform Telemedicine Encounters
Schedule, check-in, and manage the flow of telemedicine visits like a pro in PCC EHR.
- Schedule, Chart, and Bill a Telemedicine Encounter
- Schedule, Chart, and Bill a Telemedicine Visit
- Best Practices for Pediatrics in the COVID-19 Era
Work in Patient Charts from Any Web Browser or Mobile Device
Upload photos, record vitals, and make other updates to patient charts from any web browser or mobile device.
- Get Started in pocketPCC
- Signing in pocketPCC
- Get Started in pocketPCC
- Navigate in pocketPCC
- Find a Patient in pocketPCC
- Review a Patient’s Chart in pocketPCC
- Enter Vitals in pocketPCC
- Use pocketPCC to Add Photos or Upload Files to Patient Charts
- Sign Notes, Visits, and Documents in pocketPCC
- Create and Edit Phone Notes in pocketPCC
- Receive and Send Patient Portal Messages in pocketPCC
- Add pocketPCC to Your Home Screen
Add Additional Races, Ethnicities, and Languages in PCC EHR
When you update a patient’s demographics, you can select from your practice’s list of races and ethnicities and enter any language from the full CDC OMB lists. You can have up to three races, ethnicities, and languages listed on a patient’s chart.
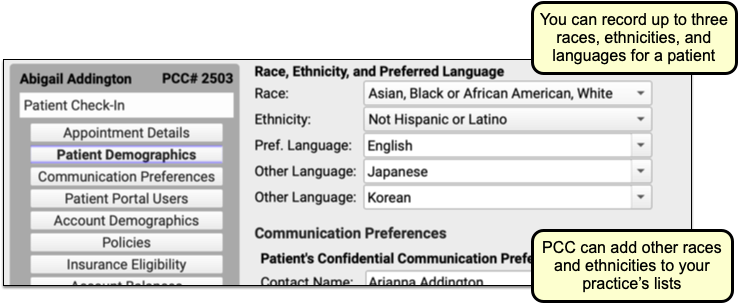
PCC EHR includes a default list of races and ethnicities, but your practice can optionally add any race or ethnicity from the full CDC OMB lists.
For convenience, you can search the list below to see if what you need is available in the CDC standards used in PCC EHR. Contact PCC Support to have any of the races or ethnicities below added to your practice’s drop-down lists. All languages are always available in PCC EHR.
Races
Default List
- American Indian or Alaska Native
- Asian
- Black or African American
- Native Hawaiian or Other Pacific Islander
- White
- Other Race
- Prefers not to answer
Other Available Races in PCC EHR
| Abenaki | Absentee Shawnee | Acoma | Afghanistani | African |
| African American | Agdaagux | Agua Caliente | Agua Caliente Cahuilla | Ahtna |
| Ak-Chin | Akhiok | Akiachak | Akiak | Akutan |
| Alabama Coushatta | Alabama Creek | Alabama Quassarte | Alakanuk | Alamo Navajo |
| Alanvik | Alaska Indian | Alaska Native | Alaskan Athabascan | Alatna |
| Aleknagik | Aleut | Aleut Corporation | Aleutian | Aleutian Islander |
| Alexander | Algonquian | Allakaket | Allen Canyon | Alpine |
| Alsea | Alutiiq Aleut | Ambler | American Indian | Anaktuvuk |
| Anaktuvuk Pass | Andreafsky | Angoon | Aniak | Anvik |
| Apache | Arab | Arapaho | Arctic | Arctic Slope Corporation |
| Arctic Slope Inupiat | Arikara | Arizona Tewa | Armenian | Aroostook |
| Asian Indian | Assiniboine | Assiniboine Sioux | Assyrian | Atka |
| Atmautluak | Atqasuk | Atsina | Attacapa | Augustine |
| Bad River | Bahamian | Bangladeshi | Bannock | Barbadian |
| Barrio Libre | Barrow | Battle Mountain | Bay Mills Chippewa | Beaver |
| Belkofski | Bering Straits Inupiat | Bethel | Bhutanese | Big Cypress |
| Bill Moore’s Slough | Biloxi | Birch Creek | Bishop | Black |
| Blackfeet | Blackfoot Sioux | Bois Forte | Botswanan | Brevig Mission |
| Bridgeport | Brighton | Bristol Bay Aleut | Bristol Bay Yupik | Brotherton |
| Brule Sioux | Buckland | Burmese | Burns Paiute | Burt Lake Band |
| Burt Lake Chippewa | Burt Lake Ottawa | Cabazon | Caddo | Cahto |
| Cahuilla | California Tribes | Calista Yupik | Cambodian | Campo |
| Canadian and Latin American Indian | Canadian Indian | Canoncito Navajo | Cantwell | Capitan Grande |
| Carolinian | Carson | Catawba | Cayuga | Cayuse |
| Cedarville | Celilo | Central American Indian | Central Council of Tlingit and Haida Tribes | Central Pomo |
| Chalkyitsik | Chamorro | Chefornak | Chehalis | Chemakuan |
| Chemehuevi | Chenega | Cherokee | Cherokee Alabama | Cherokee Shawnee |
| Cherokees of Northeast Alabama | Cherokees of Southeast Alabama | Chevak | Cheyenne | Cheyenne River Sioux |
| Cheyenne-Arapaho | Chickahominy | Chickaloon | Chickasaw | Chignik |
| Chignik Lagoon | Chignik Lake | Chilkat | Chilkoot | Chimariko |
| Chinese | Chinik | Chinook | Chippewa | Chippewa Cree |
| Chiricahua | Chistochina | Chitimacha | Chitina | Choctaw |
| Chuathbaluk | Chugach Aleut | Chugach Corporation | Chukchansi | Chumash |
| Chuukese | Circle | Citizen Band Potawatomi | Clark’s Point | Clatsop |
| Clear Lake | Clifton Choctaw | Coast Miwok | Coast Yurok | Cochiti |
| Cocopah | Coeur D’Alene | Coharie | Colorado River | Columbia |
| Columbia River Chinook | Colville | Comanche | Cook Inlet | Coos |
| Coos, Lower Umpqua, Siuslaw | Copper Center | Copper River | Coquilles | Costanoan |
| Council | Coushatta | Cow Creek Umpqua | Cowlitz | Craig |
| Cree | Creek | Croatan | Crooked Creek | Crow |
| Crow Creek Sioux | Cupeno | Cuyapaipe | Dakota Sioux | Deering |
| Delaware | Diegueno | Digger | Dillingham | Dominica Islander |
| Dominican | Dot Lake | Douglas | Doyon | Dresslerville |
| Dry Creek | Duck Valley | Duckwater | Duwamish | Eagle |
| Eastern Cherokee | Eastern Chickahominy | Eastern Creek | Eastern Delaware | Eastern Muscogee |
| Eastern Pomo | Eastern Shawnee | Eastern Tribes | Echota Cherokee | Eek |
| Egegik | Egyptian | Eklutna | Ekuk | Ekwok |
| Elim | Elko | Ely | Emmonak | English |
| English Bay | Eskimo | Esselen | Ethiopian | Etowah Cherokee |
| European | Evansville | Eyak | Fallon | False Pass |
| Fijian | Filipino | Flandreau Santee | Florida Seminole | Fond du Lac |
| Forest County | Fort Belknap | Fort Berthold | Fort Bidwell | Fort Hall |
| Fort Independence | Fort McDermitt | Fort Mcdowell | Fort Peck | Fort Peck Assiniboine Sioux |
| Fort Sill Apache | Fort Yukon | French | French American Indian | Gabrieleno |
| Gakona | Galena | Gambell | Gay Head Wampanoag | Georgetown (Eastern Tribes) |
| Georgetown (Yupik-Eskimo) | German | Gila Bend | Gila River Pima-Maricopa | Golovin |
| Goodnews Bay | Goshute | Grand Portage | Grand Ronde | Grand Traverse Band of Ottawa/Chippewa |
| Grayling | Greenland Eskimo | Gros Ventres | Guamanian | Guamanian or Chamorro |
| Gulkana | Haida | Haitian | Haliwa | Hannahville |
| Havasupai | Healy Lake | Hidatsa | Hmong | Ho-chunk |
| Hoh | Hollywood Seminole | Holy Cross | Hoonah | Hoopa |
| Hoopa Extension | Hooper Bay | Hopi | Houma | Hualapai |
| Hughes | Huron Potawatomi | Huslia | Hydaburg | Igiugig |
| Iliamna | Illinois Miami | Inaja-Cosmit | Inalik Diomede | Indian Township |
| Indiana Miami | Indonesian | Inupiaq | Inupiat Eskimo | Iowa |
| Iowa of Kansas-Nebraska | Iowa of Oklahoma | Iowa Sac and Fox | Iqurmuit (Russian Mission) | Iranian |
| Iraqi | Irish | Iroquois | Isleta | Israeli |
| Italian | Ivanof Bay | Iwo Jiman | Jamaican | Jamestown |
| Japanese | Jemez | Jena Choctaw | Jicarilla Apache | Juaneno |
| Kaibab | Kake | Kaktovik | Kalapuya | Kalispel |
| Kalskag | Kaltag | Karluk | Karuk | Kasaan |
| Kashia | Kasigluk | Kathlamet | Kaw | Kawaiisu |
| Kawerak | Kenaitze | Keres | Kern River | Ketchikan |
| Keweenaw | Kialegee | Kiana | Kickapoo | Kikiallus |
| King Cove | King Salmon | Kiowa | Kipnuk | Kiribati |
| Kivalina | Klallam | Klamath | Klawock | Kluti Kaah |
| Knik | Kobuk | Kodiak | Kokhanok | Koliganek |
| Kongiganak | Koniag Aleut | Konkow | Kootenai | Korean |
| Kosraean | Kotlik | Kotzebue | Koyuk | Koyukuk |
| Kwethluk | Kwigillingok | Kwiguk | La Jolla | La Posta |
| Lac Courte Oreilles | Lac du Flambeau | Lac Vieux Desert Chippewa | Laguna | Lake Minchumina |
| Lake Superior | Lake Traverse Sioux | Laotian | Larsen Bay | Las Vegas |
| Lassik | Lebanese | Leech Lake | Lenni-Lenape | Levelock |
| Liberian | Lime | Lipan Apache | Little Shell Chippewa | Lone Pine |
| Long Island | Los Coyotes | Lovelock | Lower Brule Sioux | Lower Elwha |
| Lower Kalskag | Lower Muscogee | Lower Sioux | Lower Skagit | Luiseno |
| Lumbee | Lummi | Machis Lower Creek Indian | Madagascar | Maidu |
| Makah | Malaysian | Maldivian | Malheur Paiute | Maliseet |
| Mandan | Manley Hot Springs | Manokotak | Manzanita | Mariana Islander |
| Maricopa | Marshall | Marshallese | Marshantucket Pequot | Mary’s Igloo |
| Mashpee Wampanoag | Matinecock | Mattaponi | Mattole | Mauneluk Inupiat |
| Mcgrath | Mdewakanton Sioux | Mekoryuk | Melanesian | Menominee |
| Mentasta Lake | Mesa Grande | Mescalero Apache | Metlakatla | Mexican American Indian |
| Miami | Miccosukee | Michigan Ottawa | Micmac | Micronesian |
| Middle Eastern or North African | Mille Lacs | Miniconjou | Minnesota Chippewa | Minto |
| Mission Indians | Mississippi Choctaw | Missouri Sac and Fox | Miwok | Moapa |
| Modoc | Mohave | Mohawk | Mohegan | Molala |
| Mono | Montauk | Moor | Morongo | Mountain Maidu |
| Mountain Village | Mowa Band of Choctaw | Muckleshoot | Munsee | Naknek |
| Nambe | Namibian | Nana Inupiat | Nansemond | Nanticoke |
| Napakiak | Napaskiak | Napaumute | Narragansett | Natchez |
| Native Hawaiian | Nausu Waiwash | Navajo | Nebraska Ponca | Nebraska Winnebago |
| Nelson Lagoon | Nenana | Nepalese | New Hebrides | New Stuyahok |
| Newhalen | Newtok | Nez Perce | Nigerian | Nightmute |
| Nikolai | Nikolski | Ninilchik | Nipmuc | Nishinam |
| Nisqually | Noatak | Nomalaki | Nome | Nondalton |
| Nooksack | Noorvik | Northern Arapaho | Northern Cherokee | Northern Cheyenne |
| Northern Paiute | Northern Pomo | Northway | Northwest Tribes | Nuiqsut |
| Nulato | Nunapitchukv | Oglala Sioux | Okinawan | Oklahoma Apache |
| Oklahoma Cado | Oklahoma Choctaw | Oklahoma Comanche | Oklahoma Delaware | Oklahoma Kickapoo |
| Oklahoma Kiowa | Oklahoma Miami | Oklahoma Ottawa | Oklahoma Pawnee | Oklahoma Peoria |
| Oklahoma Ponca | Oklahoma Sac and Fox | Oklahoma Seminole | Old Harbor | Omaha |
| Oneida | Onondaga | Ontonagon | Oregon Athabaskan | Osage |
| Oscarville | Other Pacific Islander | Otoe-Missouria | Ottawa | Ouzinkie |
| Owens Valley | Paiute | Pakistani | Pala | Palauan |
| Palestinian | Pamunkey | Panamint | Papua New Guinean | Pascua Yaqui |
| Passamaquoddy | Paugussett | Pauloff Harbor | Pauma | Pawnee |
| Payson Apache | Pechanga | Pedro Bay | Pelican | Penobscot |
| Peoria | Pequot | Perryville | Petersburg | Picuris |
| Pilot Point | Pilot Station | Pima | Pine Ridge Sioux | Pipestone Sioux |
| Piro | Piscataway | Pit River | Pitkas Point | Platinum |
| Pleasant Point Passamaquoddy | Poarch Band | Pocomoke Acohonock | Pohnpeian | Point Hope |
| Point Lay | Pojoaque | Pokagon Potawatomi | Polish | Polynesian |
| Pomo | Ponca | Poospatuck | Port Gamble Klallam | Port Graham |
| Port Heiden | Port Lions | Port Madison | Portage Creek | Potawatomi |
| Powhatan | Prairie Band | Prairie Island Sioux | Principal Creek Indian Nation | Prior Lake Sioux |
| Pueblo | Puget Sound Salish | Puyallup | Pyramid Lake | Qagan Toyagungin |
| Qawalangin | Quapaw | Quechan | Quileute | Quinault |
| Quinhagak | Ramah Navajo | Rampart | Rampough Mountain | Rappahannock |
| Red Cliff Chippewa | Red Devil | Red Lake Chippewa | Red Wood | Reno-Sparks |
| Rocky Boy’s Chippewa Cree | Rosebud Sioux | Round Valley | Ruby | Ruby Valley |
| Sac and Fox | Saginaw Chippewa | Saipanese | Salamatof | Salinan |
| Salish | Salish and Kootenai | Salt River Pima-Maricopa | Samish | Samoan |
| San Carlos Apache | San Felipe | San Ildefonso | San Juan | San Juan De |
| San Juan Pueblo | San Juan Southern Paiute | San Manual | San Pasqual | San Xavier |
| Sand Hill | Sand Point | Sandia | Sans Arc Sioux | Santa Ana |
| Santa Clara | Santa Rosa | Santa Rosa Cahuilla | Santa Ynez | Santa Ysabel |
| Santee Sioux | Santo Domingo | Sauk-Suiattle | Sault Ste. Marie Chippewa | Savoonga |
| Saxman | Scammon Bay | Schaghticoke | Scott Valley | Scottish |
| Scotts Valley | Selawik | Seldovia | Sells | Seminole |
| Seneca | Seneca Nation | Seneca-Cayuga | Serrano | Setauket |
| Shageluk | Shaktoolik | Shasta | Shawnee | Sheldon’s Point |
| Shinnecock | Shishmaref | Shoalwater Bay | Shoshone | Shoshone Paiute |
| Shungnak | Siberian Eskimo | Siberian Yupik | Siletz | Singaporean |
| Sioux | Sisseton Sioux | Sisseton-Wahpeton | Sitka | Siuslaw |
| Skokomish | Skull Valley | Skykomish | Slana | Sleetmute |
| Snohomish | Snoqualmie | Soboba | Sokoagon Chippewa | Solomon |
| Solomon Islander | South American Indian | South Fork Shoshone | South Naknek | Southeast Alaska |
| Southeastern Indians | Southern Arapaho | Southern Cheyenne | Southern Paiute | Spanish American Indian |
| Spirit Lake Sioux | Spokane | Squaxin Island | Sri Lankan | St. Croix Chippewa |
| St. George | St. Mary’s | St. Michael | St. Paul | Standing Rock Sioux |
| Star Clan of Muscogee Creeks | Stebbins | Steilacoom | Stevens | Stewart |
| Stillaguamish | Stockbridge | Stony River | Stonyford | Sugpiaq |
| Sulphur Bank | Summit Lake | Suqpigaq | Suquamish | Susanville |
| Susquehanock | Swinomish | Sycuan | Syrian | Table Bluff |
| Tachi | Tahitian | Taiwanese | Takelma | Takotna |
| Talakamish | Tanacross | Tanaina | Tanana | Tanana Chiefs |
| Taos | Tatitlek | Tazlina | Te-Moak Western Shoshone | Telida |
| Teller | Temecula | Tenakee Springs | Tenino | Tesuque |
| Tetlin | Teton Sioux | Tewa | Texas Kickapoo | Thai |
| Thlopthlocco | Tigua | Tillamook | Timbi-Sha Shoshone | Tlingit |
| Tlingit-Haida | Tobagoan | Togiak | Tohono O’Odham | Tok |
| Tokelauan | Toksook | Tolowa | Tonawanda Seneca | Tongan |
| Tonkawa | Torres-Martinez | Trinidadian | Trinity | Tsimshian |
| Tuckabachee | Tulalip | Tule River | Tulukskak | Tunica Biloxi |
| Tuntutuliak | Tununak | Turtle Mountain | Tuscarora | Tuscola |
| Twenty-Nine Palms | Twin Hills | Two Kettle Sioux | Tygh | Tyonek |
| Ugashik | Uintah Ute | Umatilla | Umkumiate | Umpqua |
| Unalakleet | Unalaska | Unangan Aleut | Unga | United Keetowah Band of Cherokee |
| Upper Chinook | Upper Sioux | Upper Skagit | Ute | Ute Mountain Ute |
| Utu Utu Gwaitu Paiute | Venetie | Vietnamese | Waccamaw-Siousan | Wahpekute Sioux |
| Wahpeton Sioux | Wailaki | Wainwright | Wakiakum Chinook | Wales |
| Walker River | Walla-Walla | Wampanoag | Wappo | Warm Springs |
| Wascopum | Washakie | Washoe | Wazhaza Sioux | Wenatchee |
| West Indian | Western Cherokee | Western Chickahominy | Whilkut | White Earth |
| White Mountain | White Mountain Apache | White Mountain Inupiat | Wichita | Wicomico |
| Willapa Chinook | Wind River | Wind River Arapaho | Wind River Shoshone | Winnebago |
| Winnemucca | Wintun | Wisconsin Potawatomi | Wiseman | Wishram |
| Wiyot | Wrangell | Wyandotte | Yahooskin | Yakama |
| Yakama Cowlitz | Yakutat | Yana | Yankton Sioux | Yanktonai Sioux |
| Yapese | Yaqui | Yavapai | Yavapai Apache | Yerington Paiute |
| Yokuts | Yomba | Yuchi | Yuki | Yuman |
| Yupik Eskimo | Yurok | Zairean | Zia | Zuni |
Ethnicities
Default List
- Hispanic or Latino
- Not Hispanic or Latino
- Prefers not to answer
Other Available Ethnicities in PCC EHR
| Andalusian | Argentinean | Asturian | Belearic Islander | Bolivian |
| Canal Zone | Canarian | Castillian | Catalonian | Central American |
| Central American Indian | Chicano | Chilean | Colombian | Costa Rican |
| Criollo | Cuban | Dominican | Ecuadorian | Gallego |
| Guatemalan | Honduran | La Raza | Latin American | Mexican |
| Mexican American | Mexican American Indian | Mexicano | Nicaraguan | Panamanian |
| Paraguayan | Peruvian | Puerto Rican | SalvadoranL | South American |
| South American Indian | Spaniard | Spanish Basque | Uruguayan | Valencian |
| Venezuelan |
Languages
Default List
All languages defined in the CDC OMB list are always available in PCC EHR.
Languages in PCC EHR
| Abkhazian | Achinese | Acoli | Adangme | Adyghe; Adygei |
| Afar | Afrihili | Afrikaans | Afro-Asiatic (Other) | Ainu |
| Akan | Akkadian | Albanian | Aleut | Algonquian languages |
| Altaic (Other) | American Sign Language | Amharic | Angika | Apache languages |
| Arabic | Aragonese | Arapaho | Arawak | Armenian |
| Aromanian; Arumanian; Macedo-Romanian | Artificial (Other) | Assamese | Asturian; Bable; Leonese; Asturleonese | Athapascan languages |
| Australian languages | Austronesian (Other) | Avaric | Avestan | Awadhi |
| Aymara | Azerbaijani | Balinese | Baltic (Other) | Baluchi |
| Bambara | Bamileke languages | Banda languages | Bantu (Other) | Basa |
| Bashkir | Basque | Batak languages | Beja; Bedawiyet | Belarusian |
| Bemba | Bengali | Berber (Other) | Bhojpuri | Bihari |
| Bikol | Bini; Edo | Bislama | Blin; Bilin | Blissymbols; Blissymbolics; Bliss |
| Bokmål, Norwegian; Norwegian Bokmål | Bosnian | Braj | Breton | Buginese |
| Bulgarian | Buriat | Burmese | Caddo | Catalan; Valencian |
| Caucasian (Other) | Cebuano | Celtic (Other) | Central American Indian (Other) | Central Khmer |
| Chagatai | Chamic languages | Chamorro | Chechen | Cherokee |
| Cheyenne | Chibcha | Chichewa; Chewa; Nyanja | Chinese | Chinook jargon |
| Chipewyan; Dene Suline | Choctaw | Church Slavic; Old Slavonic; Church Slavonic; Old Bulgarian; Old Church Slavonic | Chuukese | Chuvash |
| Classical Newari; Old Newari; Classical Nepal Bhasa | Classical Syriac | Coptic | Cornish | Corsican |
| Cree | Creek | Creoles and pidgins (Other) | Creoles and pidgins, English based (Other) | Creoles and pidgins, French-based (Other) |
| Creoles and pidgins, Portuguese-based (Other) | Crimean Tatar; Crimean Turkish | Croatian | Cushitic (Other) | Czech |
| Dakota | Danish | Dargwa | Delaware | Dinka |
| Divehi; Dhivehi; Maldivian | Dogri | Dogrib | Dravidian (Other) | Duala |
| Dutch, Middle (ca.1050-1350) | Dutch; Flemish | Dyula | Dzongkha | Eastern Frisian |
| Efik | Egyptian (Ancient) | Ekajuk | Elamite | English |
| English, Middle (1100-1500) | English, Old (ca.450-1100) | Erzya | Esperanto | Estonian |
| Ewe | Ewondo | Fang | Fanti | Faroese |
| Fijian | Filipino; Pilipino | Finnish | Finno-Ugrian (Other) | Fon |
| French | French, Middle (ca.1400-1600) | French, Old (842-ca.1400) | Friulian | Fulah |
| Ga | Gaelic; Scottish Gaelic | Galibi Carib | Galician | Ganda |
| Gayo | Gbaya | Geez | Georgian | German |
| German, Middle High (ca.1050-1500) | German, Old High (ca.750-1050) | Germanic (Other) | Gilbertese | Gondi |
| Gorontalo | Gothic | Grebo | Greek, Ancient (to 1453) | Greek, Modern (1453-) |
| Guarani | Gujarati | Gwich’in | Haida | Haitian; Haitian Creole |
| Hausa | Hawaiian | Hebrew | Herero | Hiligaynon |
| Himachali | Hindi | Hiri Motu | Hittite | Hmong |
| Hungarian | Hupa | Iban | Icelandic | Ido |
| Igbo | Ijo languages | Iloko | Inari Sami | Indic (Other) |
| Indo-European (Other) | Indonesian | Ingush | Interlingua (International Auxiliary Language Association) | Interlingue; Occidental |
| Inuktitut | Inupiaq | Iranian (Other) | Irish | Irish, Middle (900-1200) |
| Irish, Old (to 900) | Iroquoian languages | Italian | Japanese | Javanese |
| Judeo-Arabic | Judeo-Persian | Kabardian | Kabyle | Kachin; Jingpho |
| Kalaallisut; Greenlandic | Kalmyk; Oirat | Kamba | Kannada | Kanuri |
| Kara-Kalpak | Karachay-Balkar | Karelian | Karen languages | Kashmiri |
| Kashubian | Kawi | Kazakh | Khasi | Khoisan (Other) |
| Khotanese | Kikuyu; Gikuyu | Kimbundu | Kinyarwanda | Kirghiz; Kyrgyz |
| Klingon; tlhIngan-Hol | Komi | Kongo | Konkani | Korean |
| Kosraean | Kpelle | Kru languages | Kuanyama; Kwanyama | Kumyk |
| Kurdish | Kurukh | Kutenai | Ladino | Lahnda |
| Lamba | Land Dayak languages | Lao | Latin | Latvian |
| Lezghian | Limburgan; Limburger; Limburgish | Lingala | Lithuanian | Lojban |
| Low German; Low Saxon; German, Low; Saxon, Low | Lower Sorbian | Lozi | Luba-Katanga | Luba-Lulua |
| Luiseno | Lule Sami | Lunda | Luo (Kenya and Tanzania) | Lushai |
| Luxembourgish; Letzeburgesch | Macedonian | Madurese | Magahi | Maithili |
| Makasar | Malagasy | Malay | Malayalam | Maltese |
| Manchu | Mandar | Mandarin | Mandingo | Manipuri |
| Manobo languages | Manx | Maori | Mapudungun; Mapuche | Marathi |
| Mari | Marshallese | Marwari | Masai | Mayan languages |
| Mende | Mi’kmaq; Micmac | Minangkabau | Mirandese | Mohawk |
| Moksha | Moldavian; Moldovan | Mon-Khmer (Other) | Mongo | Mongolian |
| Mossi | Multiple languages | Munda languages | N’Ko | Nahuatl languages |
| Nauru | Navajo; Navaho | Ndebele, North; North Ndebele | Ndebele, South; South Ndebele | Ndonga |
| Neapolitan | Nepal Bhasa; Newari | Nepali | Nias | Niger-Kordofanian (Other) |
| Nilo-Saharan (Other) | Niuean | No linguistic content; Not applicable | Nogai | Norse, Old |
| North American Indian | Northern Frisian | Northern Sami | Norwegian | Norwegian Nynorsk; Nynorsk, Norwegian |
| Nubian languages | Nyamwezi | Nyankole | Nyoro | Nzima |
| Occitan (post 1500); Provençal | Official Aramaic (700-300 BCE); Imperial Aramaic (700-300 BCE) | Ojibwa | Oriya | Oromo |
| Osage | Ossetian; Ossetic | Otomian languages | Pahlavi | Palauan |
| Pali | Pampanga; Kapampangan | Pangasinan | Panjabi; Punjabi | Papiamento |
| Papuan (Other) | Pedi; Sepedi; Northern Sotho | Persian | Persian, Old (ca.600-400 B.C.) | Philippine (Other) |
| Phoenician | Pohnpeian | Polish | Portuguese | Prakrit languages |
| Prefers not to answer | Provençal, Old (to 1500) | Pushto; Pashto | Quechua | Rajasthani |
| Rapanui | Rarotongan; Cook Islands Maori | Romance (Other) | Romanian | Romansh |
| Romany | Rundi | Russian | Salishan languages | Samaritan Aramaic |
| Sami languages (Other) | Samoan | Sandawe | Sango | Sanskrit |
| Santali | Sardinian | Sasak | Scots | Selkup |
| Semitic (Other) | Serbian | Serbo-Croatian | Serer | Shan |
| Shona | Sichuan Yi; Nuosu | Sicilian | Sidamo | Sign Languages |
| Siksika | Sindhi | Sinhala; Sinhalese | Sino-Tibetan (Other) | Siouan languages |
| Skolt Sami | Slave (Athapascan) | Slavic (Other) | Slovak | Slovenian |
| Sogdian | Somali | Songhai languages | Soninke | Sorbian languages |
| Sotho, Southern | South American Indian (Other) | Southern Altai | Southern Sami | Spanish Creole |
| Spanish; Castilian | Sranan Tongo | Sukuma | Sumerian | Sundanese |
| Susu | Swahili | Swati | Swedish | Swiss German; Alemannic; Alsatian |
| Syriac | Tagalog | Tahitian | Tai (Other) | Tajik |
| Tamashek | Tamil | Tatar | Telugu | Tereno |
| Tetum | Thai | Tibetan | Tigre | Tigrinya |
| Timne | Tiv | Tlingit | Tok Pisin | Tokelau |
| Tonga (Nyasa) | Tonga (Tonga Islands) | Tsimshian | Tsonga | Tswana |
| Tumbuka | Tupi languages | Turkish | Turkish, Ottoman (1500-1928) | Turkmen |
| Tuvalu | Tuvinian | Twi | Udmurt | Ugaritic |
| Uighur; Uyghur | Ukrainian | Umbundu | Uncoded languages | Undetermined |
| Upper Sorbian | Urdu | Uzbek | Vai | Venda |
| Vietnamese | Volapük | Votic | Wakashan languages | Walamo |
| Walloon | Waray | Washo | Welsh | Western Frisian |
| Wolof | Xhosa | Yakut | Yao | Yapese |
| Yiddish | Yoruba | Yue | Yupik languages | Zande languages |
| Zapotec | Zaza; Dimili; Dimli; Kirdki; Kirmanjki; Zazaki | Zenaga | Zhuang; Chuang | Zulu |
| Zuni |
Post Charges
After a clinician charts an encounter, they click “Bill” to make the encounter ready for billing. Once they’ve verified procedures, diagnoses, and linking, you can “check out” the encounter by posting charges.
As you post charges for an encounter, you can review and update patient and encounter information, double-check the linking and codes that the clinician selected, work with TOS payments, and more.
Watch a Video: You can watch a quick video introduction to posting charges in PCC EHR.
Learn All Steps for the Biller Role: This article (and video) is part of the New User Training for Billers. You can use that outline to learn how to complete other billing tasks in PCC EHR.
Post Charges and Payments in PCC EHR
Read the procedure below to learn how to post charges in PCC EHR.
Click “Ready to Post” on the Schedule or Messaging Queue
Find an encounter ready to post on either the PCC EHR Schedule screen or the Messaging queue and click “Ready to Post”.
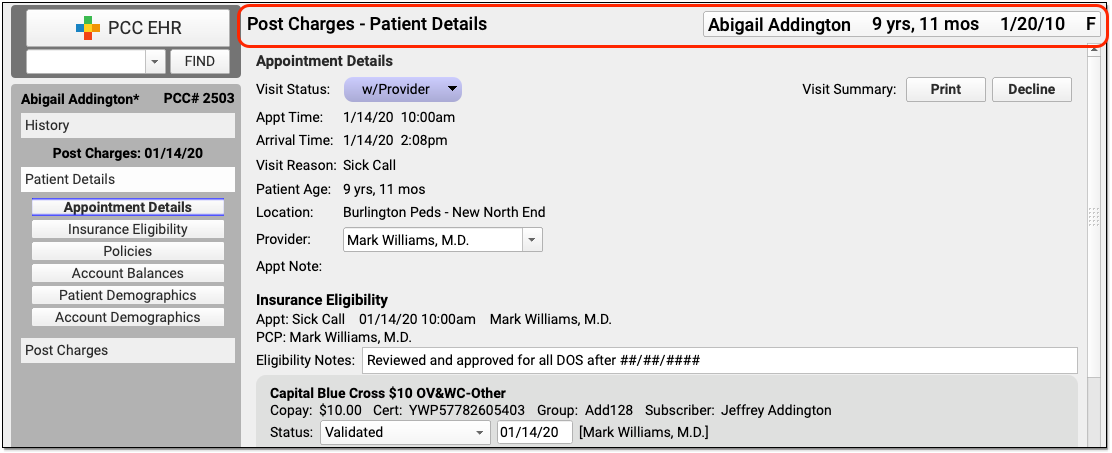
PCC EHR will open a Post Charges window.
Review Patient History, Patient Details, and the Chart Note
Review your practice’s Patient Details protocol to check eligibility, update insurance policies, or check demographic information.
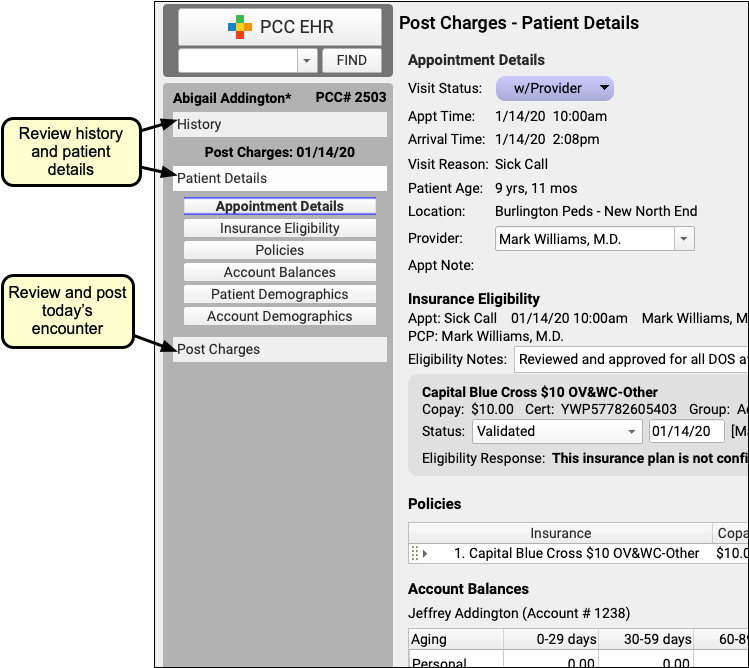
You can click “History” to visit the patient’s chart history or “Visit Note” to open a copy of the encounter’s chart note.
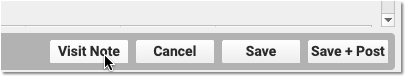
Click “Post Charges” to Open the Post Charges Protocol
When you are ready to post charges, payments, and claim information, click on the “Post Charges” navigation button.
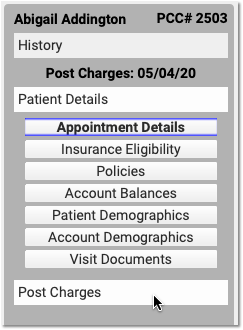
Review the Encounter’s Place of Service and Provider of Service
If you need to change the billing place of service or provider of service, you can do so in the Appointment Details component at the top of Post Charges.
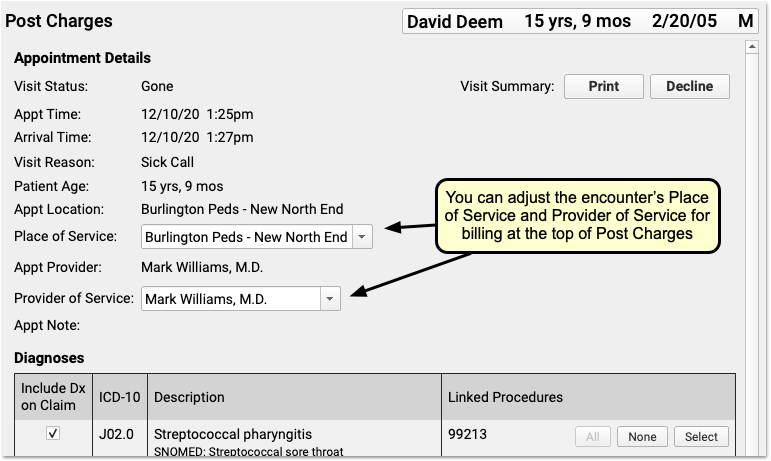
For example, if you are posting charges for a telemedicine encounter, you may need to change the billing place of service for some carriers. Also, sometimes an encounter is scheduled with a temporary or placeholder “Nurse” clinician and you must select the clinician who actually saw the patient. The changes you make here will not effect the scheduled Appointment Provider for the encounter.
Review and Update Diagnoses and Procedures
Use the Diagnoses and Procedures components to review and update codes and linking for the encounter.
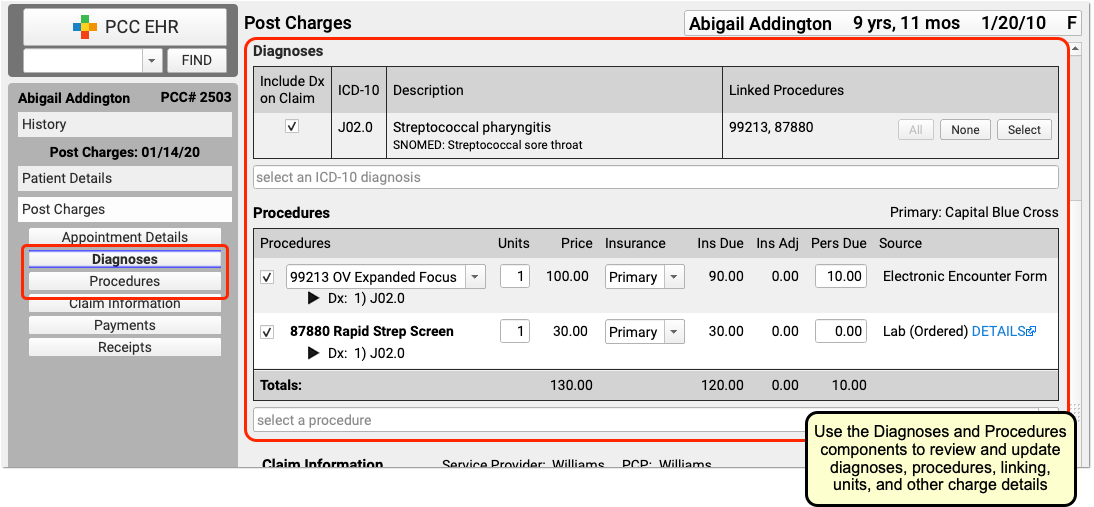
The Diagnoses and Procedures components display what the clinician selected in the Bill window (their “electronic encounter form”). If you need to add a modifier to a code, you can click on a procedure to select variations.
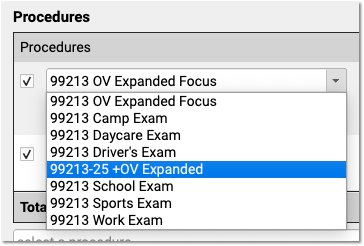
You can optionally add diagnoses or procedures that you need for billing.
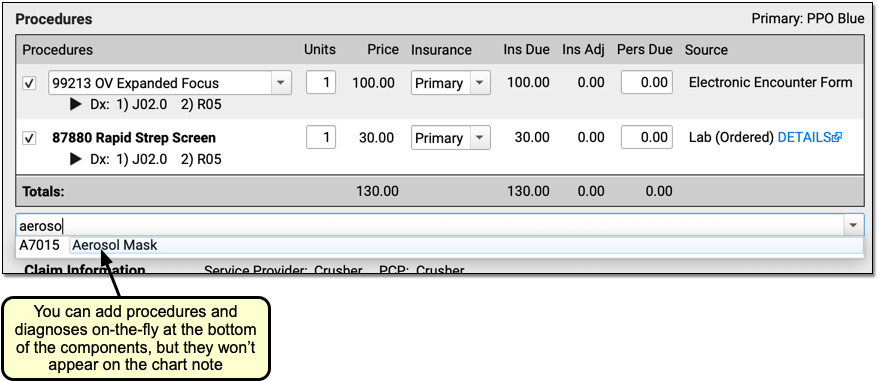
New Diagnoses and Procedures Will Not Appear on the Chart Note: While a biller can add diagnoses and procedures on the Post Charges protocol, those items will only appear in the billing record and on the claim. For most situations, the clinician should chart all procedures and diagnoses on the chart note.
Adjust Linking and Other Procedure Details
You can adjust linking in either the Diagnoses or Procedures components. You can click to link or unlink all procedures, or open a selection window.
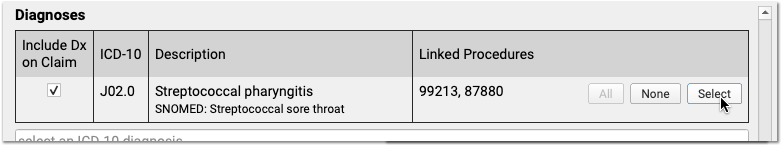
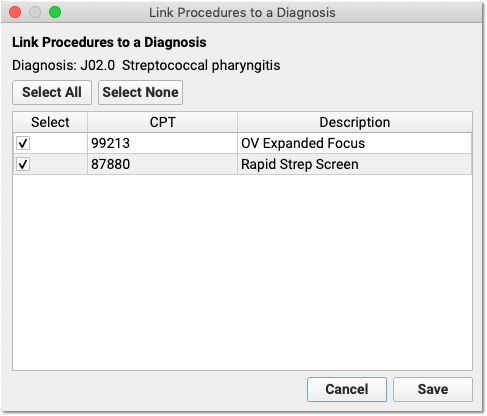
In the Procedures component, you can set which diagnosis is primary for each procedure.
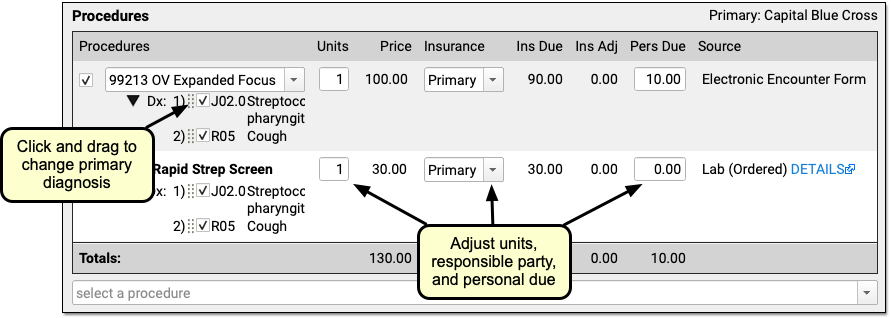
You can adjust the number of units, switch to a secondary insurance or “Self Pay”, and change the amount due personal (to adjust the copay on a charge, for example).
Complex Billing Configuration Available: As you work, you may see due amounts change based on your selection and your practice’s configuration. PCC supports configurations for price schedules, copay rules, capitated plans that adjust off charges immediately, and Medicaid plans (where nothing reverts to personal due). Your practice can customize the billing behavior of any procedure for any insurance policy. The correct amounts and adjustments will appear in the Procedures component automatically.
Select a Billing Provider or Enter Additional Claim Information
If an encounter needs to be billed under a different clinician’s supervision, is related to an accident, or has additional details that should appear on the claim, you can enter that information in the Claim Information component.
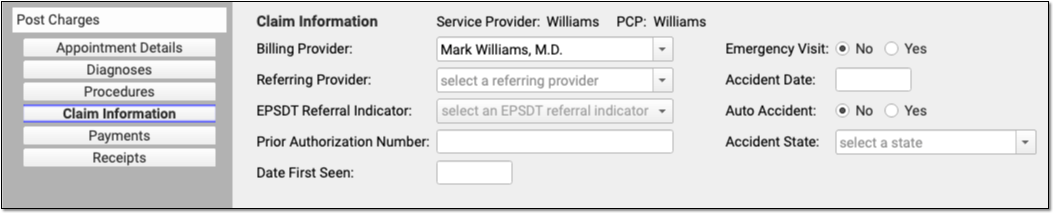
Who Are the Service and Billing Providers?: PCC EHR automatically indicates that the provider scheduled for the patient is the Service Provider. You can adjust who saw the patient in the Appointment Details component. If the encounter should have a different billing provider, you can adjust that here in the Claim Information component. See below for more details.
Review Personal Balances and Today’s Payment
What amount is due personal for this encounter? Did the family pay part of their balance today? Use the Payments component to review personal due totals and enter additional payments.
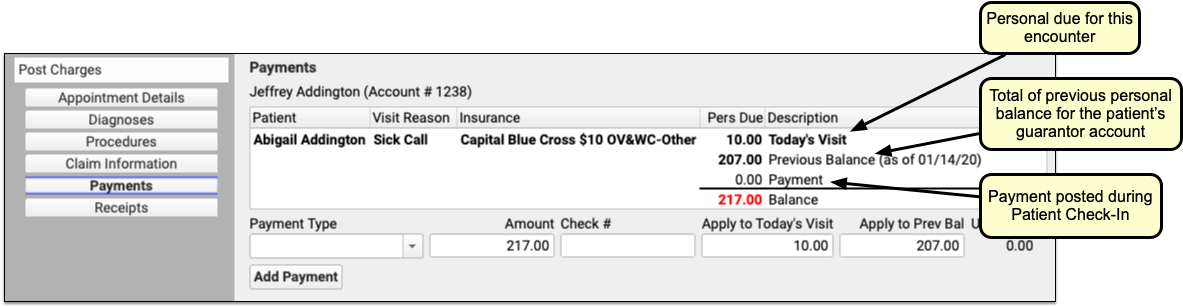
If today’s procedures result in a personal balance, you’ll see the total for the patient at the top, next to “Today’s Visit”. If the patient’s billing account has a previous balance, you’ll see that as well. If the family already paid the copay today, you’ll see that TOS payment on the screen.
Why Do I Have a Previous Balance?: As you post a charge and enter payments, you may see a previous balance. That balance could be for charges for any patient who shares the same billing account. You can review details for the personal balance on the Patient Details protocol.
Enter Additional Payments or Adjustments for the Encounter
Select a Payment Type to begin entering a payment.
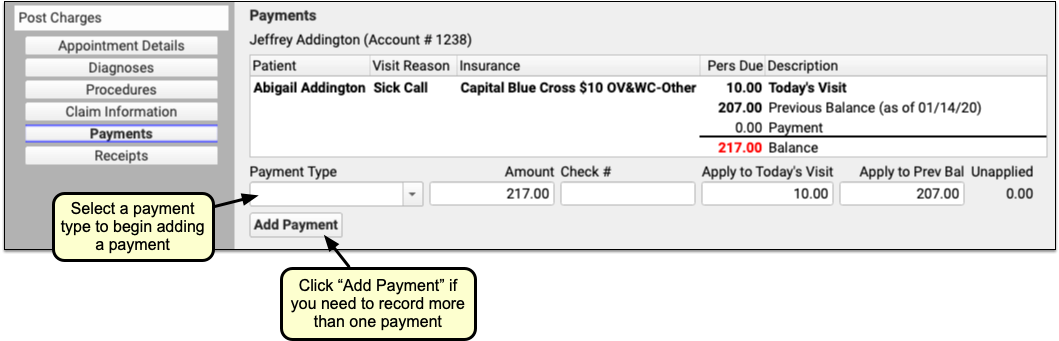
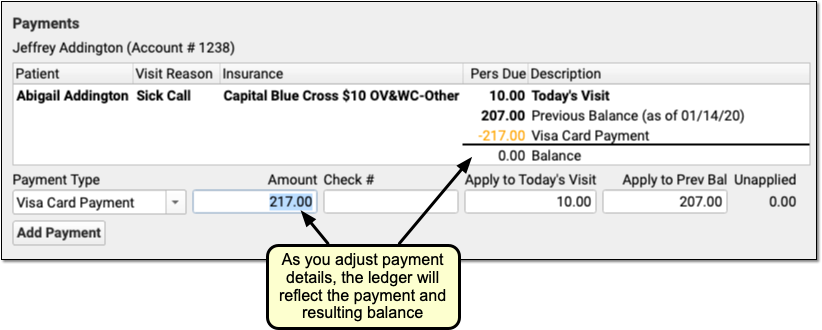
PCC EHR enters the amount due in the Amount field for you. You can adjust that amount if the parent is not paying the full amount today. You can optionally adjust how much will be applied to today’s visit or the account’s previous balance.
If you select a time of service discount as your payment type, you can optionally enter a percentage as the amount and PCC EHR will do the math for you. Once you enter a discount, PCC EHR will update the Procedures component to illustrate the amount that was discounted for each charge.
As you enter payment or discount information, the ledger in the Payments component will update to reflect the payment and the new resulting balance.
Note that payments and discounts are not saved until you click “Save + Post”.
Click “Save + Post” to Finish Posting and Queue Up a Claim
When you finish reviewing visit information, procedures, diagnoses, linking, claim information, and payments, click “Save + Post” to post the charges. (If you want a receipt right away, you can first click “Generate a Receipt”.)
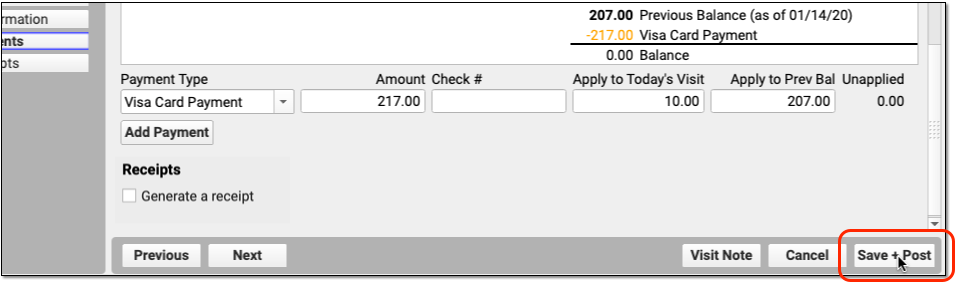

The Schedule queue will display that the encounter’s charges are now posted.
What Happens Next?: As soon as you post charges, PCC queues up a claim. Later, your practice can generate claims in the Claims tool, which will review claim information for errors and then send claims electronically.
Optional: Print a Receipt
Does the family need a receipt for today’s visit? You can click the “Generate a Receipt” checkbox before you save charges, or click the “Posted” billing status to return to Post Charges and click “Generate a Receipt”.
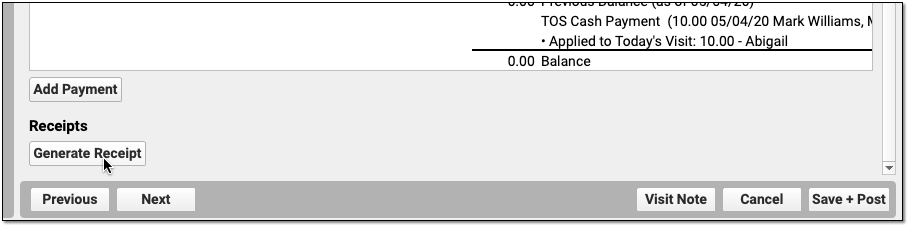
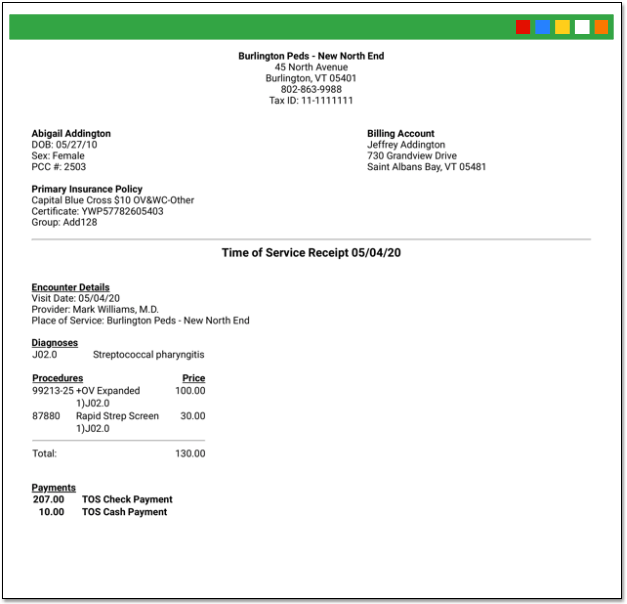
Your practice can also print receipts during Patient Check-In or in the Payments tool.
Return to an Encounter and Post More Charges and Payments Later
If a clinician returns to the chart note and adds additional diagnoses or procedures, you can spot that in the Billing Status column. (You can also use reports to find all visits with unposted charges.)
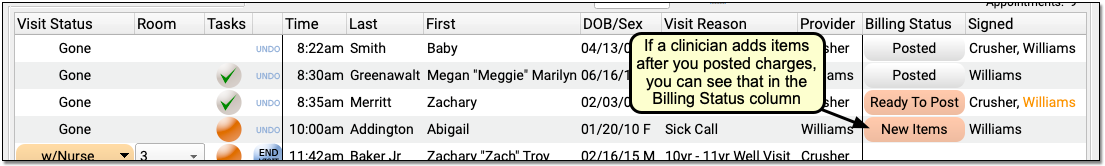
Click “New Items” to reopen the Post Charges tool and add the additional items to the claim.
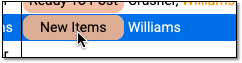
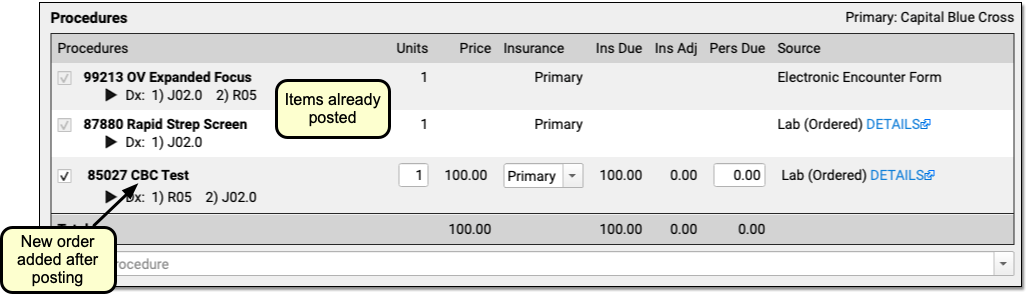
You can review and enter any new procedures or diagnoses, adjust linking, add new payments, and click “Save and Post” to adjust the queued claim.
When is an Appointment Ready to Post?
As you review the Schedule screen, how can you tell that an appointment is ready to post? Use the Billing Status and Signed columns to identify which appointments are ready to post and who has signed the appointment’s chart note.
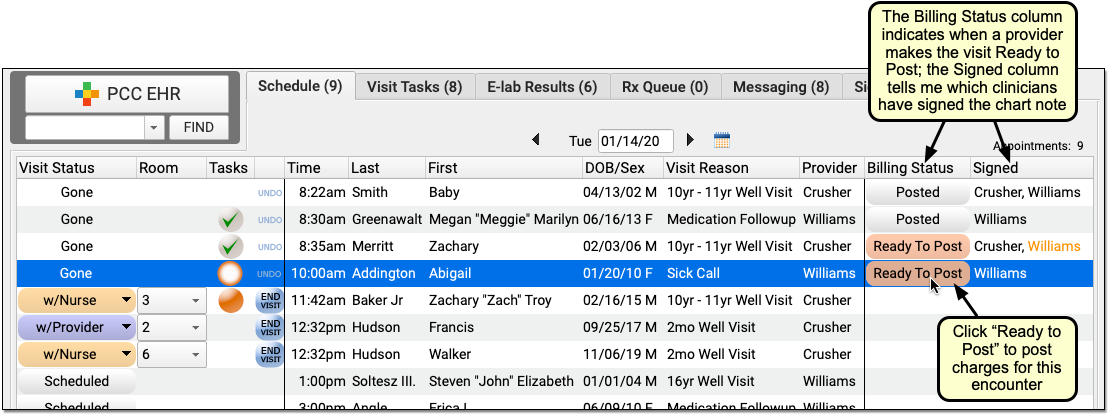
When a clinician finishes adding diagnoses and procedures to a chart note and then completes the electronic encounter form, they click “Make Ready For Billing”. That updates the status for the appointment to “Ready to Post”.
You may also want to review whether or not the clinician has signed the chart note, and check whether it has been co-signed, if required. While you can enter charges for an encounter that has not been signed, your practice’s billing policy may indicate that you wait for the chart note to be signed beforehand. An orange name indicates that a chart note requires co-signing.
For more information, see Prepare an Encounter for Billing.
Post Charges for Phone Note and Portal Message Encounters
Clinicians can create orders and make phone notes or portal messages ready for billing, just as they would an office visit. Billers can Post Charges for these encounters from the Messaging queue in PCC EHR.
To post charges for a billable phone note or portal message encounter, open the Messaging tab in PCC EHR and click Ready to Post.
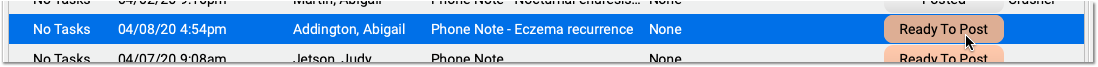
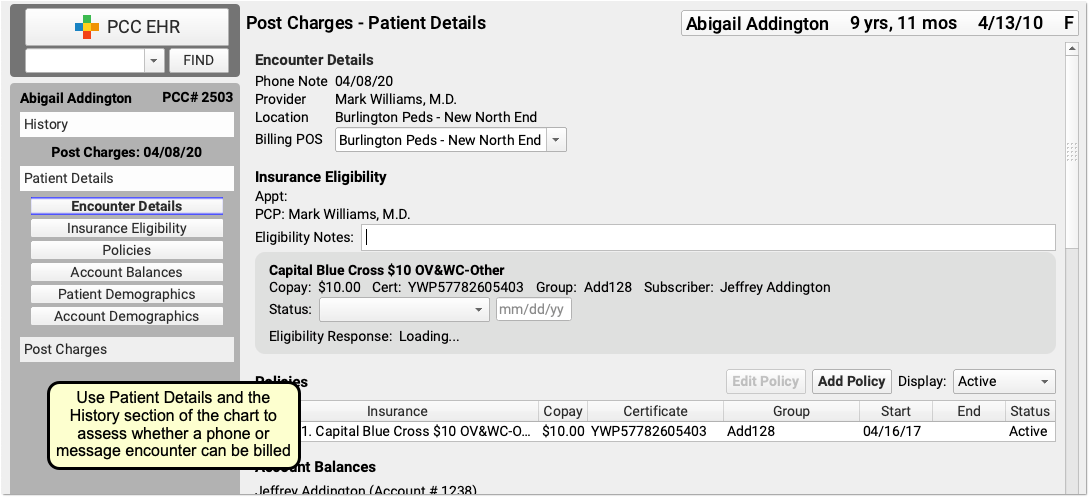
Then post charges as you would for a scheduled appointment, as described above.
To learn more, read Bill for Phone Notes and Portal Messages as Telemedicine Encounters.
Post Charges for Hospital Visits and Other Charges with No Appointment
When you need to post charges for an encounter that does not have a scheduled appointment, such as a hospital encounter or a billing-only encounter, open the patient’s chart and visit their Billing History.
To learn more, read Post Hospital Charges in PCC EHR or Post an Administrative Fee Without an Appointment in PCC EHR.
Review and Update Patient and Encounter Information as You Post Charges
As you post charges, you have many tools available to review and update patient information or research what happened during the encounter. You can post charges for some appointments in seconds. For other appointments, you may need to update insurance information, review encounter history, look back at the chart note, and more. The sections below will show you how to find the information you need to post charges and perform other billing tasks.
Review the Patient Details Ribbon: Insurance, Demographics, and More
Use your practice’s customizable Patient Details protocol to review and update eligibility, insurance policies, demographics and more.
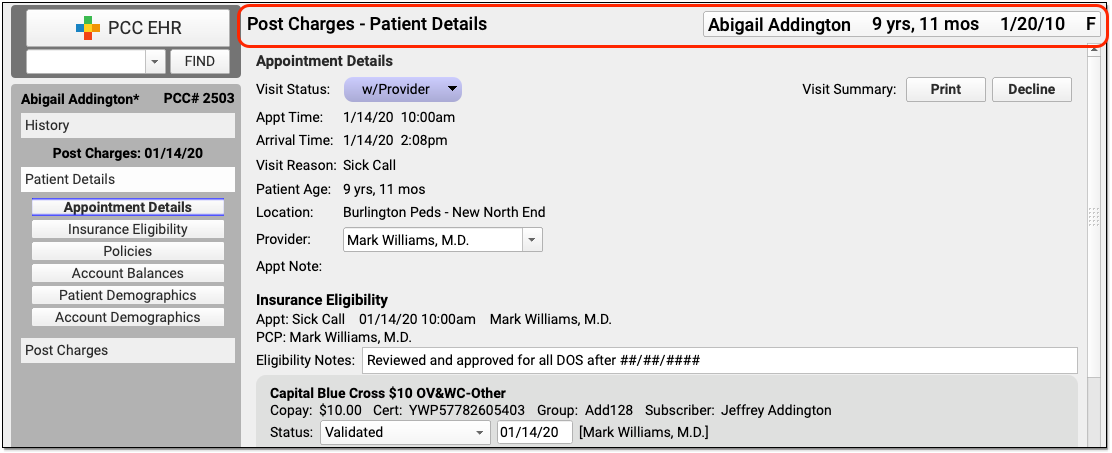
Use the navigation buttons to jump to any section of the protocol. If you’d like to add other PCC EHR components to the protocol read Configure Your Practice’s Patient Details Protocol for Post Charges, or contact PCC Support for help.
Adjust Billing Place of Service or Provider of Service for Telemedicine and Other Situations
If you need to change the billing place of service or provider of service, you can do so in the Appointment Details component at the top of Post Charges.
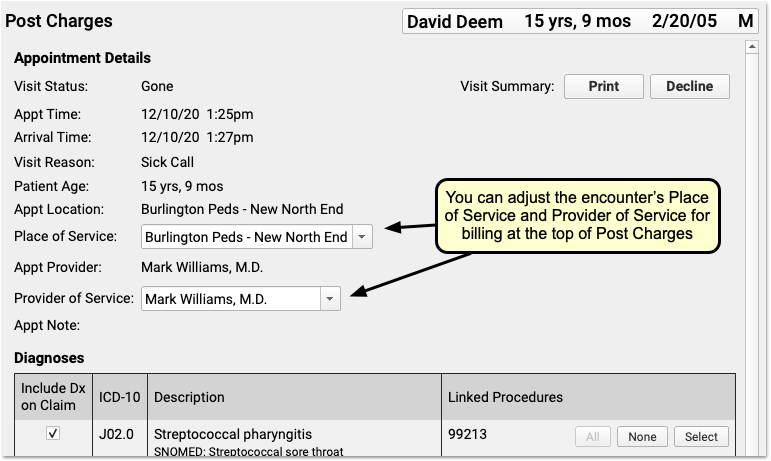
For example, if you are posting charges for a telemedicine encounter, you may need to change the billing place of service for some carriers. Also, sometimes a claim is billed out under a supervising provider of service. The changes you make here will not effect the scheduled Appointment Provider or location for the encounter.
Schedule for One Location and Provider, Change Later For Billing: When you schedule and perform an encounter, especially a telemedicine visit, it makes sense to use your office location—then doctors can see their whole schedule, and your practice can see what’s happening at a glance. When it’s time to bill, however, some carriers require a special telemedicine place of service. Additionally, you might schedule for a “Flu” provider for a flu clinic, and then change the billing provider of service.
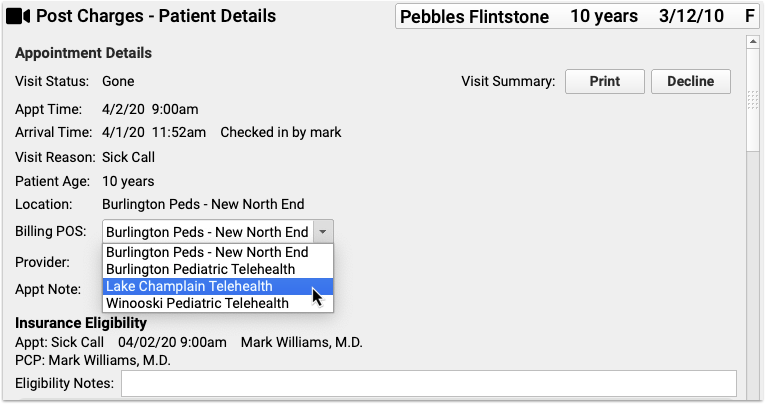
To learn more, read or watch Schedule, Chart, and Bill for a Telemedicine Encounter (Video, Article).
Research Previous Personal Balances
As you post charges, you may notice a “Previous Balance Amount” line in the Payments component ledger. The amount is the total of any past, unpaid charges for all patients who share the same Billing Account.
You can review details for the personal balance on the Patient Details protocol.
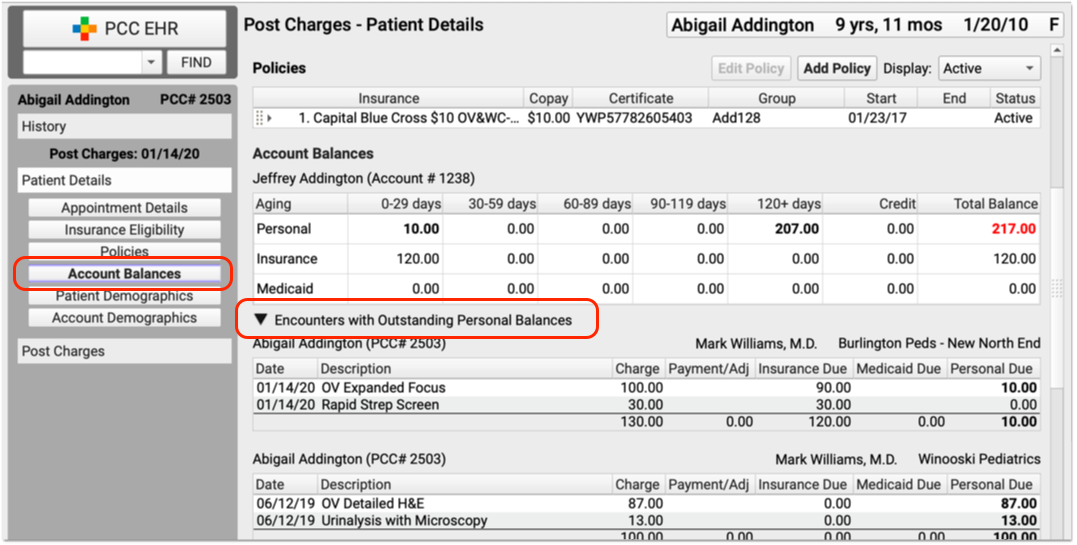
Click the disclosure triangle for “Encounters with Outstanding Personal Balances” to review details of all encounters with unpaid personal balances.
Open Documents Attached to the Encounter
Did the front desk scan the insurance card, a form, questionnaire, or some other item? Is lab information attached to an encounter? You can review any documents attached to an encounter in the Post Charges workflow.
To jump to attached documents, click the “Documents” navigation button on the Patient Details protocol. (If there are no documents attached to the encounter, this button will not appear.)
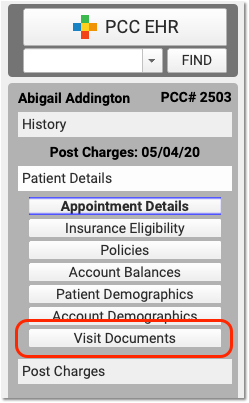
If a document is attached to the encounter, it will appear at the bottom of Patient Details. Click “View Document” on a document to open it.
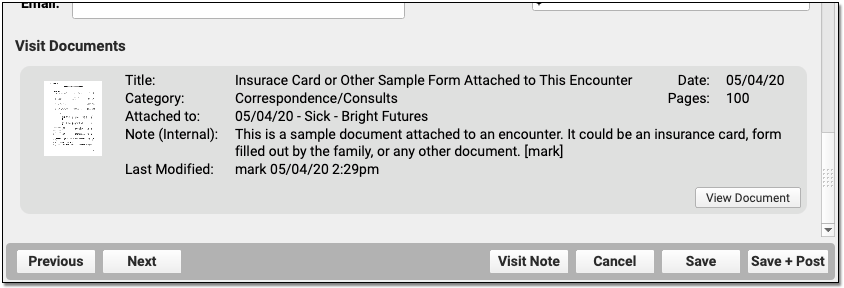
Review the Patient’s Visit History
As you work in Post Charges, click “History” to visit the patient’s chart history and review previous chart notes or other encounters.
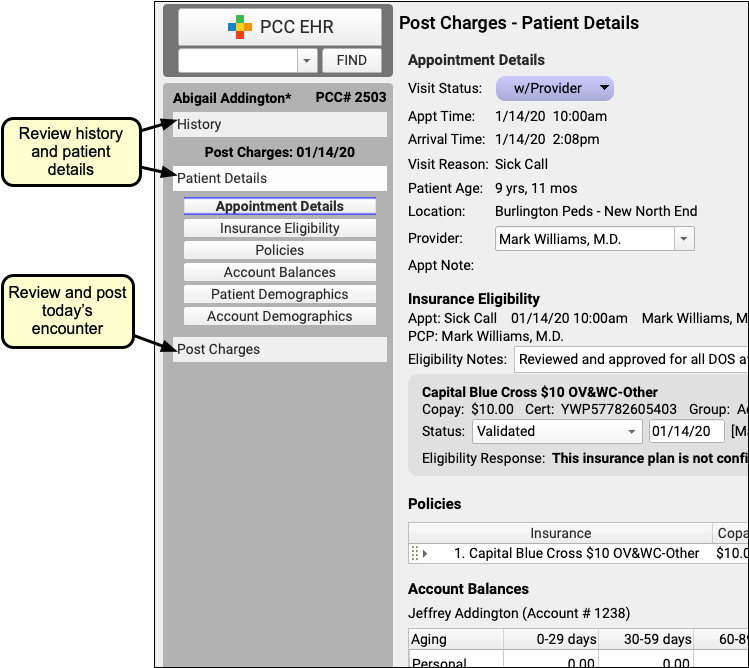
Open Today’s Visit Chart Note in a New Window
Click “Visit Note” in the lower-right corner of Post Charges to open a copy of the encounter’s chart note in a separate window.
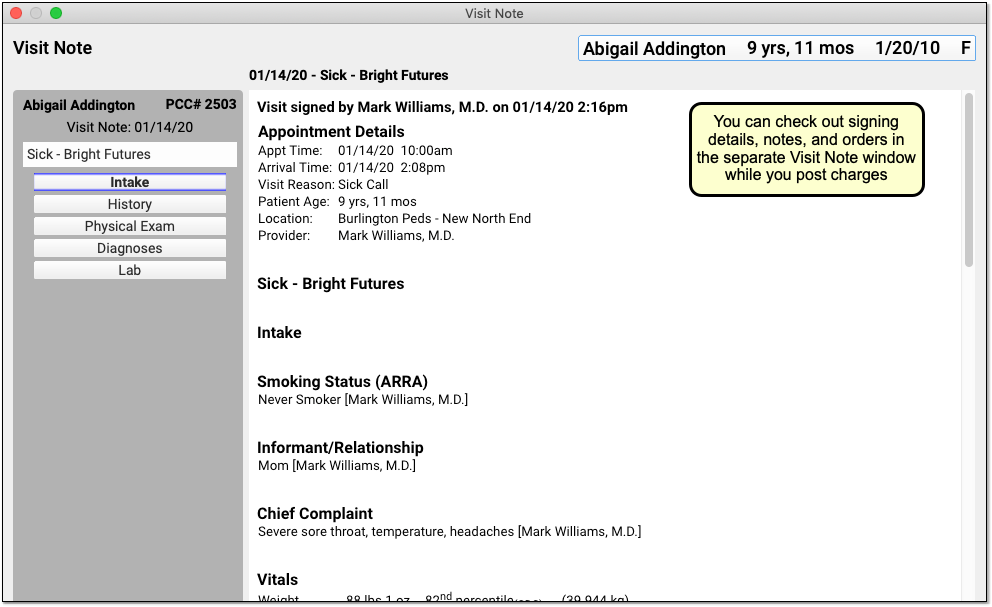
You can keep the window open, side-by-side with Post Charges, so you can review it as you update diagnoses and procedures.
Review and Update Diagnoses and Procedures As You Post Charges
The Diagnoses and Procedures components display what the clinician selected in the Bill window when they prepared the encounter for billing. As you post charges, you can adjust linking, add items, and perform other functions.
Add Diagnoses and Procedures to an Encounter
You can optionally add diagnoses or procedures that are needed for billing.
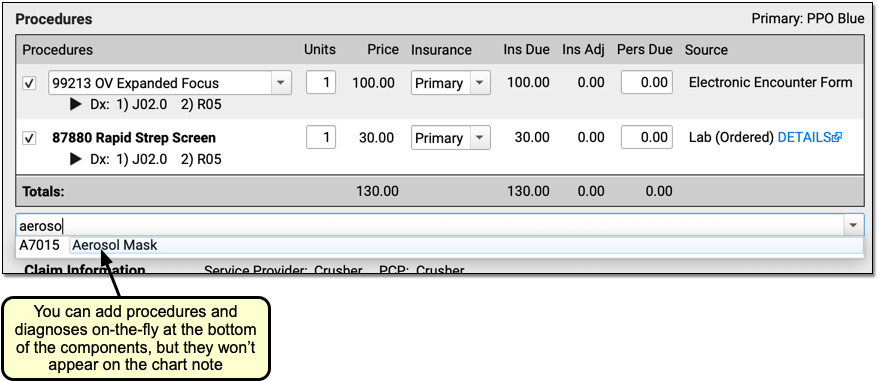
For example, a biller might identify a missed supply code or administrative code and add it when they post charges.
New Diagnoses and Procedures Will Not Appear on the Chart Note: While a biller can add diagnoses and procedures on the Post Charges protocol, those items will only appear in the billing record and (depending on your configuration) on the claim. For most situations, the clinician should chart all diagnoses and procedures on the chart note.
Add Administrative Fees to an Encounter, Form Fees, or Other Billing Procedures
As you post charges for an encounter, you can add any procedure code or billing procedure, including administrative fees.
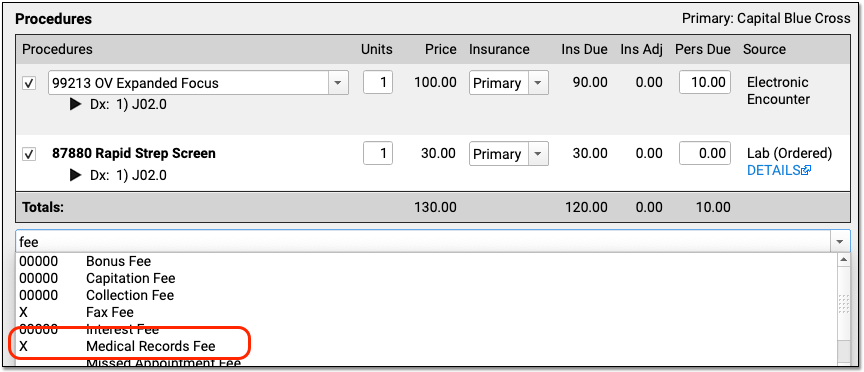
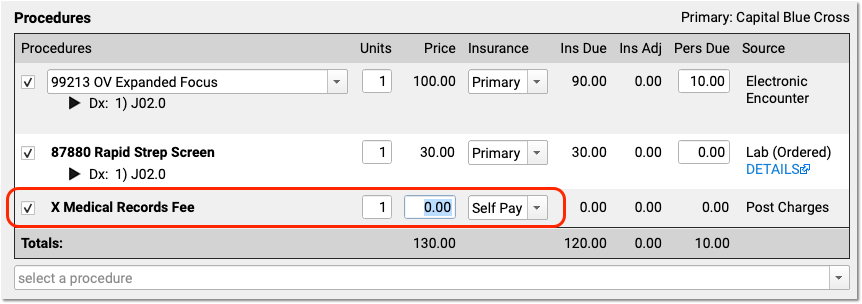
Your practice can configure procedures with unique billing behaviors. For example, the Medical Records fee above will automatically not appear on the claim. Also, your practice can configure a set price for a procedure, or have a default price of $0.00 so that the biller can enter the total fee.
Adjust Claim, Copay, Units and Insurance Billing Behavior for Procedures
In the Procedures component, you can set whether or not a procedure appears on the claim, adjust the number of units, or change the copay amount for a procedure.
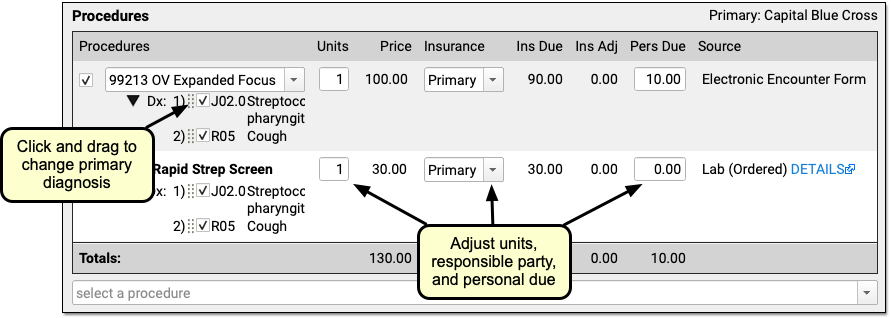
Add a Modifier to Visit Code, or Pick a Different Version of a Procedure Code
When you need to add a -25 or other modifier to a code, click on the procedure in the Procedures component.
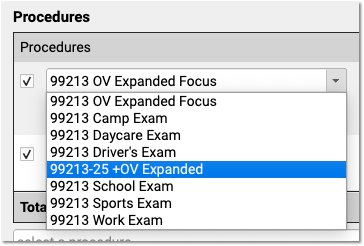
PCC EHR automatically displays all the procedures that have the same base code. If you are posting a complex visit that requires a modifier, you can pick the modified code and PCC EHR will update the prices accordingly.
In addition to adding a modifier, your practice can use this to specify a different version of the code that you track for billing purposes. For help setting up and configuring your practices procedures, codes, and prices, contact PCC Support. You can also read Edit Your Practice’s Prices and Procedure Billing Codes or watch a video tutorial.
Review the Source of Procedures and Review Procedure Order Details
How did each procedure end up in Post Charges? Use the “Source” column in the Procedures component to explain the origin of each procedure. For example, the clinician may have selected it (on the Bill window, the encounter’s “Electronic Encounter Form”), it might come from an order, or you may have added it manually in Post Charges.
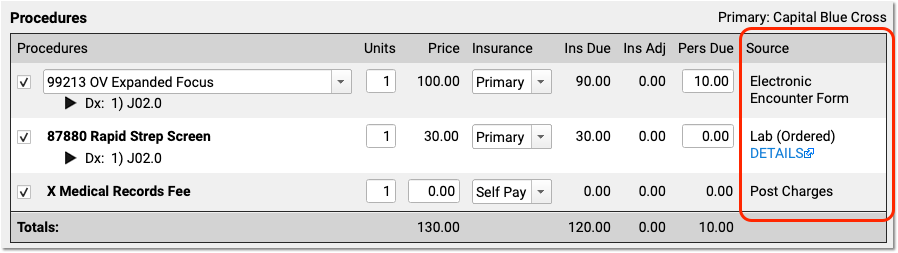
When a clinician creates an order for an immunization, screening, or other service, PCC EHR can automatically add appropriate procedure codes to the electronic encounter form. The clinician manually selects a visit code (and sometimes other codes) on the electronic encounter form. Then the clinician makes these codes “Ready For Billing”, which causes them to appear in Procedures in the Post Charges protocol. Finally, the biller can also manually add procedures before they queue up the claim.
For some orders, you can click on the “Details” link, as shown in the image above, to learn more about the order that led to the billing procedure code.
Configure Orders to Trigger Specific Procedures: Your practice can customize exactly which procedure codes should automatically be added to the encounter form for each lab, screening, or other order. See Configure PCC EHR Billing and the Electronic Encounter Form to learn more.
Post a Procedure With No Linked Diagnosis
On a claim, all procedures must be linked to one or more diagnosis. If you attempt to post a procedure that is not linked to a diagnosis, PCC EHR will stop and ask you to link before continuing.
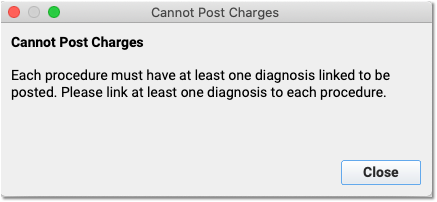
If your practice uses a procedure for an administrative fee or other non-standard purpose, you can configure that procedure with fewer than five characters (#####), and Post Charges will allow you to post the procedure without a linked diagnosis.
Change the Order of Procedures On An Insurance Claim
Some payers may require the E&M code to appear first, or have other requirements for the claim. Your practice may want to sort the CPTs so they appear in a certain order.
PCC Support can adjust the claim processing for each payer and set a priority order for procedures so they appear in the correct order on the claim. Contact PCC Support to configure your claims.
Review and Fix Invalid Codes
When you post charges, and an ICD-10 code is expired (or not yet in effect), PCC EHR will warn you and prevent posting. The diagnosis will appear in red text and include an explanation in parentheses. For example, this screenshot was taken in December of 2020:
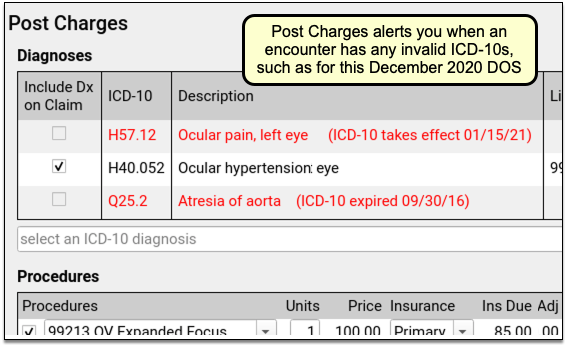
PCC EHR will not allow you to post charges with diagnoses that are invalid for the date of service. You can immediately add the correct code into the Diagnoses component, link and post the charges, and queue up a claim.
Fix Your Diagnosis Configuration: If an invalid ICD-10 appears on the Post Charges screen, you can fix the problem so it doesn’t appear again. For example, you might have an order that is configured to trigger the old diagnosis, or an expired ICD-10 might be manually mapped to a SNOMED description. You can fix these issues in the Billing Configuration tool. In Billing Configuration, you can only map ICD-10 diagnoses that are valid or will be valid in the future; expired ICD-10s are not available for mapping.
Procedure Code (CPT) Validation: Your practice can create and use non-CPT procedures and charges, such as administrative fees. PCC does not validate procedure codes when you post charges. Instead, your PCC server reviews and validates CPT billing codes when your practice processes and submits claims. As claims are processed, billing codes are evaluated against your system’s list. If a claim would include an invalid billing code, or a valid code that is invalid for the date of the encounter, it holds back the claim and adds it to the Needs Correction list.
Add a New Procedure or Update a Price
If you can’t find the correct procedure code, or you need to make a change to your practice’s price, you can update the configuration before you post charges for the encounter.
See Edit Your Practice’s Prices and Procedure Billing Codes or watch a video tutorial.
Adjust Claim Information as You Post Charges
As you post charges, use the Claim Information section if you need to change the billing provider, enter accident information, or add other details that will appear on the claim.
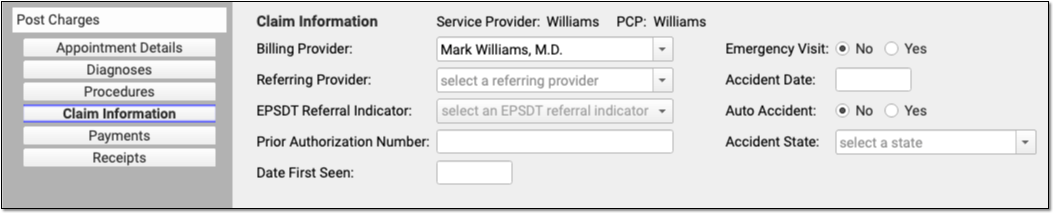
Appointment Provider, Provider of Service, Billing Provider, Rendering Provider, and Provider of Billing
PCC EHR automatically selects the scheduled Appointment Provider as the Provider of Service for an encounter when you post charges. The Provider of Service will normally appear on the claim. In the claim specification, the Provider of Service is called the “Rendering Provider”, and is also equivalent to the “Encounter Provider” term used for evaluating Clinical Quality Measures.
If an encounter was scheduled for a placeholder “Nurse” or “On Call” provider, for example, you can use the Appointment Details component to change the Provider of Service and indicate who saw the patient.
If the encounter needs to be billed under a different provider than the Provider of Service, you can change the “Billing Provider” in the Claim Information component. The Billing Provider will then appear on the claim as the Rendering Provider, overriding the Provider of Service.
Your practice can use the Providers Table (found in the Tables tool) to mark a provider as “Not Real”. The Post Charges screen will then prompt the user to select a Billing Provider.
Your practice’s information, usually the name of your business, appears on the claim as the “Provider of Billing”, along with your practice’s Type 2 NPI. If you encounter an insurance carrier that requires you to display the rendering provider in the “Provider of Billing” section of the claim, or you have other special configuration needs for making sure the right clinician appears on the claim, PCC can handle configuration changes.
Enter Accident Information
If an encounter is related to an accident, enter accident information in the Claim Information section.
As accident claims are rejected without a location, when you indicate that an encounter is related to an accident PCC EHR will automatically enter the state of your practice’s office or care center location.
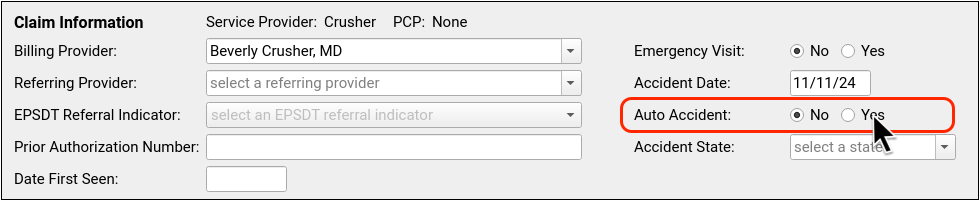
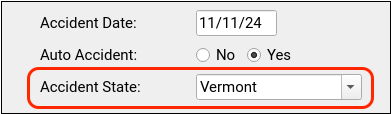
Review Payments as You Post Charges
As you post charges, you can review balances, time-of-service payments, and enter a new payment. Read below to learn more about payments, receipts, and the live ledger found in the Payments component.
Adjust How a Payment is Applied
For each payment, you can adjust what portion of the payment will apply to today’s visit or the past due balance.
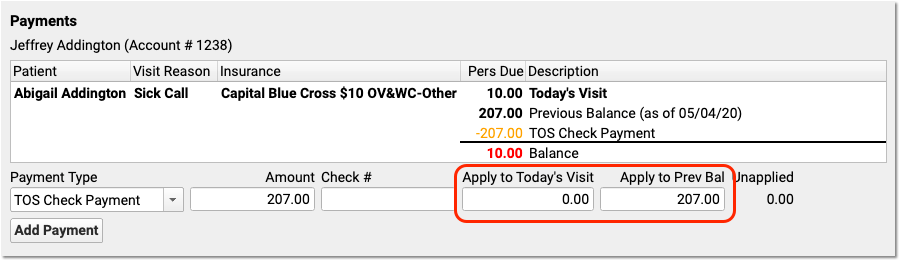
In the above example, the user designated that the $207 check should fully apply to past-due balances and not to today’s required copay.
How are Payments Applied to Multiple Past-Due Balances?: If there are many unpaid previous balances, PCC will begin by applying payments to the oldest charges first. It will link the payment to charges in turn. Later, your practice can optionally unlink and relink payments in the Payments tool.
Add Multiple Payments
When a parent pays with multiple payments, you can add each payment and then adjust which payments apply to today’s encounter and which apply to past-due balances.
After you enter details for one payment, click “Add Payment” to create additional payment lines.
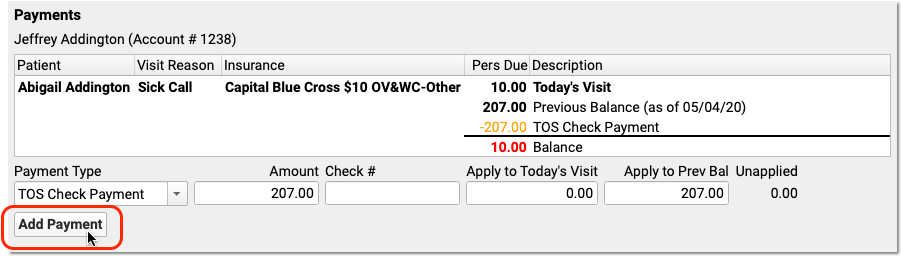
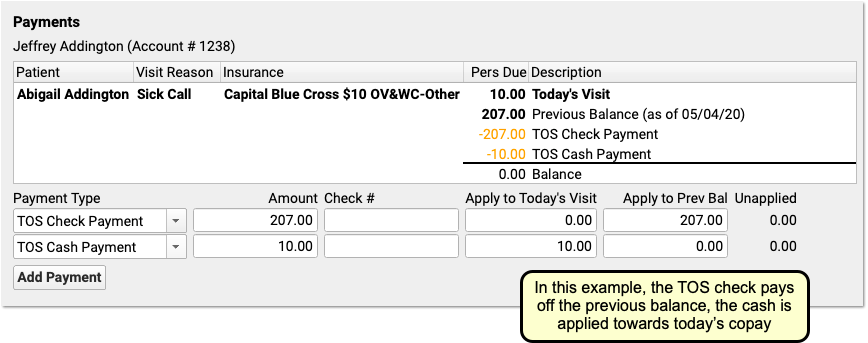
For each payment, you can select a payment type, enter an optional check number, and adjust what portion of the payment will apply to today’s visit or a past-due balance.
As you enter payments and make changes, the ledger in the Payments component will display the end result of your actions. The payments will not be posted or saved until you click “Save and Post”. All payments will appear on the receipt.
Enter Time-of-Service Discounts
As you post charges, you can enter a discount amount or discount percentage. There are two ways to enter a discount amount.
First, you can enter discounts for any procedure in the Discount column in the Procedures component.
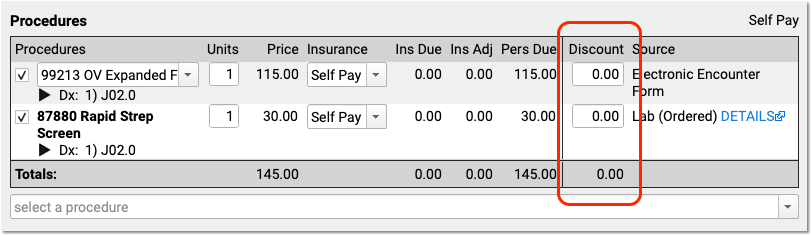
If you type a percentage, PCC EHR will automatically calculate the discount amount.
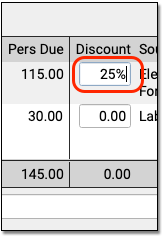
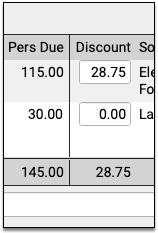
The Payments component below will automatically fill out the details of the discount for you.
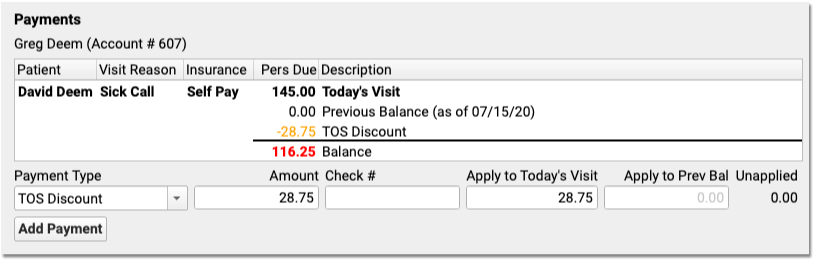
Alternatively, if you want to apply a discount towards all charges in the encounter, you can skip the Procedures component. In the Payments component, select a discount as the “Payment Type” and enter a percent or an amount.
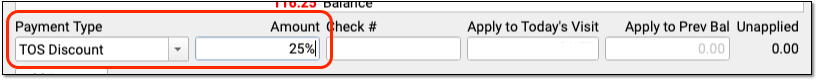
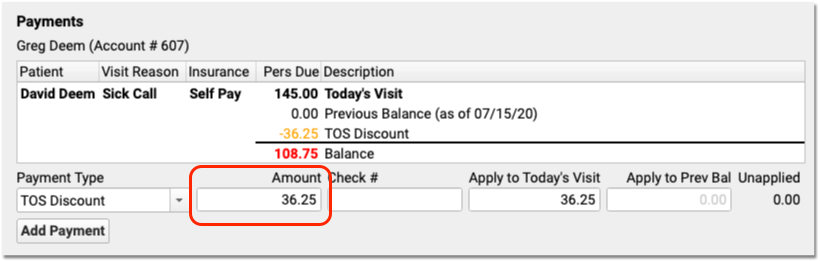
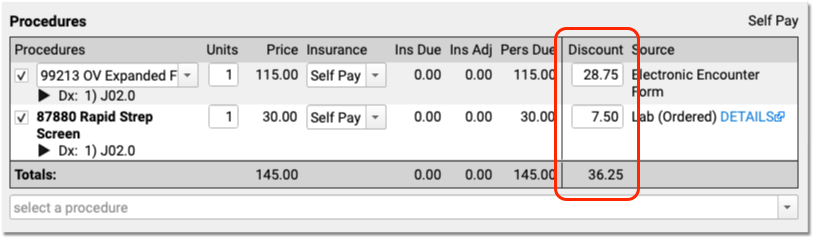
The Discounts column in the Procedures component will automatically update with the discounted amounts. If you enter an exact discount amount instead of a percentage, PCC EHR will apply the discount to the procedures in order, starting from the top.
You can adjust discount amounts in either component, make other changes to the charges, or add additional payments for the remaining balance. Click “Save + Post” to finish posting the charges, payments, and discounts.
The Billing History section of the patient’s chart will display the discount along with other time-of-service payments or adjustments.
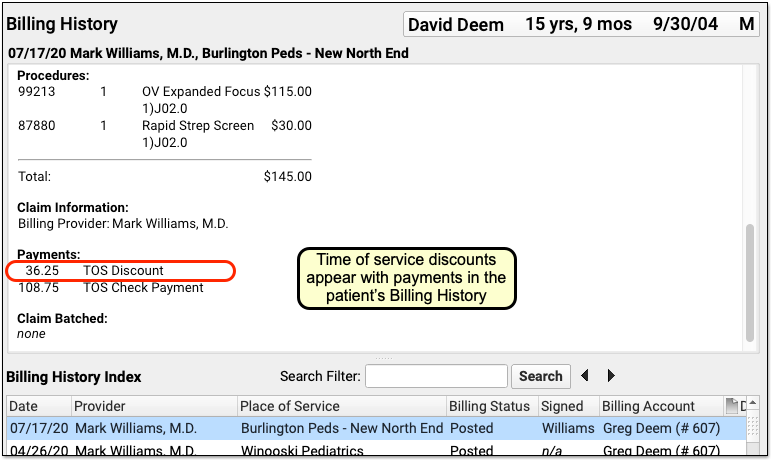
How Much Can I Adjust Off With a Time-Of-Service Discount?: Time-of-service discounts are for the amount due to the personal billing account of the patient, not for charges pending an insurance payer. You can only discount up to the total amount due personal on a charge.
Receipts Display Only Services and Payments: Discounts occur for a variety of reasons, some of which involve PHI or administrative decisions. Therefore time-of-service discounts do not appear on the printed receipt. The Post Charges receipt only displays the billed services and any payments. To create a complete account history (including discounts), use the Account History in the patient’s chart.
Configure Your Practice’s Default TOS Discount Type
When you enter a discount in the Procedures column while posting charges, PCC EHR automatically creates the Discount line in the Payments component for you.
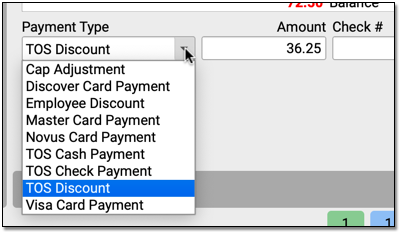
If your practice has many different types of discounts or adjustments that you apply at the time of service, you can change the discount to a different type with the drop-down menu in the Payments component.
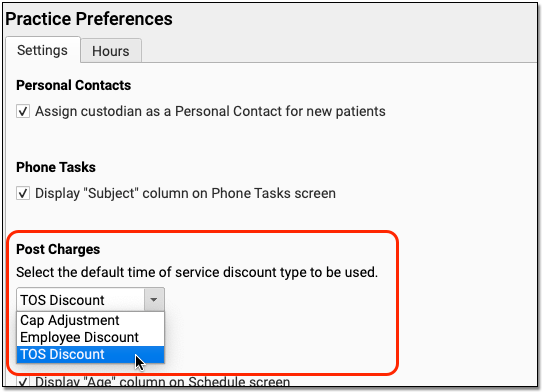
Use the Practice Preferences configuration tool to adjust your practice’s default TOS Discount. During your PCC 8.13 update, PCC copied your practice’s default TOS discount from the charge posting configuration in Practice Management. You can review and update this default in PCC EHR, and pick from any payment type in your PCC system that is marked as an “Adjustment” and is configured for charge posting.
Understand Payments Made for Siblings or Multiple Patients Who Share a Billing Account
As you post charges for a series of visits for patients with the same billing account, the Payments component will track your progress and let you know what amounts have already been posted for the account.
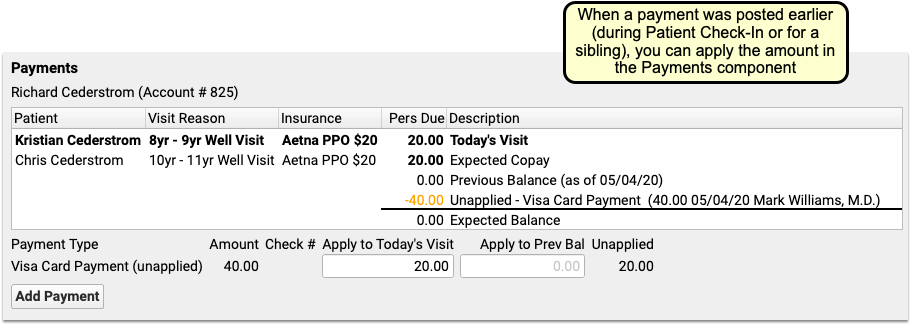
If you post the total of both copays for sibling patients during Patient Check-In, or do so when you post charges for the first sibling, the payment amount will appear in the ledger and you can adjust how much to apply to the encounter’s charges.
In example in the screenshot above, the $40 payment appeared in the Payments component, and the ledger was already showing that the family’s balance is $0.00. The user enters $20 into the “Apply to Today’s Visit” field to directly link that portion of the payment to this encounter’s charges. When they post charges for the sibling, they can apply the remaining $20.
Generate a Receipt for Today’s Payment
Your practice can generate receipts at many different times during a visit and the post charges process.
First, if your practice collects a copay or other payment during Patient Checkin, the front desk can generate a receipt for the payment right away.
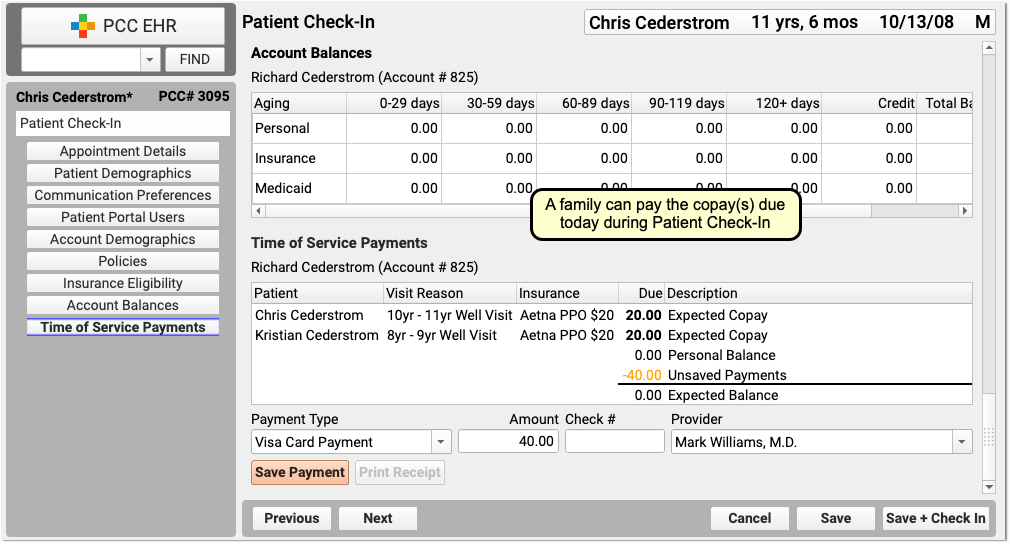
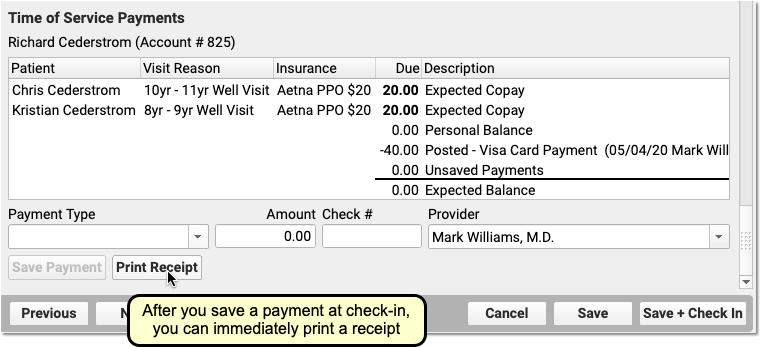
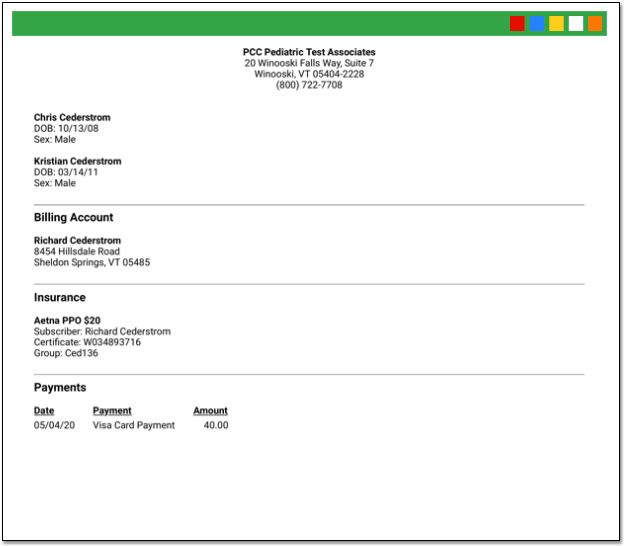
Next, if you’d like a receipt to print out as soon as you save and post charges and payments, check the “Generate a Receipt” checkbox.
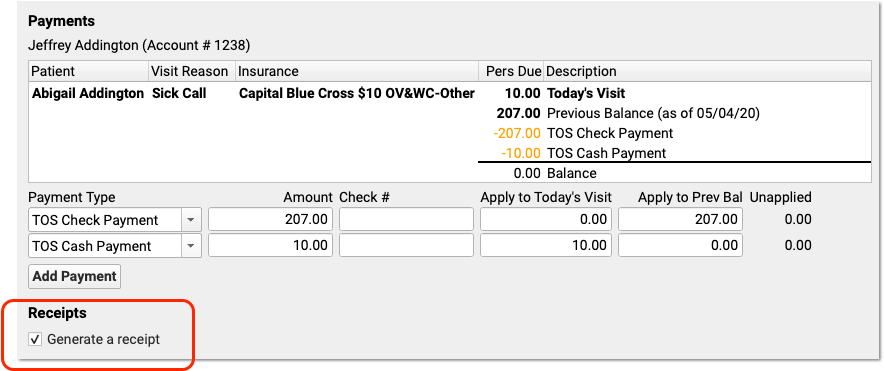
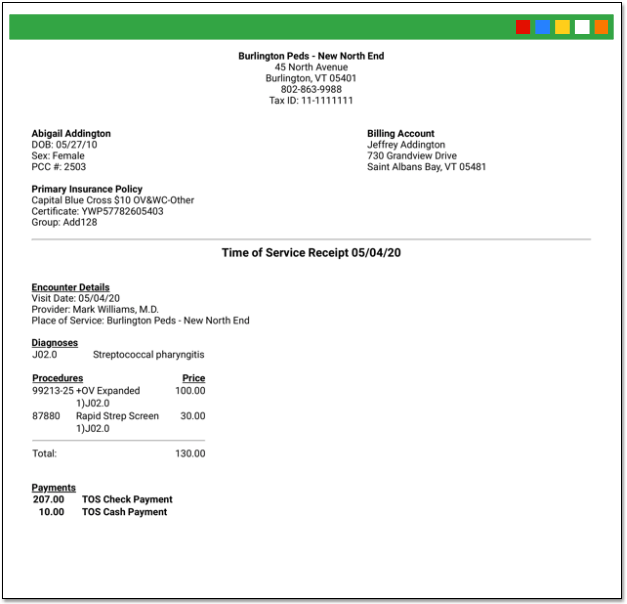
After you save and posted charges, you can return to the Post Charges protocol for an encounter at any time and click “Generate a Receipt” to print another receipt.
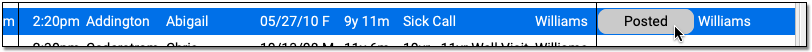
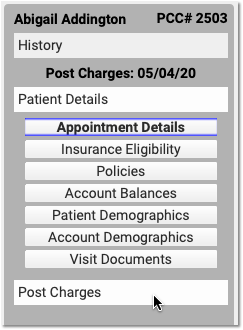
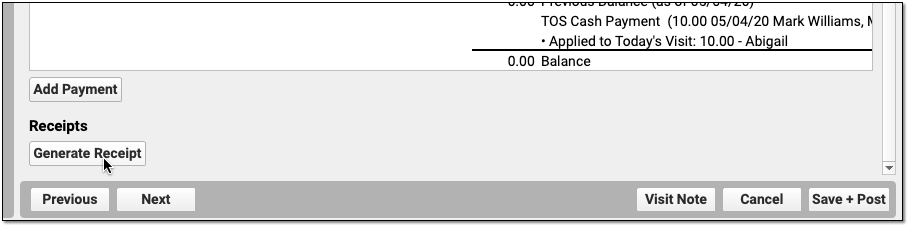
Finally, you can generate a receipt for a single payment or multiple payments in the Payments tool.
Differences Between the Patient Checkin Receipt and Post Charges Receipt: When you generate a receipt from Post Charges, you will see more visit information including procedures and diagnoses. When you generate a receipt from Patient Checkin, you will only see the amount paid.
Apply a Past Credit to Today’s Charges
When you post charges, PCC EHR will display any credits on the patient’s Billing Account in the Payments component.
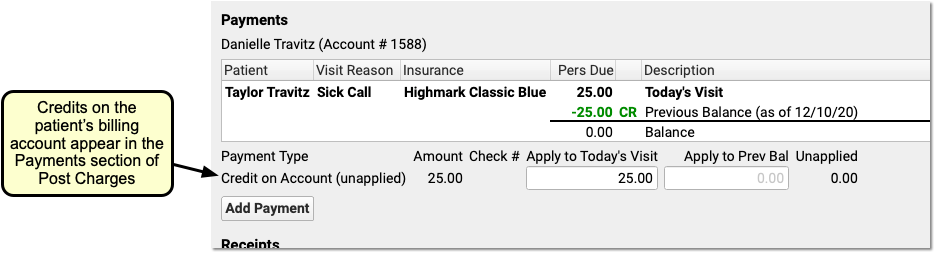
By default, the full credit will be applied towards any personal (non-insurance) charges for today. Optionally, you can adjust the amount you wish to link to today’s charges.
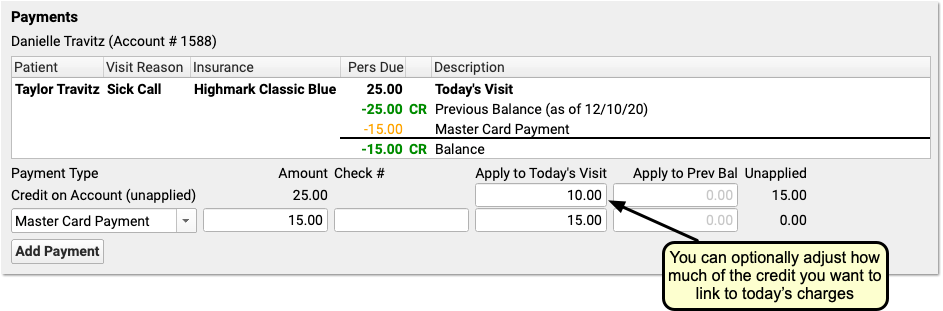
You might do this in order to apply only the amount of a copay, for example, or if only part of the credit should be applied.
When you are finished reviewing charges and payments, click Save and Post. PCC EHR will link the payment from the past directly to the charges that have a personal amount due.
Add More Diagnoses, Procedures, or Payments After You Post Charges
You can click on the “Posted” status to return to Post Charges to review what was posted and/or add additional diagnoses or procedures.

If a clinician returns to the chart note, adds diagnoses or procedures, and updates the Electronic Encounter Form, the Billing Status will display “New Items”.
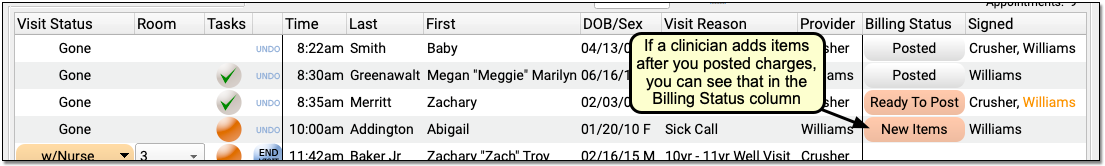
Click “New Items” to reopen the Post Charges tool and add the additional items to the claim.
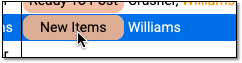
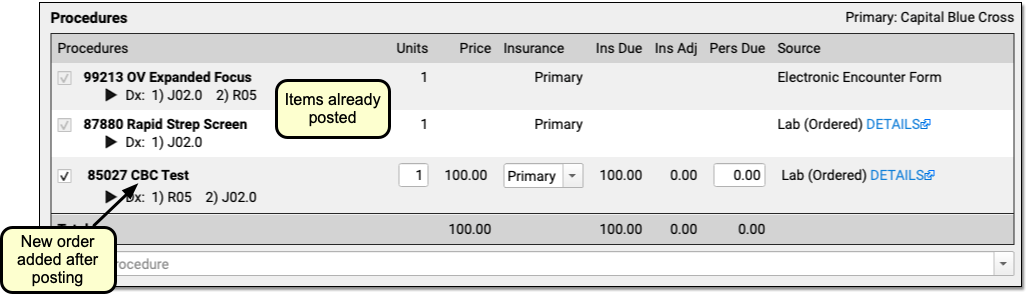
You can review and enter any new procedures or diagnoses, adjust linking, add new payments in the Payments component, and click “Save and Post” to adjust the queued claim.
Be aware that since charges and payments may have already been posted, the ledger in the Payments component will first display only totals and amounts for any new unposted charges for this encounter. Charges and payments you already posted are summarized below.
How to Find New Items: While you can easily spot the “New Items” on appointments for today, what about visits in the past? Use the Visits By Billing Status report in the PCC EHR report library to find all appointments that may include “New Items”.
Edit or Delete Charges Posted In Error
If you need to delete or update posted charges or other billing information for an encounter, visit the Billing History section of the patient’s chart. Select the encounter and click “Edit Charges” to make changes.
See Edit Encounter Charges and Other Claim Information and Resubmit a Claim to learn more.
EPCS Migration: Connect Your Authy App to the new PCC eRx Account
PCC has just transferred Exostar EPCS credentials from FDB to PCC eRx. With this migration, providers can no longer process prescriptions using the FDB-owned account inside the Authy app.
In order to associate the new PCC account in your Authy app, you will need to go into your settings within PCC eRx and reactivate your mobile credential.
You Can Still Use Your Hard Token to Prescribe: Providers can continue to use their hard token throughout this entire process.
Use a Token to Authenticate Your Account
You need to authenticate your account using either your hard token or your back-up authentication method (back-up texting option) to unlock your account and add the new PCC eRx account as a mobile credential.
Open the Token Management Tool
From the PCC eRx My Settings tab, click on the “Exostar Token Management” button to access your EPCS tokens.
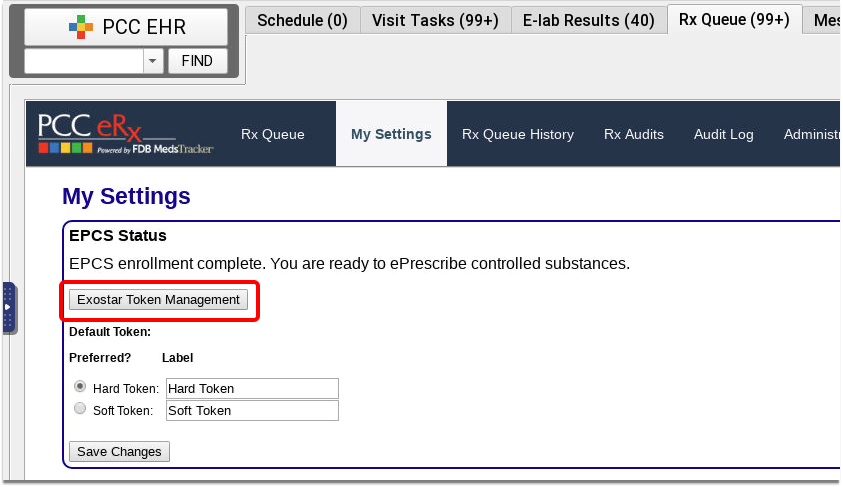
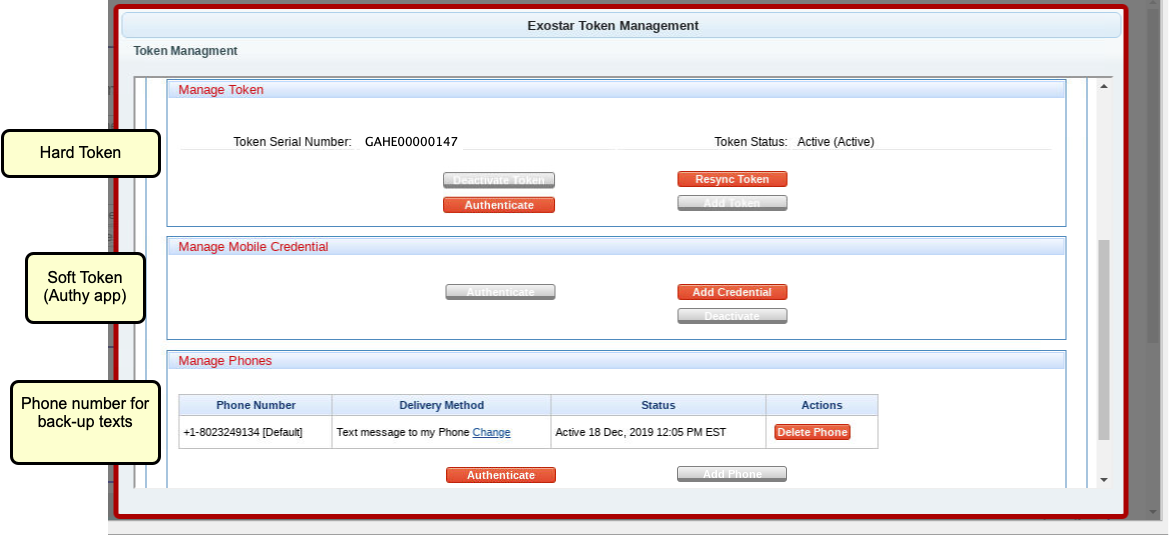
The Manage Mobile Credential box, which displays your Authy info, will be disabled, as the FDB-owned account has been deactivated.
If you registered your cell phone as a back-up authentication method, the Manage Phones box shows that cell phone number.
Authenticate Either Your Hard Token or Your Back-up Texting Option
Click the “Authenticate” button in either the Manage Token box or the Manage Phones box.
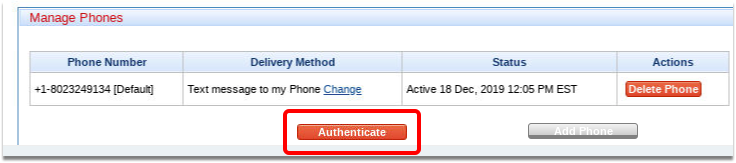
Acknowledge the Exostar Validation
You will receive a 6-digit one-time code on either the hard token or your phone.
Enter the validation code as directed on screen.
Add a New Mobile Credential
Once you authenticate your account, the “Add Credential” button in the Manage Mobile Credential box will be enabled, and you will be able to add PCC eRx to your Authy account.
Click “Add Credential”
Click the “Add Credential” button within the Manage Mobile Credential box.
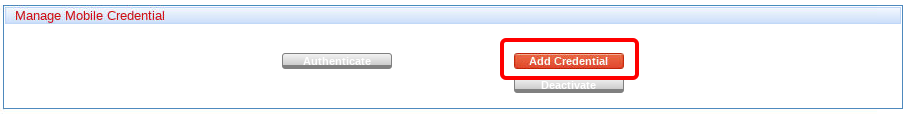
Register Your Phone
Enter the phone number and email address that you use with your Authy app, and click “Register Phone”.
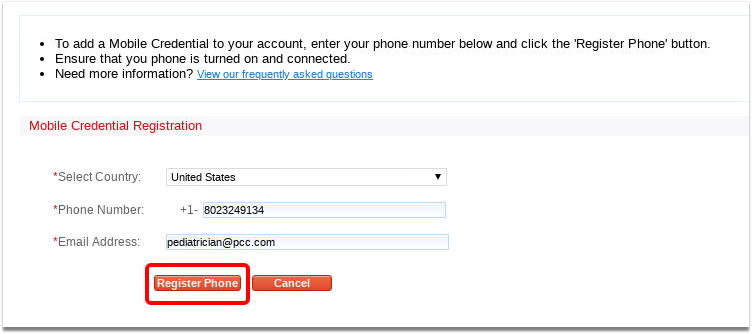
Verify the New Account
You should receive either a text or a notification from the Authy app on your phone to approve.
Verification Not Working?: If you don’t receive the notification within a few seconds, open the Authy app on your phone and click on “Settings” (gear icon in the top right), and then “Accounts” (people icon in the bottom middle) and you will see a new pending Authy account titled something like PCC eRx. Click on that to approve the new account.
Your Authy App Has Been Switched!
Back on the Exostar Token Management tool, you will see your phone number within the Manage Mobile Credential box. The Mobile Credential Status will be “Active”.
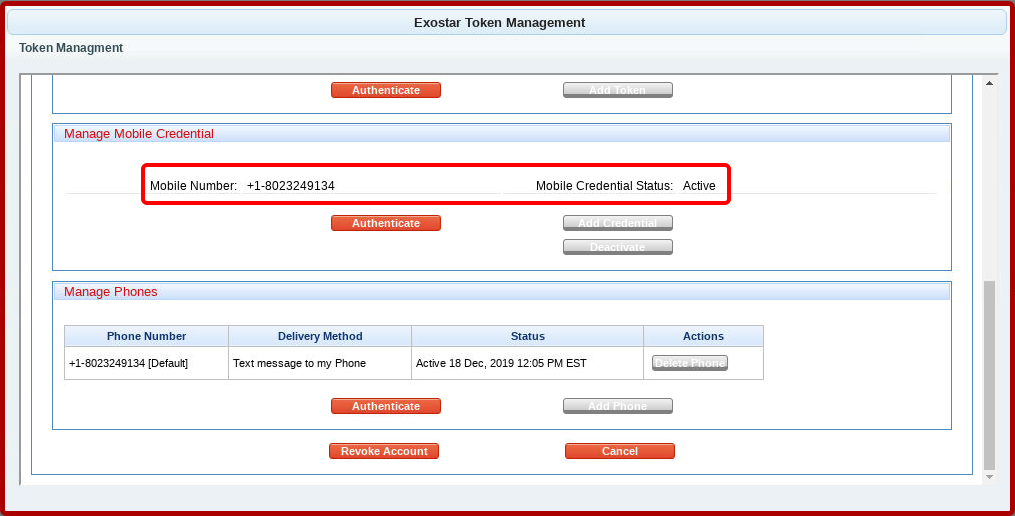
You can click “Cancel” to return to the My Settings window.
Remove the Old FDB Icon from Authy App
Finally, you’ll want to “hide” the FDB icon from Authy.
Open Your Authy Accounts
Open the Authy app on your phone and click on “Settings” (gear icon in the top right), and then “Accounts” (people icon in the bottom middle).
Hide the FDB Account
Press on the FDB account and slide to the left. You should then get a Hide option, which will take that tile off the “main” screen.
Restrict Access to Reports in the Report Library
PCC’s Report Library organizes reports by category. Each category contains a list of reports that are only visible to those who have role access to that category. Users with Manage Categories permission can limit access to specific categories by role.
Restrict Access to Specific Categories
When you want to limit access to certain report categories, click the “Manage Categories” button in the Report Library window.

Here you can manage access to each category by role. Select a category and click the “Edit” button, then select one or more roles that should have access to the reports included in the category you selected.
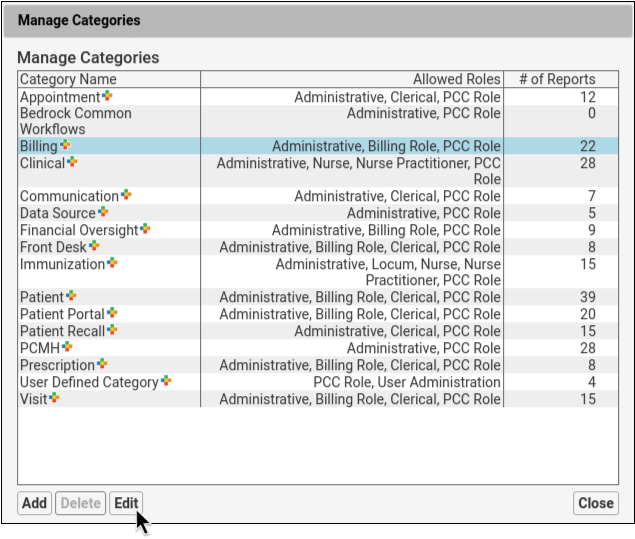
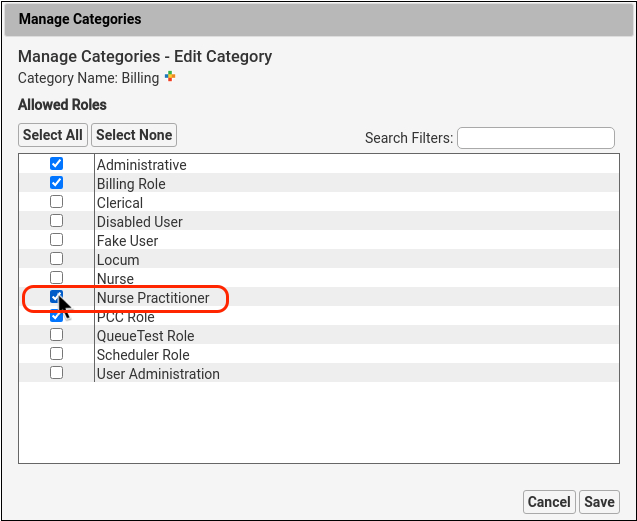
Users whose roles are unchecked will not see this category in the Report Library window.
Assign at Least One Category to Custom Reports
If a custom report is not assigned to a category, then it will appear under All Reports and will be available to any user with access to the Report Library. To restrict access to a custom report, you’ll first need to assign it to a category in the Customize Report window.
Optionally Allow Full Access to a Specific Report
To allow access to a specific report, click “Select None” in the report’s Edit Categories window. This report will be available to all user roles that have access to the Report Library.
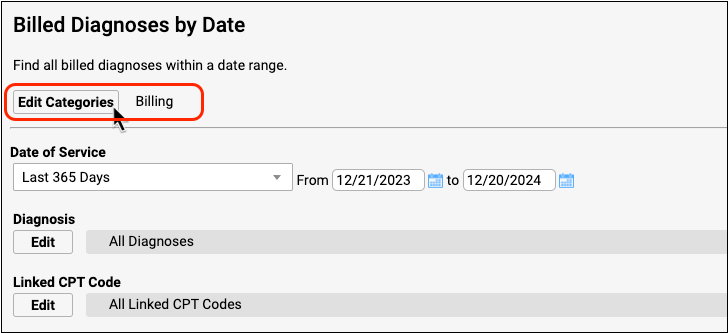
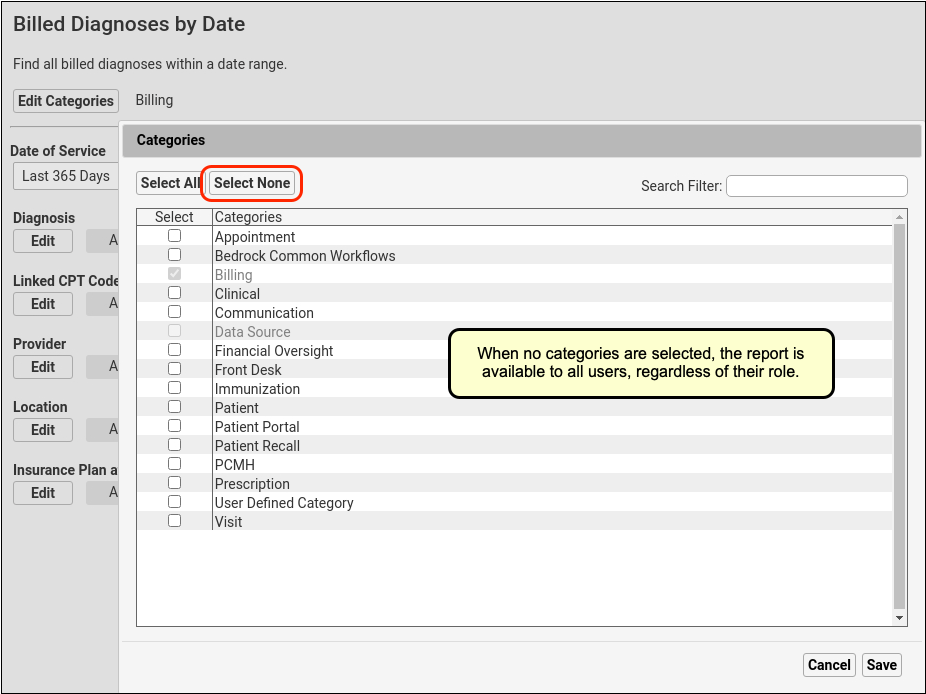
Stock reports cannot be removed from their default categories. For example, in the screenshot above the Billed Diagnoses by Date report cannot be removed from the Billing category.
Restrict Access to Manage Categories and Customize Reports
Access to the Customize Report and Manage Categories tools are controlled like other permissions: through the Roles tab within the User Administration tool. User roles with the Manage Categories permission control access to which roles can see specific reporting categories.
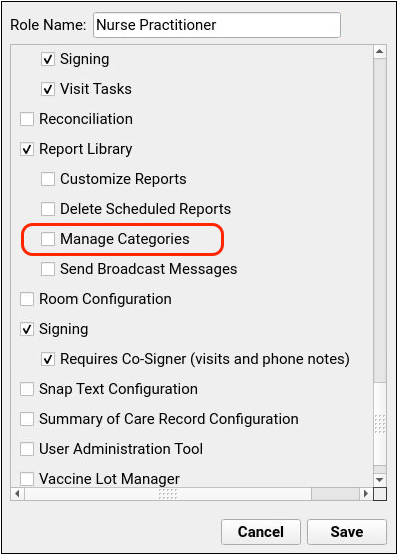
Users with permission to Customize Reports can customize existing reports and create new reports. Users without that permission will only be able to run preexisting reports.
Likewise, users without the Manage Categories permission will not see the Manage Categories button on the Report Library window.
Troubleshooting Slowness in PCC EHR
Occasionally, you may find that PCC EHR runs slowly– either just for certain actions, or for all actions. There’s a wide range of causes for software slowing down- some that you may be able to deal with on your own, and some that PCC Support can help you with, and some that our Development Group may need to investigate and resolve. Either way, there’s a few things you can check out before calling PCC that will either resolve the issue for you, or help PCC find and fix them cause.
Try A Different Workstation
Is this happening just for you, or just on one workstation in your office? If so, it may be an issue with the computer itself, or its network usage. If the slowness is being experienced by only one user, ask that user to log into the workstation of another user who hasn’t experienced any slowdown. That’s the fastest way to find out if it’s a workstation issue, rather than a problem with the EHR, the server itself, or the local network.
Find Out if It’s Just PCC EHR, Or Your Whole Computer
Run some other applications: open a web browser and visit a few pages, come here to Learn.pcc.com and play a video or two, launch Excel and open couple spreadsheets, resize a photo. See if anything else runs slower than usual.
What happens when you or the user logs into PCC EHR on another workstation? On this other workstation, go through the same actions as above, open some other applications alongside PCC EHR and run through various actions in all of them. If it’s speedier on that second workstation, then the issue is probably with the first workstation.
Troubleshoot Performance of a Single Workstation
If the affected workstation is using Windows, run the Task Manager by pressing Ctrl + Shift + Esc, or by searching for “Task Manager” in your Start Menu.
In Task Manager, select the Performance tab and check the left column’s CPU, Memory, and Ethernet or Network usage. Anything above 80% may explain general slowness of Windows applications or internet usage on that particular workstation.
On a Mac, run Activity Monitor from the Spotlight Search on the upper right, or find Activity Monitor in your Applications folder. At the top of the Activity Monitor window, click through the CPU, Memory, and Network options.
In CPU, check the System percentage in red at the bottom of the window. A high percentage may indicate that one or more processes are using most of your workstations processing power, and not leaving enough for the EHR to run smoothly.
In Memory, look at the Memory Pressure graph at the bottom left. This graph shows your memory usage, and a lot of red indicates some process is using most of your available memory- which can cause lag in other applications.
Check Your Wireless Connectivity
The Network tab shows current network resources, the packets meter at the bottom shows sent and received data. Big spikes in either direction could indicate that a process or application is using all your available network problem that would cause trouble remotely accessing your server and slowing down PCC EHR.
If the Network tab shows no big spikes of activity, but you’re still seeing websites load slowly in addition to PCC EHR, it may be helpful to move that workstation- if it’s a laptop- to another part of the office. Getting closer to the wireless access point or toward a different one, may show some improvement.
If you do see improvement by moving, it’s likely that other users are encountering the same problem when in that area. PCC’s Technical Solutions Team can look at your network and make suggestions on how to proceed to improve network coverage within your office.
Check Your Power Settings
MacOS users may find that adjusting their Power Saver settings can reduce instances of PCC EHR running slowly after waking up from sleep. In your System Preferences, open Energy Saver, and ensure that “Prevent computer from sleeping automatically when display is off” is checked, and “Put hard disks to sleep when possible” is not checked.
Tell PCC About Any New Equipment
Have you replaced a printer, scanner, or network device and not informed PCC? Depending on what’s been replaced, new devices can cause printing to lag, scanned documents to fail to arrive promptly in Import Documents, or network interference. Get in touch with PCC’s Technical Solutions Team with the make and model number of the new device and, if it’s replacing an existing item, which item it’s replacing.
Determine if Slowness Occurs Only At Certain Times During Day
Depending on your office staffing and your appointment schedule, it’s likely that more users are actively using PCC EHR at certain times of the day, so there will always be some variability in speed, though mostly not a noticeable amount- PCC provides hardware sturdy enough to carry the load. If you do notice PCC EHR running significantly slower at certain times of the day, our Technical Solutions Team can look into your network and server usage and determine if adjustments or upgrades are needed to keep you running smoothly over the course of the day.
The EHR Runs Slowly After Log In and After PCC EHR Release Updates
Be aware, however, that some variability in speed is always going to exist. For instance, the first couple charts each user opens after logging in will take a small amount of time longer than is usual for the rest of the day. On login, EHR caches some data, and refers to that data for the remainder of the session. This is one case where restarting PCC EHR won’t help, since it will just start the caching process over again. Power through the first few charts, and opening charts will speed up.
Likewise, similar caching occurs after a PCC EHR update- though an update includes much more data- the EHR will generally run somewhat slower in the first day or two of usage after an update.
Contact PCC Support
With the above complete, you’ll either have found the cause, or gathered enough information for PCC’s Technical Solutions Team to get right to work.
Review Your Schedule With Appointment Reports
PCC EHR includes a wide variety of appointment reports. You can use them to produce a daily huddle sheet, figure out when appointments are being overbooked, and even plan inventory for upcoming well visits.
The Appointment Reports Section of the Report Library
When you need to report on appointments, you can use the Appointment Reports section of the report library in PCC EHR.
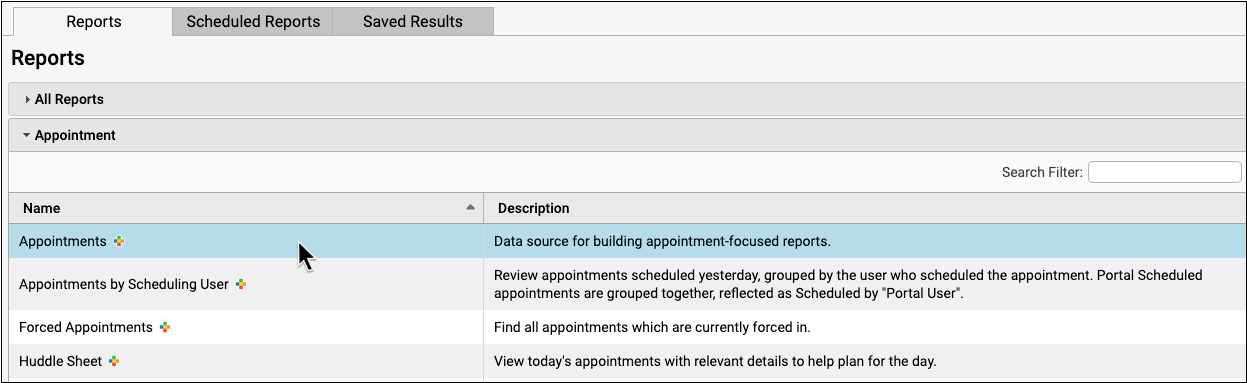
You can use one of the reports created by PCC or by your practice, or create a new custom report based on the parent “Appointments Report”.
Find Forced Appointments
Use the “Forced Appointments” report to find all appointments that have been forced into the schedule.
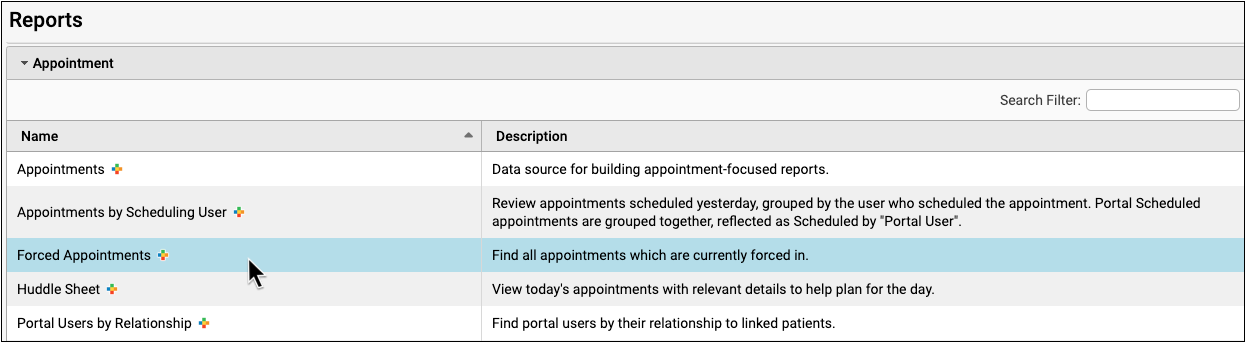
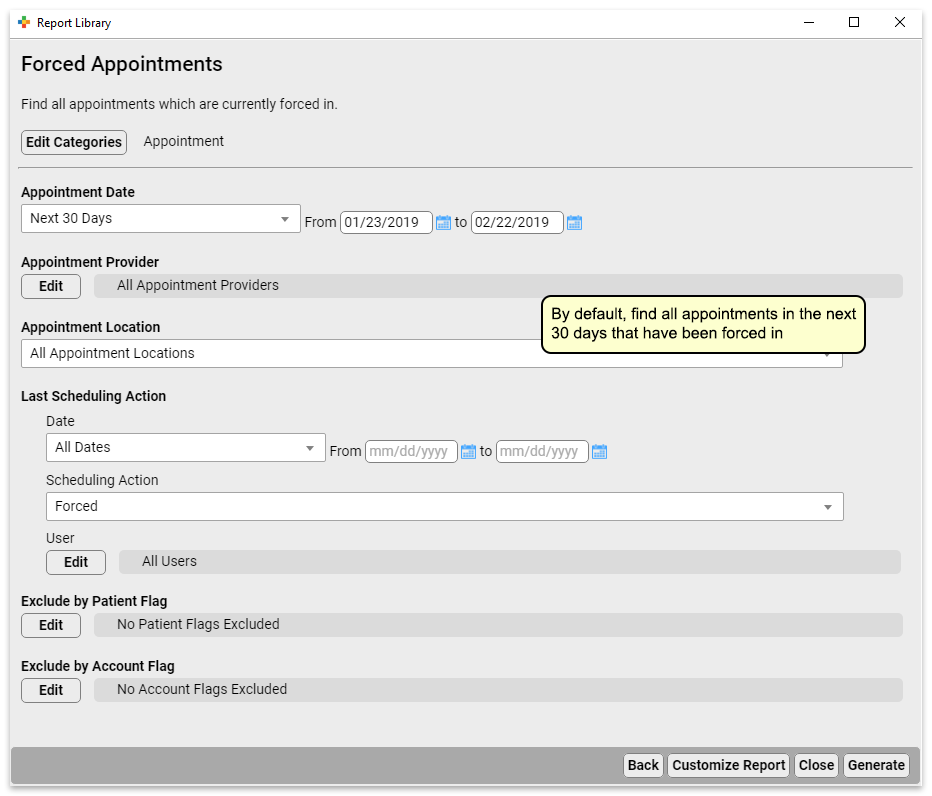
If your practice has a habit of double-booking appointments, or you need to understand when your providers are most often over-booked, you can review the Find Forced Appointment list to get the data you need to make adjustments.
Create a Daily “Huddle” List for Your Morning Meeting
Use the “Huddle Sheet” report to generate a list of all appointments on a date or range of dates that you can use to prepare for the day.
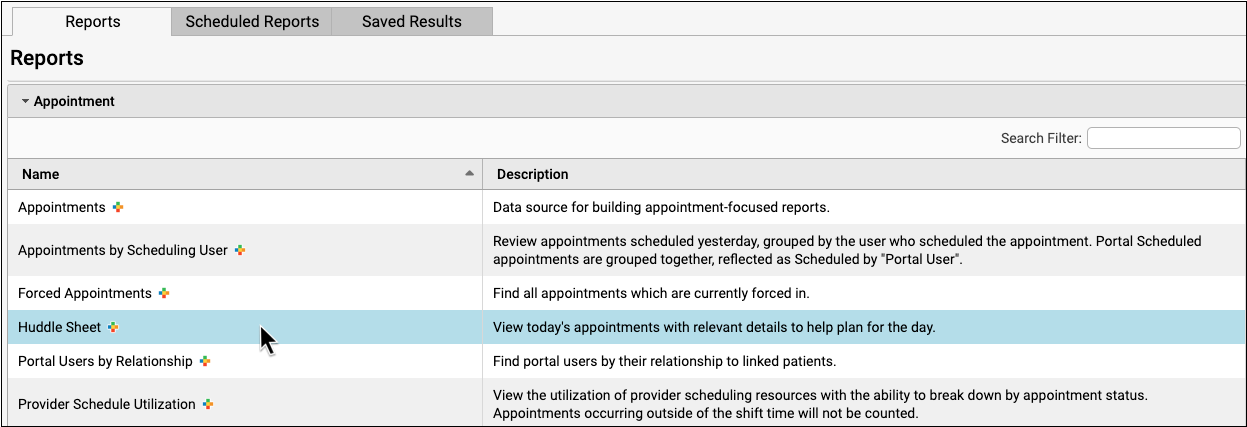
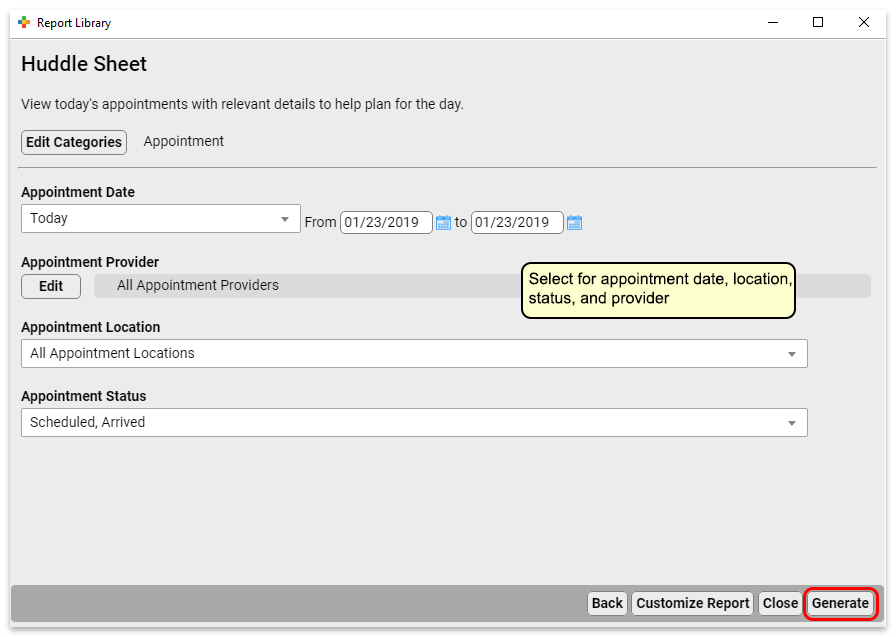
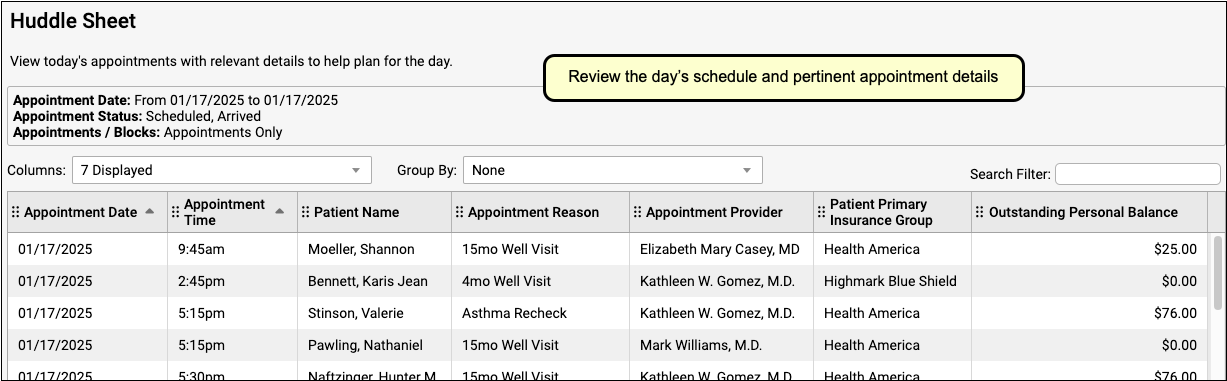
When you meet together in the morning, your staff can use the information on the Huddle Sheet report to review special circumstances for each patient or family and plan accordingly.
Create Custom Appointment Reports
Do you need to review and research your practice’s scheduling history? You can customize one of the existing appointment reports to create your own appointment report.
The data source “Appointments” report includes all the filters you need to create a custom appointment-based report.
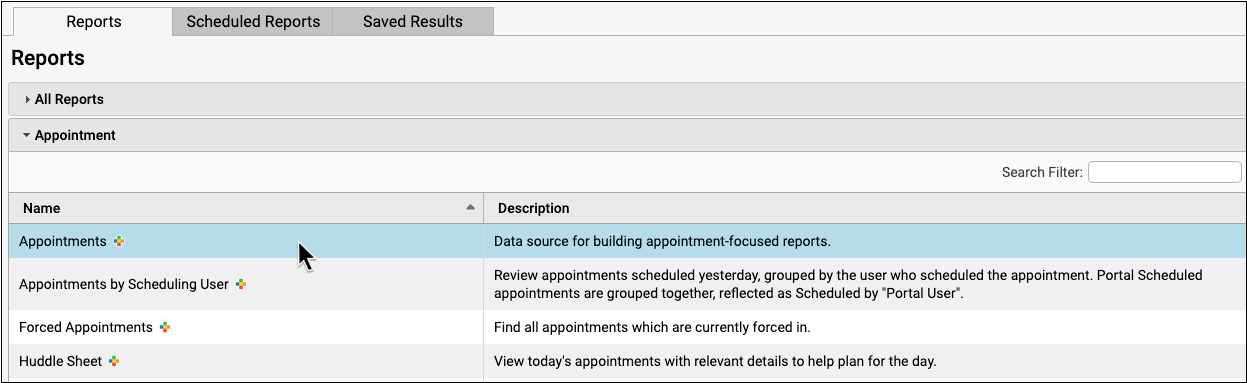
Appointment Book Web Lab: Why You Should Make the Jump
In May of 2019, PCC’s Lynne Gratton held a live webinar for existing PCC clients considering implementation of PCC’s Appointment Book. The Web Lab shows off all the functionality of the Appointment Book and answers questions.
Clinical Document Exchange
The promise of interoperability between EHRs — that patients’ data will be accessible to any clinician whom they see for treatment — is one step closer to realization.
PCC has implemented an interoperability framework that allows practices to automatically make clinical information available to other providers and organizations who participate in the Carequality Interoperability Framework. This includes many hospitals, specialists, and other networks who may serve your patients.
Participation is Optional: Participation in clinical document exchange with other organizations who are also implementing the Carequality framework is optional, and is included in PCC’s comprehensive service plan. In order to participate, contact PCC Support. If you choose to proceed, which include signing an addendum to your PCC EHR agreement acknowledging and agreeing to the Carequality Connection Terms.
Watch an Introductory Video: Watch Clinical Document Exchange: The Responder Role to learn the basics of CDE along with details about the Responder role, wherein your practice receives requests and shares information.
What is Clinical Document Exchange?
Clinical Document Exchange (also referred to as Query Based Clinical Document Exchange, or QBCDE) allows different healthcare organizations to exchange patient records. Your participation would allow other providers who see your patients to obtain your patients’ records for treatment purposes, as defined in the Health Insurance Portability and Accountability Act (HIPAA).
The Carequality Framework
Carequality is an organization that maintains a framework of technical, data, and privacy standards that allows organizations who implement that framework to directly exchange data.
All implementers of the Carequality Framework sign an agreement with Carequality, outlining rights, obligations, and “rules of the road” for trusted exchange of data. All implementers of the framework are able to exchange patient records with all other implementers of the framework. Carequality maintains a list of software vendors, Health Information Exchanges (HIEs) and others who have adopted the Carequality Interoperability Framework, as well as a tool to search for hospitals clinics, and other entities who are participating. Use this tool to see if you can exchange data with your local hospital or specialists.
The Responder Role
There are two sides to clinical document exchange; an organization in the Initiator Role makes record requests, and an organization in the Responder Role responds to record requests.
What Data will be Shared?
If your practice participates in clinical document exchange, the patient’s most up-to-date Summary of Care Record is made available and contains information including:
- Demographic data (Name, D.O.B., Address)
- Clinical data
- Diagnoses
- Allergies
- Medications
- History of Procedures
- Diagnostic and Laboratory Test Results
- History of Immunizations
- Insurance Policies
Customize the Summary of Care Record: Your practice can configure which information is included in patients’ Summary of Care Records. Click here to learn how.
Who has Access to Patient Data?
Other healthcare organizations that participate in clinical document exchange through the Carequality interoperability framework are able to retrieve your records. They may retrieve your records for treatment purposes only.
Is Clinical Document Exchange Safe and Secure?
Yes. Many layers of security protect patient data both in storage and when it is transmitted to a different healthcare organization.
Do patients or their families need to consent to Clinical Document Exchange?
Your practice needs to make an informed decision about whether you will have an opt-out or opt-in policy for clinical document exchange. Some practices choose an opt-out policy, meaning that all patients are considered to have consented to clinical document exchange unless otherwise indicated. Practices that choose an opt-in policy will require patients to give explicit consent to participate in exchange activities.
You will need to consider your state’s patient privacy and consent laws, your existing office policies, and provider preferences. Laws and policies vary between states. Some state policy is more stringent than federal HIPAA policy and if that is the case, the state policy should be followed, not the federal. PCC recommends that you consult with your practice’s legal counsel and/or malpractice carrier to determine what laws apply in your specific circumstances.
What Does it Cost?
Nothing. Clinical Document Exchange is offered to all PCC clients as part of our comprehensive service plan. There are no hidden fees or additional charges for PCC clients to participate in the Carequality Interoperability Framework.
How do I Participate?
If you are interested in participating in clinical document exchange, contact PCC Support.
Getting Started with Clinical Document Exchange
Follow these steps to get started with clinical document exchange.
Find Out Who You can Connect With
Follow this link to search for Carequality enabled organizations near you.
Determine Your Practice’s Consent Policy
Before contacting PCC Support, please decide whether your practice will have an opt-in or opt-out policy. PCC recommends consulting your practice’s legal counsel as you determine which policy will work for you.
Contact PCC Support
Contact PCC Support to let them know you are interested in clinical document exchange. Your CA can answer general questions about Carequality and and the document exchange process. When you are ready to move forward, they will put you in touch with the PCC teams that will manage your onboarding and go-live.
Review and Sign Carequality Connection Terms
When you are ready, PCC Sales will send you the Carequality Connection Terms for your review and signature. This is an agreement to follow Carequality guidelines – there is no charge to you to participate in the Carequality Interoperability Framework.
Train with PCC
You will have a one-hour training with PCC’s Interoperability Implementation team, in which you will:
- Learn about document exchange functionality
- Review patient consent configuration options in PCC EHR
- Discuss your practice’s consent policy and workflow considerations
- Find out how to talk to your patients about clinical document exchange
Schedule a Go-Live Date
Schedule a go-live date with PCC to enable clinical document exchange functionality! Once you are live, Carequality enabled organizations will be able to retrieve Summary of Care documents for patients who have consented. No more faxing!
Notify Carequality Enabled Organizations
Notify Carequality enabled organizations who work with your practice that your patients’ documents will soon be available for retrieval. You can explain the new capability in the following way: “Our practice will be making our patients’ documents available to you through Carequality.”
Configure PCC EHR for Clinical Document Exchange
Once you have worked with PCC Support to get started with clinical document exchange, there are a few things you will need to configure in the EHR.
Set Default Consent Status for New Patients
You need to decide whether you will have an opt-out or opt-in policy for clinical document exchange. Once you have done so, set this status in the Practice Preferences tool.
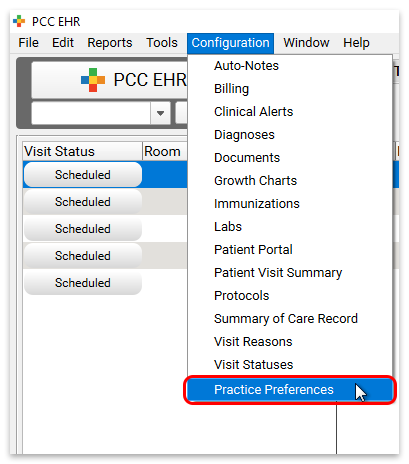
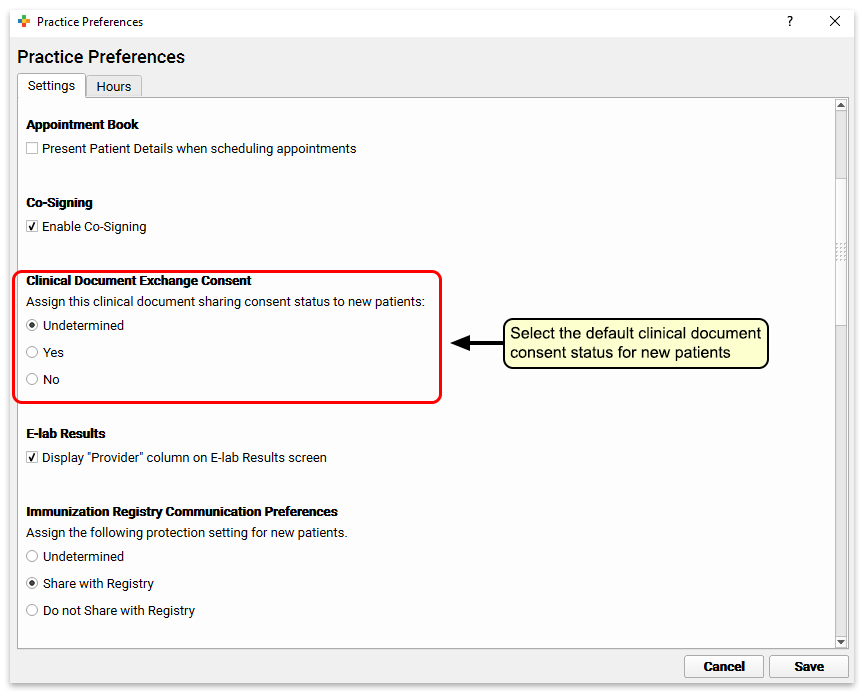
You can choose whether new patients’ consent status will default to “Undetermined”, “Yes”, or “No”. Note that a status of undetermined is functionally the same as a status of no. The data of patients with the status of either undetermined or no will not be shared, while those with a status of yes will.
Add Clinical Document Exchange Consent to Communication Preferences
Once clinical document exchange has been activated for your practice, a section for patients’ consent status will appear in the Communication Preferences component in your chart notes. To make this status appear prior to activating clinical document exchange (perhaps you are acquiring patient consent in advance of implementing this feature), edit the Communication Preferences component with the Protocols configuration tool.
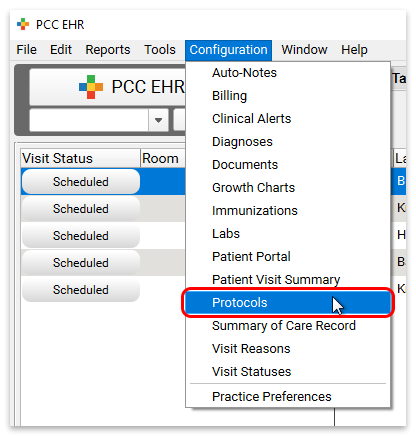
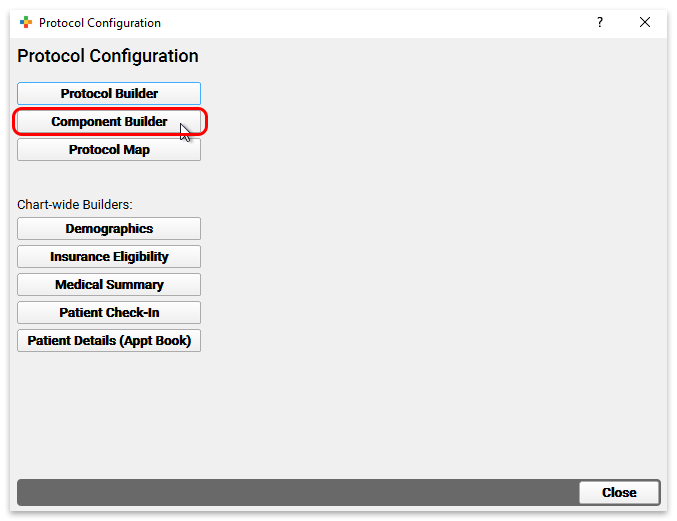
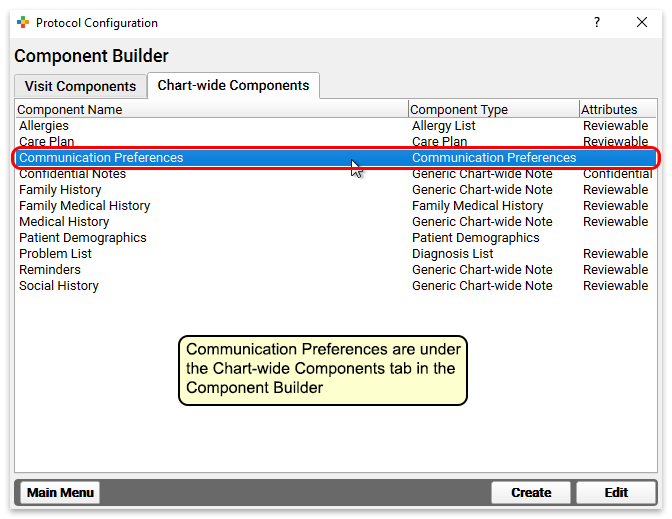
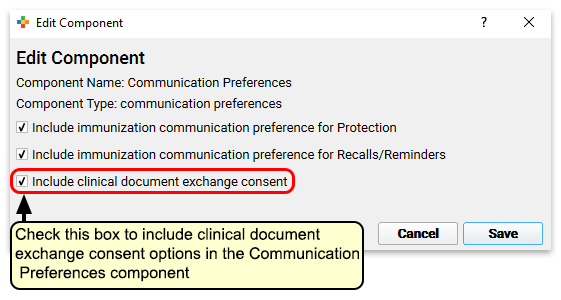
After choosing to include clinical document exchange consent in this component, it will appear in all patients’ charts.
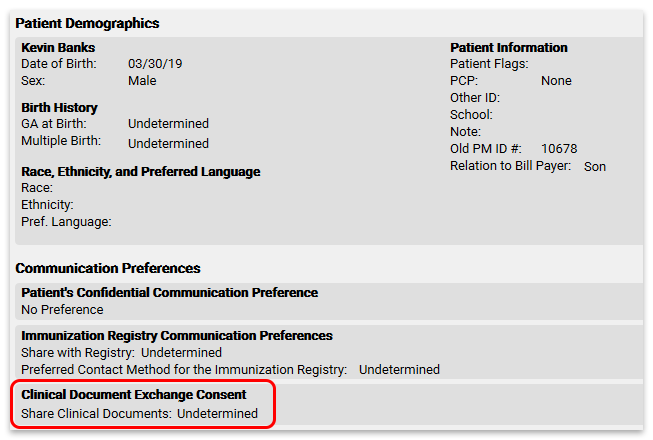
Change a Patient’s Consent Status
To change a patient’s consent status, edit their chart and select a new status.
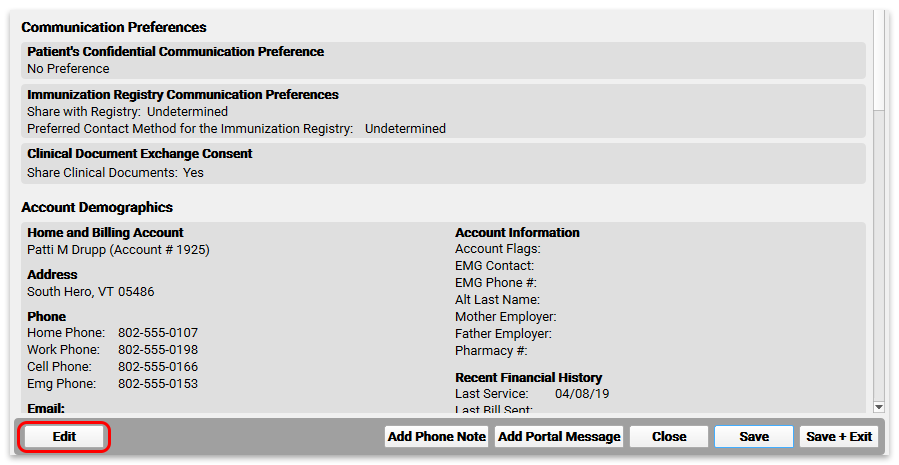
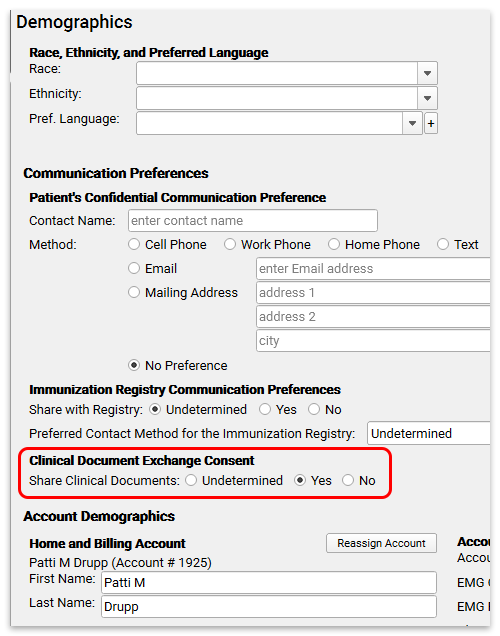
Retrieve Clinical Documents from Other Healthcare Providers
Once you become a Clinical Document Exchange Responder, the groundwork is laid for your practice to enable the “Initiator” role, which allows you to securely retrieve patients’ clinical documents from other healthcare providers.
Read about how to Securely Retrieve Clinical Documents from Hospitals and Other Providers Through PCC EHR.
Reconcile Personal Payments
You can quickly and easily reconcile personal payments posted for the day. Use the Payment Reconciliation report to prove out and review cash, check, and credit card totals at the end of your shift.
Open the Payment Reconciliation report from the Report Library in PCC EHR.
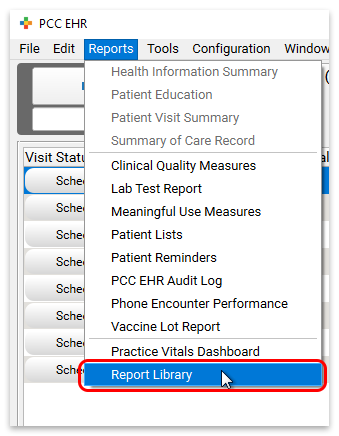
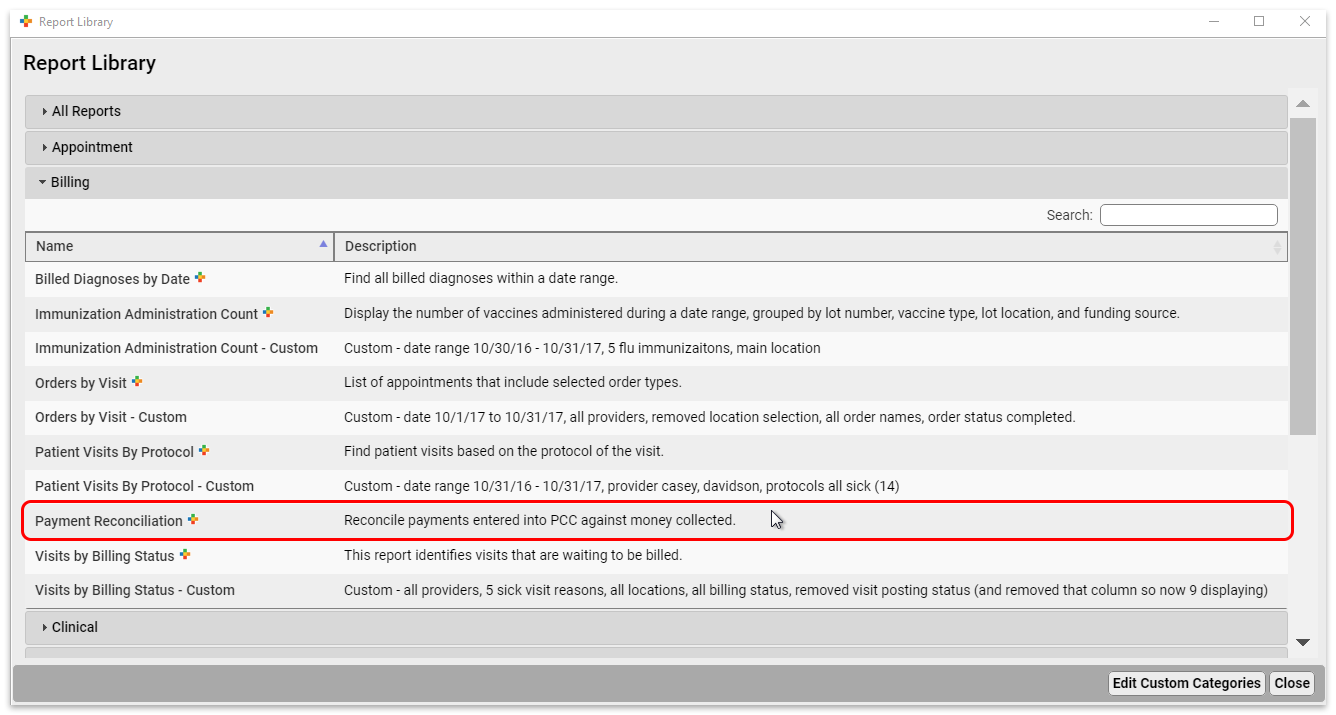
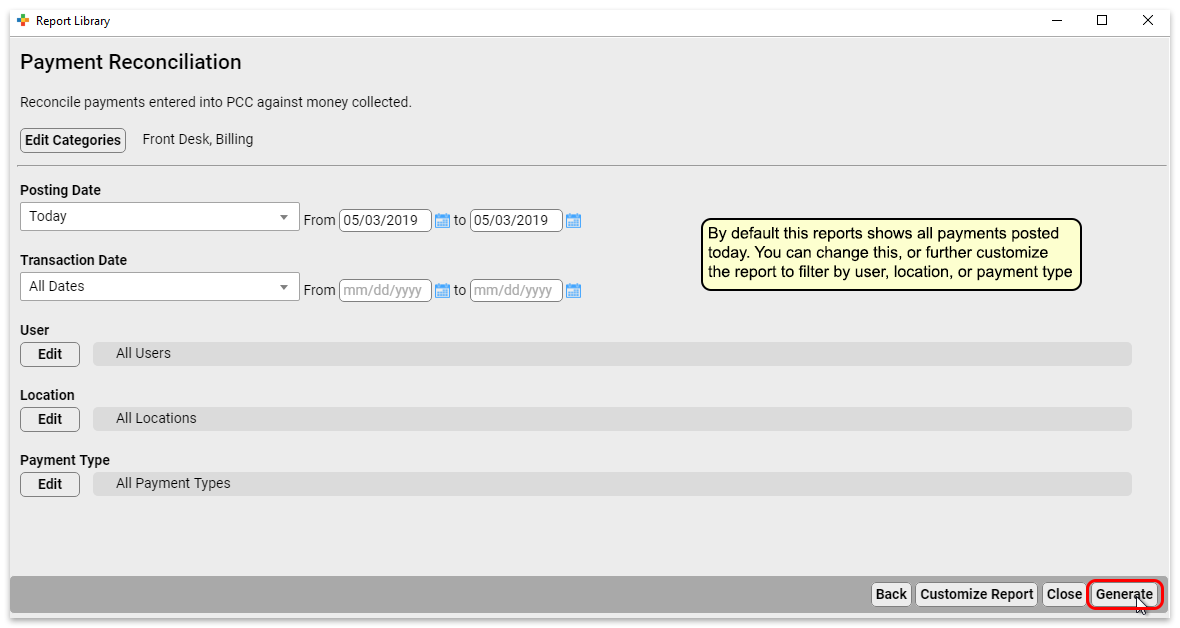
You can customize the Payment Reconciliation report to filter your results by date, user, location, and payment type.
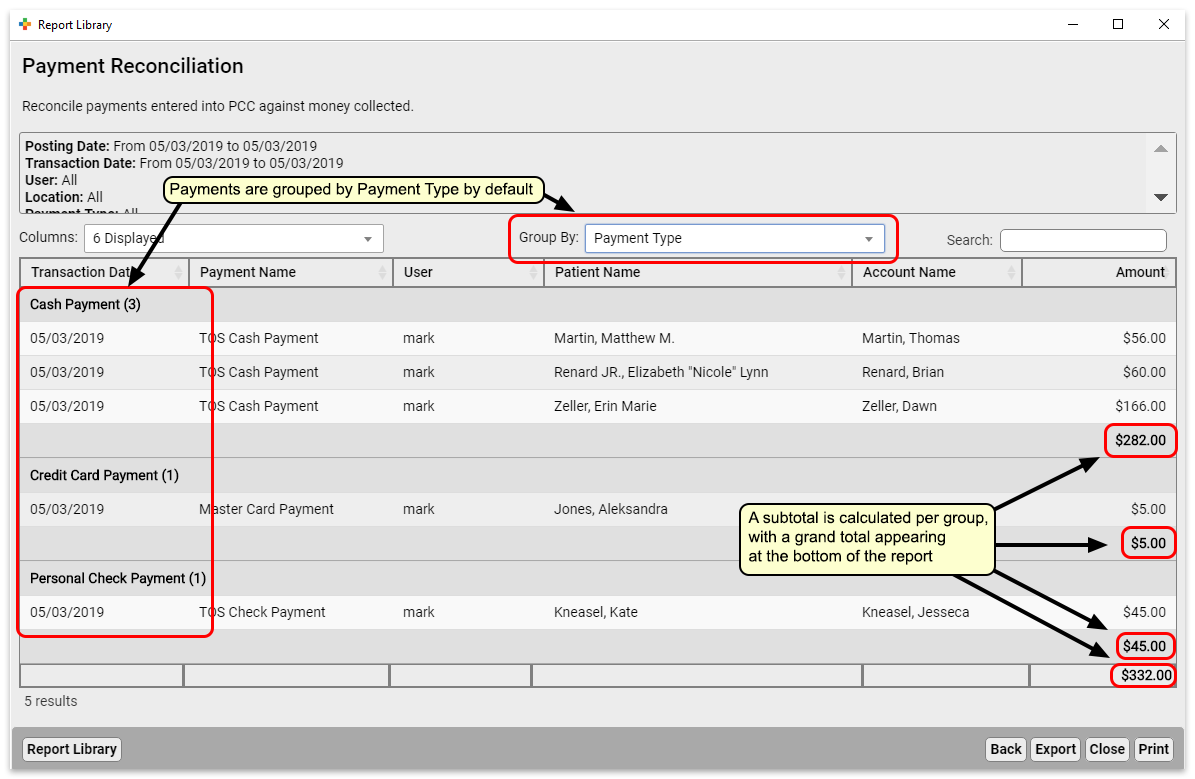
The Payment Reconciliation report subtotals each payment type to make proving out easy.
If you want to view this report grouped in a different way, for example organized by the user who posted the payment, you can use the “Group By” drop-down to select “User” instead of the default “Payment Type”.
Export to .csv: You can click “Export” to export the report data to a .csv file, which you can later import to a spreadsheet program. Note that subtitles and groupings only appear on your screen, and will not be included in .csv exports.
Fix Payments that Were Posted Incorrectly
As you review the Payment Reconciliation report, you may find payments that were posted incorrectly.
Use the Payments tool in PCC EHR to edit any personal payments. You can update the transaction date, the payment type, the payment amount, and how the payment applies to charges on the account.
For more information, read Review Payment History and Edit Personal Payments.
Configure Your Patient Portal Message Templates
Busy parents want a way to communicate effectively with your practice when it’s convenient for them, without having to play phone tag.
PCC EHR includes three optional patient portal message templates that you can use as-is, or customize to work better for your office.
You can also create your own messaging templates.
How do Portal Message Templates Work?
When a parent or other portal user sends you a message using a template, the results appear in the portal message in PCC EHR.
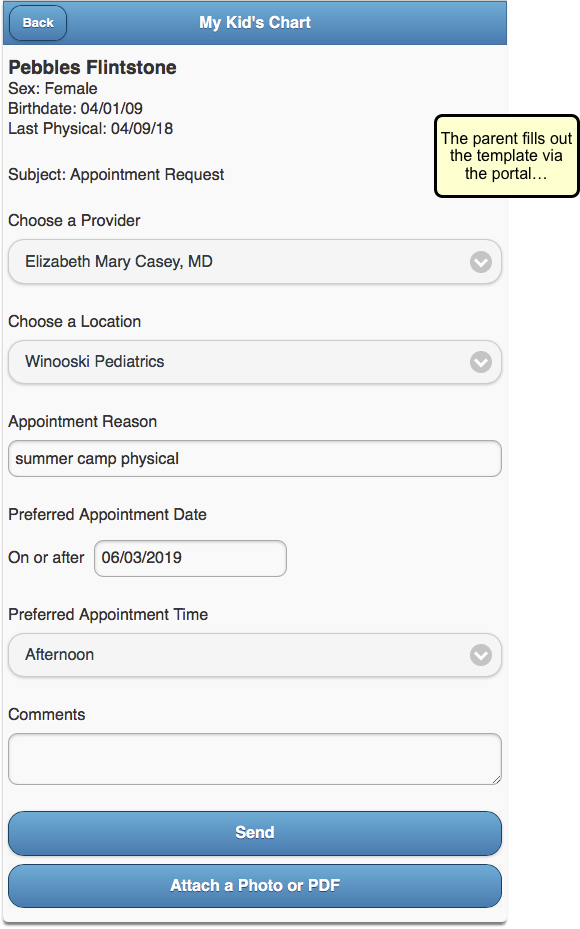
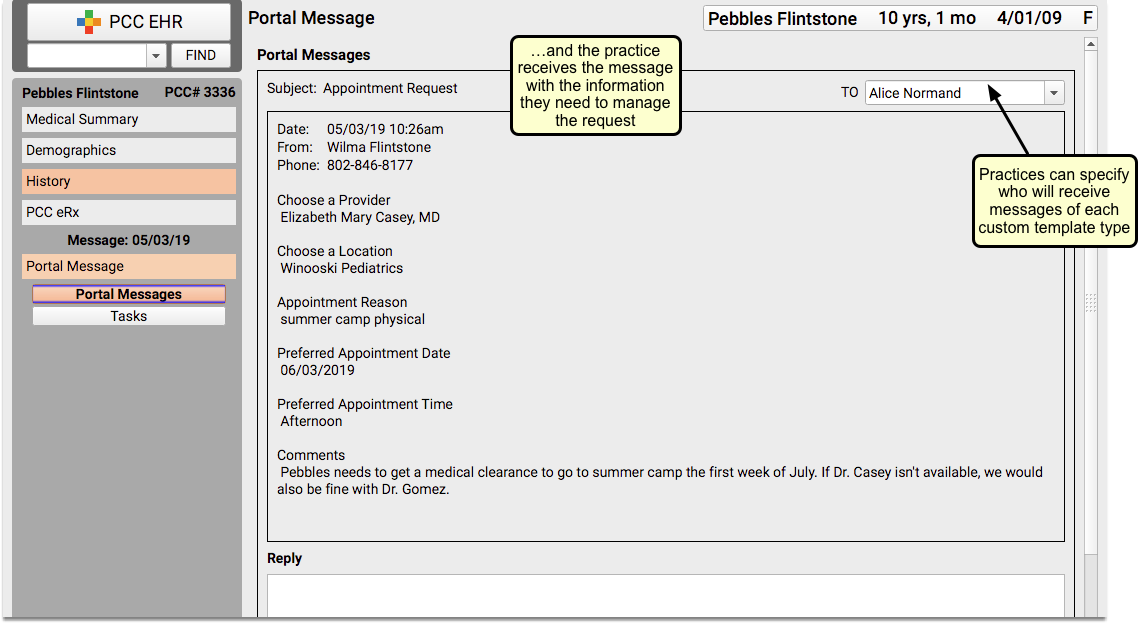
To work with your practice’s patient portal message templates, click on the Messaging Templates tab of the Patient Portal Configuration tool.
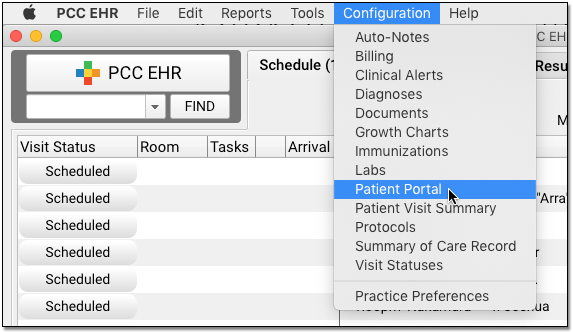
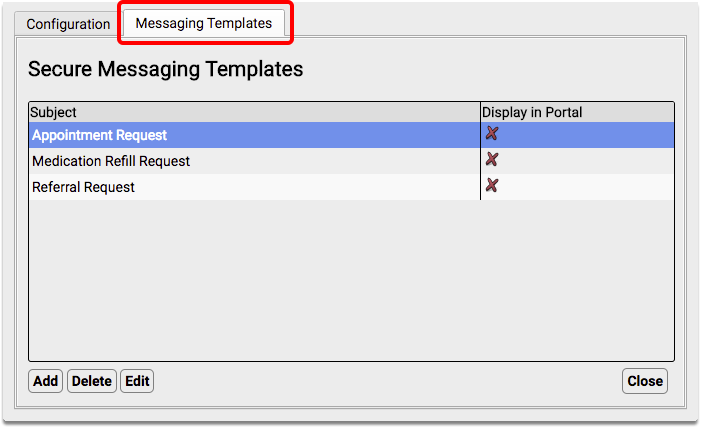
In order to use portal messaging templates, your practice must have Secure Messaging enabled. For more information about configuring your patient portal, read Patient Portal Practice Settings and Configuration.
Templates are Turned Off by Default: If you want to use the three optional patient portal message templates, you will need to turn them on. Edit the template and check the “Display in Portal” checkbox to make the template available to your patient portal users.
Default Templates: What Families Will See
If your practice chooses to enable patient portal messaging templates, your portal users will see a new Subject drop-down option when they choose to create a message:
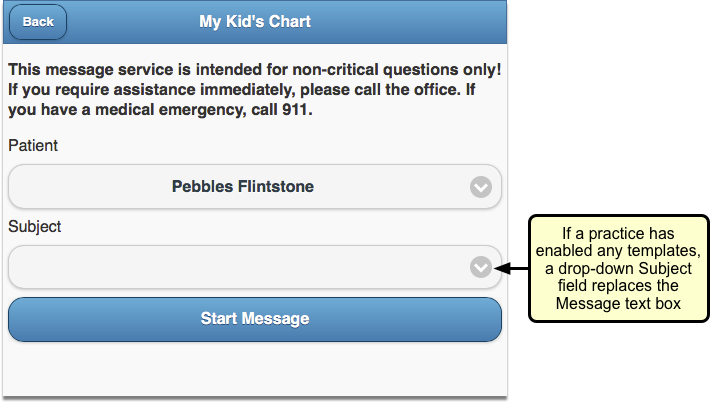
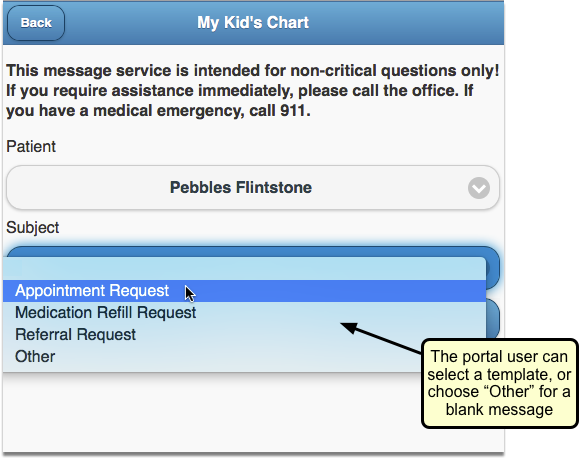
When the portal user selects a message subject, they will see a list of information to fill out, depending on which subject they select.
Appointment Request
The Appointment Request default portal message allows the portal user to select a desired provider and location on a specified date at a preferred time of day.
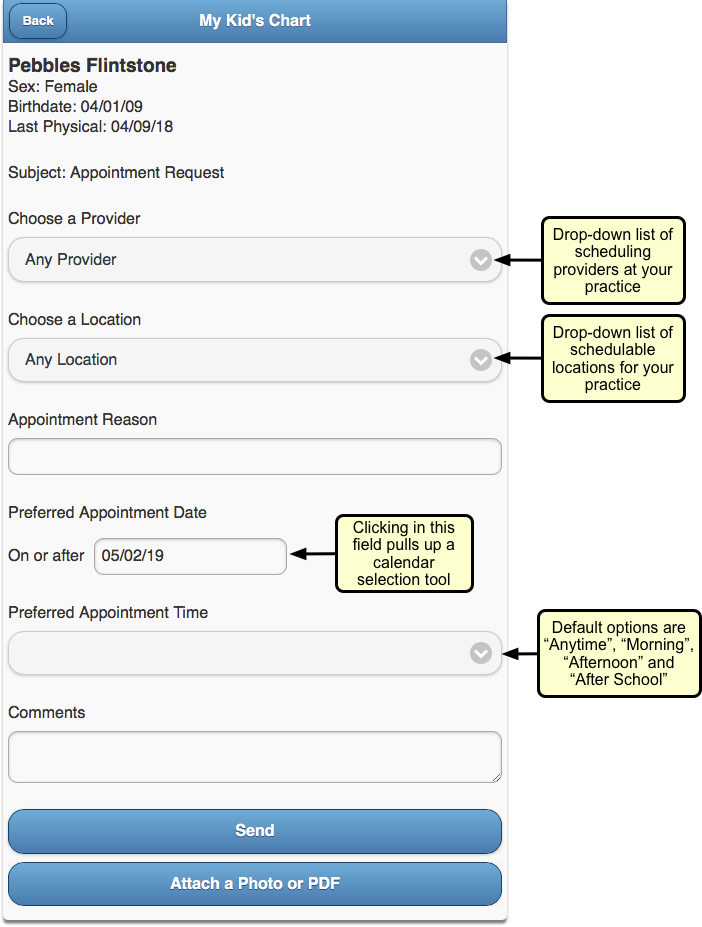
The portal user can write a short note about the type of appointment they need and can include a longer note with comments. They can even attach a related photo if they choose.
Your practice can edit the Appointment Request default template to better suit your needs.
Medication Refill Request
The Medication Refill Request default portal message includes a list of the patient’s medication allergies, with a request to confirm them. There are entry fields for the portal user to record the prescription they want refilled and the name and location of the pharmacy they want to use.
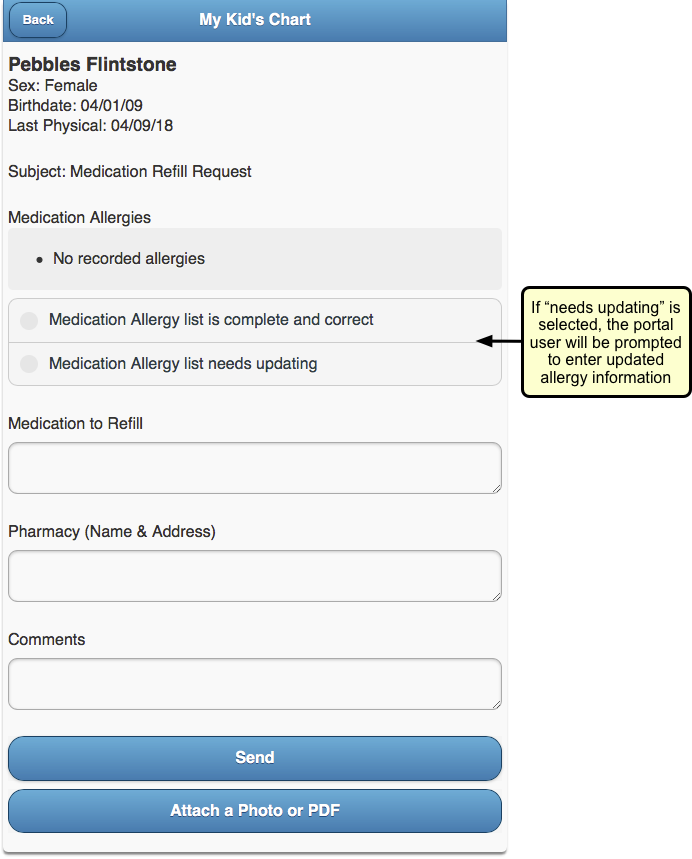
The portal user can add comments if they need to, and can attach a photo as well, if applicable.
Your practice can edit the Medication Refill Request default template to better suit your needs.
Referral Request
The Referral Request default portal message includes entry fields for the portal user to describe why they want a referral, who they wish to see and what the provider’s speciality is, along with the provider’s phone, fax, and office name and address.
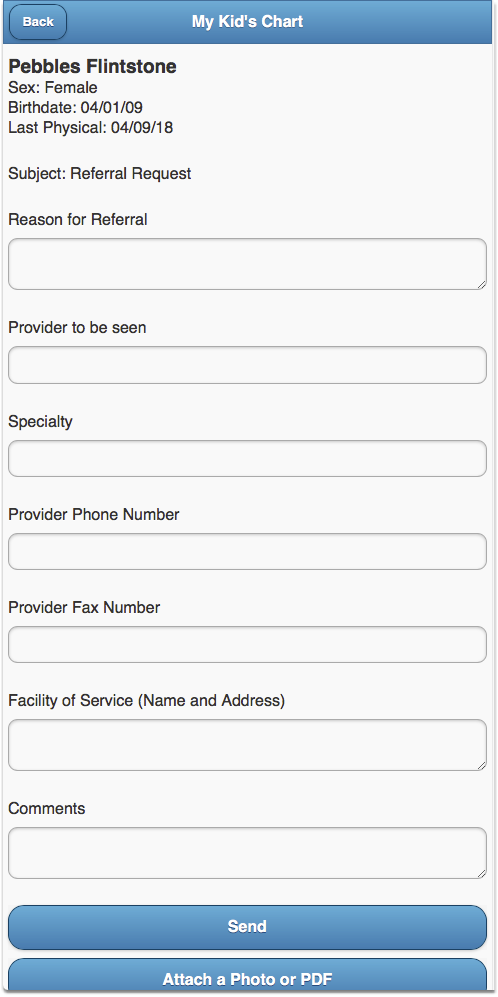
The portal user can add comments if they need to, and can attach a photo as well, if applicable.
Your practice can edit the Referral Request default template to better suit your needs.
Edit Portal Message Templates
If the default portal message templates don’t work for your practice, or if you want to update a custom template, you can easily make changes.
Edits are Permanent: Keep in mind, when you edit a default template, the original template will be lost. You will need to recreate it from scratch if you wish to use it again.
From the Messaging Templates tab of the Patient Portal Configuration screen, highlight the template you want to update and click “Edit”.
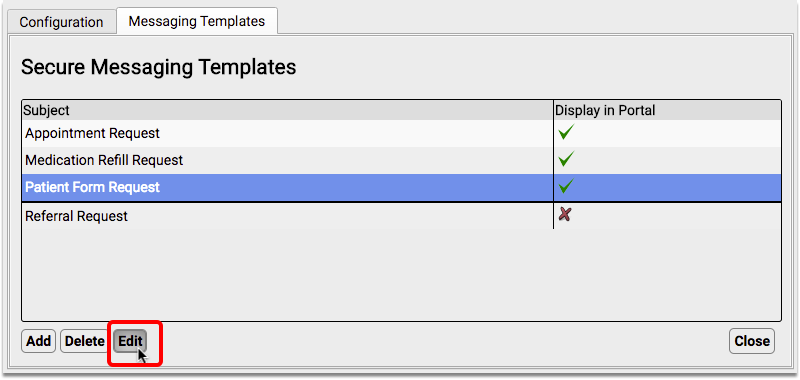
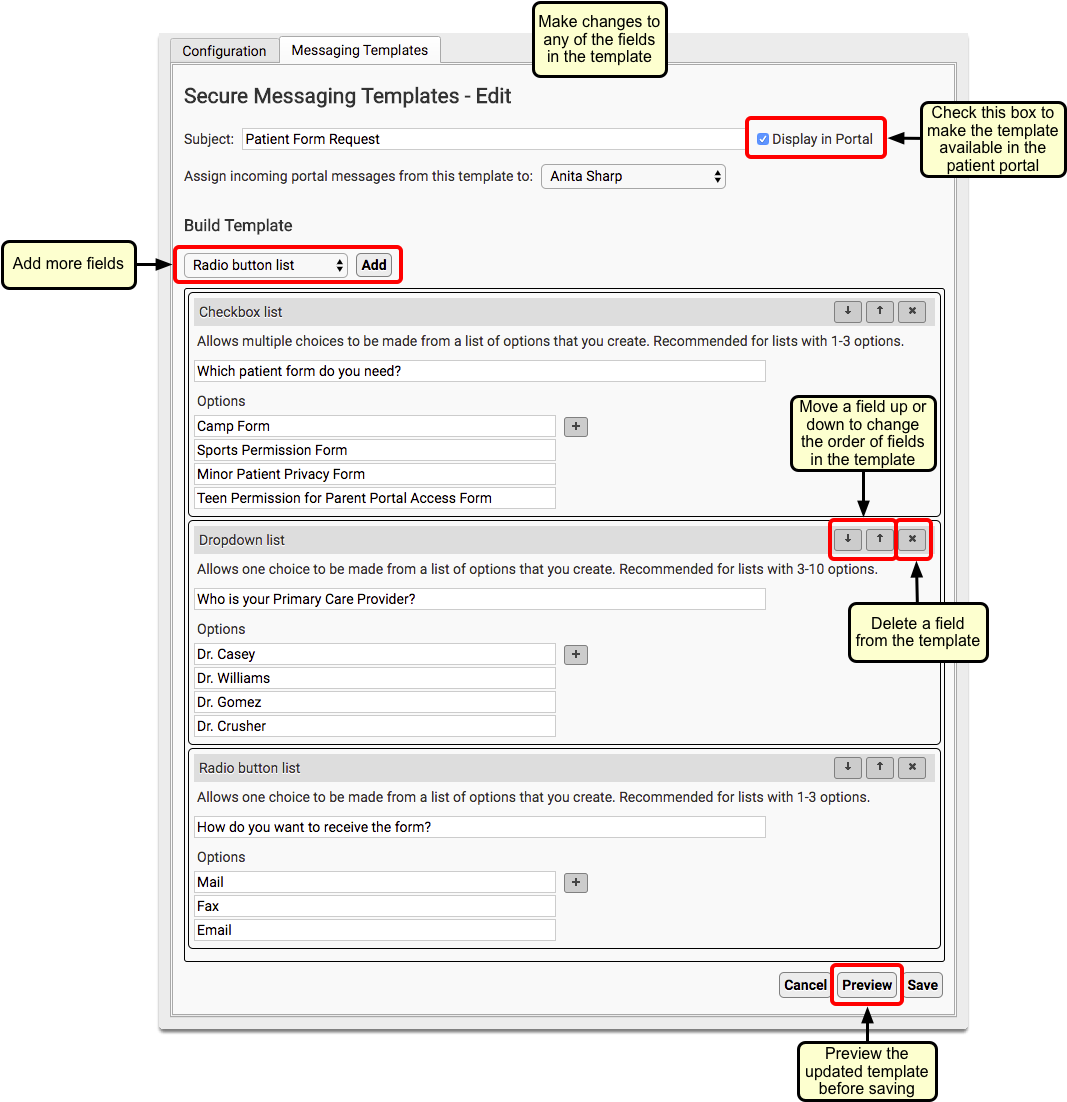
You can make changes to any of the template fields. You can add new fields (see the Portal Message Template Field Reference, below), move fields up or down, and delete fields that you don’t want.
To see what your changes will look like before you save, you can click “Preview”.
When you are satisfied with your changes, click “Save”.
Create New Message Templates
Your office can create your own custom messaging templates.
Click “Add”
From the Messaging Templates tab of the Patient Portal Configuration screen, click “Add”.
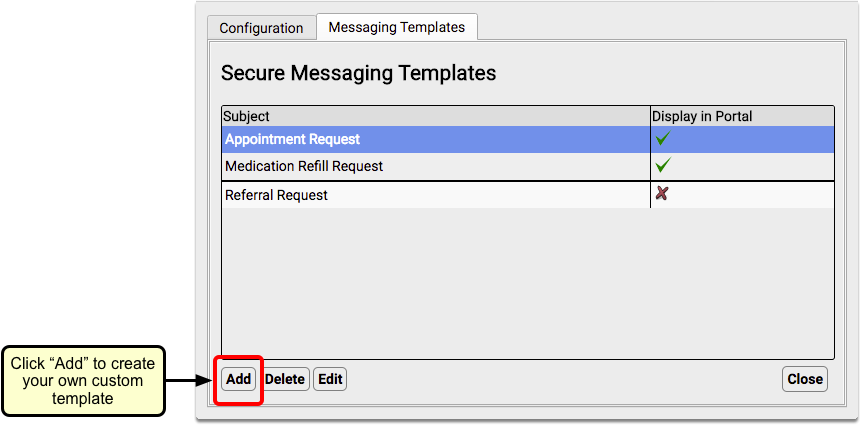
Name the Template and Optionally Enable and Assign
Enter a name for your new template in the Subject field, and select the “Display in Portal” checkbox to make the template visible to portal users.
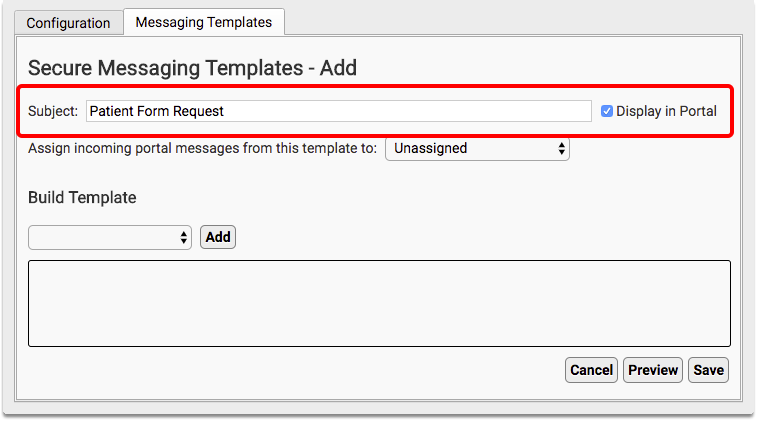
You can also choose to automatically assign incoming messages of a certain template to a specific person at your practice.
Add a Field to the Template
Select a field type from the Build Template drop-down and click “Add”.
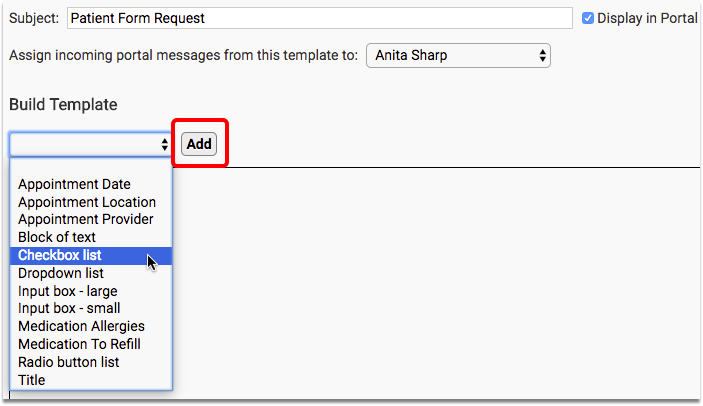
In this example, we are creating a checkbox field. Check out the Portal Message Template Field Reference, below, for a description of each available field type.
Name the Field and Add Options (for some types of fields)
Give the field a name.
Since we are adding a checkbox field, we will add checkbox list options one after another.
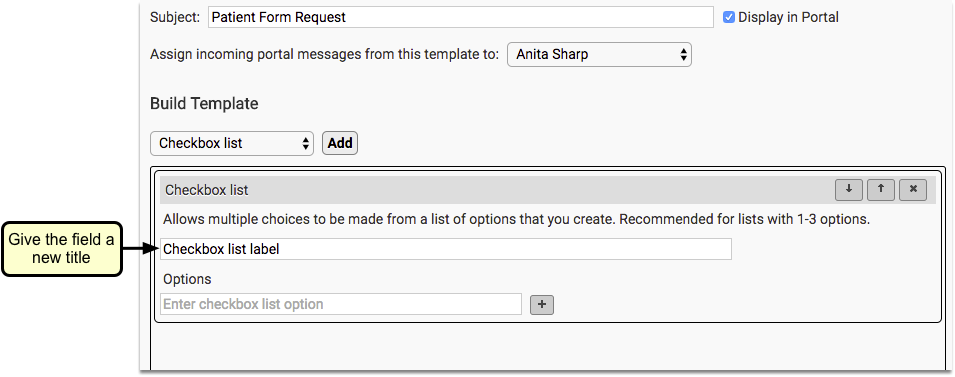
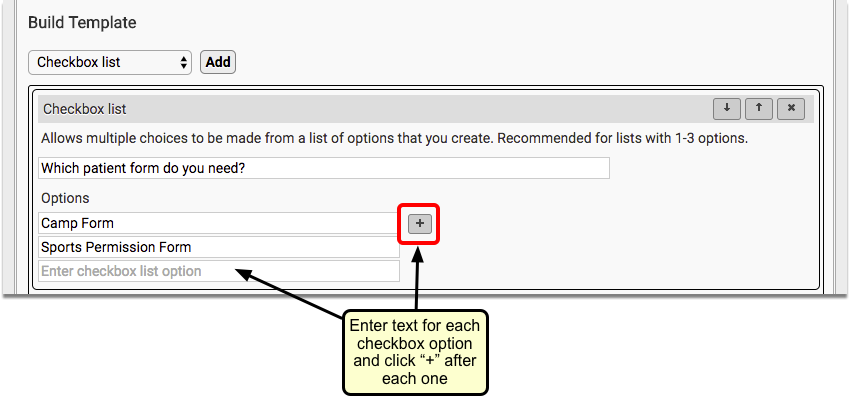
Enter text in the Options fields and click the “+” button after each entry.
Add Additional Fields, as Desired
Repeat Steps 3 and 4 until your template is complete.
Preview Your Template
Click the “Preview” button to see what the template will look like to families in your patient portal.
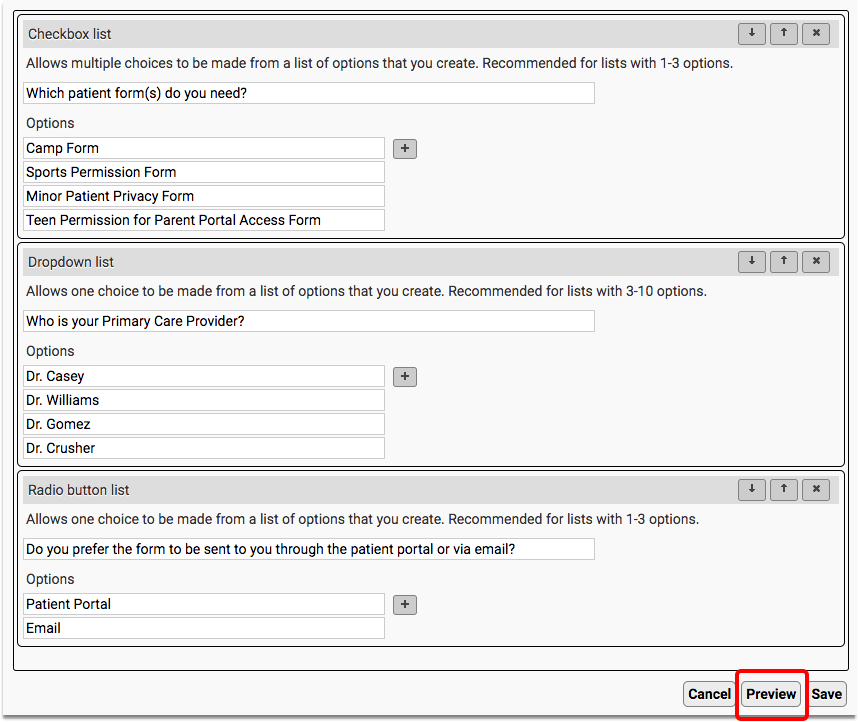
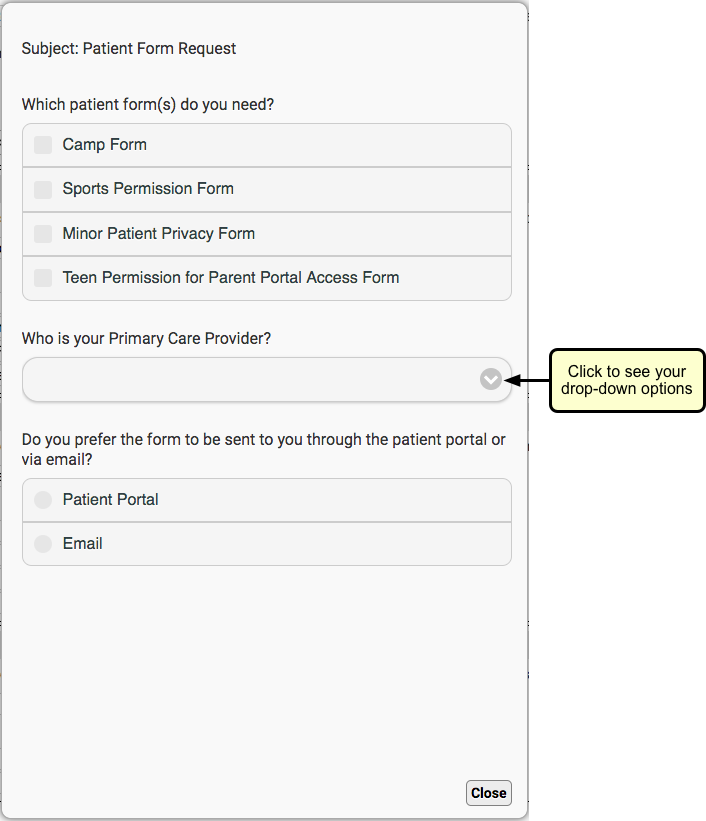
Click “Close”. Make any changes needed.
Click “Save”
When you are satisfied with your template, click “Save”.

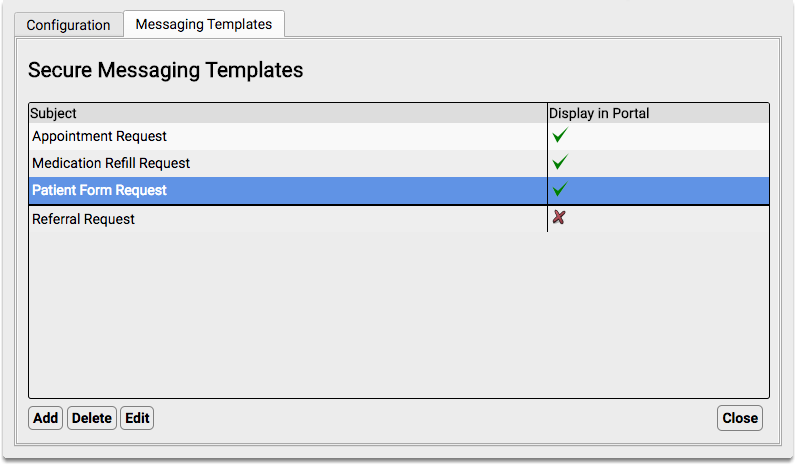
You will see your new template in the Secure Messaging Templates list.
Portal Message Template Field Reference
The following field types can be used when creating new portal message templates. Several of them also appear in the default portal message templates provided with PCC EHR.
-
Agreement: Adds the option to upload a document, such as a policy document, and the option for the user to electronically sign the document. For detailed information about this field, click here.
-
Appointment Date: Adds a Calendar selection tool to your template. The selected date will default to the current date.
-
Appointment Location: Creates a drop-down selection field that includes all of your practice’s scheduling locations. An “Any Location” option will also be included and selected by default.
-
Appointment Provider: Creates a drop-down selection field that includes all of your practice’s scheduling providers. An “Any Provider” option will also be included and selected by default.
-
Attachment: Adds the option to attach an image or PDF file, and a text field for a label.
-
Block of text: Display-only sentence or paragraph. Use this to create an introduction, instructions, or comment.
-
Checkbox list: Creates a list of custom checkbox items. Any or all of the options may be selected. None of the boxes will be checked by default.
-
Dropdown list: Creates a drop-down selection field where one choice can be made from a list of options you create. PCC recommends using this field type for lists with three to ten options. The field will be blank by default.
-
Input box-large: Creates an expanding entry field within which the portal user can input several lines of text. This field type is recommended when you want a sentence or paragraph length answer.
-
Input box-small: Creates an entry field within which the portal user can enter one line of text. This field type is recommended when you want a one-word or short answer.
-
Medication Allergies: Displays a bulleted list of the patient’s active medication allergies, followed by radio buttons for the portal user to verify the allergies or provide updates. If the portal user indicates that the list needs updating, an entry field will appear in which they can enter comments. Nothing will be automatically updated; the updated information will need to be manually added to the patient’s chart.
-
Medication To Refill: Displays a checkbox list of active medications from the patient’s Medication History. Any or all of the options may be selected. None of the boxes will be checked by default. Additionally, entry fields are included for the portal user to record additional medications they want refilled, and the name and location of the pharmacy they want to use.No prescriptions will be automatically generated; a prescriber will need to manually create the medication refill, if appropriate.
-
Radio button list: Creates a radio button selection field where one choice can be made from the options you create. Nothing will be selected by default.
-
Title: Display-only larger sized bold text. Use this to create a form title and for section headings.
Send and Receive Direct Secure Messages
When you need to send a secure message to another provider, or a hospital needs to send you patient records, you can use Direct Secure Messaging–a communication technology used to exchange private medical information. You can send your message, along with a Summary of Care Record, directly to a specialist, another pediatrician, or other healthcare provider.
Read the procedures below to learn how to exchange Direct Secure Messages with other healthcare providers.
Setup and Configuration Needed First: Before you can send and receive Direct Secure messages, your practice must activate the feature and you must register an account. Read Get Started with Direct Secure Messaging to learn how.
Watch the Video: Watch Send, Receive, and Reconcile Direct Secure Messages to learn how to send, receive, and reconcile direct secure messages on your PCC system.
Send a Direct Secure Message to Another Healthcare Provider
Read the steps below to learn how to send a message, along with a Summary of Care Record (C-CDA), using Direct Secure Messaging.
Open a Chart and Select the Summary of Care Record Report
When you wish to send a Direct Secure Message, first open a patient’s chart.
Then select the “Summary of Care Record” from the Reports menu.
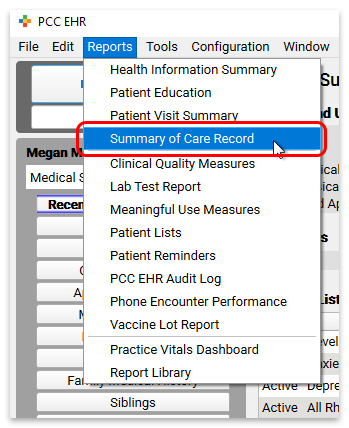
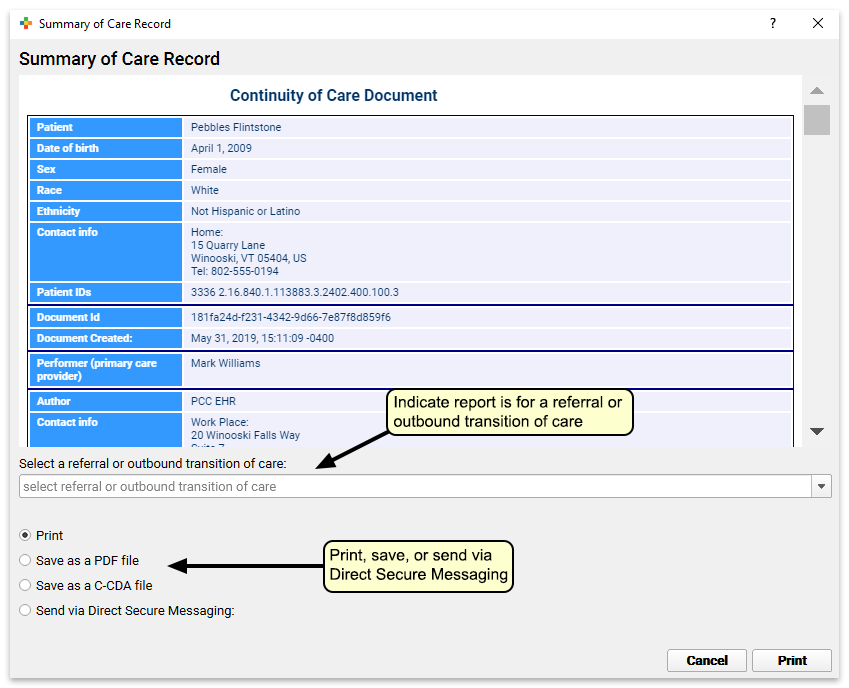
Optional: Indicate Whether the Message is For a Referral or Transition of Care
On the report’s criteria screen, you can indicate whether or not you are creating the record for a referral or transition of care.
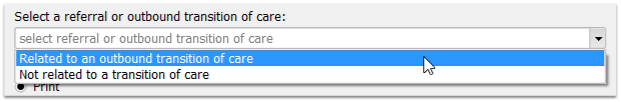
Transition of Care For Meaningful Use: If you have indicated that the record is being created for a referral or transition of care, PCC EHR will track that you have generated the C-CDA document and it will update your Meaningful Use reporting totals.
Optional: Limit Record to a Specific Encounter
When you are sending a Direct Secure Message for a referral, you can select a specific referral and optionally limit the record you send to information from that referral encounter. Choose the specific referral order from the selection pull-down menu.
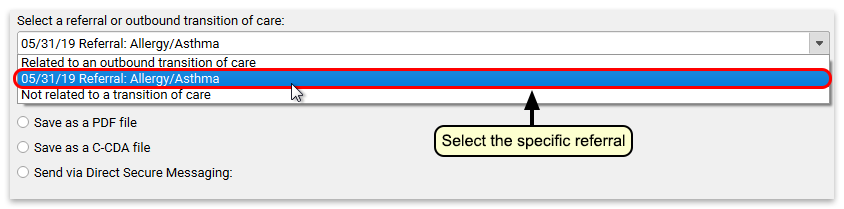
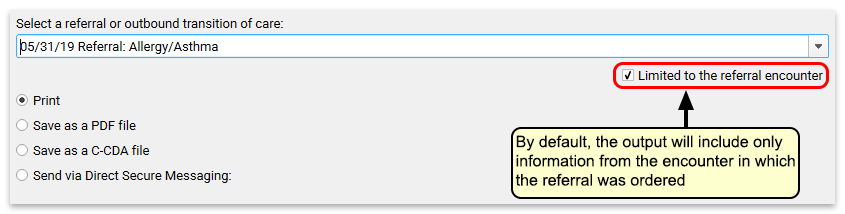
The Summary of Care Record transmitted with the Direct Secure Message will be limited to procedures, orders, and vitals noted for that given encounter date. (Along with the patient’s Problem List, insurance policies, and some other chart information not specific to a particular encounter.) Optionally, you can deselect the “Limited to the referral encounter” check box, and the Summary of Care report will generate the patient’s complete C-CDA with all available patient information.
Select ‘Send via Direct Secure Messaging’
Click “Send via Direct Secure Messaging” and then click “Send to…” to indicate you wish to send a Direct Secure Message.
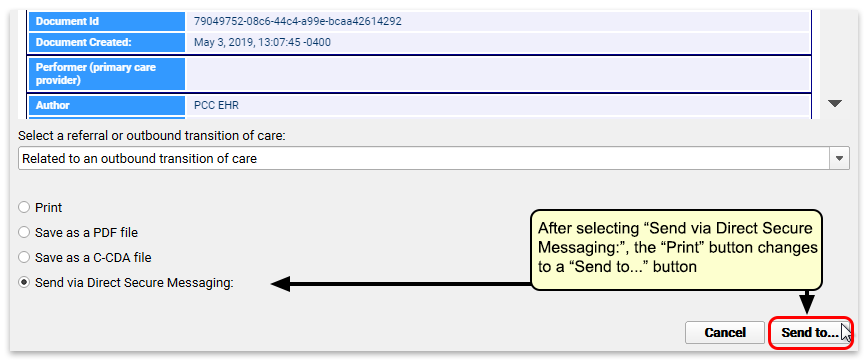
Enter a Direct Address, or Search for One
Enter the care provider’s Direct Address (not their e-mail address) into the “To” field. Optionally, you can search by provider or practice name.
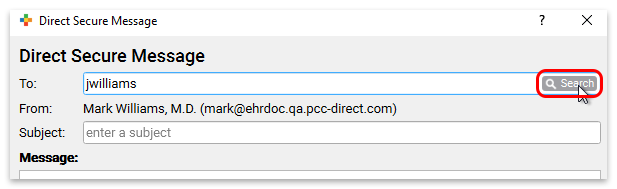
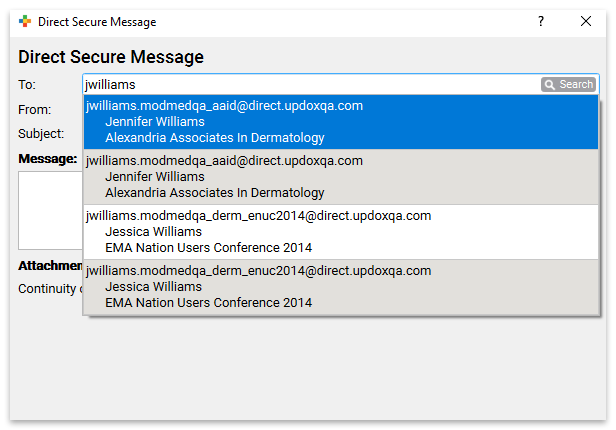
You will see more results if a user at your practice is registered with the DirectTrust network (learn how). PCC EHR also displays search results from contacts your practice has entered into the Professional Contact Manager–those results will appear at the top of your search.
Type a Subject and a Message, and Click “Send”
Finally, enter an explanatory subject and message text for your Direct Secure Message. Optionally, you can attach files or documents from your workstation or from the patient’s chart. When you are finished, click “Send” to send the message along with the patient’s care record.
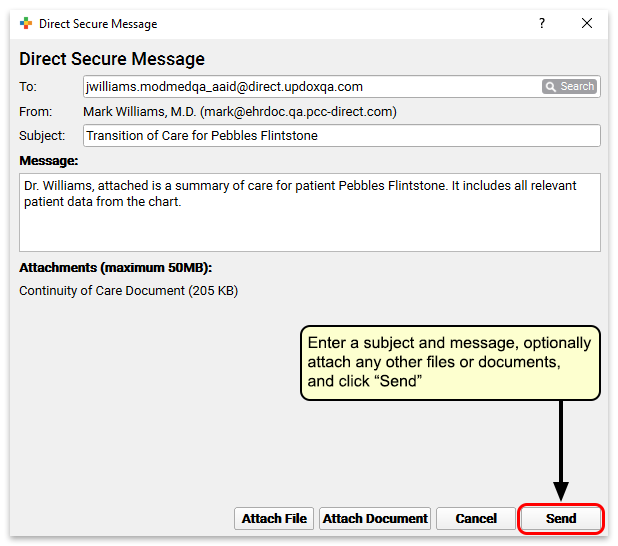
Attach a Patient Document to a Direct Secure Message
You can use the “Attach Document” button to attach any documents associated with the patient to a Direct Secure Message.
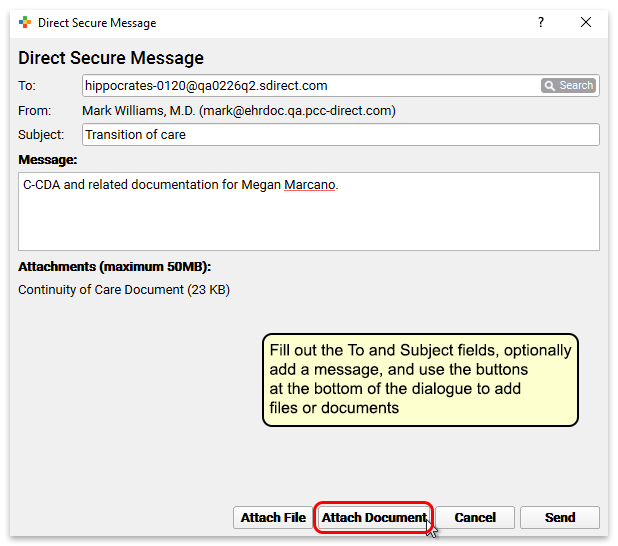
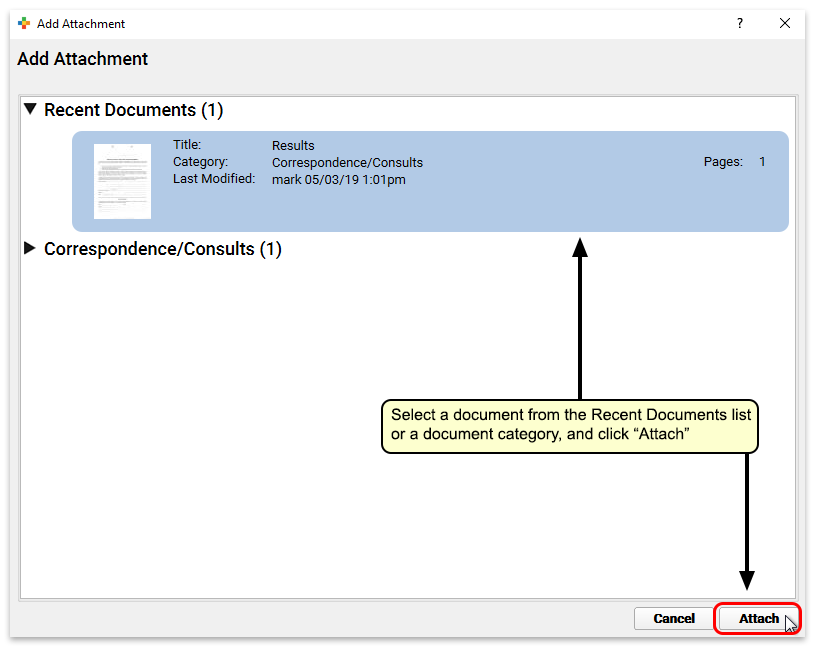
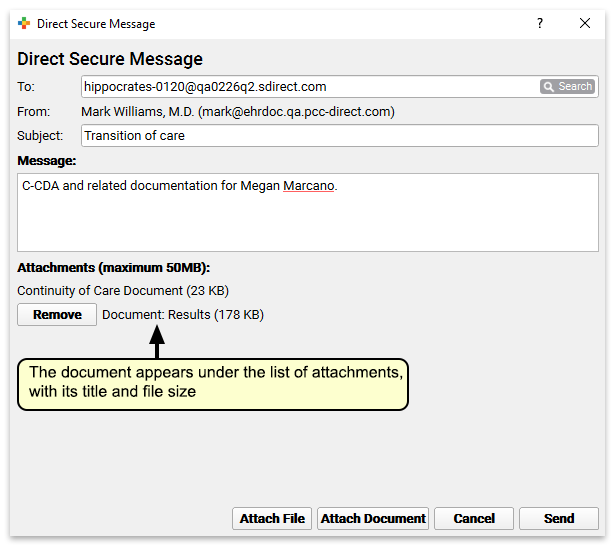
Attach a File to a Direct Secure Message
Use the “Attach File” button to attach any file from your workstation to the message.
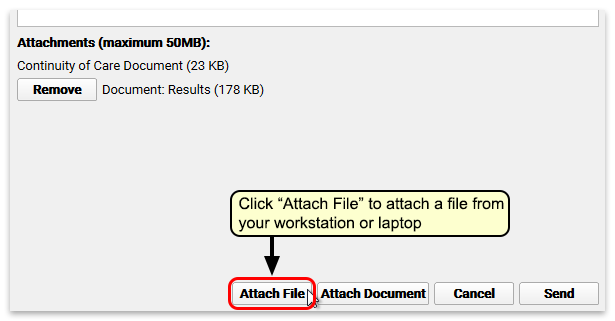
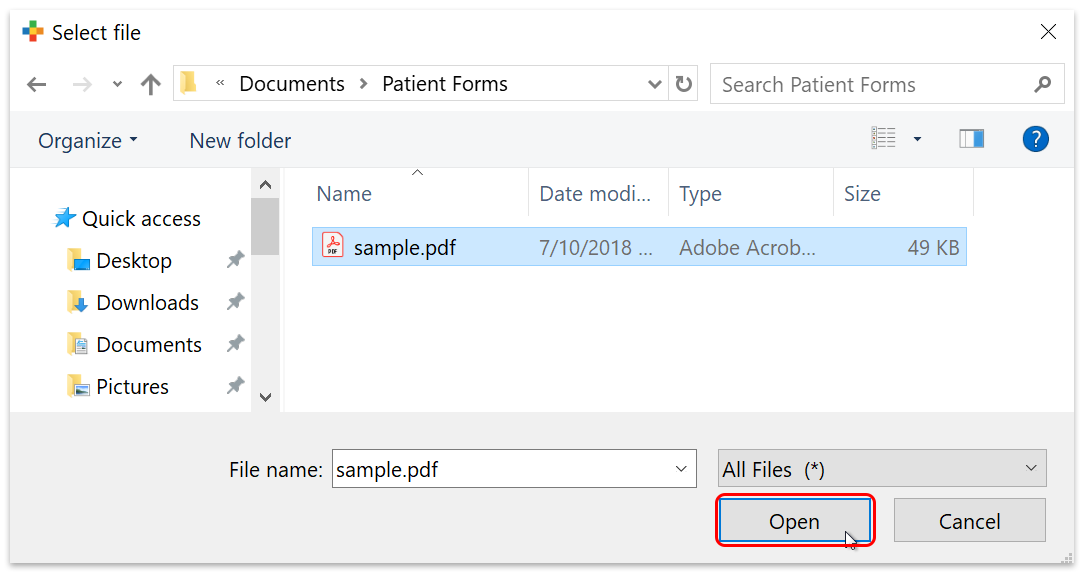
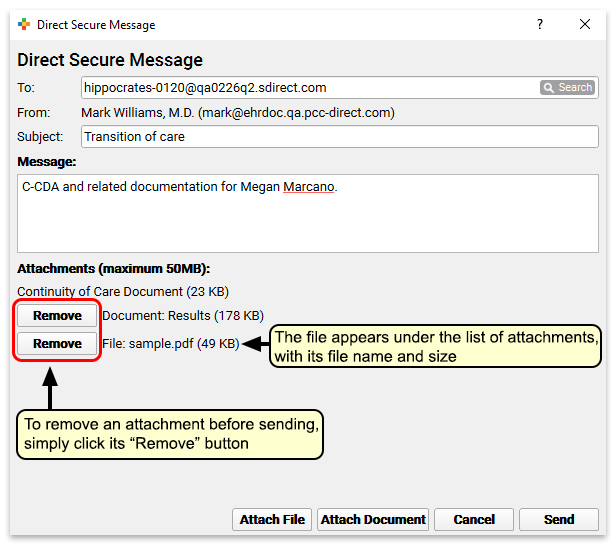
Size Limit and Removing Attachments: Before you send the document you have the option to remove any attachments you may have selected. Direct Secure Messages have a 50MB size limit; if you try to send a message that is too big, you will be prompted to remove attachments.
Receive a Direct Secure Message and Add It to a Patient’s Chart
Once your practice has activated Direct Secure Messaging (learn how), other medical practices can send Direct Secure Messages to users at your practice. Those messages can include transition of care C-CDA attachments and other documents.
When a Direct Secure Message arrives, it will appear on the Messaging queue. Double-click on a message to review it and associate it with a patient chart.
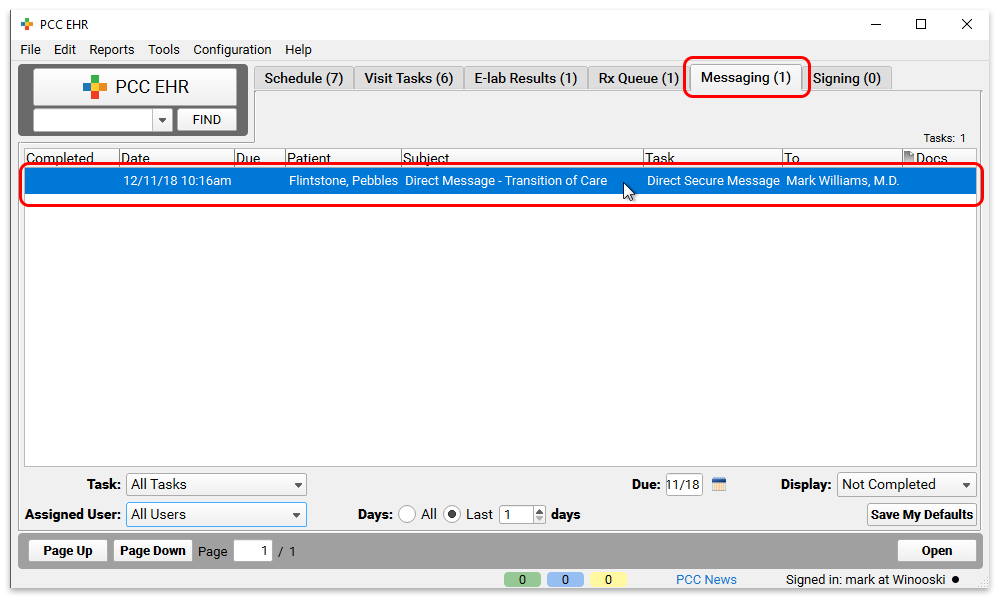
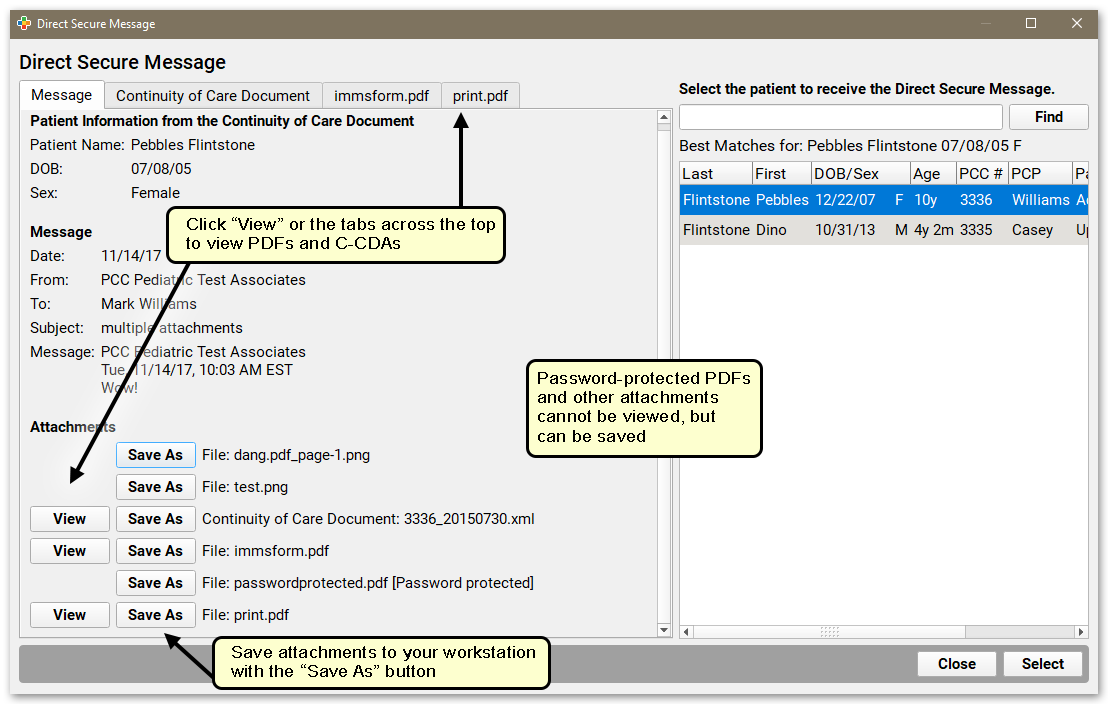
Similar to the process for importing an electronic lab result, you can review message information, including patient name, birthdate, and sex, and message details, if available. You can view PDF, Continuity of Care documents, and the contents of zipped attachments, and optionally save any attachments to your workstation. Use the panel on the right to associate the message with a patient’s chart. In most cases, PCC EHR does the work for you and suggests a matching patient. Otherwise, you can search for any patient.
Click “Select” to place the Direct Secure Message into the patient’s chart.
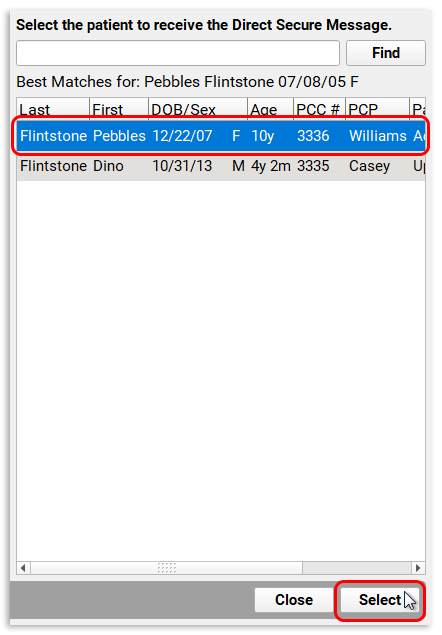
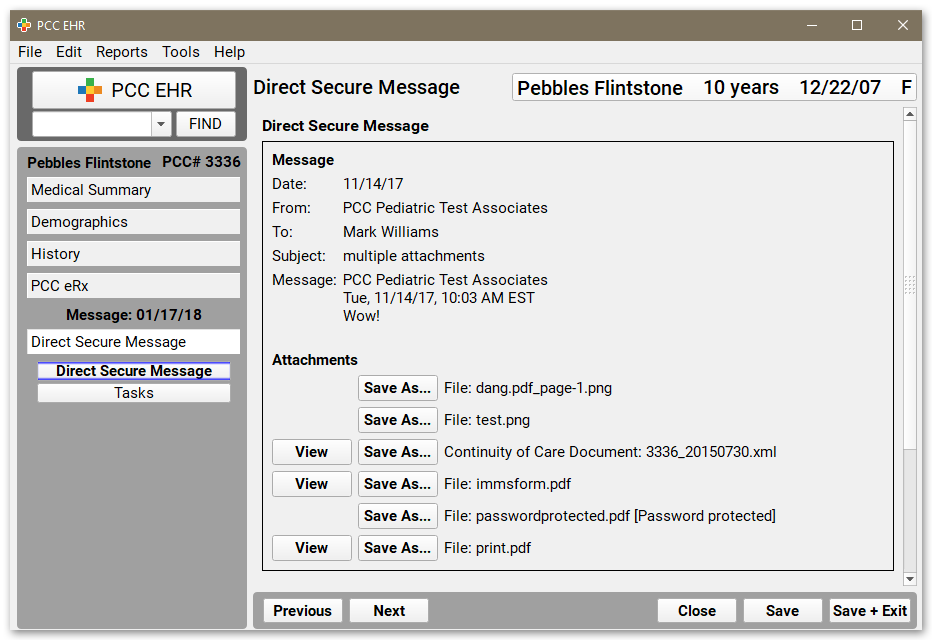
After you click “Select”, PCC EHR will open the Direct Secure Message as it appears in the patient chart. You can see the full message details and any attachments.
Add a Custom Summary to a Direct Secure Message
After a Direct Secure Message is placed in a patient’s chart, you can optionally write your own summary of its contents. Custom summaries appear in place of the message subject in the patient’s Visit History.
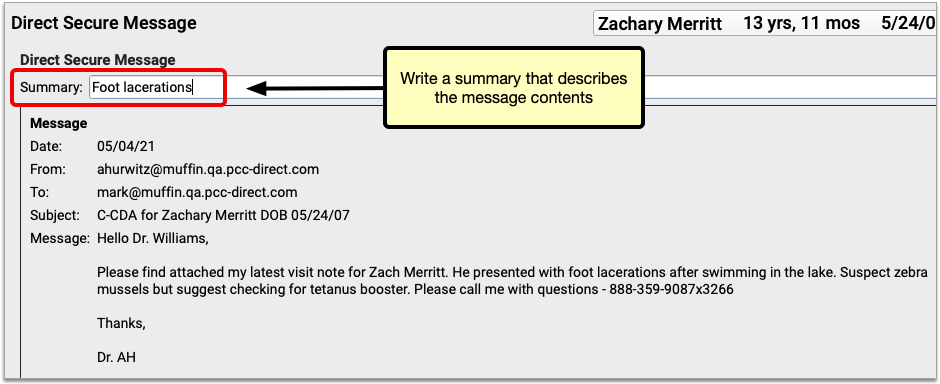
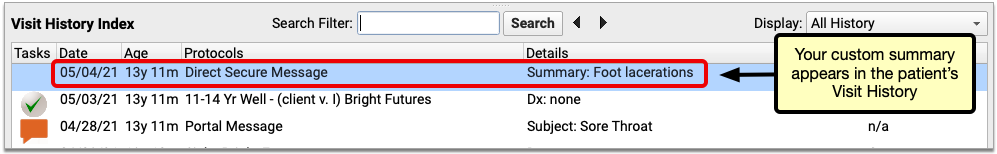
You can edit the summary of a Direct Secure Message at any time.
Review and Work With a Direct Secure Message
After a Direct Secure Message is placed in a patient’s chart, it appears in the Visit History. You can review it as you would a chart note or phone note.
As you review a message, you can click to open message attachments and create and complete tasks. For example, you can click “View” to view a C-CDA document or other attachment.
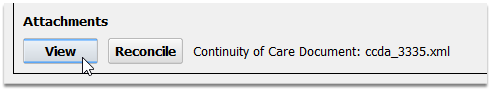
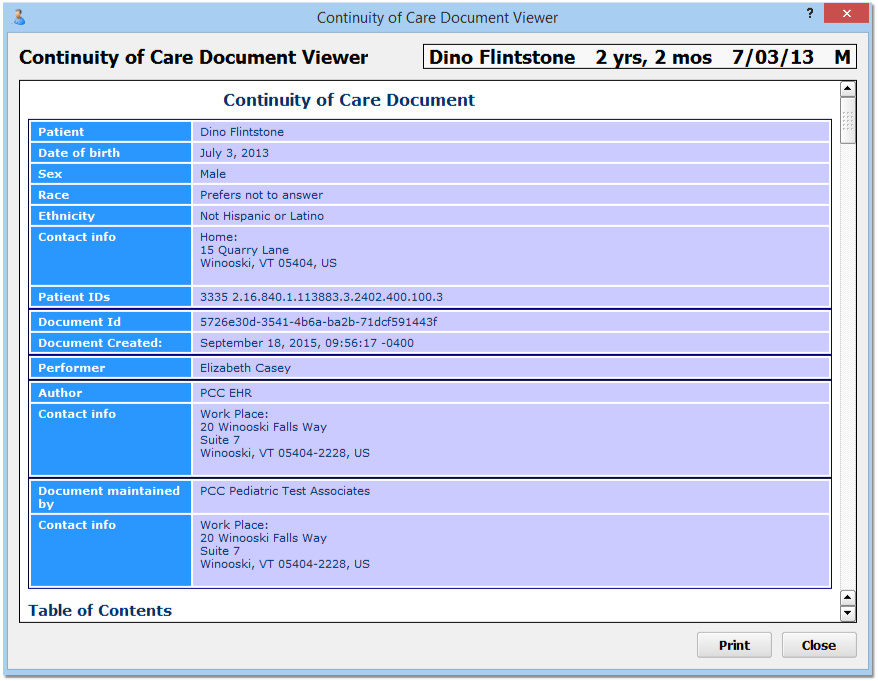
You can also create a task for any user so they can follow up on the message.
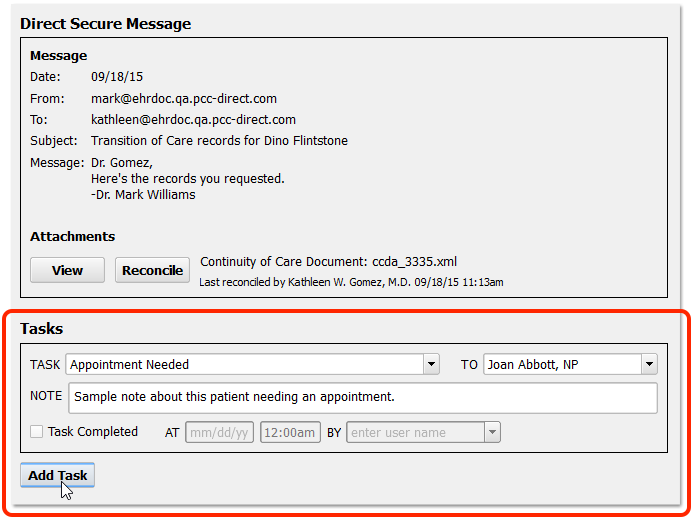
Reconcile a C-CDA Document
If a Direct Secure Message includes a transition of care document in C-CDA format, you can import any Problems, Medication Allergies, and Medications from the C-CDA document into the patient’s chart record.
When you see an incoming C-CDA in a Direct Secure Message, you can click “Reconcile” to review and import patient data.
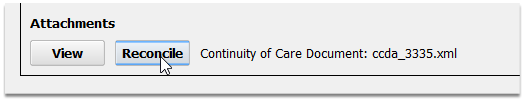
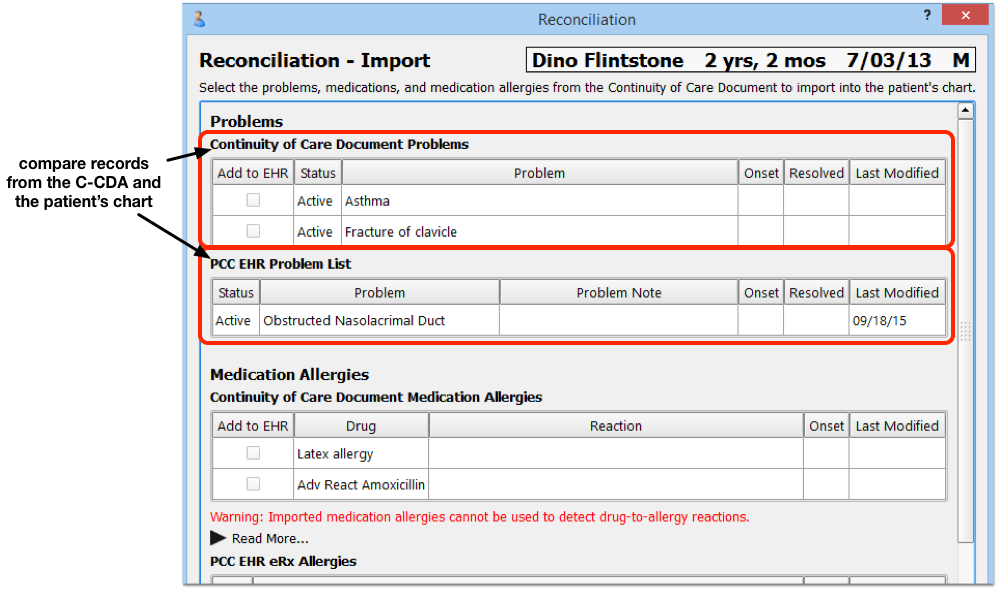
On the “Reconciliation – Import” screen, you will see three sections: Problems, Medication Allergies, and Medications. In each section, you will see both the information in the C-CDA and the information that is already in the patient’s chart. When you want to import information, select it in the “Add to EHR” column.
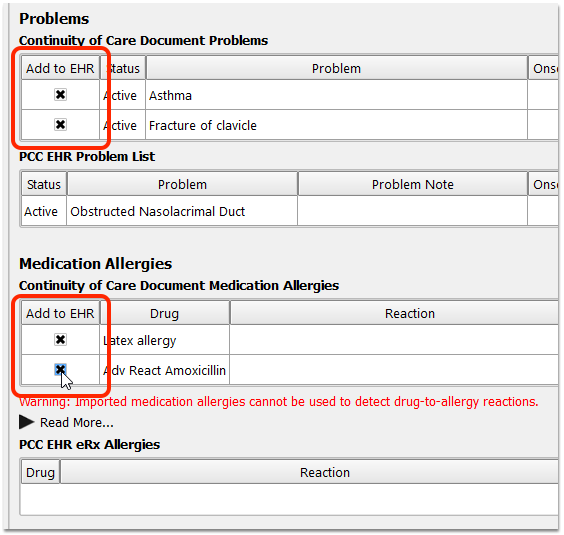
After you have reviewed each section (Problems, Medication Allergies, and Medications) and selected any items you wish to add to the patient’s chart in PCC EHR, click Next.
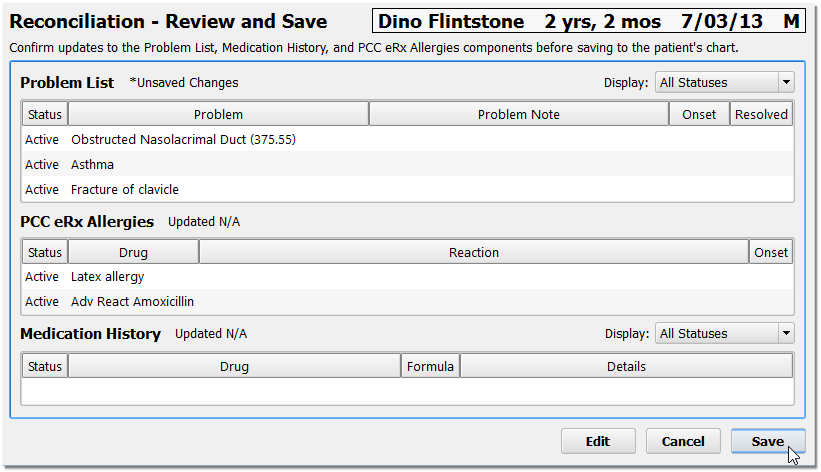
On the “Reconciliation – Review and Save” screen, you can review what the final result of the patient’s record will be. You will see what the patient’s new Problem List, PCC eRx Allergies, and Medication History will display after the import is complete.
Optionally, Click Edit: You can click “Edit” and modify the items on these lists before saving. If you have a duplicate entry, for example, you may want to edit and combine notes or delete an item.
Click “Save” to save your changes and import the data. You can also click “Cancel” to close the C-CDA without making any changes to the patient’s chart.
Last Reconciled: PCC EHR tracks when a user clicked the “Reconcile” button, whether or not they decided to import data to the chart. You will see a “Last Reconciled” attribution on the Direct Secure Message as well as in the patient’s Visit History. You can revisit the message and choose to reconcile the C-CDA data with the patient chart again at any time.
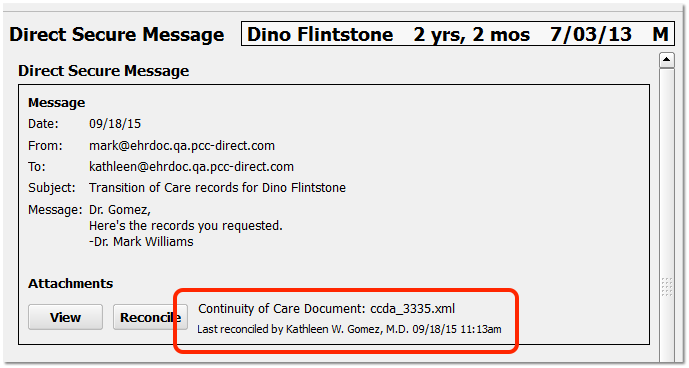
Check Imported Medications and Medication Allergies in PCC eRx
When you reconcile and import medications and medication allergies from a C-CDA, PCC eRx attempts to match each drug description with a known item in its database. Where a match is found, drugs are added to the Allergies and Medication History components in PCC eRx in such a manner that they participate in drug safety checking. Where no match is found, drugs are added as free text. Free text entries are denoted by a pill bottle icon with a question mark and do not participate in drug safety checking.
In order to facilitate the safest possible e-prescribing, PCC recommends that you check for free text entries after reconciling a C-CDA and recreate them as items that can participate in drug safety checking. Use the “Add New Allergy” button in the Allergies component to recreate medication allergies imported as free text. Use the “Add Hx Med” button in the Medication History component to recreate medications imported as free text.
Once you have recreated imported free text entries as items that are able to participate in drug safety checking, you can delete the original free text versions from the patient’s record.
Remove a Direct Secure Message from the Incorrect Patient’s Chart
If you accidentally attach a Direct Secure Message to the wrong chart, you can un-attach it and send it back to the queue.
From the Visit History, double-click to open a Direct Secure Message.
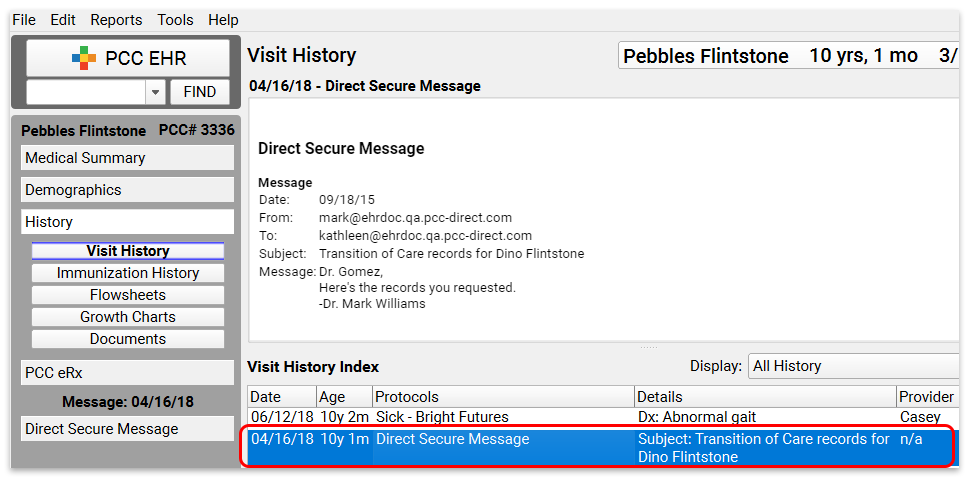
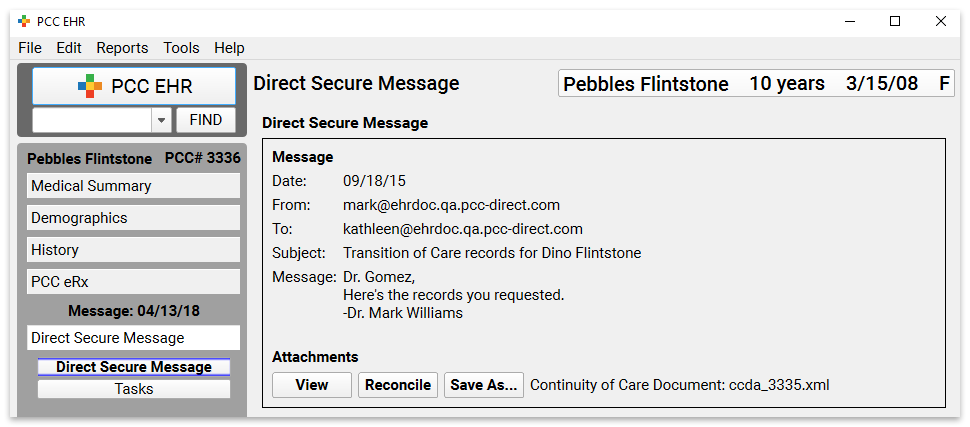
While viewing the Direct Secure Message protocol, select “Remove Direct Secure Message” from the Edit menu and then click “Remove”.
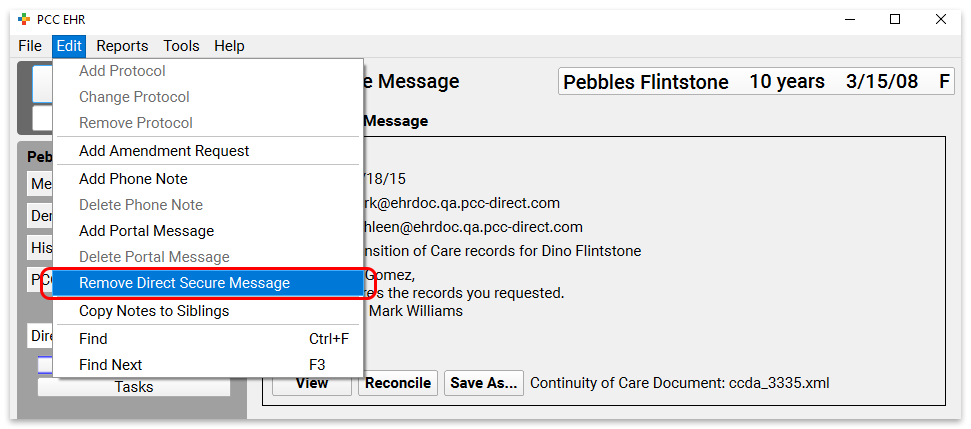
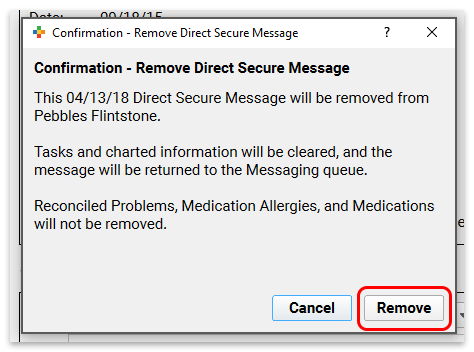
Reconciled Items: If your practice reviewed the Direct Secure Message and reconciled Problems, Medication Allergies, or Medications, they will not be removed by the above process.
The Direct Secure Message will now appear back in the messaging queue, where you can import it to the correct patient’s chart.
Patients and Families Can Send Direct Secure Messages in the Patient Portal
Once your practice has activated Direct Secure Messaging, your patients and families can use the patient portal to send their own visit summary directly to other physicians and medical practices. They can use your practice’s Direct Secure Messaging connection to send the visit summary directly to another Direct Secure Messaging user.
When users want to save or send a visit summary in C-CDA format, they first select the patient and visit from their history.
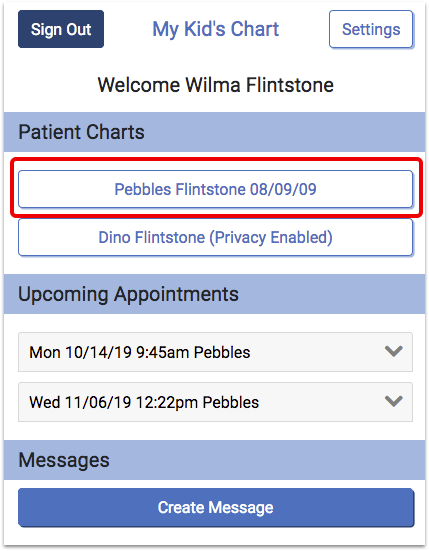
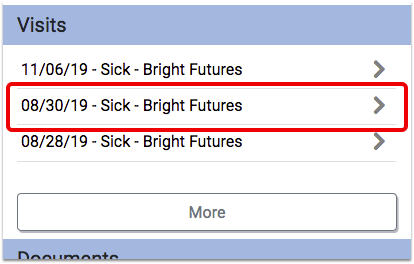
At the bottom of the visit, they can choose to download or send the visit summary.
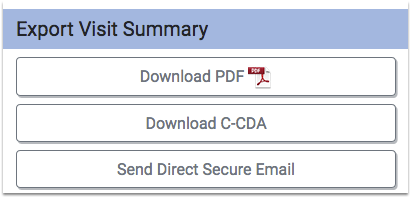
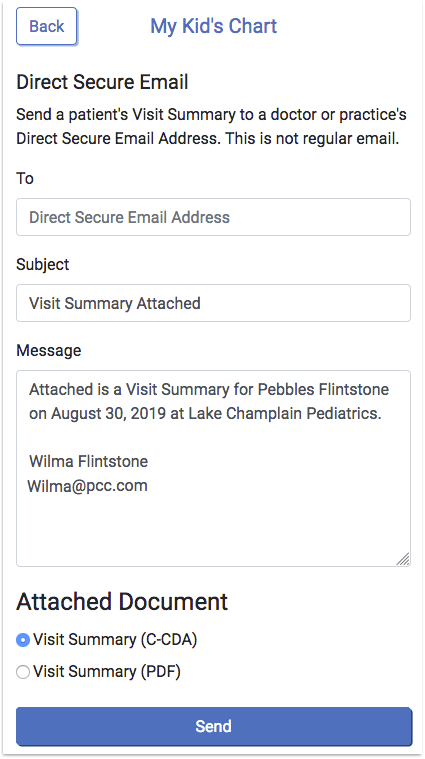
On the Direct Secure Email screen, the user can enter the Direct Secure Messaging address provided by the recipient. For example, a specialist might provide a parent with an address for the purpose of sending a visit summary directly to them.
After they enter an address, the user can optionally edit the default subject and message. Next, the user can choose whether to attach a C-CDA or PDF, and click “Send” to send the message and visit summary.
Direct Secure Messaging Required: Portal users can only send Direct Secure Messages if your practice has activated Direct Secure Messaging. Additionally, until a user at your practice registers with the DirectTrust Network, parents and families can only send messages to physicians and other practices within the Updox network. For more information, read the Get Started with Direct Secure Messaging article.
Steps to Take When a Clinician Leaves the Practice
When a clinician leaves your practice, there are certain steps that you should take to turn off their access to your PCC system, handle outstanding tasks and prescriptions, and remove them from your practice’s day-to-day workflow.
Edit the Clinician’s Account Settings
A user with access to the User Administration tool must complete the following steps.
Open the User Administration Tool and Select the Provider
In PCC EHR, open the User Administration tool and double-click on the provider who has left.
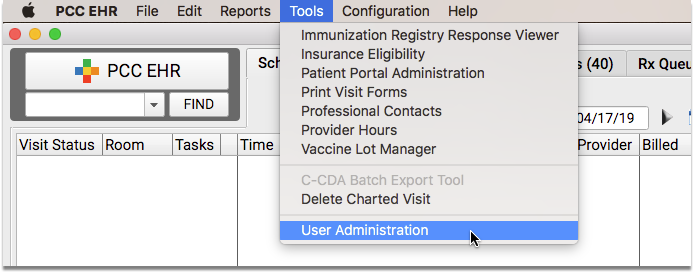
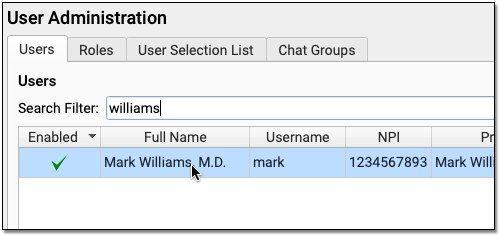
Turn Off Task Assignment and Appointment Book Scheduling
In the Account Information tab, uncheck the two checkboxes, “Tasks can be assigned to this user” and “This user is a Scheduling Provider”.
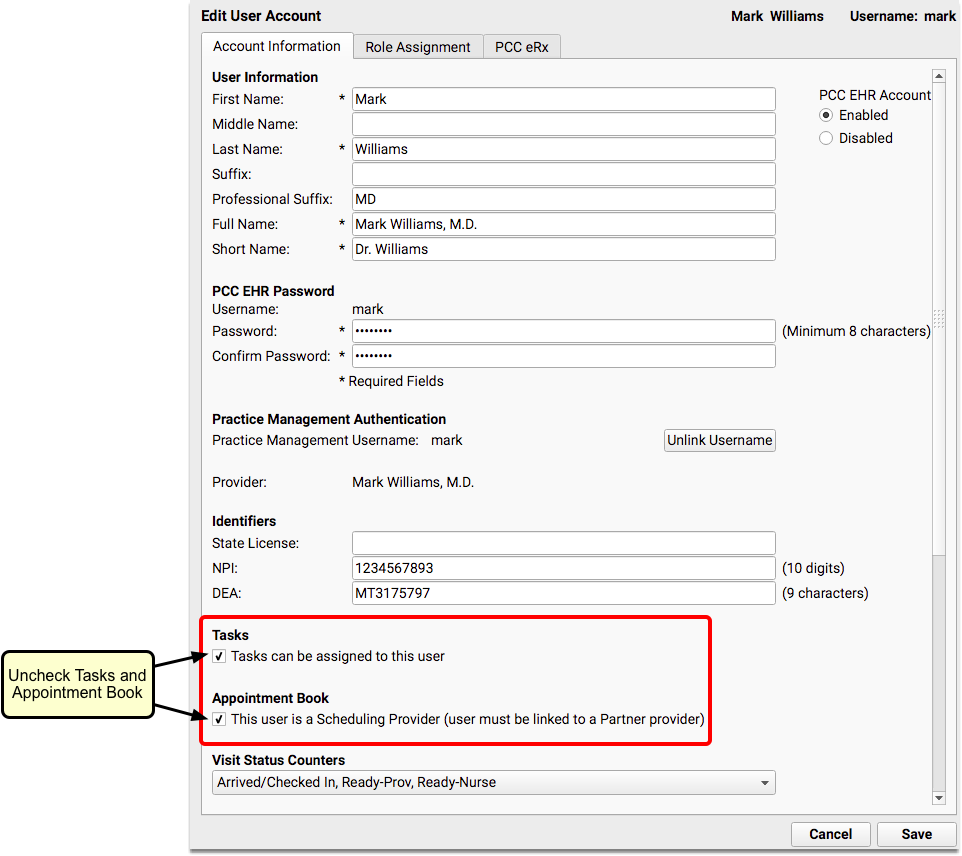
Unchecking “This user is a Scheduling Provider” will remove the provider from the Appointment Book schedule after you log out and back in.
Stop Medication Renewal and Change Requests
In the PCC eRx tab, uncheck the “Electronic Renewal Request Service” and “Electronic Change Request Service” boxes.
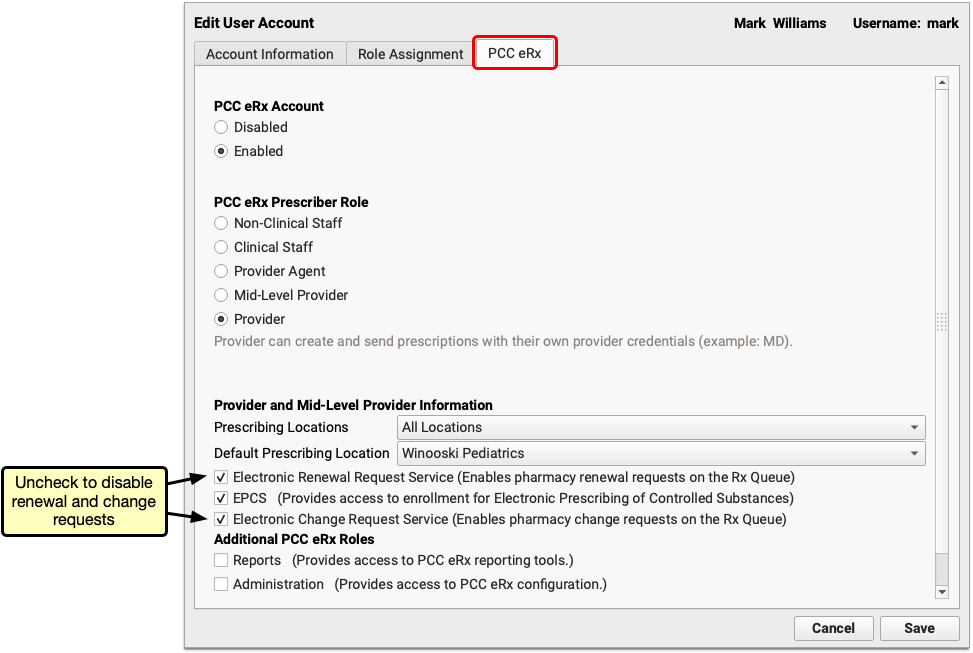
Optional: Deactivate DSM
If your practice uses Direct Secure Messaging, open the DSM tab and set the provider’s status to “Inactive”.
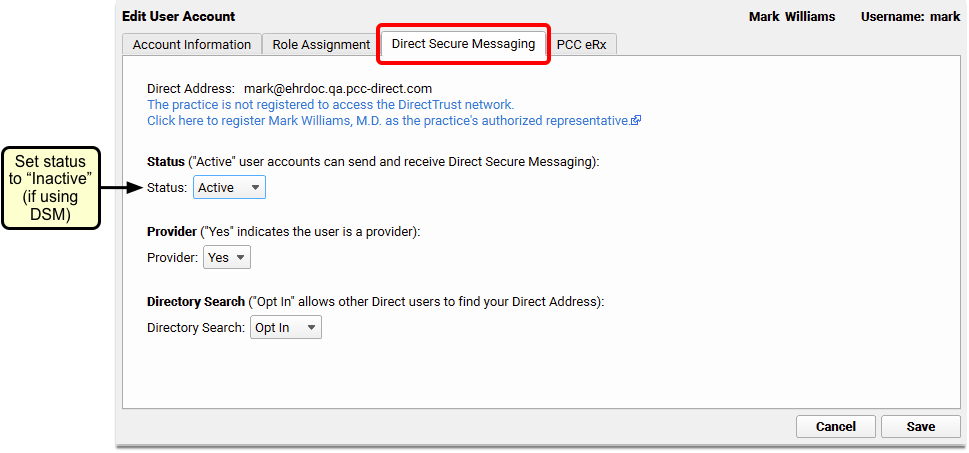
Log Out for 5 Minutes
After making the above changes, log out of PCC EHR and wait 5 minutes to give the user’s status change time to sync with the eRx system. By doing this step, you ensure that electronic prescription renewal requests sent to your practice won’t get lost in the shuffle.
Disable PCC eRx
After you’ve edited the provider’s account settings, you can move on to disabling their prescribing privileges.
IMPORTANT NOTE: Make sure you have completed the first section before you disable PCC eRx.
Log Back In
Log back in to PCC EHR (at least 5 minutes after completing the section above).
Open the User Administration Tool and Select the Provider
In PCC EHR, open the User Administration tool and double-click on the provider who has left.
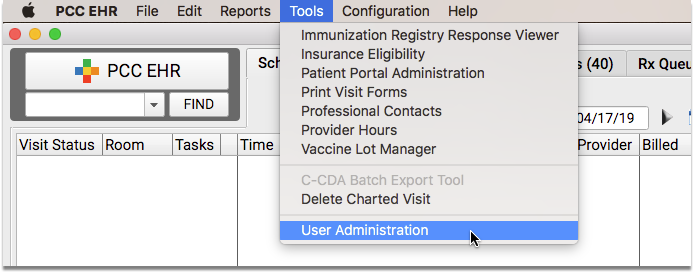
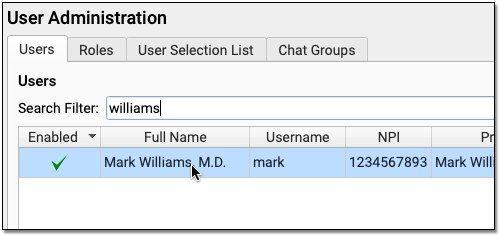
Disable eRx
In the PCC eRx tab, mark the departed user’s PCC eRx Account as “Disabled”.
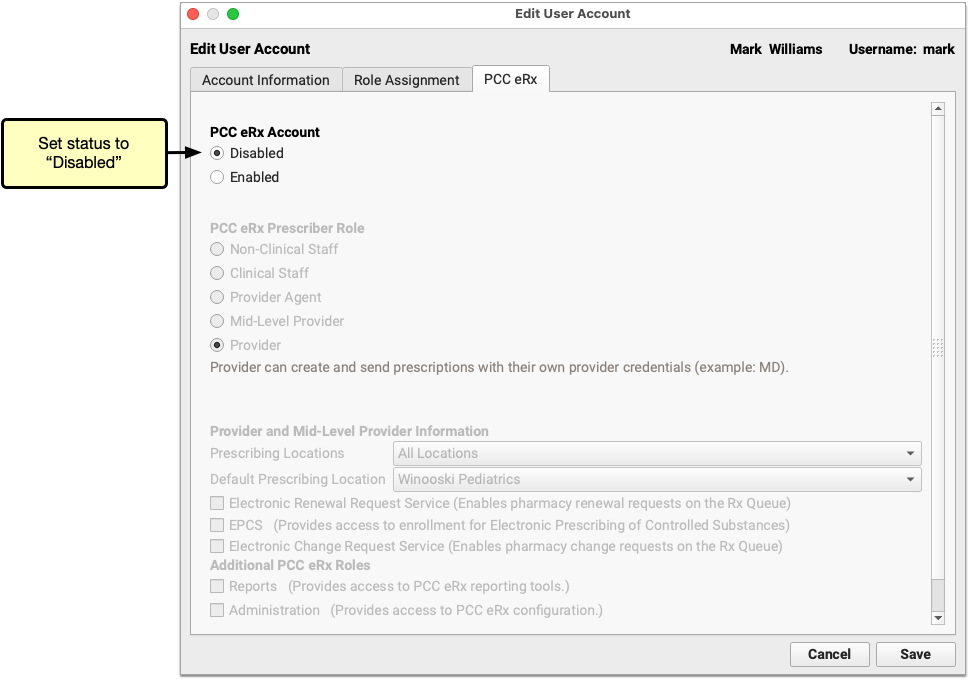
Close the User Administration Tool
Close the User Administration tool.
Reassign the Provider’s Open Tasks
Before disabling the provider’s PCC EHR account, you need to deal with the items that have been created for the provider (if any).
Check for Open Visit Tasks
Within the Visit Tasks queue, set the filters to show only tasks with a status of “Not Completed”, where the assigned user is the provider who has left.
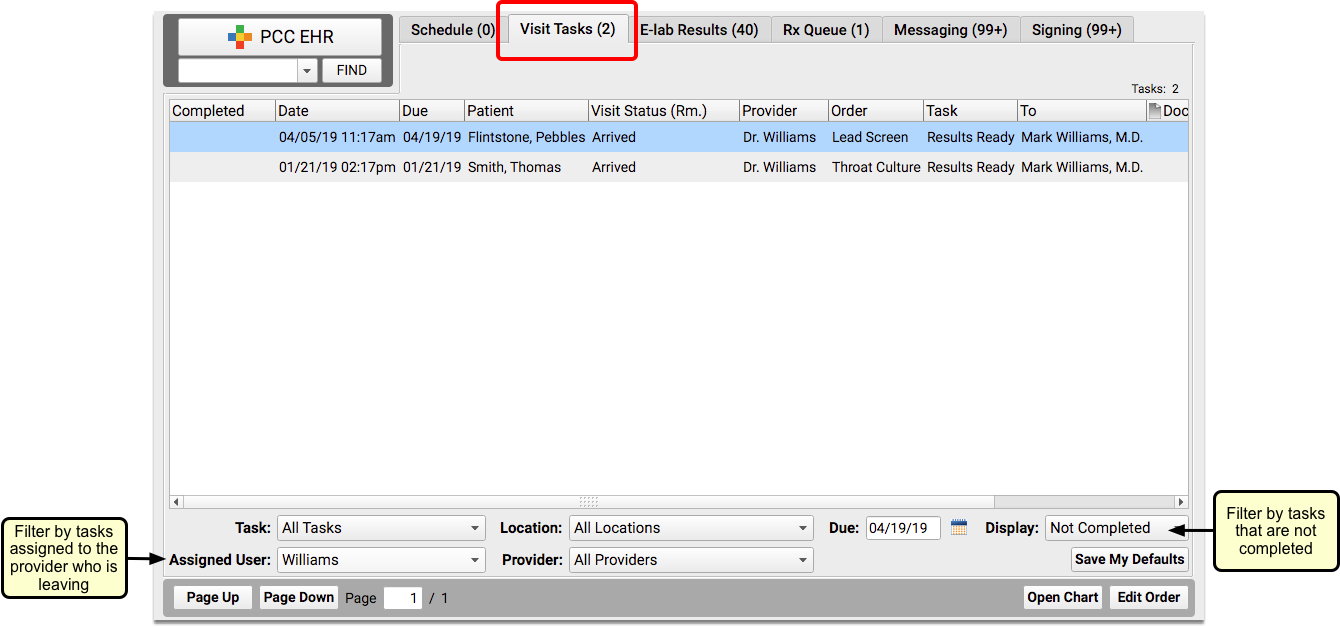
Check to see if there are any open tasks assigned to the provider.
Reassign Open Visit Tasks
Double-click on each incomplete task and assign it to a different person.
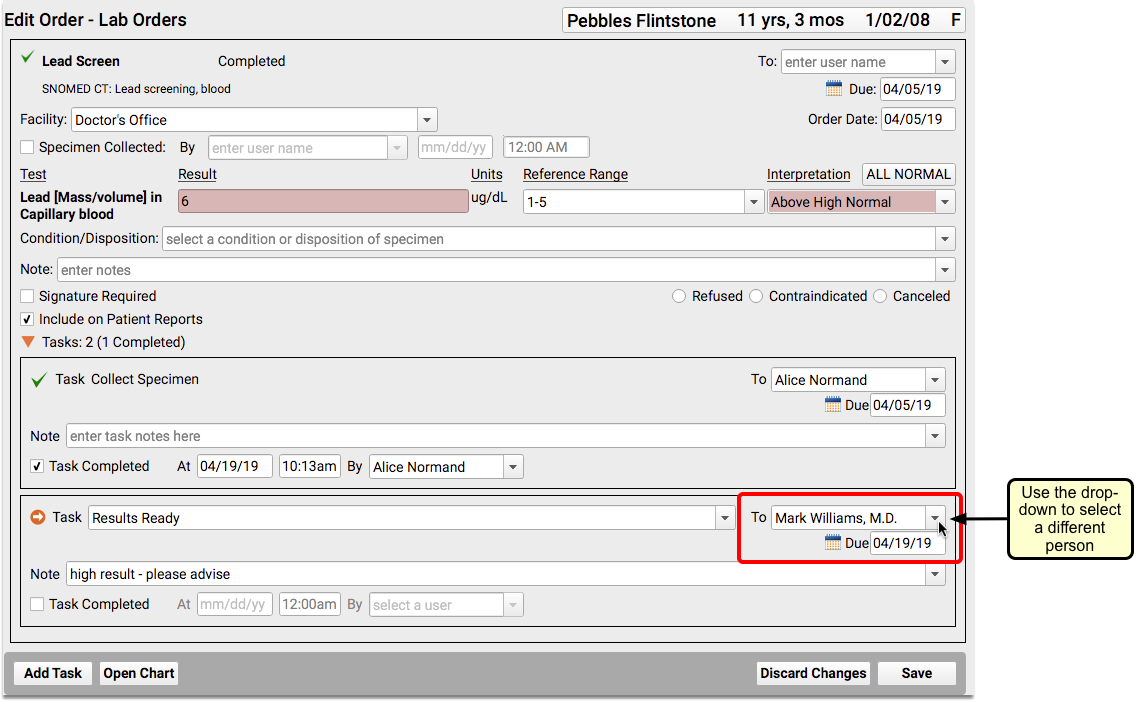
Check for Unprocessed Prescriptions, Renewal Requests, and Change Requests
Within the Rx Queue, select the provider’s name from the “Prescriber” drop-down field.
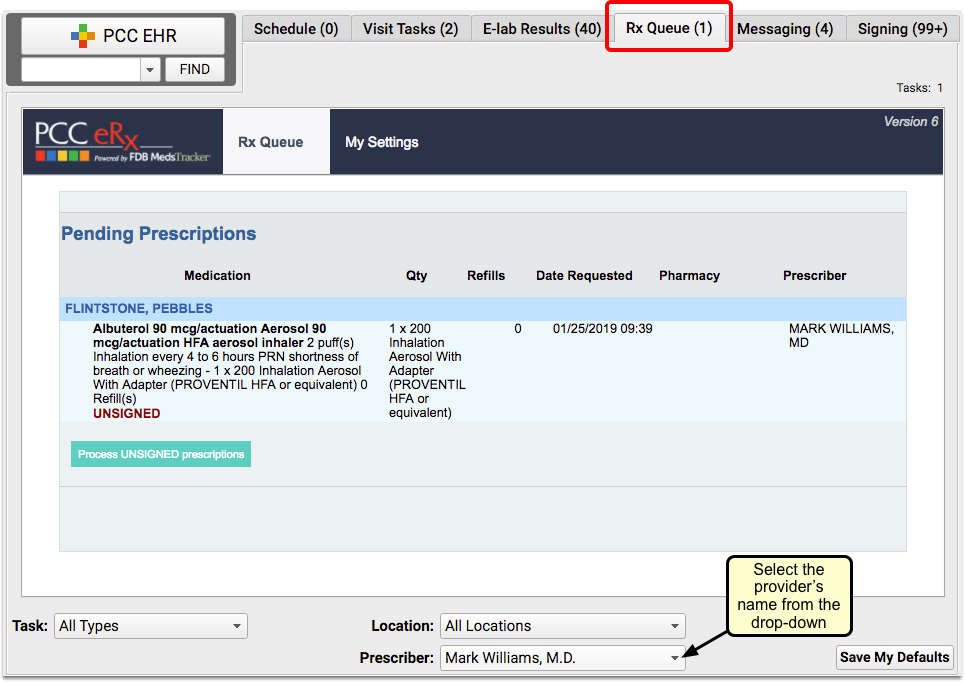
Check to see if there are any unprocessed prescriptions.
Have Another Prescriber Process the Prescriptions
If there are pending prescriptions or refill requests, another prescriber needs to approve or deny each one, with their own credentials.
Have another prescriber log in with their own user name and process the incomplete prescriptions for the provider who has left.
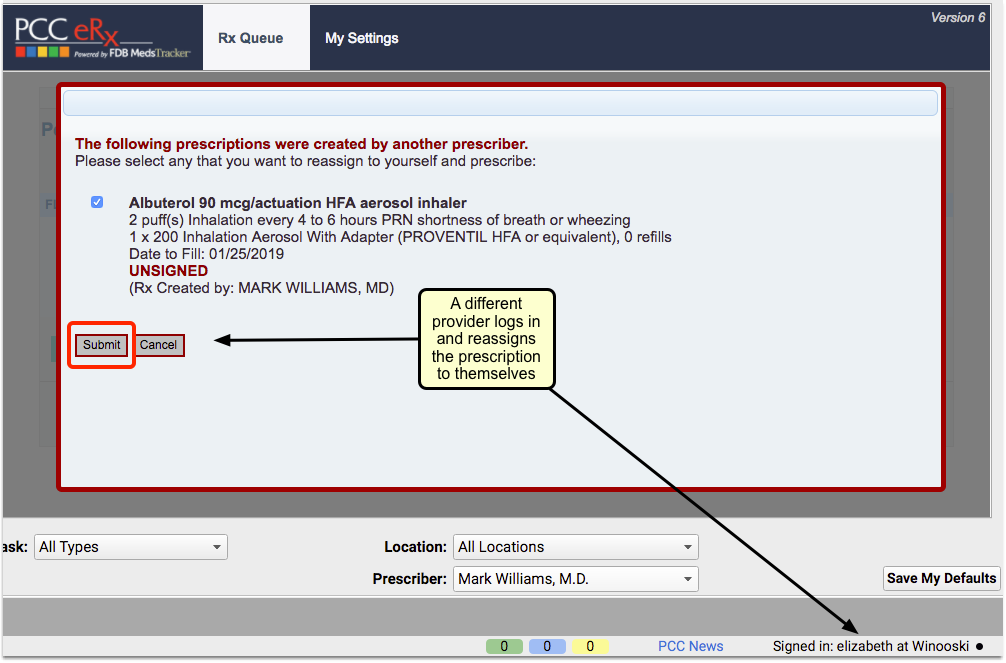
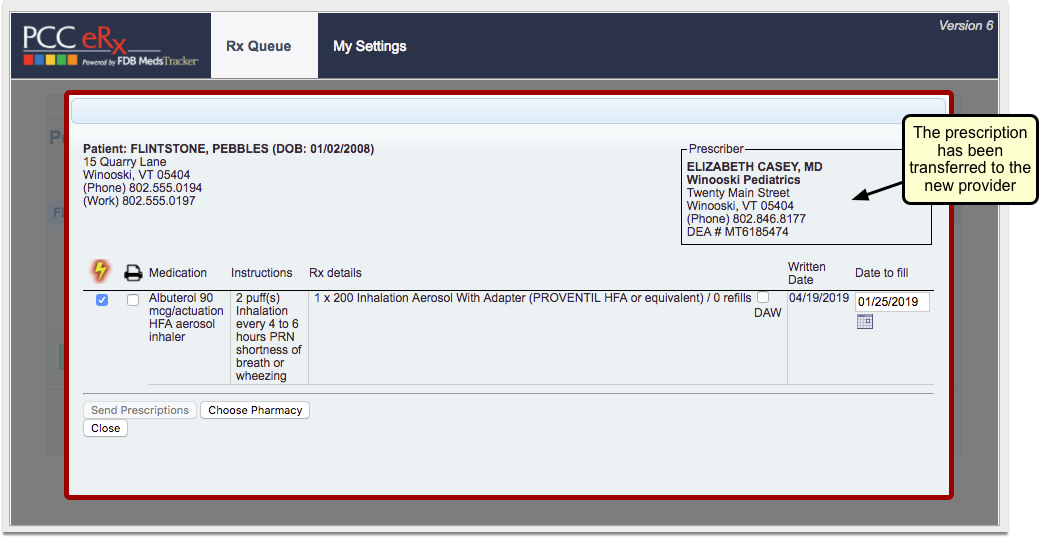
Don't Want to Prescribe for Someone Else's Patient?: There is a denial option for “Provider not associated with this practice”, which includes space for an optional note.
Check for Unsigned Items
Within the Signing queue, set the filters to show only items with a status of “Ready to Sign” for the provider who has left.
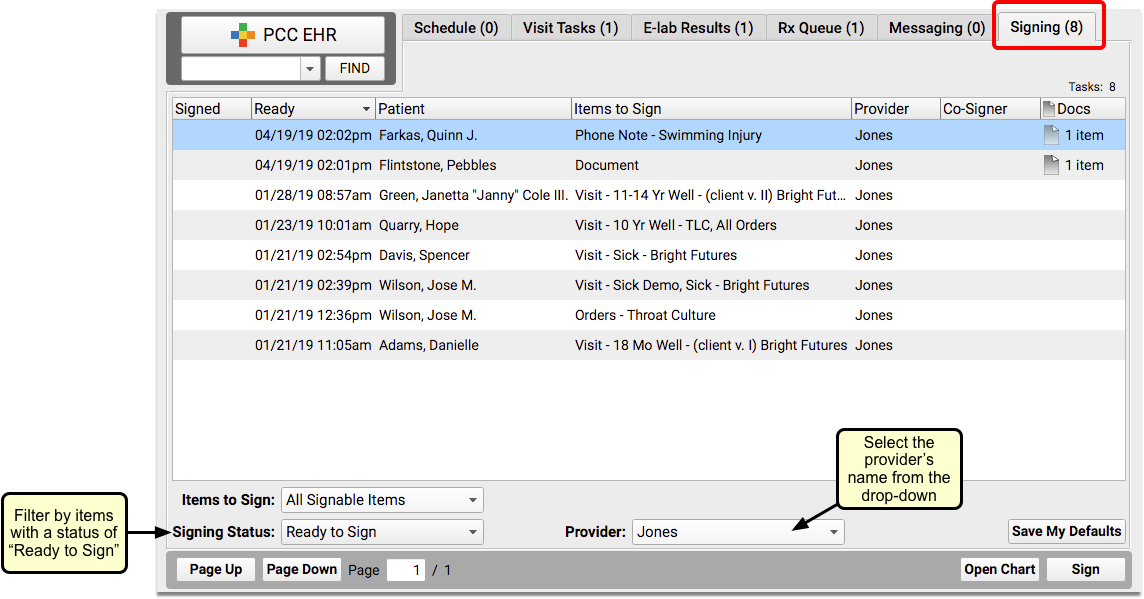
Check to see if there are any items the provider left unsigned.
Have Another Provider Sign Items Left Unsigned
If there are unsigned items, another provider with signing permissions needs to sign each one, with their own credentials.
Have another provider log in with their own user name and sign the items for the provider who has left.
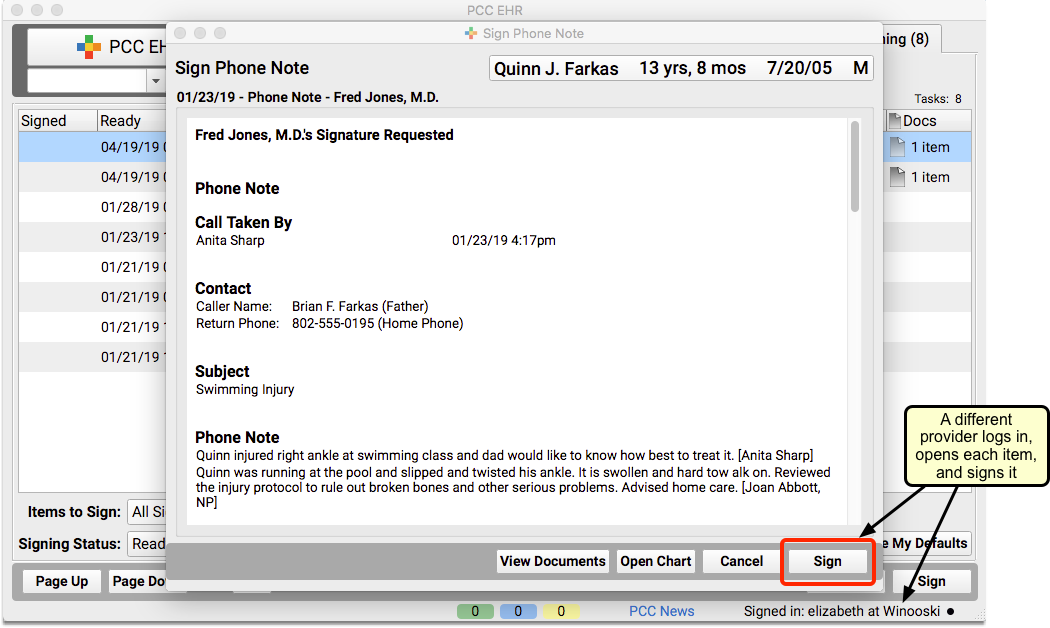
If Applicable: Reassign Direct Secure Messages
If your practice uses Direct Secure Messaging, check the Messaging queue to see if there are any Direct Secure Messages addressed to the provider. If yes, someone else will need to address any outstanding reconciliation needs.
If the provider who has left is the person who initially completed the one-time ID proofing (also known as vetted or authorized user) for Direct Secure Messaging, contact PCC Support. PCC will send you a manual link that allows a different user at the office to complete ID proofing. To learn more about Direct Secure Messaging, visit Get Started with Direct Secure Messaging.
Disable the Provider’s PCC EHR Account
Once all their outstanding items have been addressed, go back into the User Administration tool for the provider and change their PCC EHR Account status to “Disabled”.
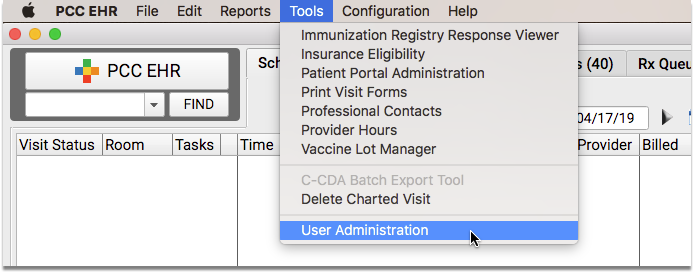
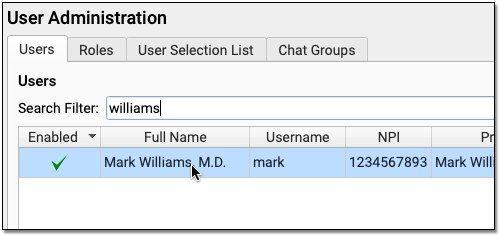
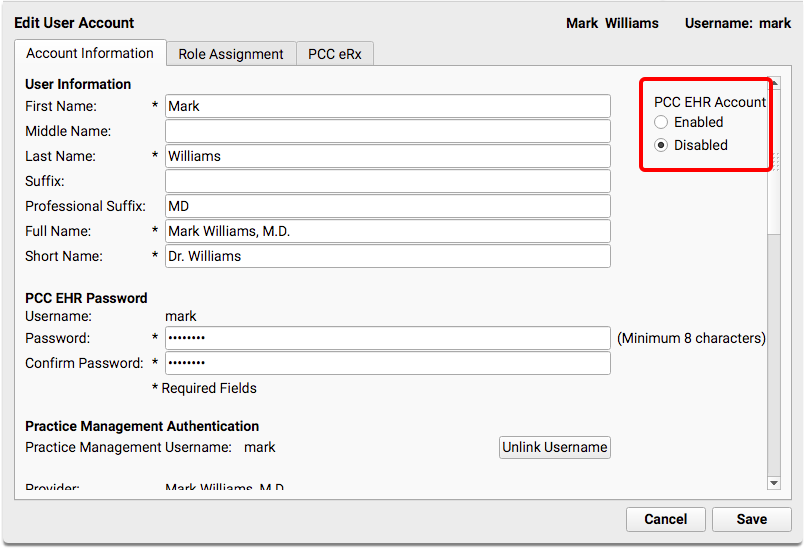
Did You Miss Anything?: If any outstanding tasks still exist for the provider, you will receive a warning that they can still be disabled, but their name will not be removed from the queue selections until their tasks have been completed.
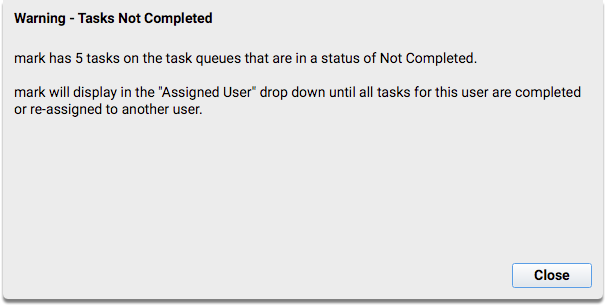
Adjust the Under-the-Hood Provider Table
After all the above steps are complete, you may also decide to hide the provider from various interfaces and reporting tools. This step is optional.
Run the Table Editor (ted) in your Practice Management window. Select the provider who has left and put a tilde (~) in front of the “Provider Name” and “Short Name” fields. This hides the provider on lists, filters, reports, and other interfaces. You can optionally mark the provider “Retired” to ensure that they do not display in the appointment book and filter lists.
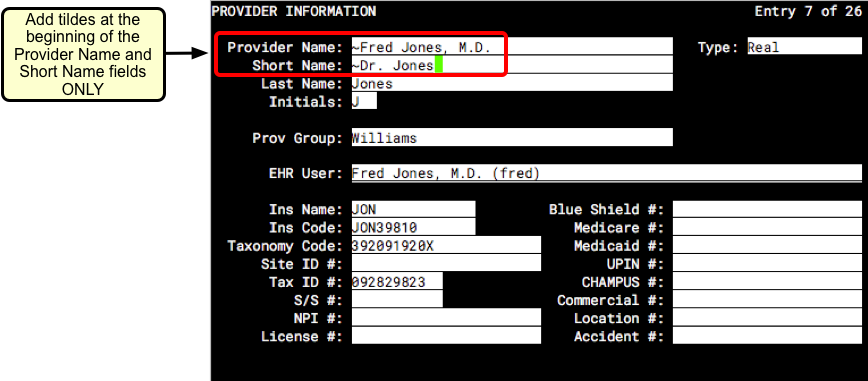
Press F1 – Save and Quit.
Leave the Last Name Field and EHR User Field As-Is: Do not change the Last Name field, as that may interfere with outstanding claim processing. Removing or changing the EHR User field will alter historical visits.
Run Reports for Patient Outreach
Want to inform patients that their provider has left the practice? You can generate a list of patients that are scheduled with that provider by running an appointment-based report such as the Huddle Sheet or Appointments report.
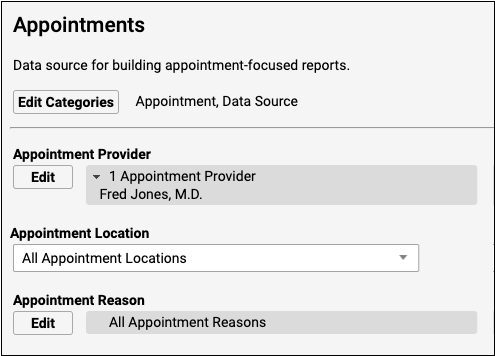
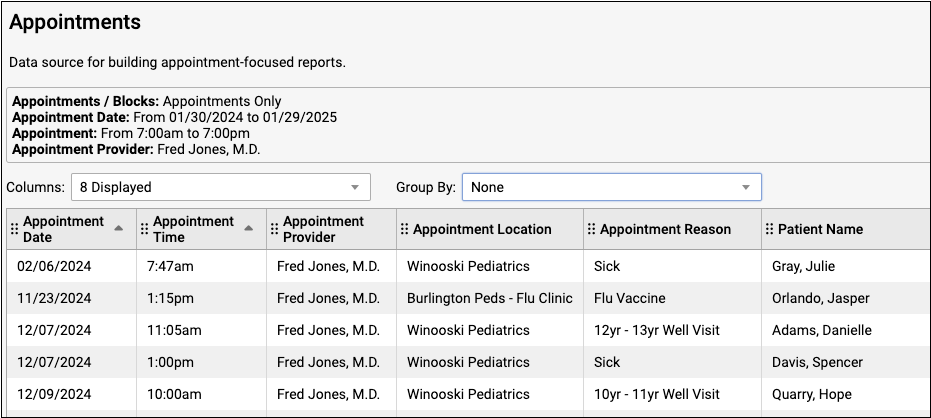
If your practice uses broadcast messaging, you can reach out to patients directly from the report output screen.

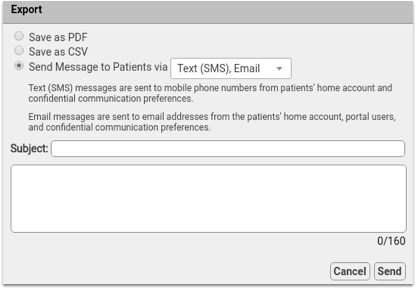
To find out more about broadcast messaging, read Send Broadcast Messages to Patients and Families.
New User Training for Billers
Use the new user training outline below to learn how to complete billing tasks in PCC.
For personalized training, help with configuration, or other needs, contact PCC Support.
Get Started
Learn how to log in, navigate in PCC EHR, and use chat.
Log In to PCC EHR
- Log In and Navigate PCC EHR
- Log In to PCC EHR
- Change Passwords and Other User Account Settings
- Connect to Your PCC System from Home
Navigate PCC EHR
Chat with Colleagues
Update Demographics and Insurance Policy Information
Work with patient and family account records and update a patient's insurance policies.
- Review and Update Patient and Family Demographics
- Update a Patient’s Insurance Policies
- Review and Update Patient and Family Demographics
- Review and Update Patient Insurance Policies
- Find Patients and Accounts
- Add New Patients and Accounts
Verify Insurance Eligibility for Encounters
You can review insurance eligibility en masse for all upcoming encounters, or for a single patient's encounter.
Work with Account Notes and Encounter Billing Notes
Whenever you work with a family on a billing issue, you may want to take notes on the account. You may also have encounter-specific billing notes as you work on a rejected claim.
- Account Notes and Encounter Billing Notes
- Enter and Review Account Notes
- Enter and Review Encounter Billing Notes
Post Charges for an Encounter
Clinician Prepares an Encounter for Billing
Before the biller’s job begins, the clinician must prepare their encounter for billing.
Post Encounter Charges and Queue Up a Claim
A biller selects an encounter that is ready to bill, reviews the codes and payments, and then posts the charges to queue up an insurance claim.
Post Other Types of Encounters
How does PCC EHR work for a telemedicine visit? Can you bill for care provided through portal messages? These additional examples review the post charges workflow and illustrate charge posting for other types of encounters.
- Post Hospital Charges
- Schedule, Chart, and Bill a Telemedicine Encounter
- Post an Administrative Charge
- Bill for Phone Encounters and Portal Messages
- Post Hospital Charges
- Schedule, Chart, and Bill a Telemedicine Visit
- Post Administrative Fees Without an Appointment
- Bill for Phone Encounters and Portal Messages
Review Posted Charges, Find and Add Missing Items
How do you review and update posted charges, and what reports will help you make sure you’ve found every charge that needs to be posted? Read the articles below to learn about PCC EHR tools that help you make sure you’ve completed the work needed before you send claims out.
- Review an Encounter’s Billing History
- Review an Encounter’s Billing History
- Find Encounter Charges That Need to Be Posted
- Reconcile Personal Payments
- Review Posted Charges In Daily Check
Bill Insurance
Submit Claims
Work on Claim Errors and Rejections
- Respond to Claim Rejections
- Respond to Claim Rejections
- Work on Claim Errors, Rejections, and All Unpaid Claims
- Read EDI Responses to Claim Submissions
- Review Archived EDI Reports
Edit Encounter Charges and Submit Corrected Claims
You may need to change the responsible party for encounter charges, change a code suffix, or add an authorization or reference number to a claim. How do you make changes and then resubmit a claim?
- Edit Encounter Charges and Resubmit Claims
- Edit Encounter Charges and Other Claim Information and Resubmit a Claim
- Change the Copay and Responsible Party for Posted Charges
- Enter and Review Encounter Billing Notes
- Unlink and Relink a Payment
- Add an Attachment Code to a Claim
Bill Families
- Generate Personal Account Bills
- Print a Single Account Statement
- Generate Personal Account Bills
- Explain Account Balances
- Review What Appeared on a Printed Bill
Post Payments
Post Personal Payments and Write Off Charges
Post Insurance Payments
Automatically post straightforward ERAs that do not include rejections or errors. Then manually review any outliers and post adjustments, make changes, and resubmit charges or send claims to the next responsible party.
- Autopost ERAs in PCC EHR
- Manually Post Insurance Payments and Adjustments
- Invalid article ID or slug
- Post Insurance Payments and Adjustments
- Read ERA 835s from Payors
- ERAs and EOBs with PCC
- CARC and RARC Values in PCC
Post Less-Common Payments
How do you post capitation checks, incentive payments, interest payments, overpayments, and withhold payments?
- Post Less-Common Payments
- Post Capitation Checks, Incentive Payments, Interest Payments, Overpayments, and Withhold Payments
Review Payment History and Edit Payments
Print Receipts
Review and Audit Charge and Payment Posting
PCC includes a variety of tools and reports for double-checking charge and payment posting for the day.
- Prove Out and Reconcile Charge and Payment Posting
- Reconcile Personal Payments
- Reconcile Insurance Payments
- Report on Adjustment Trends in PCC EHR
Work Insurance A/R and Personal A/R
How do you ensure that no unpaid encounters slip through the cracks? How can you identified families that need an extra phone call to get their bill paid?
- Follow Up on Unpaid Encounters with Insurance Balances
- Work Personal Balances
- Review a Family’s Account History
- Review a Family’s Account History
- Follow Up on Unpaid Encounters with Insurance Balances
- Work Personal Balances
- Explain Account Balances
Handle Less-Common Accounting Tasks
Every day, billers post charges, post payments and adjustments, and bill families. What about less-common events, or challenging accounting tasks?
- Refund Personal Credits
- Post a Returned Check or Other Personal Payment Reversal
- Reverse an Insurance Payment (Post a Takeback)
- Requeue Large Numbers of Claims and Resubmit
- Refund or Write-Off Account Credits
- Post a Returned Check or Other Personal Payment Reversal
- Reverse an Insurance Payment (Post a Takeback)
- Requeue Large Numbers of Claims and Resubmit
- Write Off Charges and Bad Debt
- Turn an Account Over to Collections
Configure Insurance and Billing
Billers may need to configure how diagnoses and procedures are coded, add a new insurance payer to the system, and adjust procedures and their prices. PCC Support can help with these tasks.
- Edit Your Practice’s Configuration Tables
- Edit Your Practice’s Procedures, Codes, Adjustments, and Prices
- Edit the Insurance Plans on Your PCC System
- Configure Claim Holds and Claim Delay
- Configure Order Billing, Diagnoses, and the Bill Window
- Edit Your Practice’s Configuration Tables
- Edit Your Practice’s Procedures, Codes, Adjustments, and Prices
- Edit the Insurance Plans On Your PCC System
- Configure Claim Holds and Claim Delay
Print Visit Forms
What do you hand patients and families when they walk in the door? Your practice may generate educational handouts specific to a visit reason, encounter forms for the clinician, and other visit forms.
Use the “Print Visit Forms” features in PCC EHR to generate all the visit forms for the day, or to print them for individual patients as they come in, whichever method suits your office’s workflow.
Other Types of Forms: To learn about other form output in PCC EHR, visit Generate Form Letters in PCC EHR.
Use Print Visit Forms Tool to Print All Forms for a Day’s Appointments
You can use the Print Visit Forms tool to generate all the forms you need for appointments on a given day.
Open Print Visit Forms from the Tools Menu.
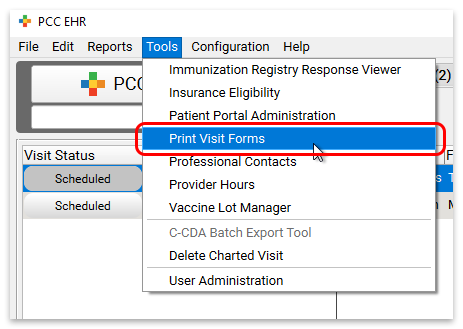
Select a date, location, and provider, and click “Print Visit Forms”.
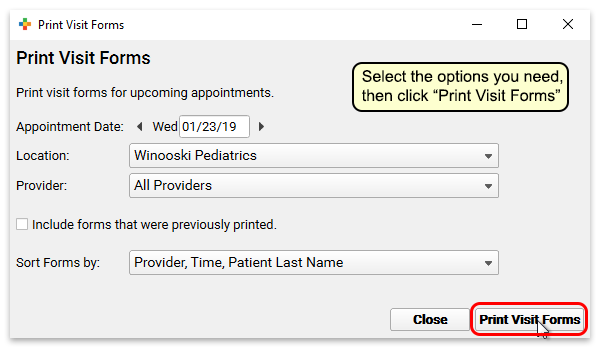
Then use your system’s print dialogue to print the forms.
Print or Reprint Visit Forms For a Single Encounter
You can print visit forms as you check in a patient, or right from the patient’s chart.
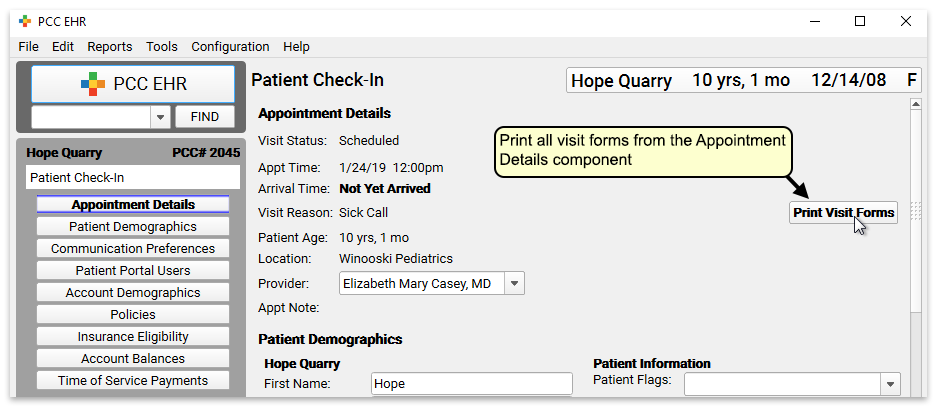
Appointment Details Component: The “Print Visit Forms” button appears anywhere you use the Appointment Details component—in Patient Check-In, and also at the top of chart notes.
Reprint Visit Forms: If you have already printed the forms once, the button text will read “Reprint Visit Forms.” Click the button to print the forms a second time if necessary.
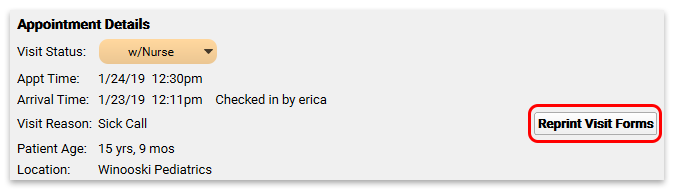
Disable Form Printing: You can remove the Print Visit Forms button from charts and Patient Check-In by editing the Appointment Details component in the Component Builder.
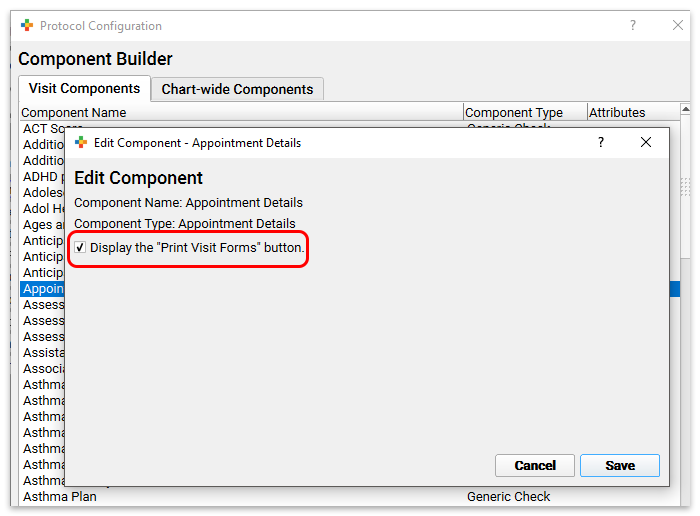
Use pocketPCC to Add Photos or Upload Files to Patient Charts
A picture is worth a thousand words. Rather than try to describe a patient’s rash in your chart note, you can take a photo with your mobile phone and use pocketPCC to upload it right into the chart. You can also use pocketPCC to upload a photo or a form sent to you by the patient’s family.
Add Photos/Files
The “Add a Photo or File” chart menu option in pocketPCC allows you to add photos and files from your mobile device directly into the patient’s chart.
You can add a photo you take during an office visit, or upload a form or photo that the family emailed you.
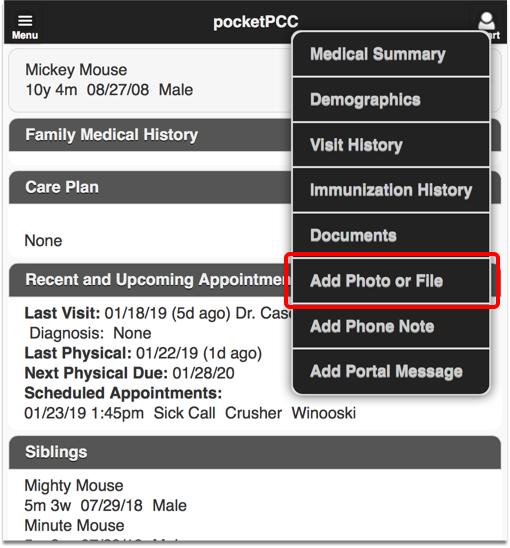
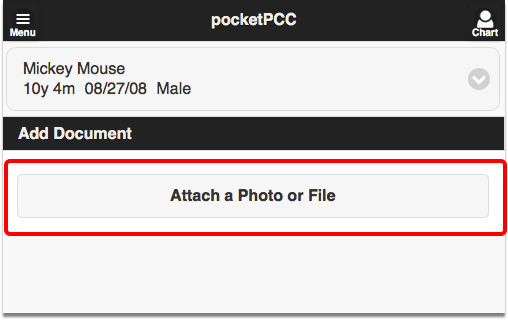
You can attach multiple photos or files, and then click “Save Document”.
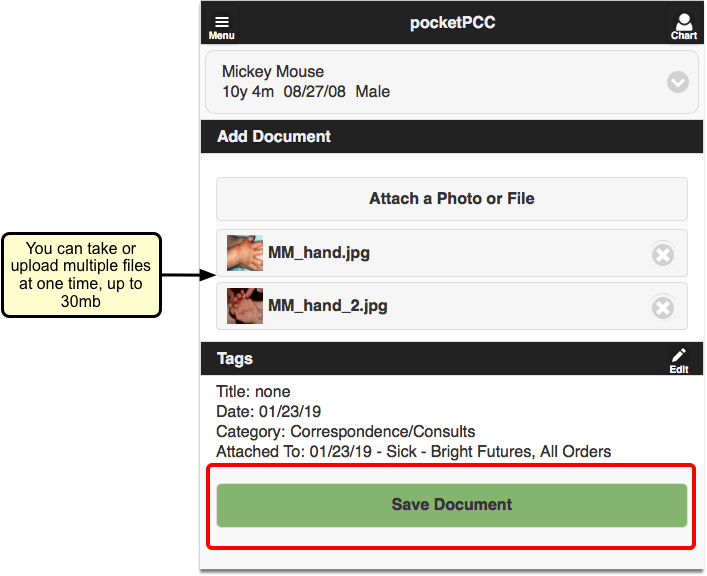
The photos/files will be attached to the current day’s visit by default. If the patient does not have a visit today, the item will be added as an unattached file.
If you want to change the visit attachment or add a title, tasks, or signature requirements, edit the tags before saving.
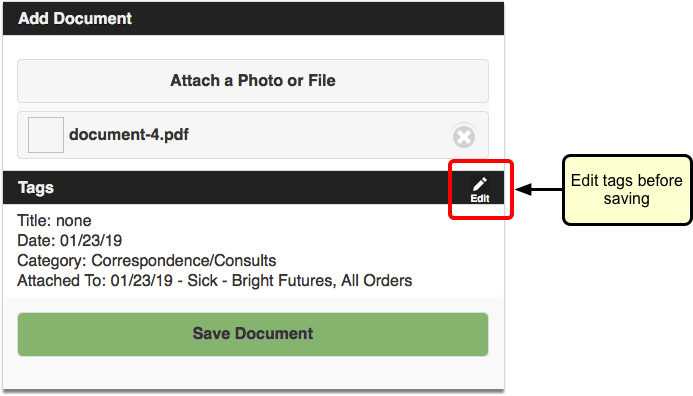
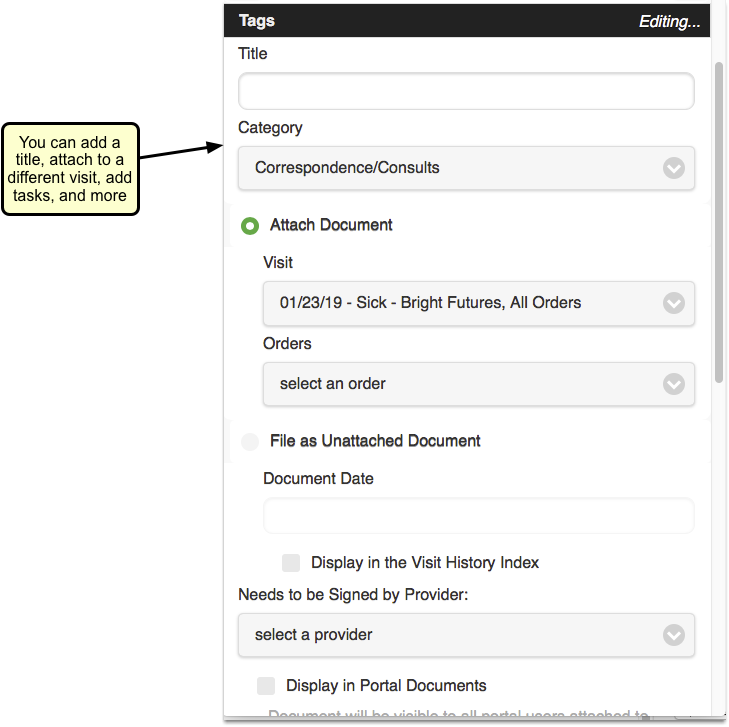
Uploads through pocketPCC are limited to 30 megabytes.
Does the Photo or Document Also Save to My Device?: Under normal conditions, the photo you take from pocketPCC will not save to your mobile device. However, if you take the photos before launching pocketPCC, or if your phone automatically saves photos to your camera roll or gallery, you may end up saving private health information to the device. PCC is not responsible for the security of your workstations or portable devices, and you should review your device’s operation and take appropriate precautions.
View Files/Photos in pocketPCC
To view previously saved photos or files within pocketPCC, open the “Documents” menu option, and find the date of the visit.
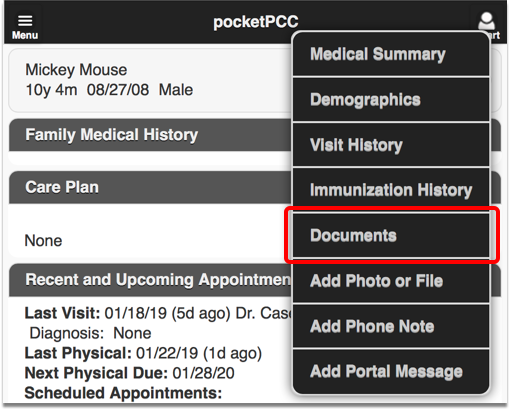
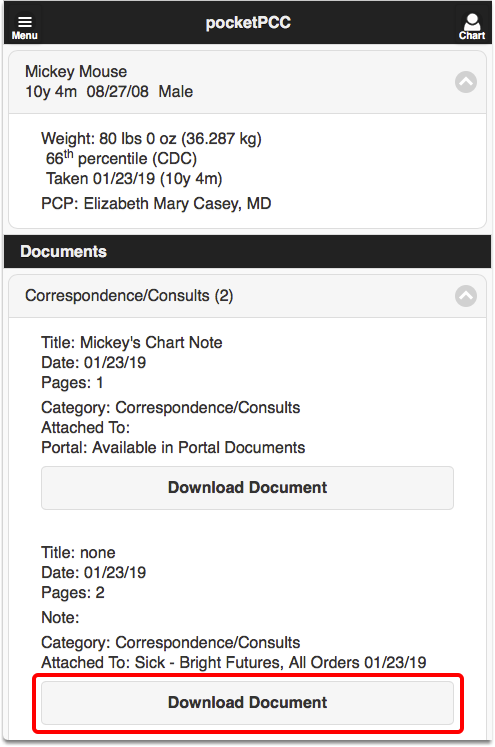
You can click “Download Document” to view the file(s).

Review and Edit Files/Photos in PCC EHR
You can view photos and files that were uploaded through pocketPCC within the visit chart note in PCC EHR, or anywhere else that Documents appear.
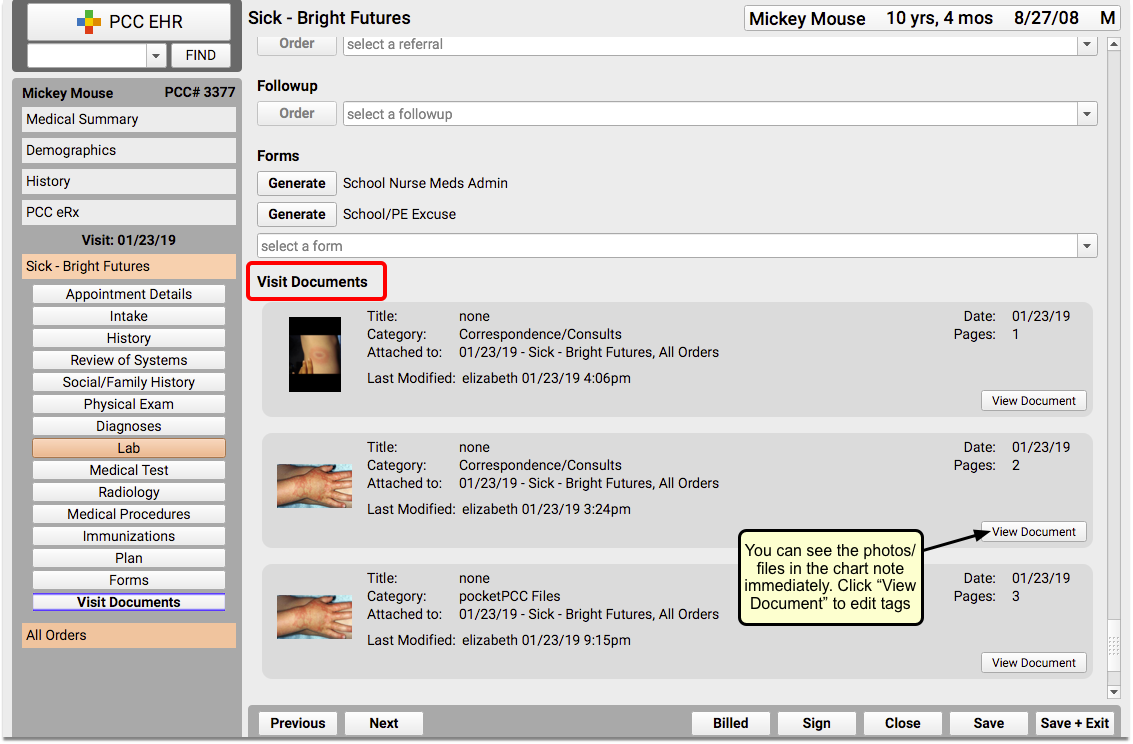
If you want to change the visit attachment or add a title, tasks, or signature requirements after saving, you can make edits in PCC EHR. For more information on editing documents or photo files through the Document Viewer, read Working with Patient Documents.
If you want to keep track of photos or documents that were uploaded through pocketPCC, you can add a new document category, and add it as the default assigned category for pocketPCC. Read the Documentation Administration guide for more information about creating and assigning document categories.
Recall Overdue Patients for Well or Chronic Condition Visits
The best and easiest way to recall patients who are overdue for their well or chronic condition visit in PCC EHR is to run the Preventive Care Recall report or the Chronic Condition Recall report.
Open The Report Library
Open the Report Library from the Reports menu in PCC EHR.
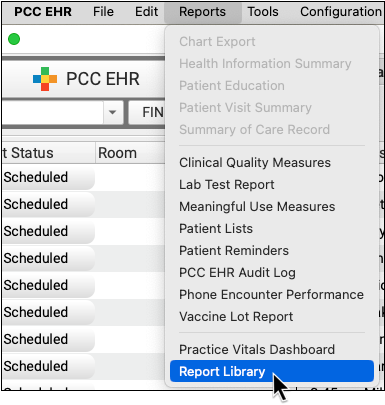
Open the Patient Recall Section
Search for or select the Patient Recall Section of the report list.
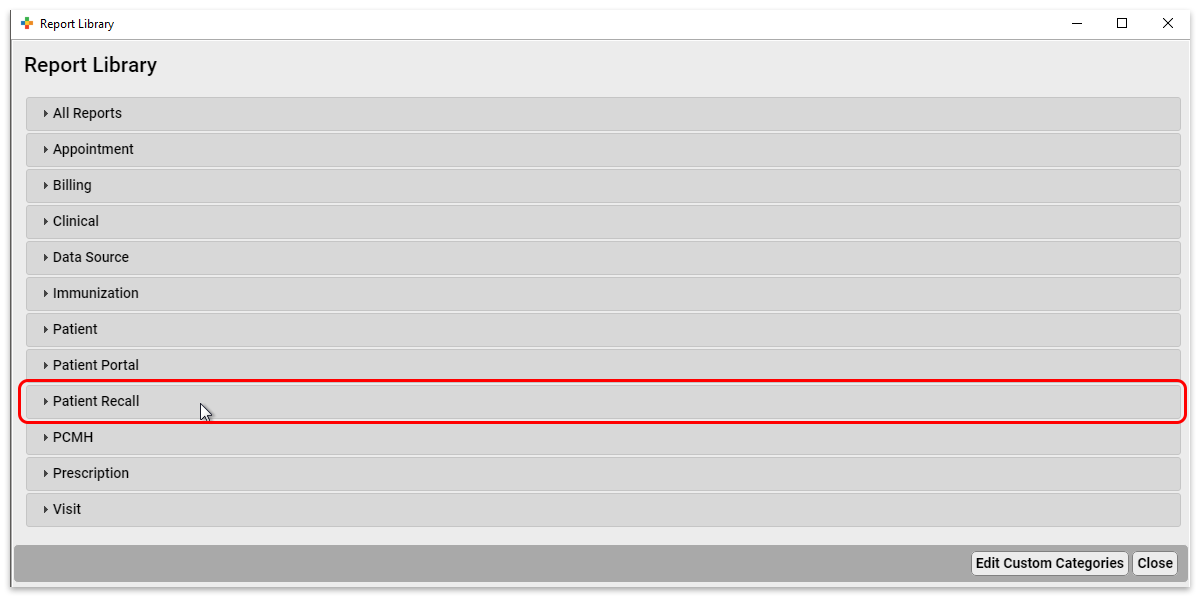
Open the Preventive Care Recall or Chronic Condition Recall Report
Click on either the Preventative Care Recall report or the Chronic Condition Recall Report to open it.
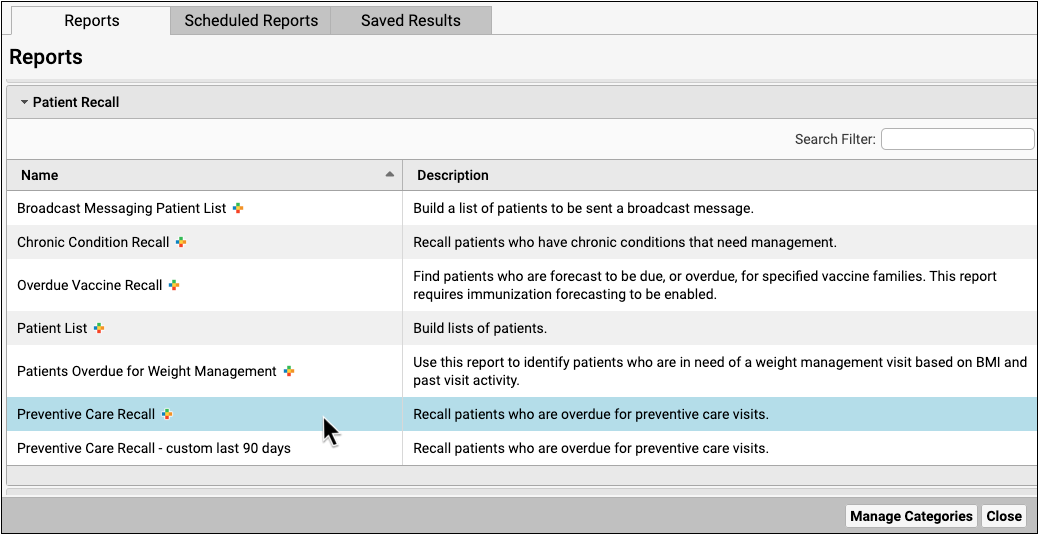
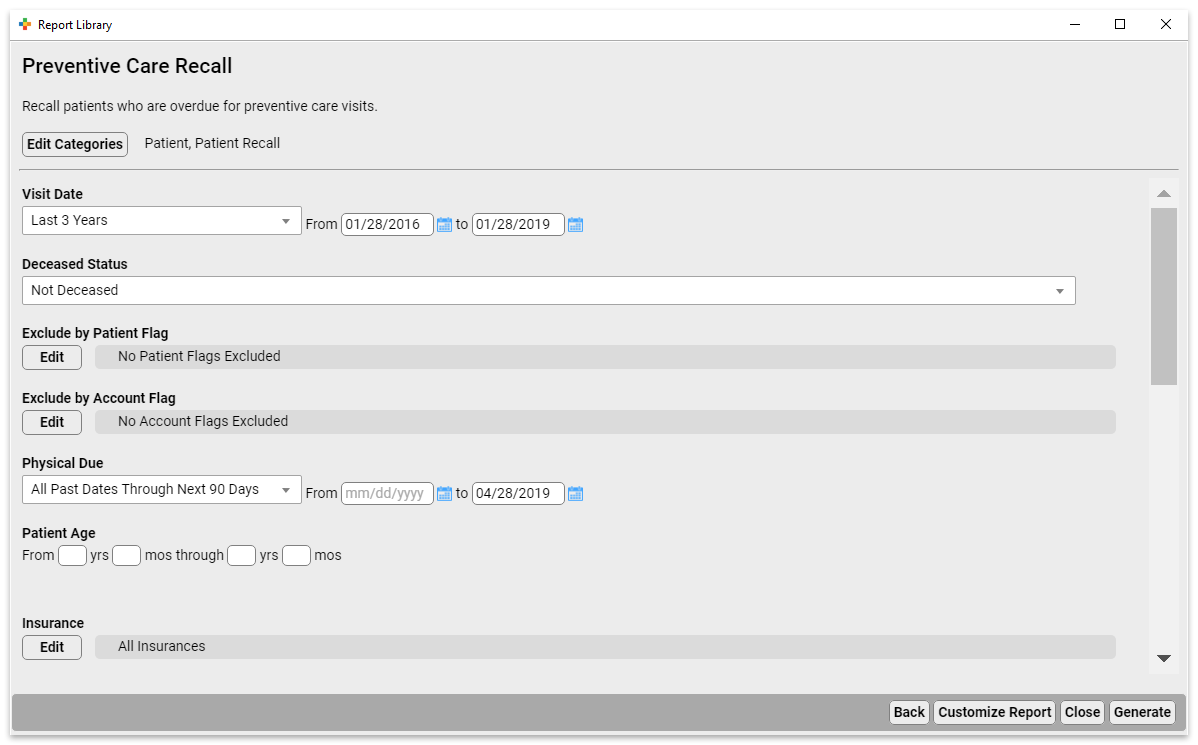
Select Criteria and Run The Report
The Preventive Care Recall report gives you many options for tailoring your recall list.
- Use the Exclude Patient Flag criteria to exclude patients who are deceased, have transferred, have been dismissed, or are otherwise no longer at your practice.
- Use the Exclude by Account Flag criteria to exclude patients whose accounts are inactive.
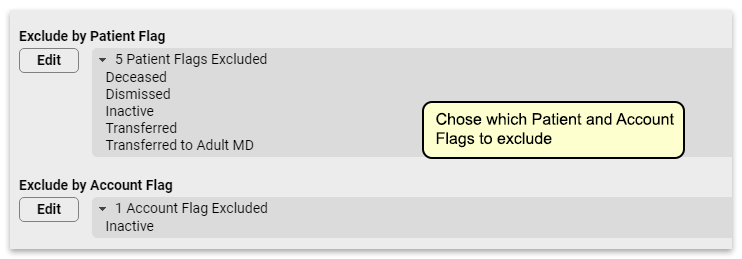
Set the Physical Due criteria to match the time frame you expect to be scheduling for. If you’re already scheduled for 3 months out, setting this to “All Past Dates Through Next 90 Days” will give you a list of patients that includes patients who will be due for their physicals at the time your schedule is open.
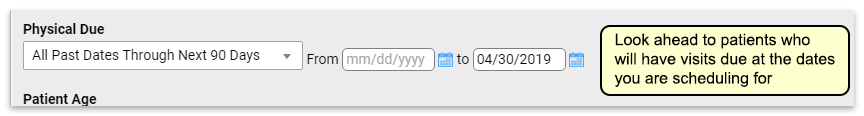
You’ll want to exclude patients who already have a physical scheduled, so use the Exclude by Scheduled Appointment criteria to remove those patients from this list.
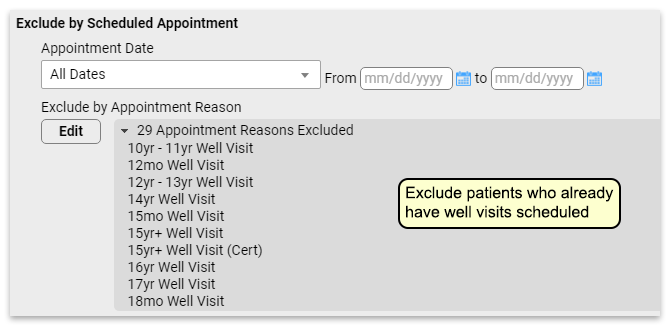
It’s likely that running the report with just these criteria set will still leave you with an unmanageable recall list. You might further refine this list in various ways:
- Focus on a specific age range. Maybe you want to focus on kids who will need vaccines before they start kindergarten, so you run this for patients who are 4-5 years old. Or you could run a list of 10 year olds so you can get them in for their HPV vaccination.
- If your list is still too long, you might choose to recall patients with a specific insurance carrier.
Adjust the Report
Adjust report output to include your preferred columns for patient contact, such as phone, address, etc. Once you’ve got a list of a manageable size, you can use this report to recall patients.
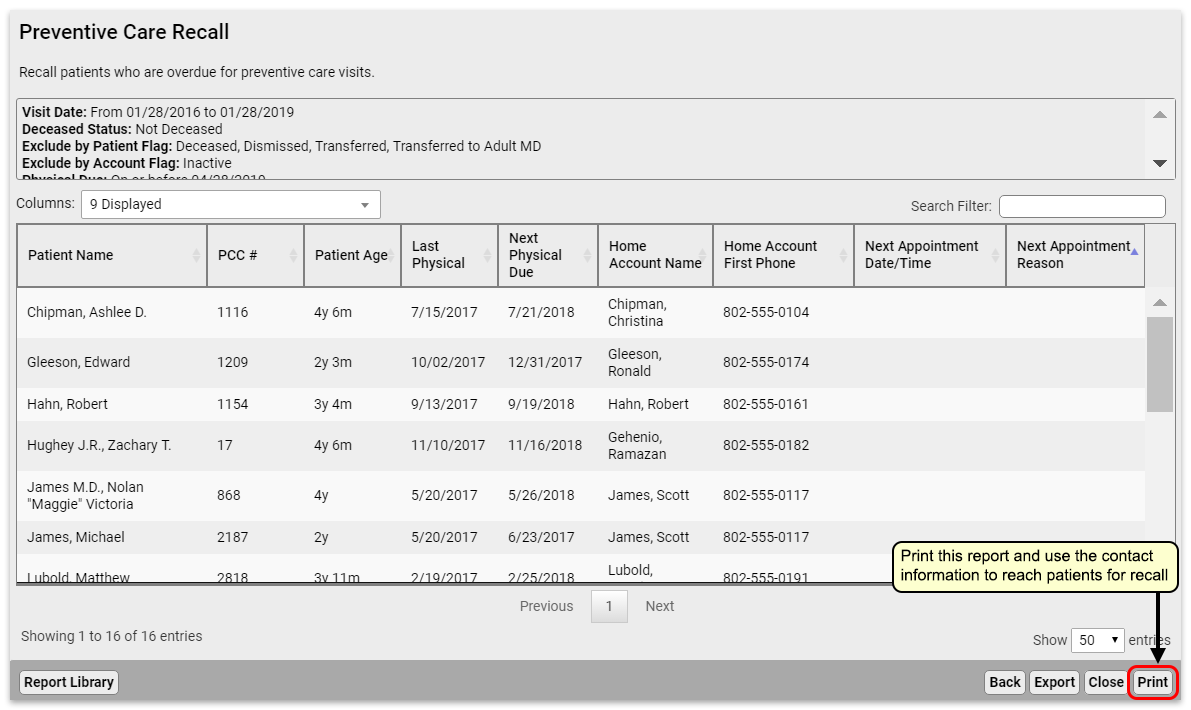
You can optionally print your report if your practice offers personalized phone calls.
Export the Report or Send Batch Messages
In the Report Library, you can export to PDF, CSV, or send batch messages to patients via email or text message.

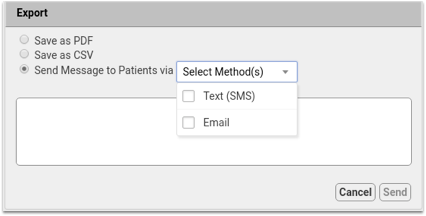
- Export to PDF for a digital version of the printed report. Report output cannot be adjusted once exported to PDF.
- Export to CSV to work with your report output in a spreadsheet. Totals and sorting using Group By do not transfer to CSV.
- Once you build a patient list in the Report Library, you can compose batch messages and text or email them to patients and families.
To learn how, read Send Batch Messages to Patients and Families.
Optionally Schedule the Report
You can make several customized recall reports, such as overdue well visits by specific ages, and then schedule each of your custom recall reports to run on a monthly cycle.
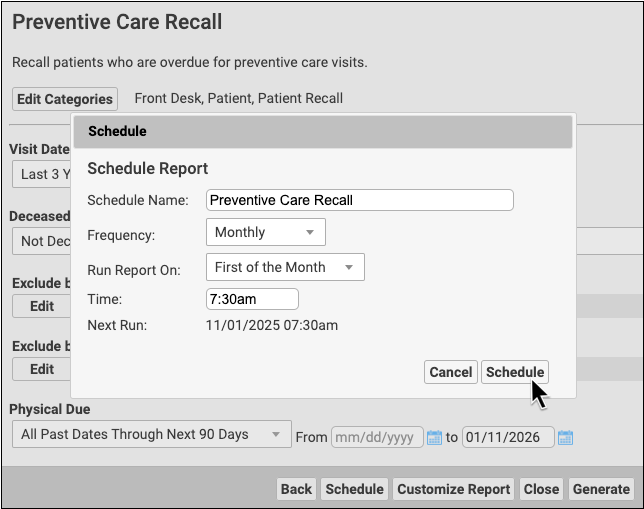
To find out more about scheduling a report read Schedule Reports to Run Automatically.
Find and Recall Patients Who Are Overdue for Vaccines
Which 13-year-olds at your practice never came in for an HPV shot? Can you quickly find all the six-year-olds who never made it in for their final IPV, MMR, and Varicella? PCC can find all of your patients that are due or overdue for vaccines and produce customizable reports.
Tracking immunizations is important for patient health. Being able to get accurate lists of patients who are due or behind on an immunization schedule is vital to maintaining a proper immunity for your patients and the public health of your community.
PCC EHR offers a few different tools for finding and recalling patients who are overdue for a vaccination.
Use the Overdue Vaccine Recall Report to Find Patients
Use the customizable Overdue Vaccine Recall report to find all of your patients who are due or overdue for vaccines.
Watch a Video: For a quick introduction to finding patients who are due for a vaccine, watch the Recall Patients Who Are Overdue for Vaccines video.
When you are ready to create a patient list, run the Overdue Vaccine Recall report in the PCC EHR Report Library.
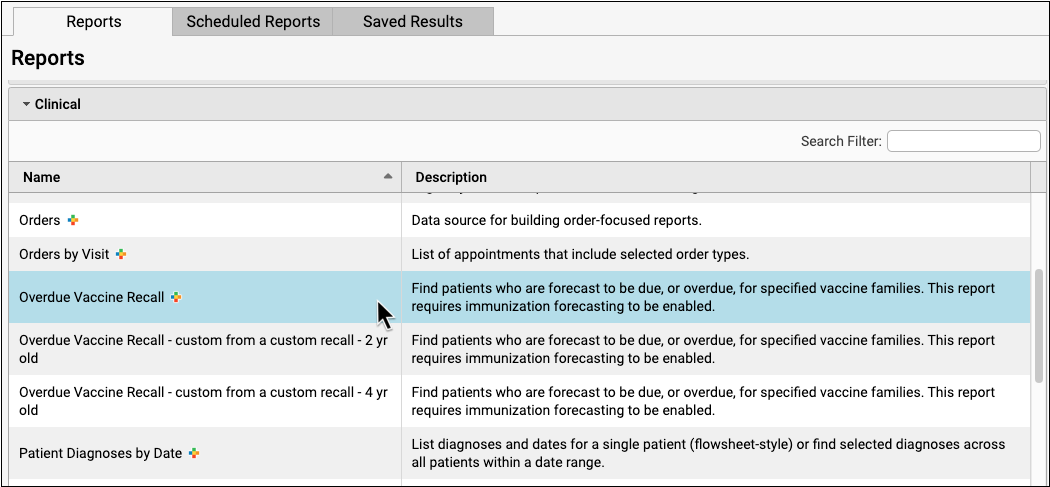
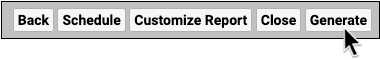
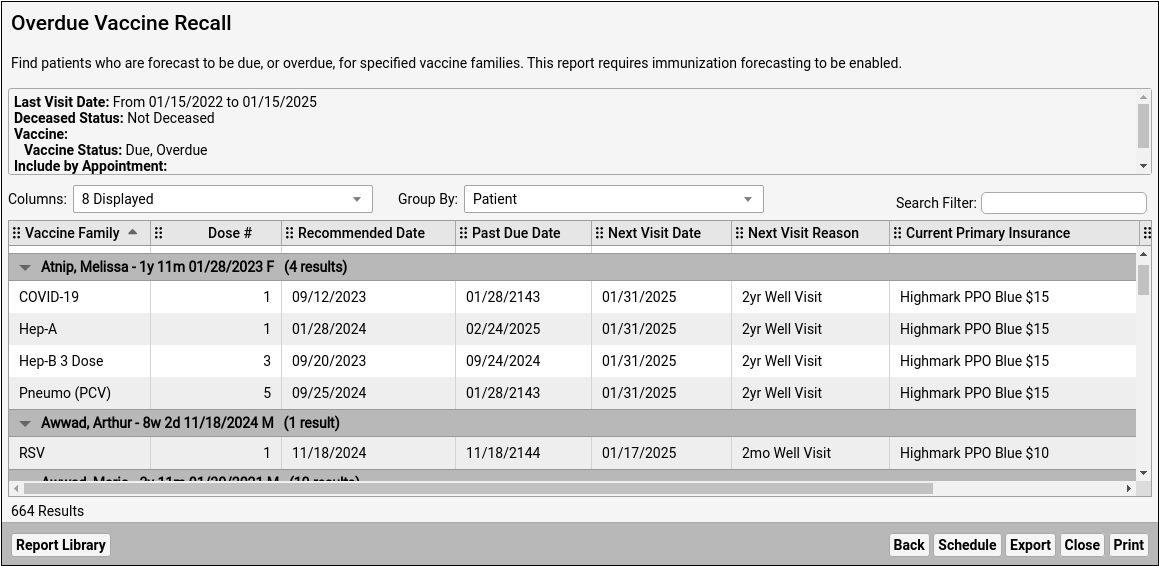
By default, the report will review the records of all patients who have visited your practice for the past three years and who are not marked as deceased. The report will compare those patient’s immunization records to ACIP guidelines.
Depending on your report criteria, the report will show you all missing vaccines and dose numbers for each patient. By default the report displays the recommended date, the patient’s next scheduled appointment, and their current insurance. You can add or show additional columns, such as phone numbers or other demographic information, in order to contact the family.
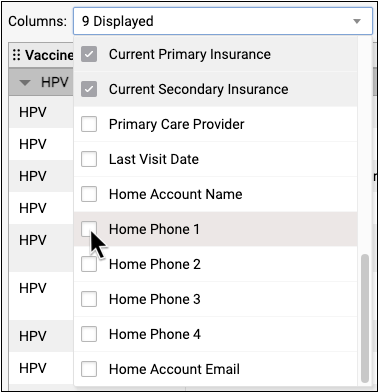
You can also change the Group By setting to “Vaccine Family” in order to see lists of patients behind on a particular vaccine.
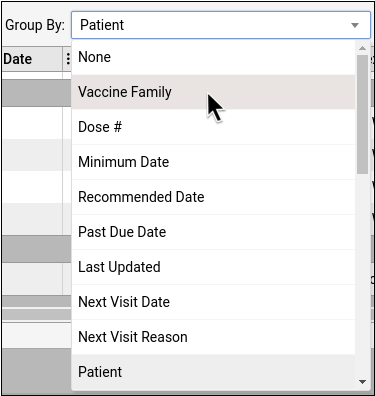
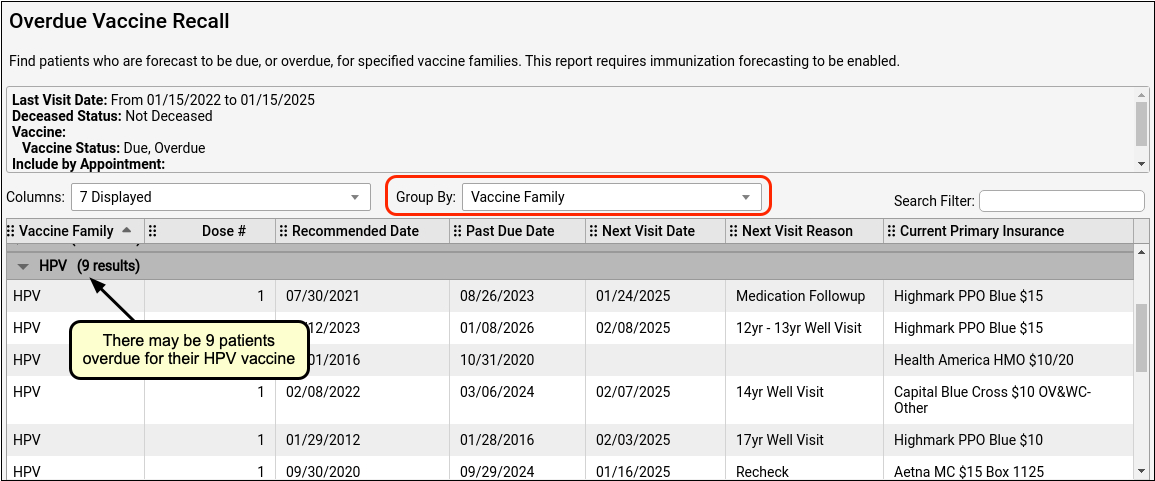
Vaccine Recall Relies on Patient Records and Immunization Forecasting: The Overdue Vaccine Recall report calculates overdue vaccines based on immunization forecasting data. If you do not have up-to-date immunization records for a patient in their chart, the patient may appear on this report even though they are immunized. Additionally, if your practice does not use Immunization Forecasting (which is included in PCC EHR but can be turned off), the report will not display any data. To learn more about PCC’s immunization forecasting tool, read Immunization Forecasting. You can always contact your PCC Client Advocate or PCC Support for help.
Refine Vaccine Recall With Criteria
Before you run the report, you can set specific criteria for your search.
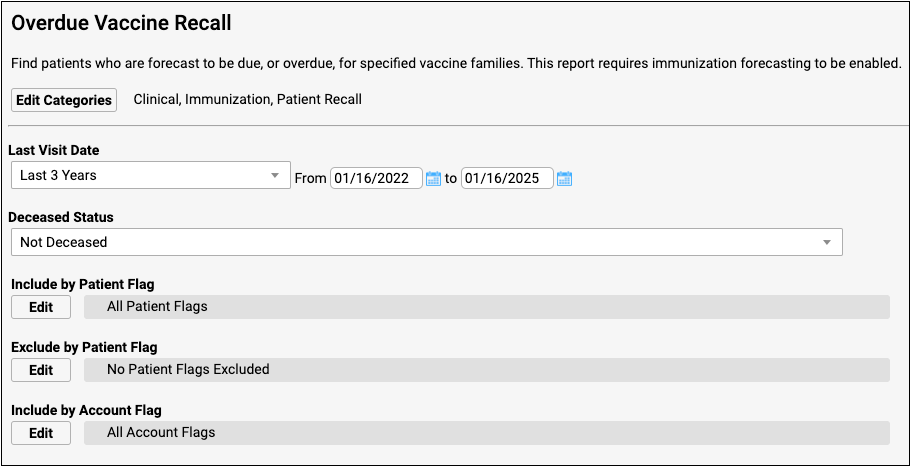
What if a patient is already scheduled for an upcoming physical? You may want to exclude all patients who are scheduled for an upcoming appointment.
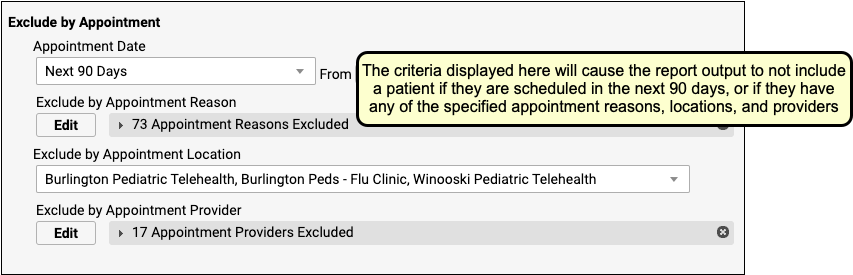
You could also select a specific vaccine family to search.
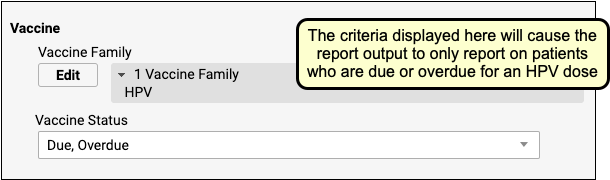
You can also include or exclude patients by status flags, age ranges, care center, sex, or many other criteria. After you set criteria, click Generate to find patients.
Create Custom Vaccine Recall Reports For Your Specific Needs: You can use the Report Library to create custom versions of the Overdue Vaccine Recall report based on your needs. For example, if your practice was working to improve HPV vaccination rates, you could create a specific custom report with saved criteria and columns in order to help quickly identify and contact patient families. To learn more, watch the Create a Custom Report in PCC EHR’s Report Library video.
Export Results and Contact Patients and Families
Once you’ve got a list of patients who are overdue for a vaccine, what will you do with it? Click “Print” to print the results, either to a printer or to a file.
You can also export the data as either a PDF or a CSV (for use in a spreadsheet), or use the broadcast messaging feature to send a batch text or email message to patients on the list.
Export Results as a PDF or CSV
Export results as a PDF if you plan to email the information to someone, or as a CSV if you want to put the information into a spreadsheet.

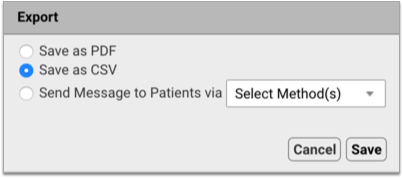
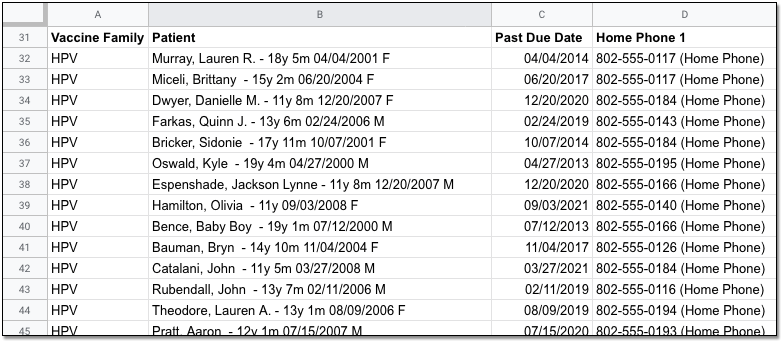
Before you export your report, you can optionally add columns for family phone numbers and other demographic information. You can use a CSV export for mail merge or another method to contact each family. As always, remember that report output and other files from PCC EHR may contain private health information and should be handled appropriately.
Send a Batch Text or Email Message to Patients on the List
When you export report results, you can compose a text (SMS) or email message and send it to all patients on the list who are opted-in to broadcast messages from your practice.

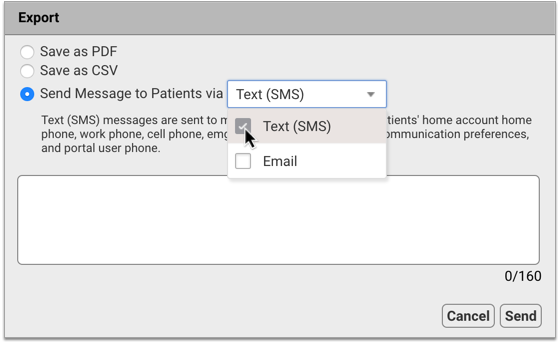
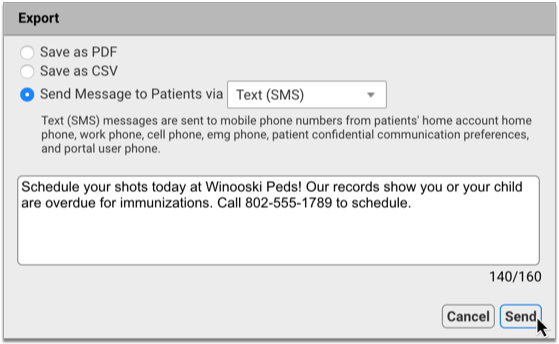
You can find comprehensive information about how to use broadcast messaging in the article Send Batch Messages to Patients and Families.
Patient Immunization Administration Summary
The Patient Immunization Administration Summary, in the Report Library, can create a list of all patients who are due for a vaccination.
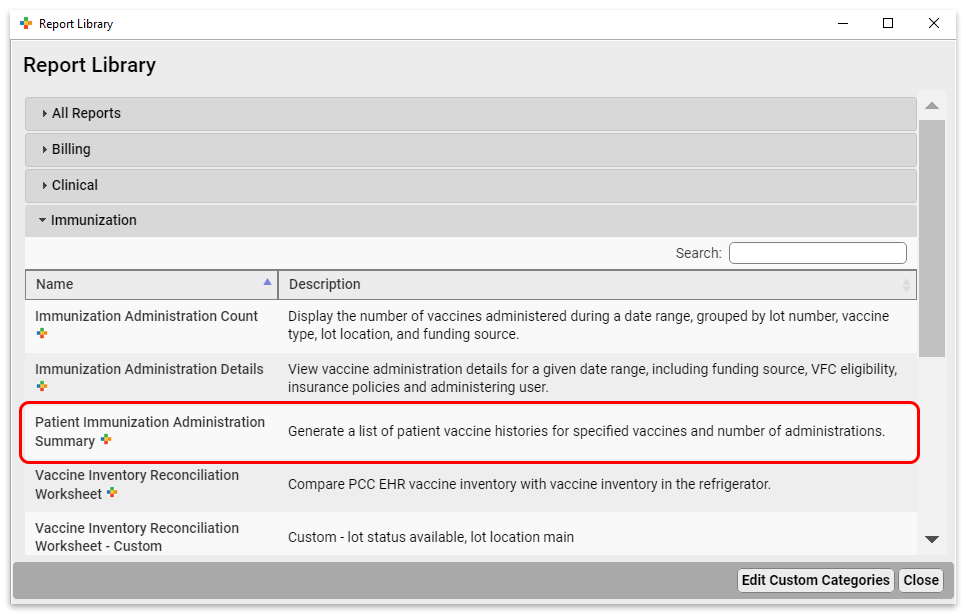
Let’s say you wanted to find all patients who are due for HPV. You would run the report with the following criteria:
- Excluding inactive patient flags
- Patients who are 12 years old
- Patients who have been seen in the last 3 years
- Patients who have received 0 or only 1 shots (from 0 to 1 in the “Number of Shots” criteria) of HPV. Note, your practice might have different or multiple immunization names for HPV, such as Gardasil
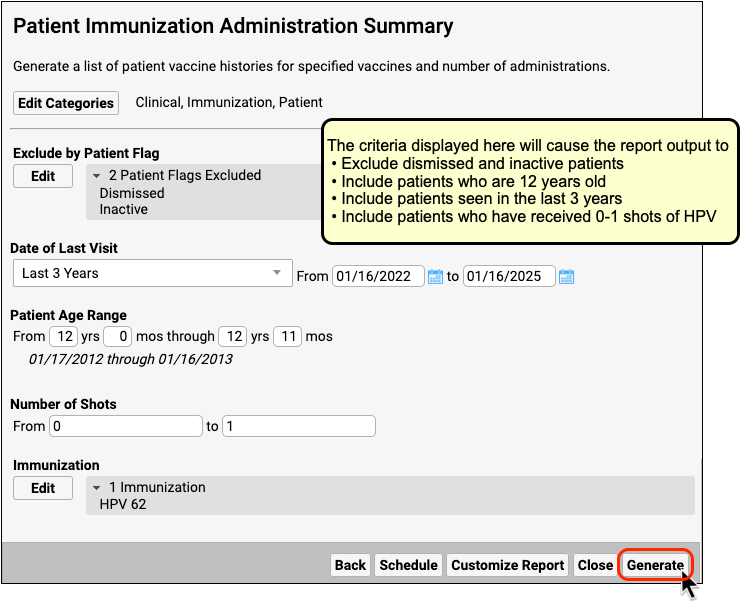
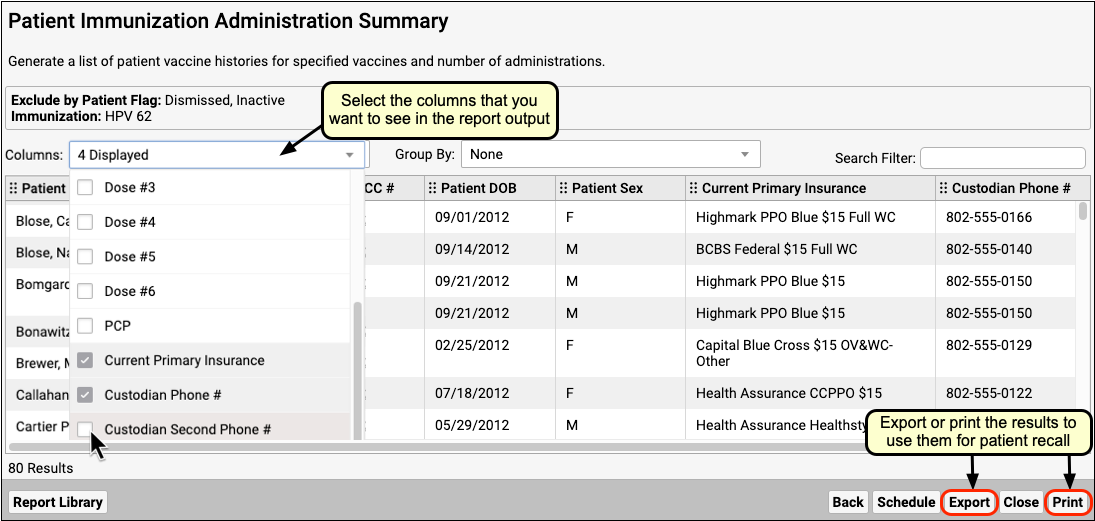
Create a Custom Report for Recall: You may want to create a custom report for patient recall for a particular immunization, or one that automatically includes the custodial phone numbers. Read here to learn how to create and save custom reports.
Use Practice Vitals Dashboard for an Overview
Your Practice Vitals Dashboard is a great way to get a broad picture of your immunization rates, broken down by various patient populations. The Dashboard can also produce lists of overdue patients.
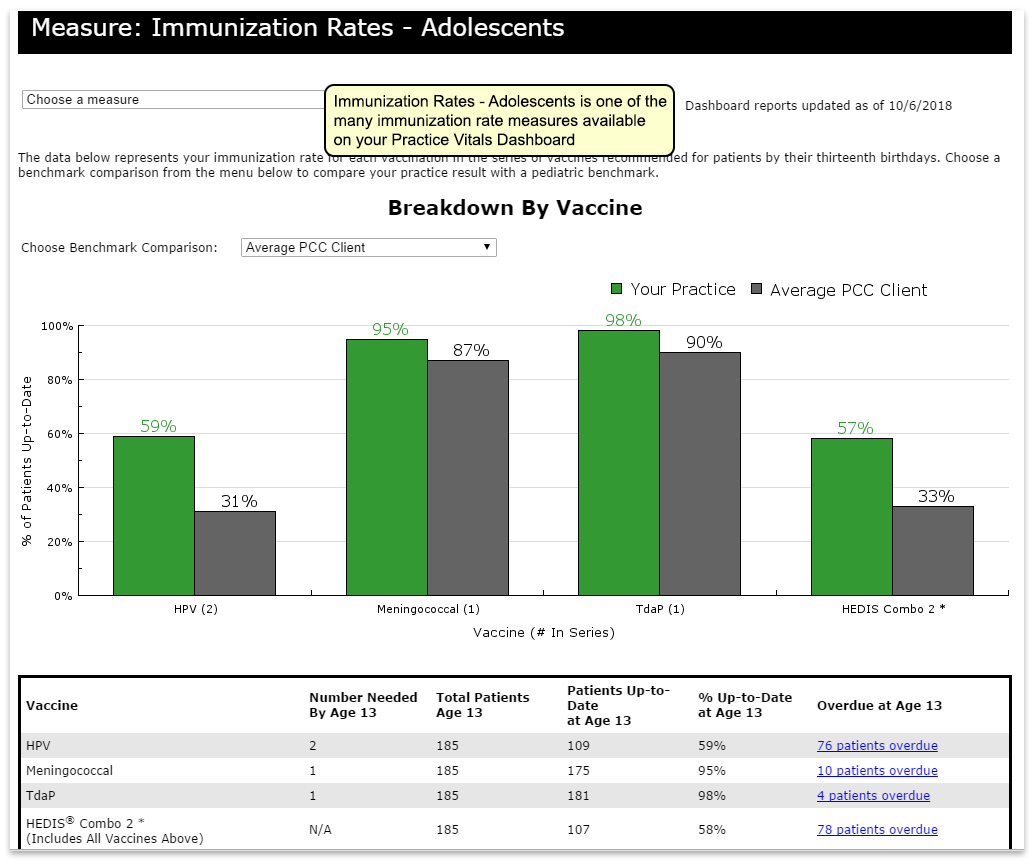
Dashboard Data is Not Live: The Dashboard pulls data from the EHR once a month. On any given day the data is anywhere from 0-31 days old. By the end of the month, patients who are listed as being due for a vaccination might have already received it, or might already be scheduled to come in. Because of this, the Dashboard is not an ideal tool for immunization recall, though for some purposes the overdue lists can be useful. For an up-to-date list, use the Patient Immunization Administration Summary report as described above.
Look Up ICD-10 Codes For Referrals, DME Requisitions, and Pre-Authorizations
When you are filling out a lab requisition, referral, or a request for DME, you may need the ICD-10 codes for a patient’s diagnoses. In PCC EHR, you can quickly review ICD-10 codes for patient diagnoses and Problem List items on the Diagnosis flowsheet.
First, open a patient’s chart and navigate to the Flowsheets section inside the Visit History section.
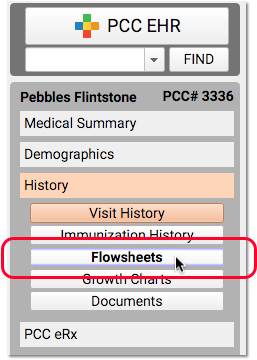
On the Diagnosis flowsheet, click on the ICD-10 link under a date to view the ICD-10 codes used for the encounter.
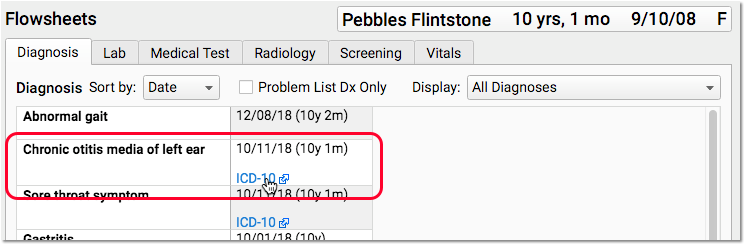
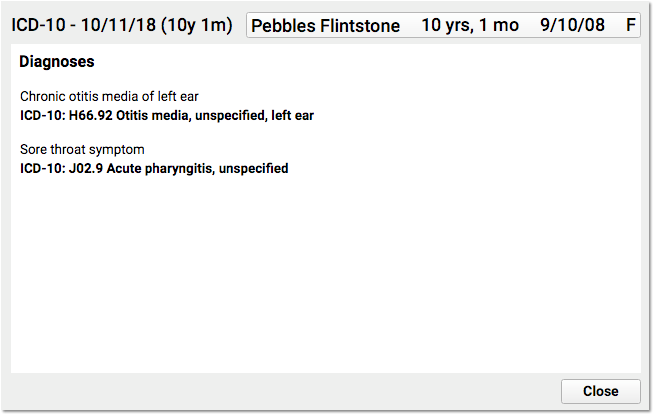
The Diagnosis flowsheet displays all of a patient’s SNOMED diagnosis descriptions, with a list of each date when the diagnosis was made. When you click on a particular date’s ICD-10 link, PCC EHR displays all of the ICD-10 codes for that encounter, which may also include information about laterality, episode of care, and other considerations.
You can use the ICD-10 information to complete the requirements of a lab requisition, referral form, durable medical equipment request, prior authorization form, or other task that requires the ICD-10 billing diagnosis code.
Read Your PCC Email with Roundcube
You can access your PCC-provided email services with Roundcube, a Web-based email program. This manual contains an introduction to Roundcube, along with a guide for setting up two-factor authentication (2FA) for your PCC email using the Authy app.
Start Roundcube and Log In
Open a Web Browser
Open your web browser of choice. Roundcube will work in any browser. Note that browsers on mobile devices may display a more limited interface optimized for mobile devices.
Enter Your Office’s Web Mail Address
In the browser address bar, enter your practice’s Web Mail address. Your address is your PCC acronym followed by pcc.com/roundcube. For example, if you work at Bedrock Pediatric Associates, your PCC acronym might be ROCKPA. Your Web Mail page would be https://rockpa.pcc.com/roundcube/.
You can bookmark this page or create a Web shortcut on your desktop for quick access to Roundcube.
Type Your Name and Password
Your email name and password are the same as for PCC EHR. If you do not have a PCC login, contact your practice’s system administrator or office manager.
Click “Login”
View Your Email
You can now use your Roundcube email. Roundcube opens to your inbox, where you can read, reply, and otherwise manage your messages.
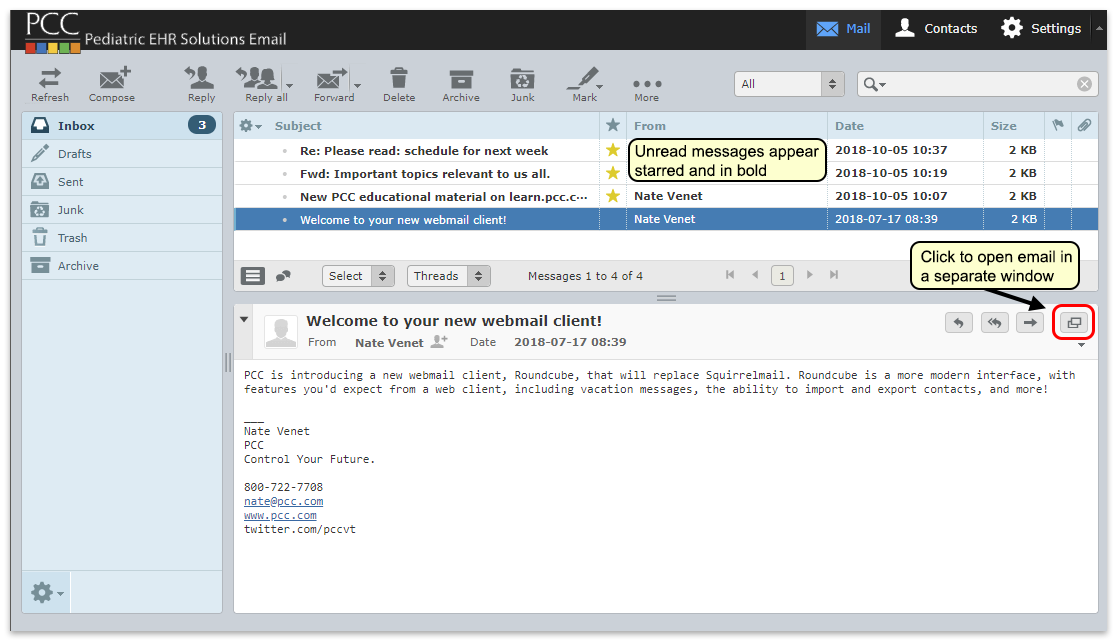
Send an Email Message
Follow the procedure below to send an email message.
Click “Compose”
Click “Compose” to begin writing a new email message. Or, click “Reply” while viewing a message to compose a reply email to the sender. You can click “Reply all” to ensure that your message will also be sent to everyone who received the original message.
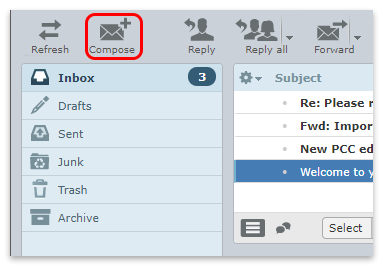
Compose Your Message
Enter the address of the recipient, subject, and message text in the fields provided. Press the Tab key to move from field to field.
Use the “Attach a file” button to browse your local computer or network for attachments, or simply drag the file onto the attachment area of the email, as shown below.
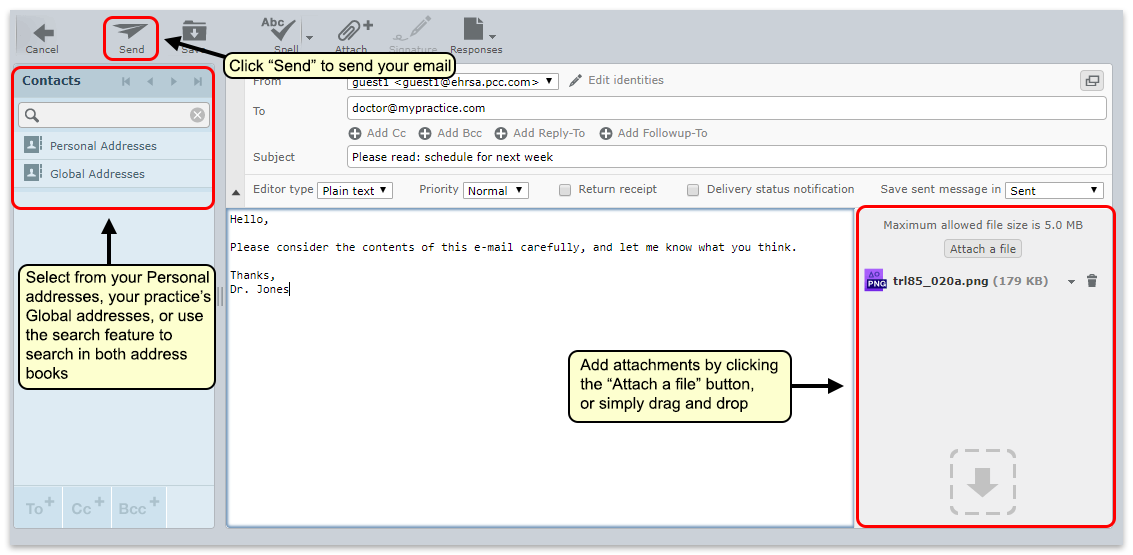
Multiple Recipients?: You can add several email addresses in the “To” field, separating each one with a comma. You can also use the “Add Cc” or “Add Bcc” features to send copies of your email to additional recipients. Recipients that you list in the “Bcc” field will not see the list of other recipients of the email.
HTML vs. Plain Text: Sometimes you might want to compose an email using fonts, formatting, bullets, and embedded images. By default Roundcube composes all emails in plain text, but you can switch to an HTML formatted version using the “Editor type” drop-down. You can change this default behavior in the “Settings” menu.
Manage Folders
You may want to set up folders for your mail. You can do this using the “Manage folders” option under the gear icon.
Open Folder Settings
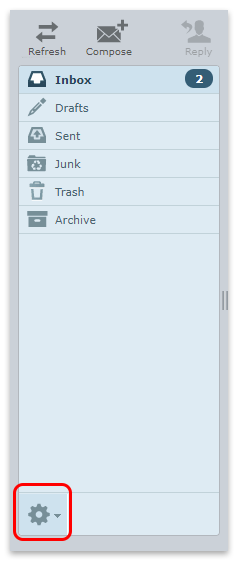
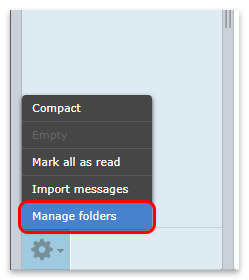
Settings Menu: You can also access this page through the “Settings” gear icon at the top of your Roundcube window.
Add Folders
Here you can review, add and delete folders.
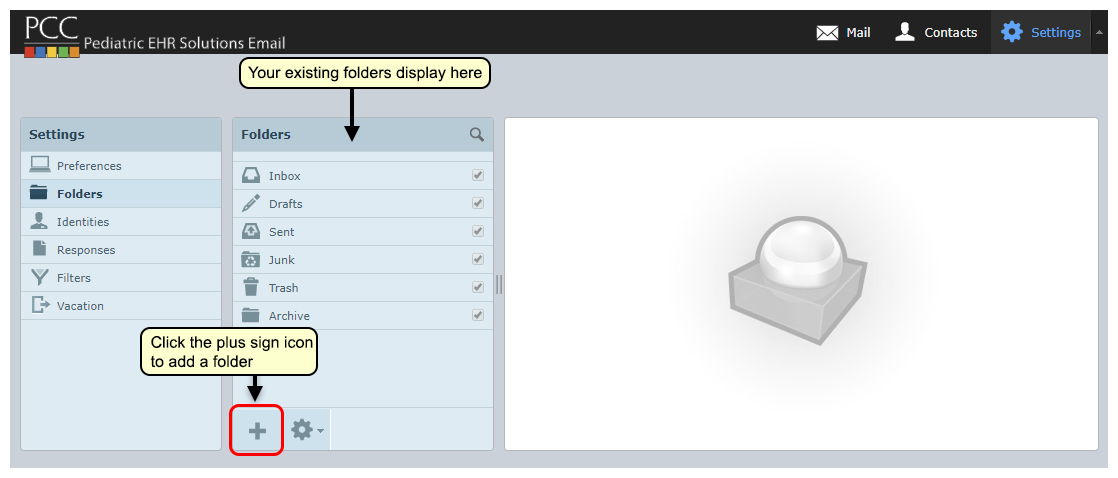
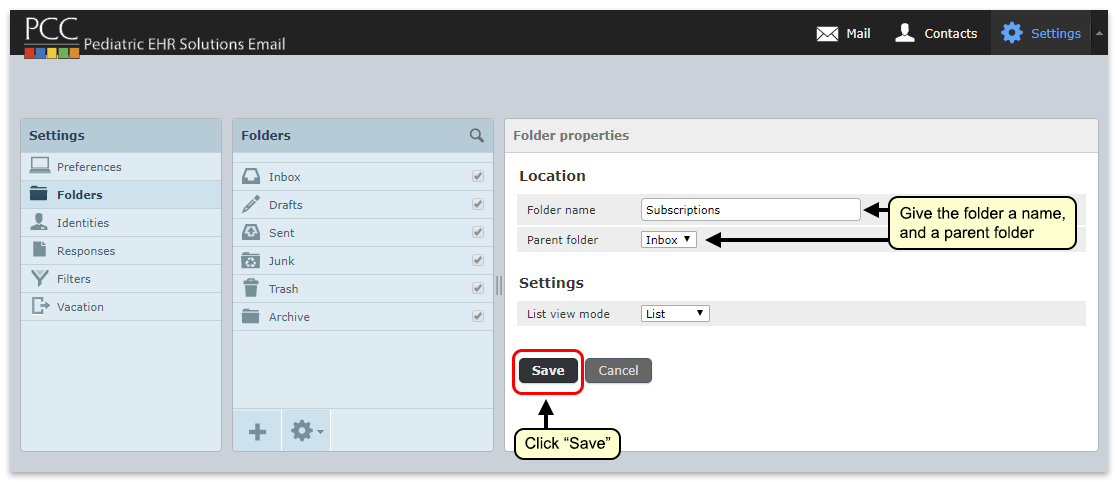
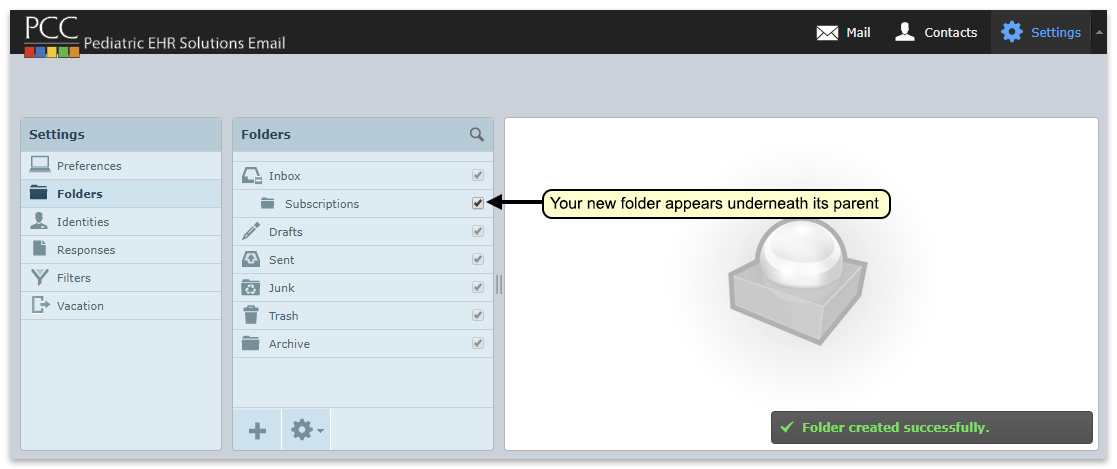
Back on your Mail screen, you will see your new folder. Drag and drop emails into the folder, or set up filters to automatically file incoming mail into various folders.
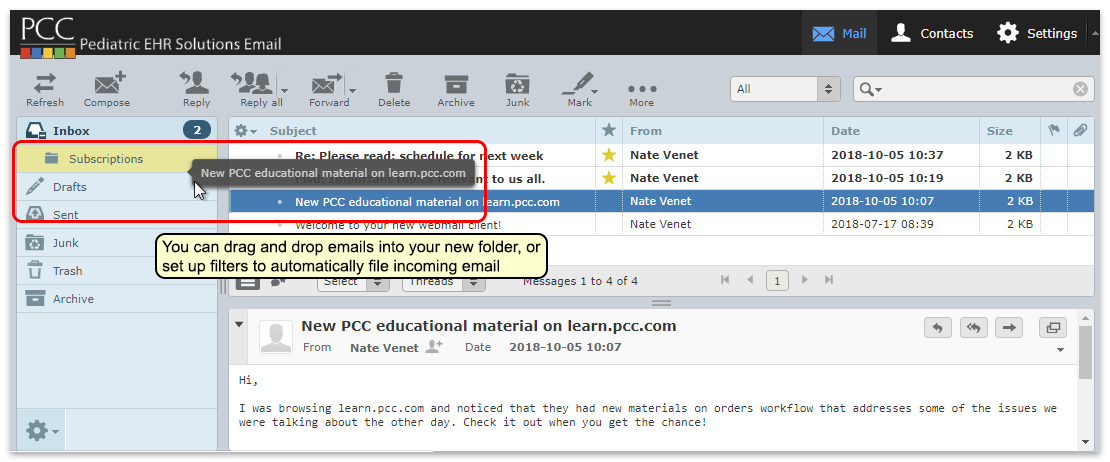
Flat File Structure: Roundcube uses a flat file structure for folders. This means that you cannot normally “nest” folders. You can only create folders at the top level or inside your Inbox. However, if you used nested folders with a different e-mail program, such as Squirrel Mail, Roundcube will recognize and preserve that folder structure.
Contacts
You can add email addresses to Roundcube’s address book, making it faster and easier to email your frequent contacts.
Access your address book by clicking on the “Contacts” button at the top of the page.

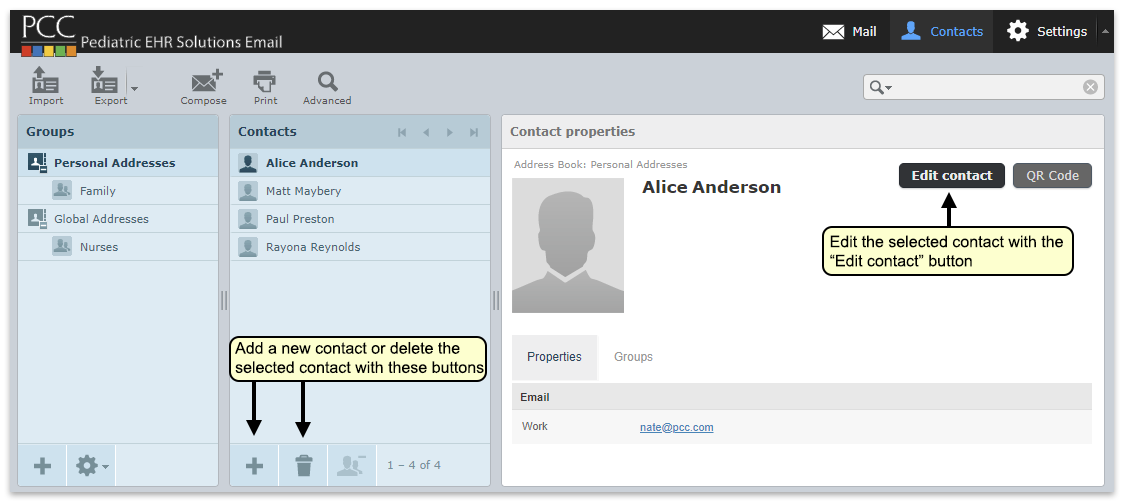
You can add, remove, and edit contacts from your address book. Contacts in your address book will auto fill in any of the “to” fields when you compose email.
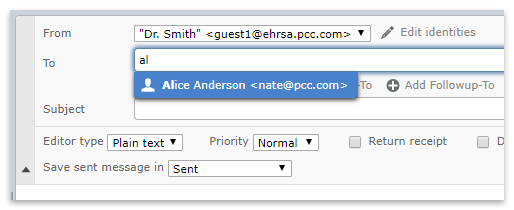
Contact Groups
You can add addresses to Contact Groups. You can then send an email to an entire group just by selecting the group, instead of manually adding each email.
On the Contacts Page, click the Plus icon to add a group.
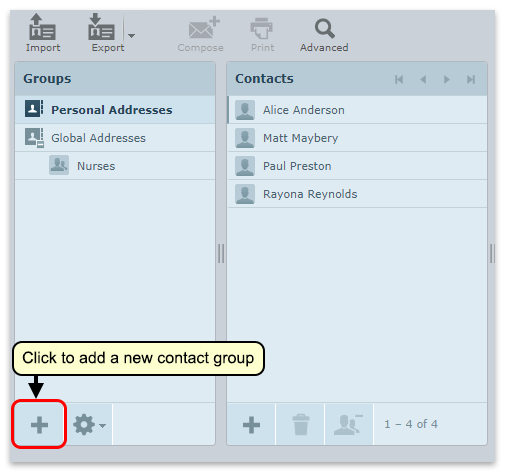
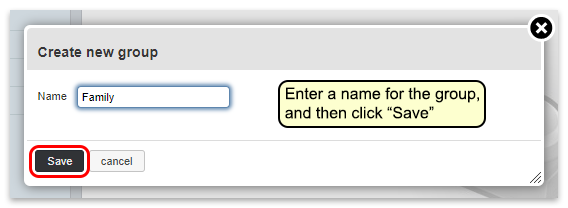
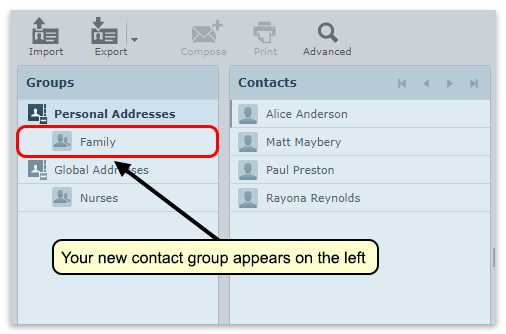
Then, drag contacts from your contact list into the group.
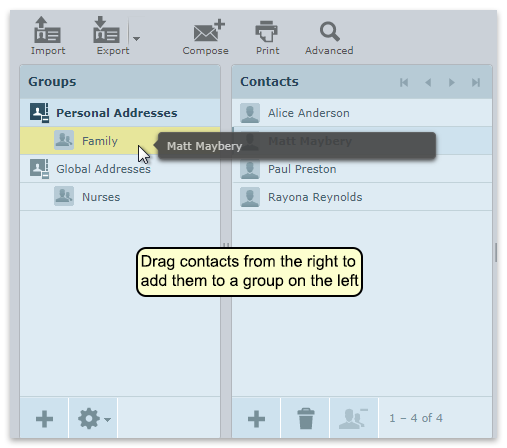
When composing an email, entering the group name into the to/cc/bcc fields will add all contacts in that group.
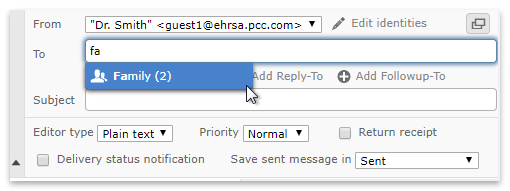
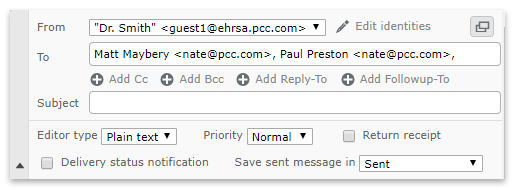
Global Addresses
Your personal address book is only available to you, but your practice’s administrator can add contacts to a practice-wide, global address book that is available to all email users. Contact PCC Support for help with your global address book.
Vacation Messages
Roundcube allows you set up an auto-reply away message. You can adjust and activate your away message on the “Vacation” window under “Settings”.
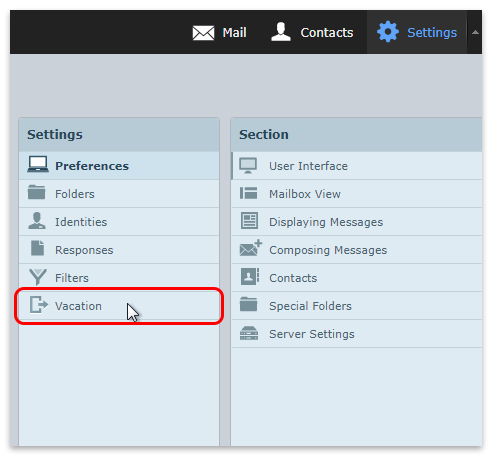
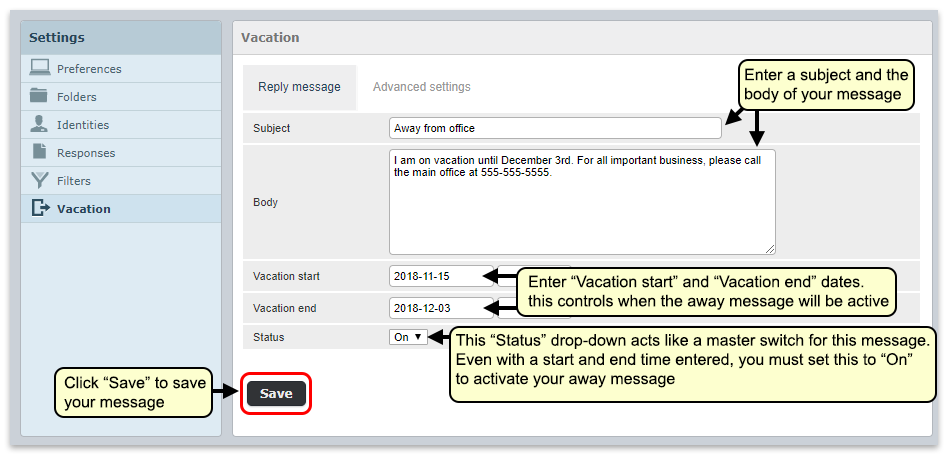
Start and End Dates vs. On/Off Status: You can set specific start and end dates for your away message so that it will automatically activate on a specific date and turn off on a subsequent date. You can also manually turn your message on and off by leaving the start and end times blank and using the Status drop-down to turn the message on and off. Note that if the Status is set to “Off”, your away message will not be sent, even if there are start and end dates set.
Use Two-Factor Authentication with Your PCC Email
You can use two-factor authentication with your PCC RoundCube e-mail. Two-factor authentication (“2FA”, “2-Factor Authentication”) improves the security of email services and is recommended for use in a medical setting or other environment where confidentiality is important.
Why Should I Use 2FA?: There are many reasons you should use two-factor authentication for your practice’s email. 2FA improves the security of your practice’s communication, which may include PHI, sensitive business data, contact information for patients and staff, and other data that should be secured. 2FA helps you comply with security rules that may affect your practice. Your practice’s cyber insurance may requires 2FA, or charge a higher rate if you do not use it. Additionally, PCC began requiring 2FA for all new client installations in 2022, if the practice opts to use PCC’s email service.
Activate Two-Factor Authentication for Your Practice
Your practice can use 2FA on a person-by-person basis, or you can require it for all staff that use PCC’s email service. Contact PCC Support for help.
PCC implements 2FA for all new clients by default. Your practice can decide to opt-out.
When 2FA is required by your practice’s configuration, users will see a warning message and be unable to read their PCC RoundCube email until they activate two-factor authentication.
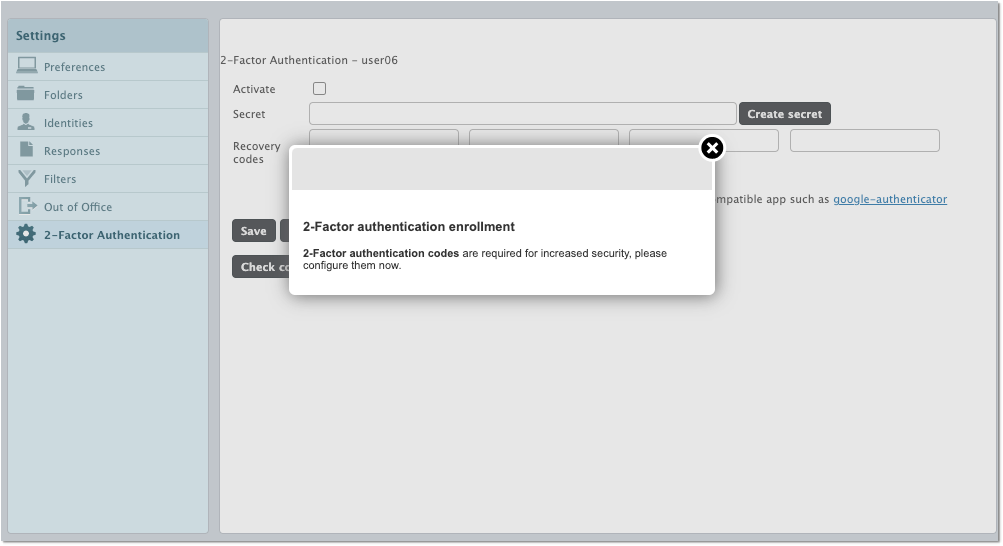
At a future date, PCC may decide to make two-factor authentication a requirement for all practices that use PCC’s e-mail service.
Activate Two-Factor Authentication for Your Personal PCC Email Account
Whether your practice requires 2FA for PCC email or not, each individual user can enable it for themself.
Follow the procedure below to set up two-factor authentication for your PCC email.
Install Authy on Your Mobile Phone
Install the “Authy” application on your mobile phone or other mobile device you will use to generate tokens. You may already have Authy installed if you use Direct Secure Messaging, PCC eRx, or another service.
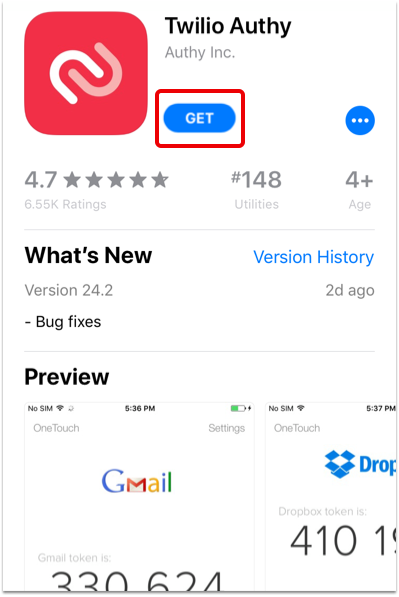
Why Does PCC Recommend Authy?: While you can use many different 2FA applications, PCC has experience with Authy and can provide basic support. Additionally, Authy allows the user to create a recovery backup password, which means you can transfer your tokens to a new phone should you lose or replace your current one.
Log In To Your PCC Email
Log in to your PCC RoundCube email account.
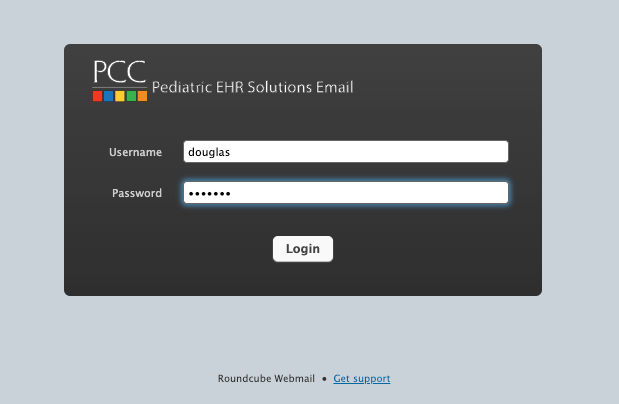
Click “Settings” and “Two-Factor Authentication”
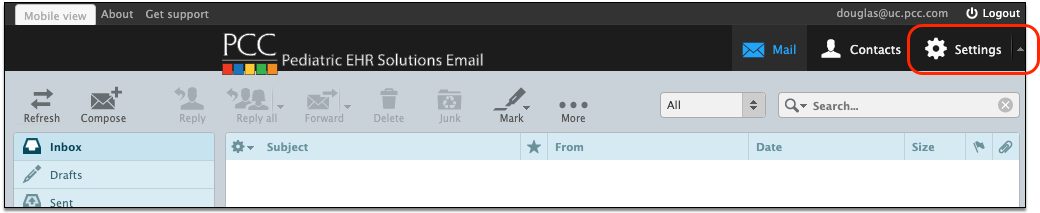
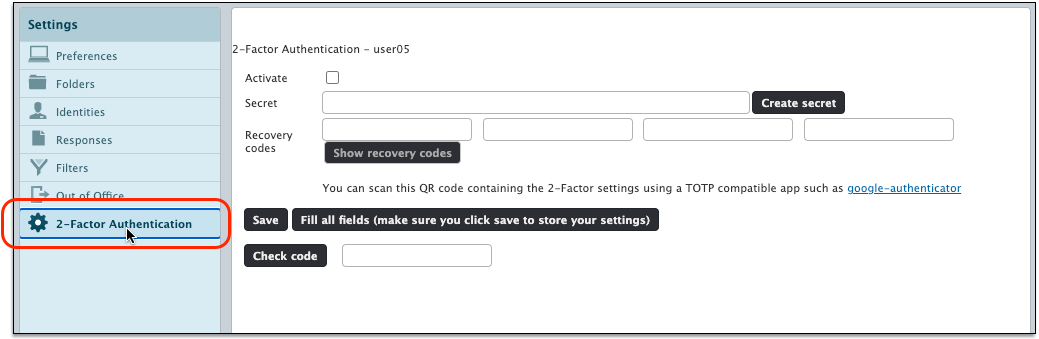
Click “Fill all fields…”
Click the “Fill all fields…” button to generate a unique secret, recovery codes, and a QR code that will make setup easy.
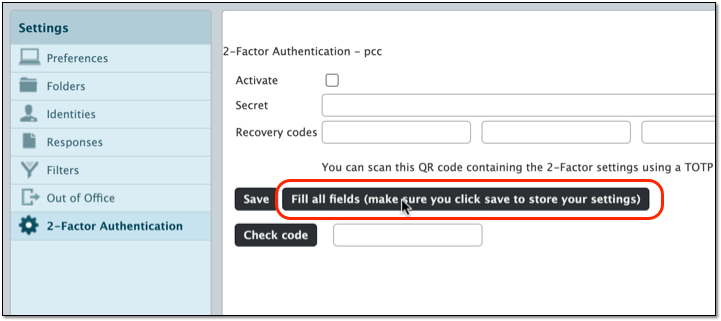
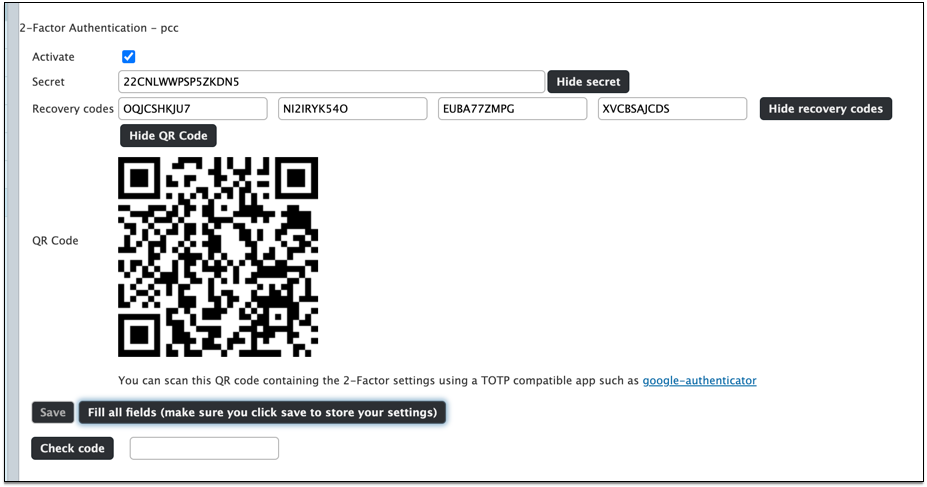
Use the Authy App to Create the Connection
Follow the onscreen prompts in Authy to create a new connection.
Create a New Connection, Can't Re-Use: You may already use Authy for other services (like PCC eRx or PCC SecureConnect). You can not reuse those connections, but must instead create a new connection in the Authy app, specifically for you PCC Roundcube email.

You will be prompted to name your connection, for easy reference later.
Create a Backup Password in Authy
When you use Authy to create a connection, you will be prompted to create a backup password. This optional step can help you later if your phone is lost, stolen, or replaced.
Backup Password is Highly Recommended: If you do not create a backup Authy password, you will be unable to access your e-mail if you lose your phone. PCC recommends you create a backup Authy password so you can reactivate your secure connections when you switch to a new phone.
Scan the QR Code
During the process, Authy will prompt you to scan a QR code (or enter a text code manually). You can find the QR code in the Two-Factor Authentication panel in RoundCube. (You can also click “show secret” to view the code and enter it into your phone manually.)
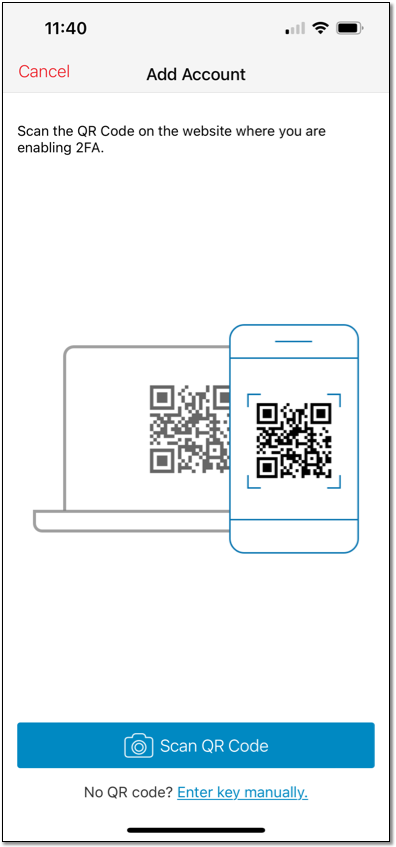
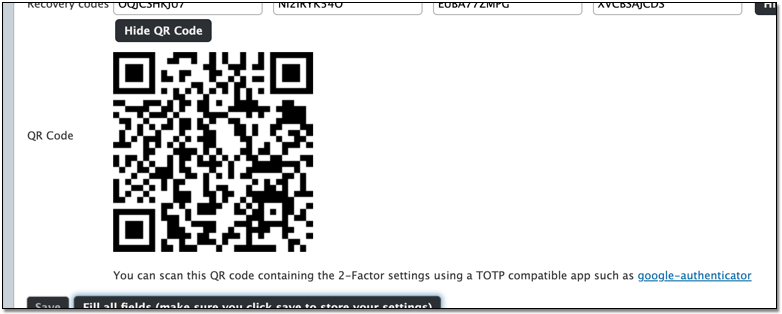
Test a Token
The Authy app will now generate a new RoundCube PCC email token every 30 seconds.
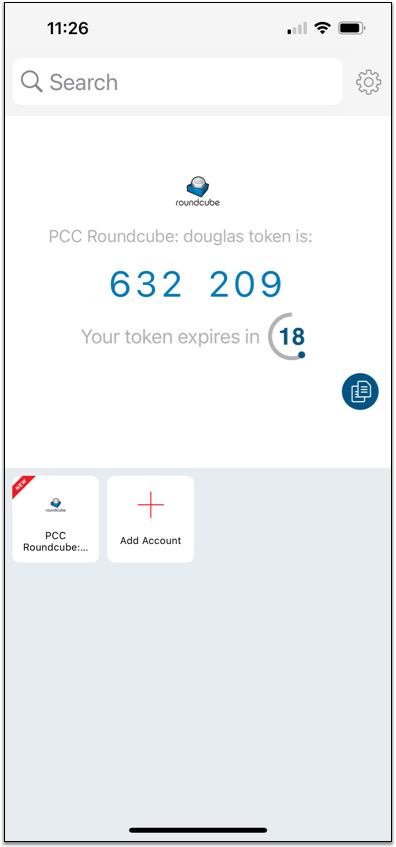
To test your two-factor authentication setup, enter the code from the Authy app into the “Check code” field in RoundCube and click “Check code”.
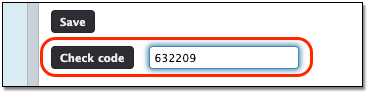
You will see a pop-up message letting you know that two-factor authentication is now working.
Review Recovery Codes, Screenshot or Print Your Screen
RoundCube has automatically generated a secret and a set of recovery codes. The recovery codes are temporary token passcodes that expire after they are used once.
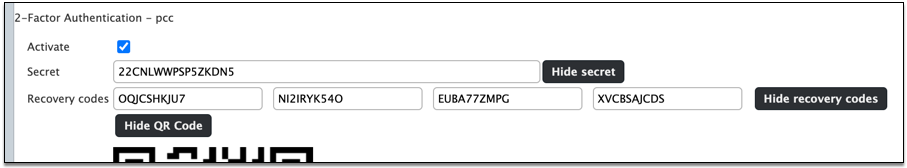
Print or take a screenshot of this page so you can store your recovery codes. They will allow you to access your email, even if you’ve lost your phone.
Click “Save”
Click “Save” to enable two-factor authentication whenever you log into your email account.
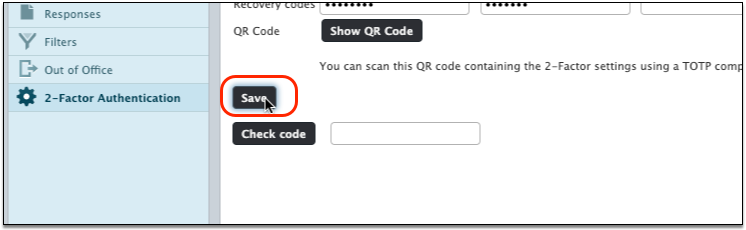
Test Your New 2FA Email Login
Log out of your email account and log back in.
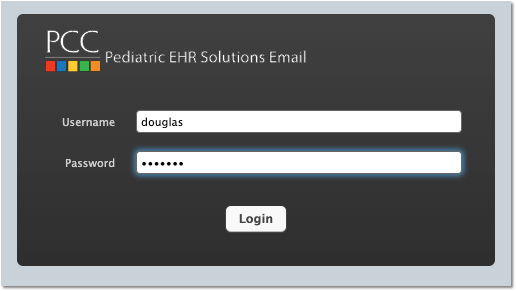
After entering your username and password, you should be prompted to enter a 2FA token.
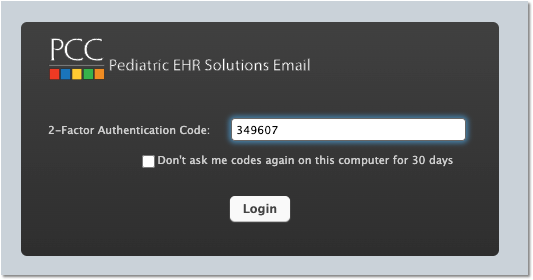
You can retrieve a token from the Authy app on your phone. Optionally, you can click “Don’t ask me codes again…” if you are working in a secure location that does not require two-factor authentication.
Turn Off Two-Factor Authentication, or Reset Your Token
If you need to disable 2FA for some reason, you can deselect the “Activate” checkbox and click “Save”.
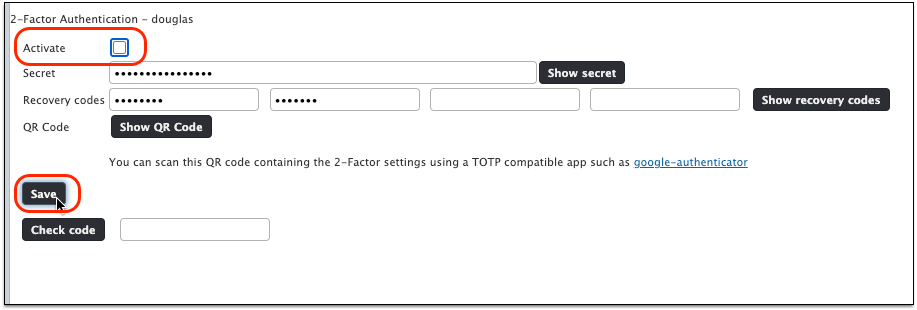
You can re-enable 2FA later.
Lose Access To Your Email: If you get stuck and can not access your email, contact PCC Support.
Create a Custom Report
You can generate and save custom reports and report categories in PCC EHR.
Video Overview: For a video walk-through of custom report creation, watch Create a Custom Report.
Create a Custom Report
When you want more details on a specific data set, customize a report to get the information you need.
Click “Customize Report”
To create a custom report, click the “Customize Report” button at the bottom of any report.
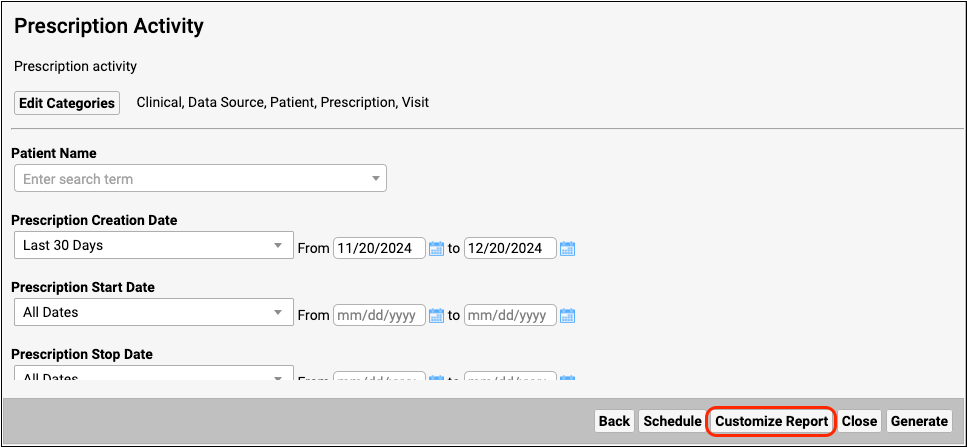
Rename, Describe, and Categorize Your Custom Report
Give the report a new title and description, assign any number of categories, and select which criteria you want to appear on the report.
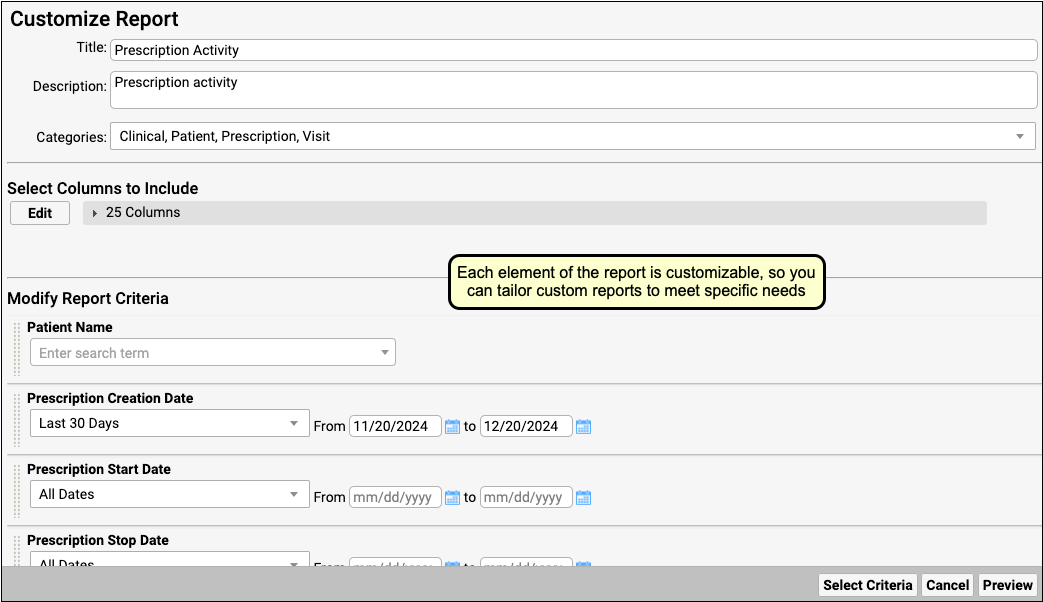
Selection boxes remember your last selection when you run the report.
Select Criteria
Use the “Select Criteria” button to add or remove criteria from a report. This is particularly useful if you are starting from a large Data Source report that contains criteria that are not needed to find the information you need.
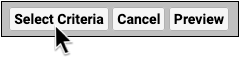
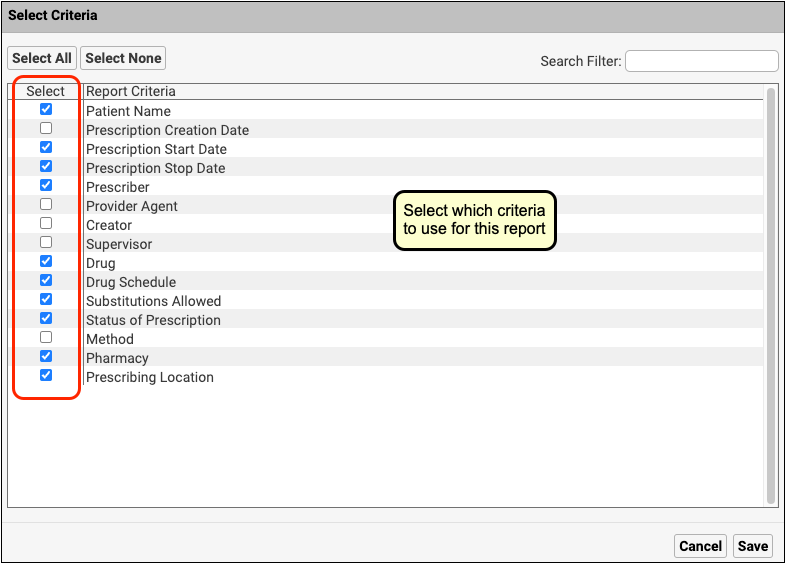
Select Columns
Click “Edit” under “Select Columns to Include”, then choose which columns to include in the report. The more columns your report includes, the longer it will take to generate.
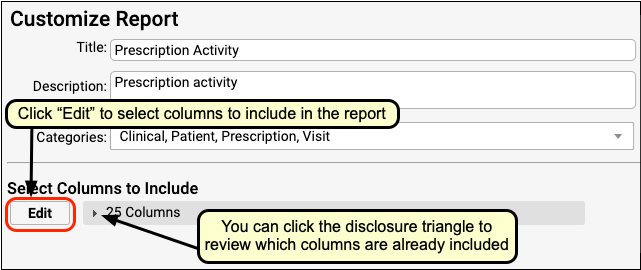
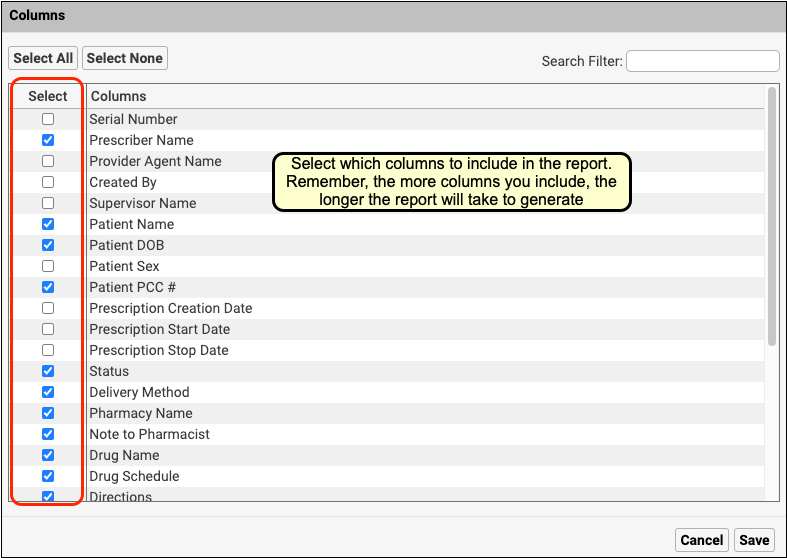
Set Defaults and Preview
Set criteria selections that you want to display by default, then click “Preview”.
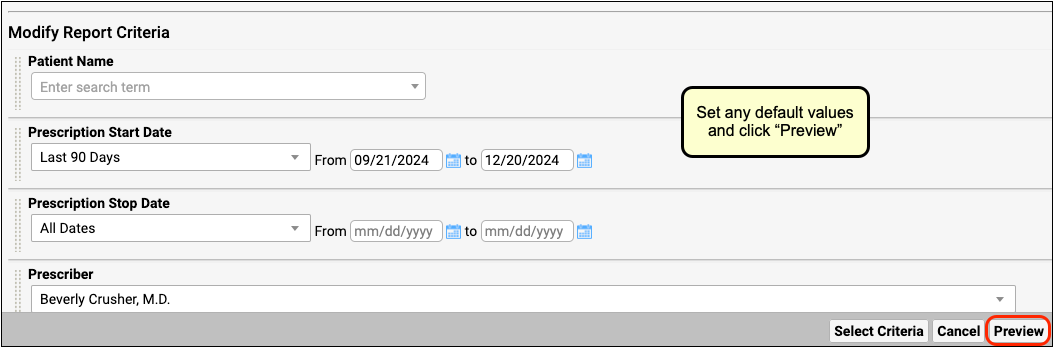
Refine Default Output
In the report preview, select which columns will display by default when you run the custom report.
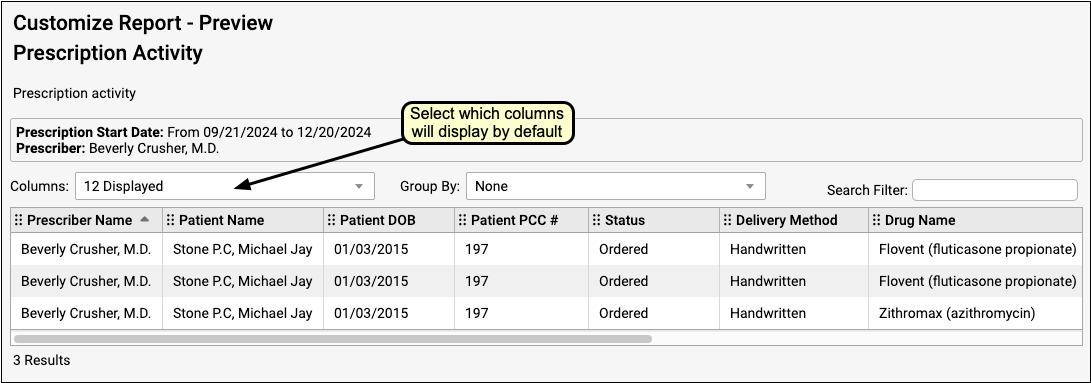
You can click “Back” to make criteria adjustments.
20,000 Row Limit: Reports in the Report Library are currently limited to 20,000 rows. If your output appears to be exactly 20,000 rows long, it may not contain all of the information that you are looking for. If this occurs, return to the Criteria screen and limit your report criteria until your rows are under 20,000. If all of your current criteria settings must be included in your report but you are still hitting the 20,000-row limit, contact PCC Support for help creating a specialized report.
Save Your Custom Report
Click “Save As” to make final adjustments to the report title and description. Then click “Save”.

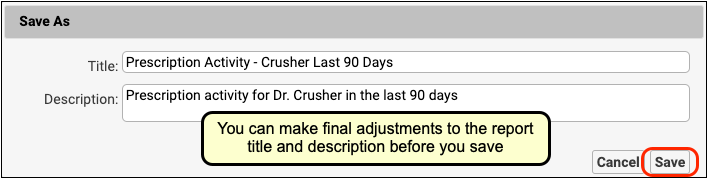
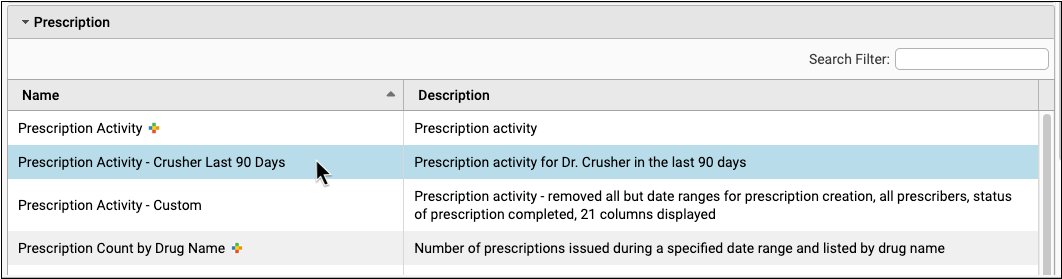
Once you have saved your new report, you can run it just like any other report. It will appear alphabetically in each report list category that you assigned it to.
Get the Most Out of Your Reports
To get the most out of your reports, start by identifying the precise information that you want to collect. Then restrict your report criteria to display only your desired information.
Refine Your Question
Think about the question you’re trying to answer before creating your report and see if you can narrow it down to a key data set.
Example question: Which active patients with an Asthma diagnosis were prescribed an inhaler in the last three months?
Restrict by Date
Restrict your reports by date when possible for faster reporting. Ensure that your date range is specific to the question that you are asking.
Remove Criteria When Possible
Remove extraneous criteria from the Select Criteria window. The more criteria that the report needs to evaluate, the longer it takes to run.
Reduce Column Volume
Choose only the columns that provide information essential to your question. Edit the Columns criteria when customizing and remove unnecessary columns.
Think Critically About Default and Filtering Criteria
The inclusion of certain criteria may cause information to be left out of a report. Think carefully about each criterion that you set, remove, or leave as a default.
For example, the default Document Modification report includes a timestamp set for 8am-5pm, which prevents patients who were seen after hours from appearing on the report output. You can remove the timestamp when customizing so that your report output includes patients seen after hours.
Another example is the Last Visit Date criterion in the Patient List report, which excludes patients who have not had a visit. If you want a list of all active patients regardless of whether they’ve had a visit, remove the Last Visit Date filter criterion when customizing the Patient List report.
Set Limits on Data Source Reports
Data Source reports contain many criteria to choose from, but these reports are most useful when pared down. Make sure to remove all criteria that do not pertain to your question when customizing a Data Source report.
Use Data Source Reports to Start a Custom Report
The Data Source report category contains a number of master reports with extensive filter sets, which may be perfect for using as a foundation for custom reports. If you want to go beyond adjusting a report that already exists and create something totally new, a Data Source report is a great place to start.
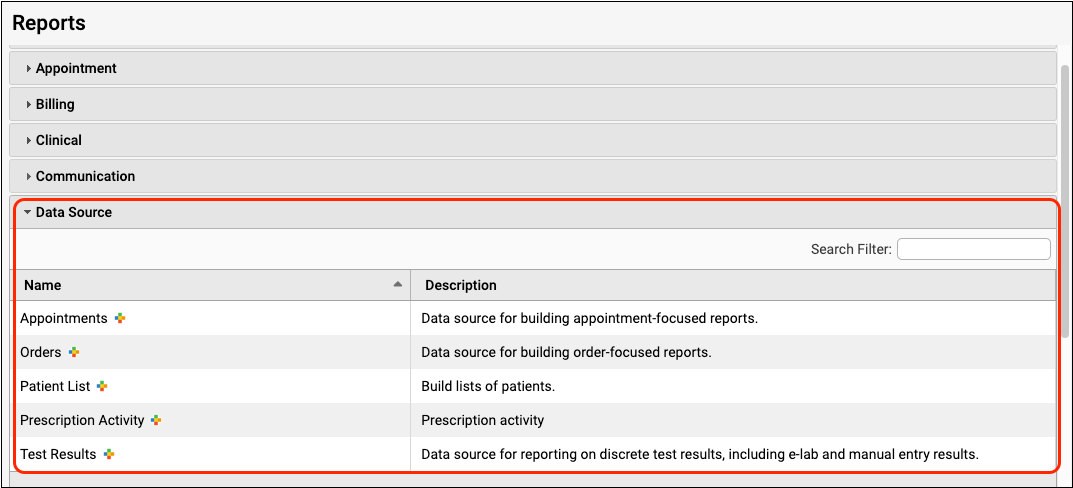
Edit or Delete a Custom Report
You can return to your custom report to edit it again at any time. When you open the report, click the “Customize Report” button.
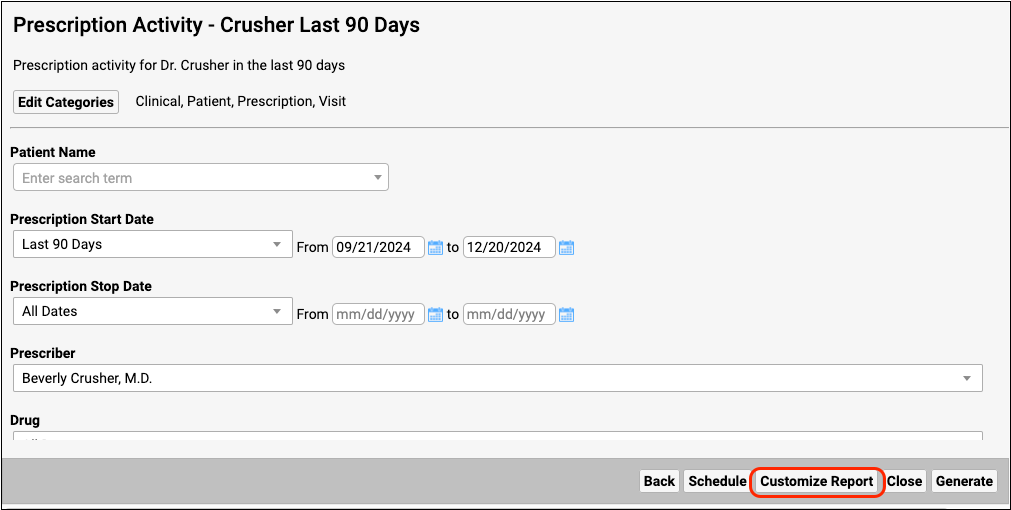
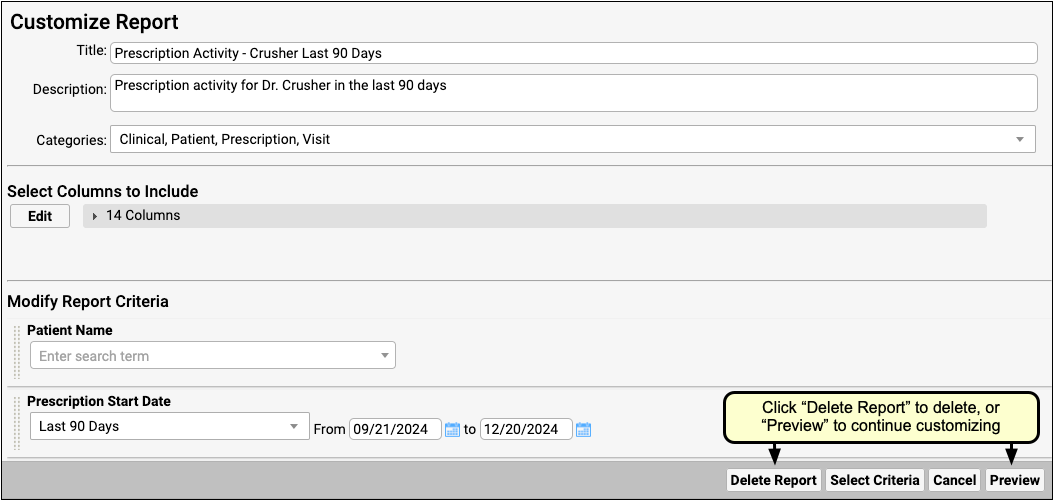
Click “Delete Report” to delete your custom report. Click “Preview” to continue customizing.
Create Custom Report Categories
The Report Library in PCC EHR organizes reports into categories. Your practice can create its own custom categories and can choose which roles have access to specific report categories.
Manage Categories
Click the “Manage Categories” button at the bottom of the report list.
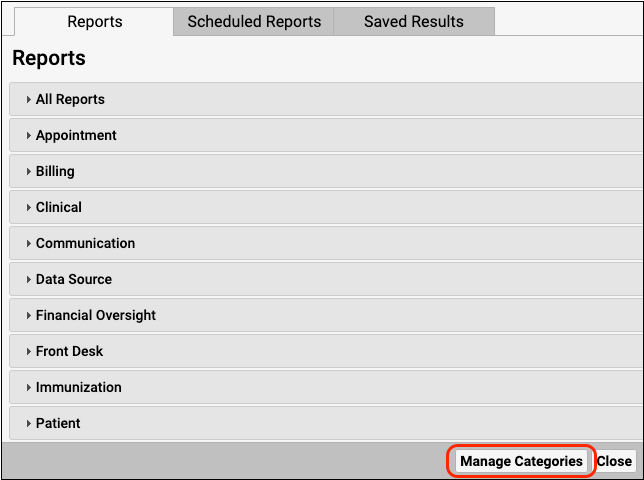
You can add, delete, or edit categories from the Manage Categories screen.
Add a New Category
Click “Add” in the Manage Categories screen to create a new category.
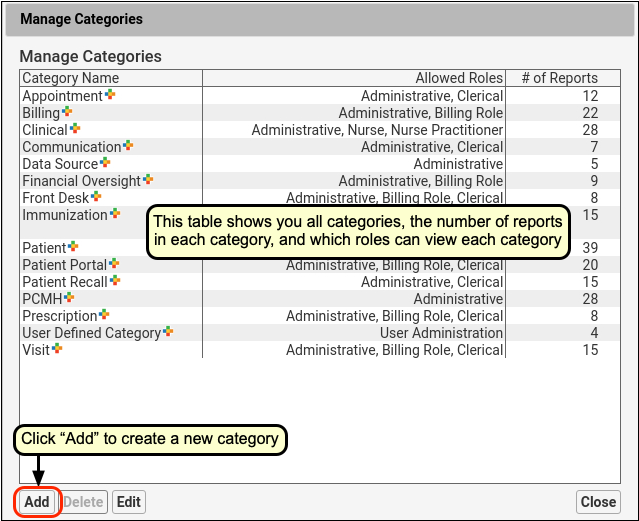
Configure Category Name and Role Access
Enter a name for your new category and select the roles that can view this category. Then click “Save”.
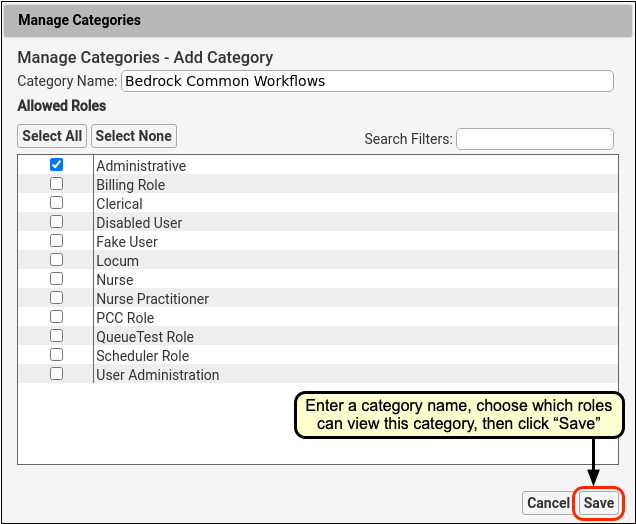
Category Access is Role-Specific: Categories are not user-specific; they are available to everyone with the roles you select in the Manage Categories screen. To find out more about how to limit access to specific categories, read Restrict Access to Reports in the Report Library.
Review and Close
Review your choices and click “Close” to exit the Manage Categories screen.
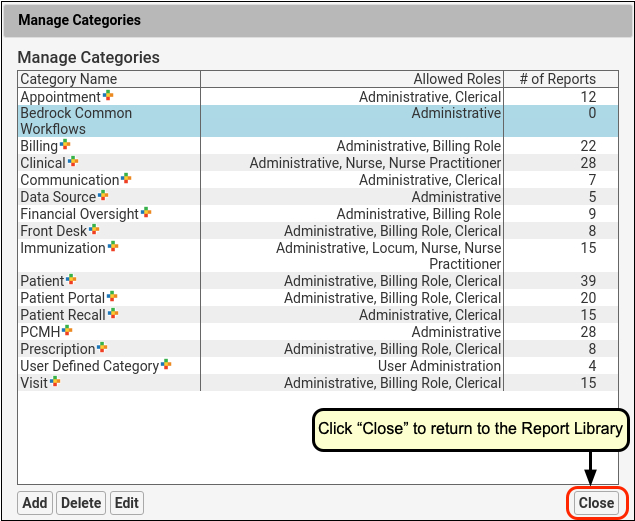
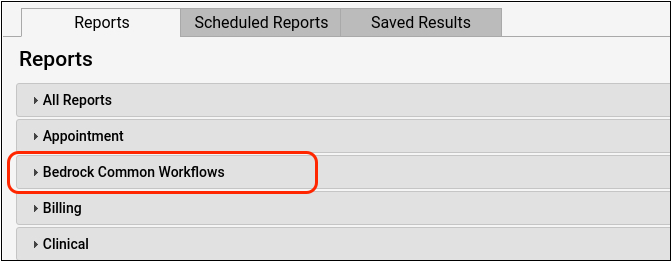
Add a Report to a Custom Category
Once you have created a new custom category, you can add any report to it. The categories that the report is already assigned to are displayed in the Categories column in the report list as well as at the top of the open report.
Select the Report
To add a report to a new category, open the report in the report list.
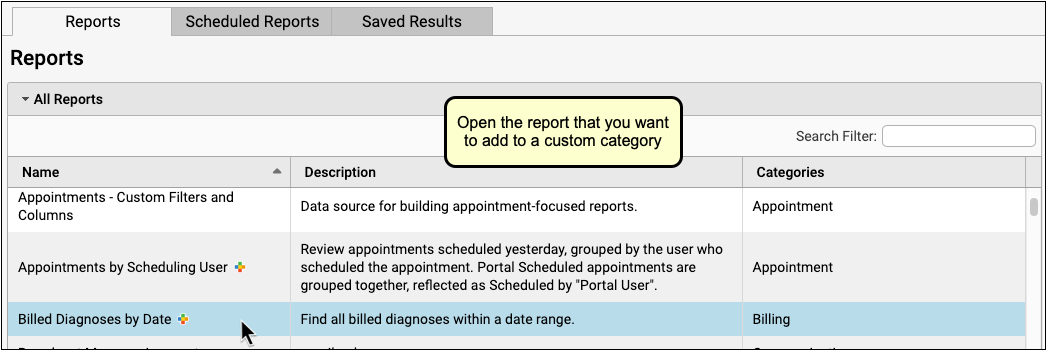
Edit Categories
Click “Edit Categories” to change the report’s category settings.
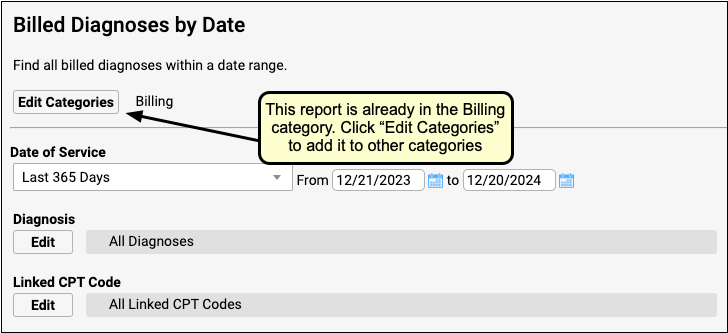
Configure Categories and Save
Use the checkboxes to add and remove the report from categories, then click “Save”.
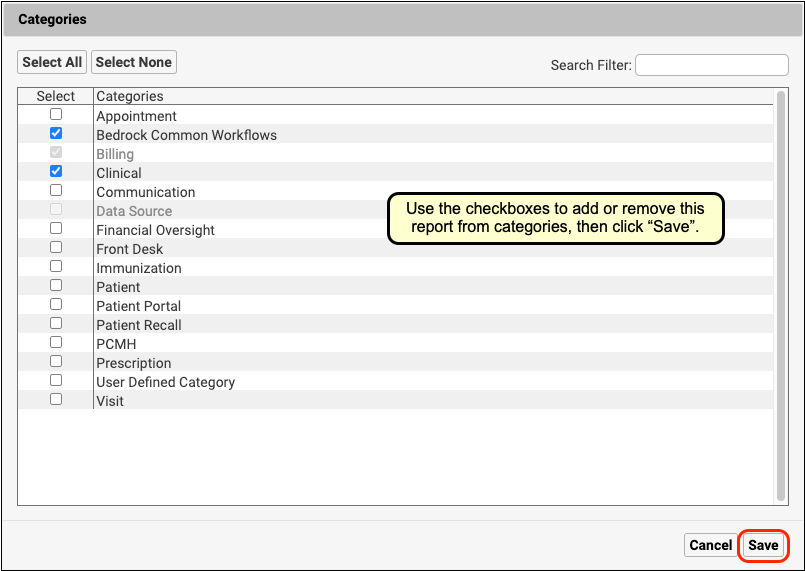
Stock reports cannot be removed from their default categories.
Review Category Changes
You can review the category settings in the report list and within your report.
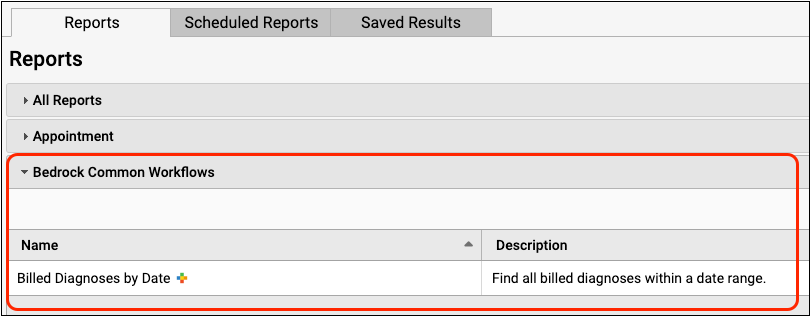
You can click “Edit Categories” within the report to make further changes.
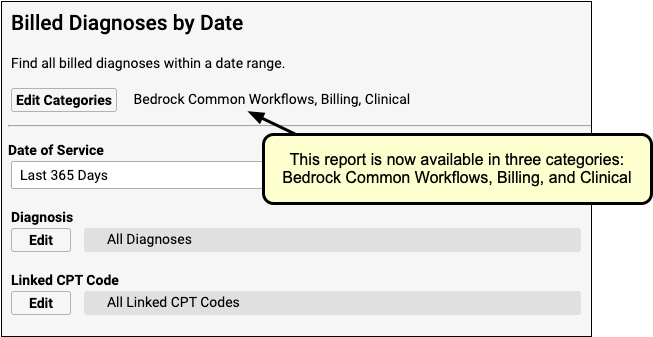
Enter Vitals in pocketPCC
Does a nurse need to carry around a cumbersome laptop just to record height, weight, and blood pressure? Maybe there’s a better way.
Clinicians can view and enter vitals in a large, easy-to-use interface on their iPhone, iPad, or other mobile device.
Edit the Visit to Enable Vitals
Once a patient has been “Checked In” or “Arrived” in PCC EHR, you will be able to access their visit from the Visit History in pocketPCC.
Select the patient from the schedule, and then use the Chart menu to find the visit from the Visit History.
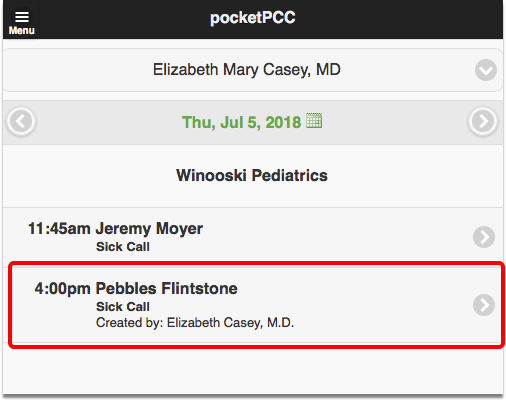
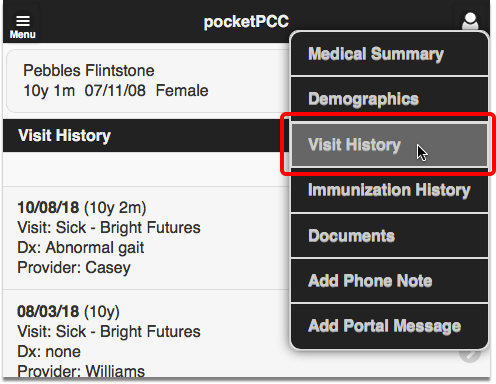
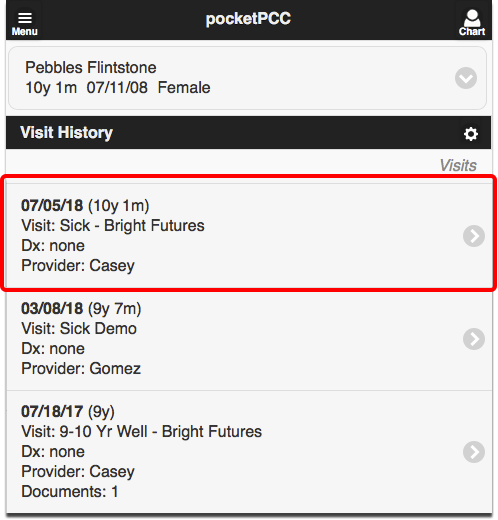
When you are viewing a visit in pocketPCC, you can enter or edit vitals by clicking the “Edit” button.
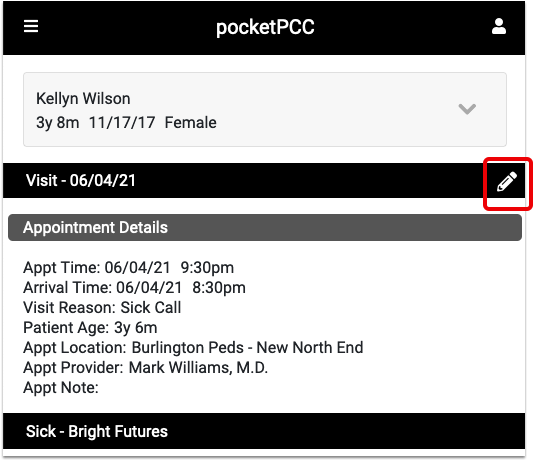
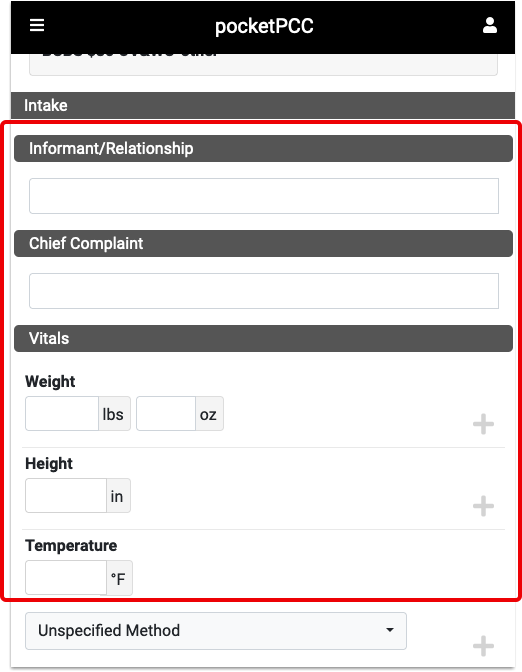
Enter or Edit Vitals
The Vitals component will display the same fields that are configured to appear for the visit type in PCC EHR.
Clicking “More” will show all possible vitals measurements.
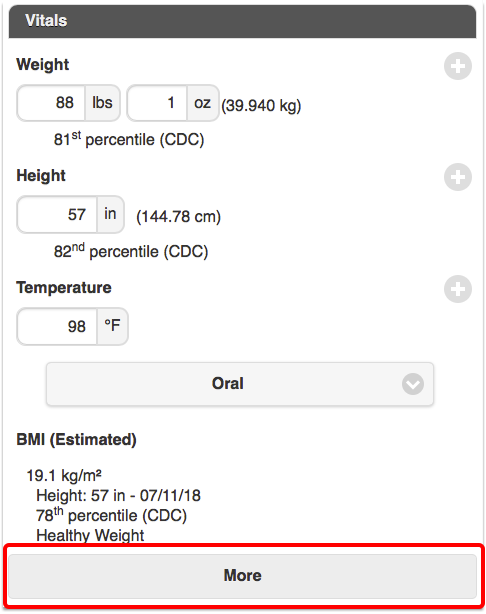
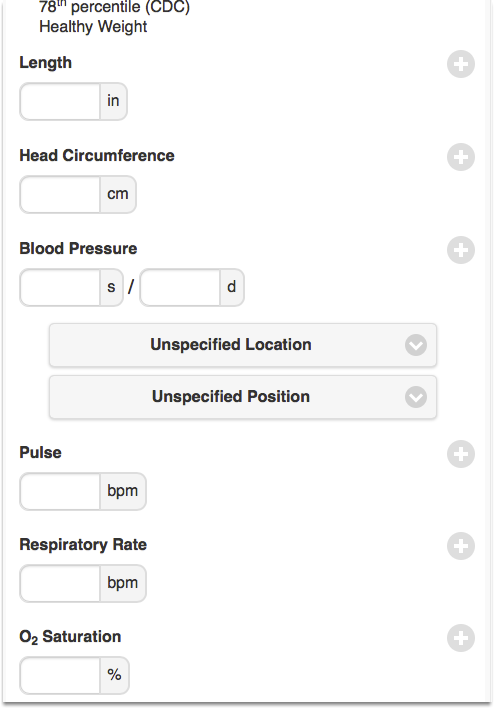
You can enter as many vitals as you need to for the same visit.
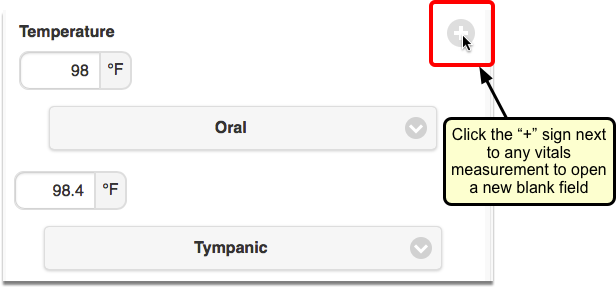
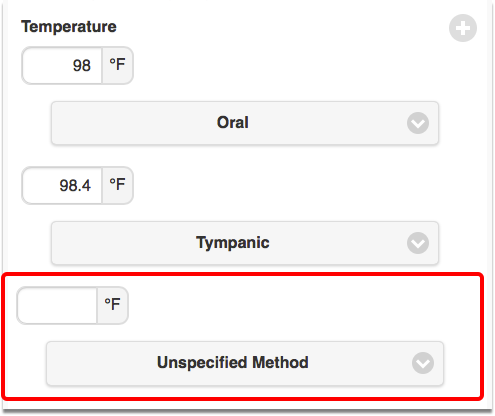
Integration with PCC EHR
Vitals entered in pocketPCC will show up immediately in PCC EHR, everywhere that vitals are displayed. You can edit any vitals that you entered, and you can see who entered other vitals by hovering over the vitals measurement.
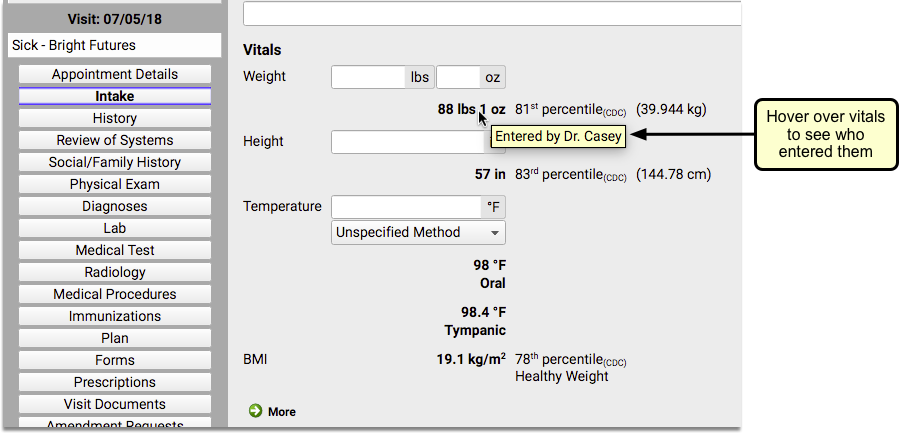
Always Log In As Yourself: It is important that when using pocketPCC at your practice, you don’t just hand off the device between staff members. Make sure that you log in individually, so that in addition to having your username connected with your vitals entries, you also don’t commit a HIPAA violation.
Configure Patient Check-In
You can configure Patient Check-In in PCC EHR to meet the specific needs of your practice. You can adjust what components appear, create custom headers for your front desk staff, and create custom Patient Check-In Clinical Alerts.
Read the sections below to learn the different tools and features for Patient Check-In.
Watch a Video Instead?: You can learn about how to configure Patient Check-In to meet the needs of your practice by watching the Patient Check-In Configuration Video.
Configure the Check-In Protocol, Add or Remove a Component
Like other screens in PCC EHR, your practice can decide exactly which components should appear on the Patient Check-In protocol. You may decide to add useful components like Forms or Care Plans, and you can rearrange components or create custom notes that you want staff to see whenever a family checks in.
To get started, open the Patient Check-In Builder in the Protocol Configuration tool.
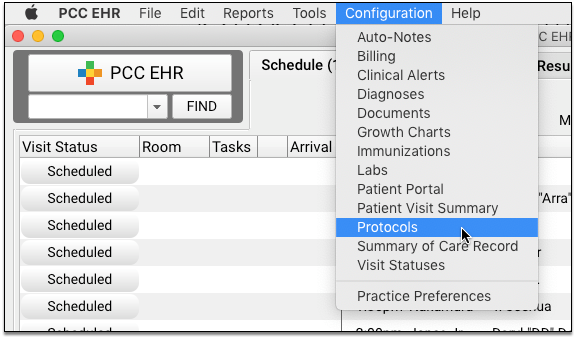
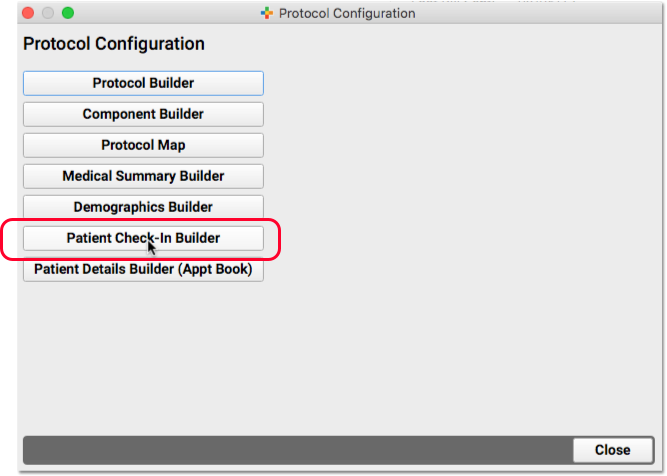
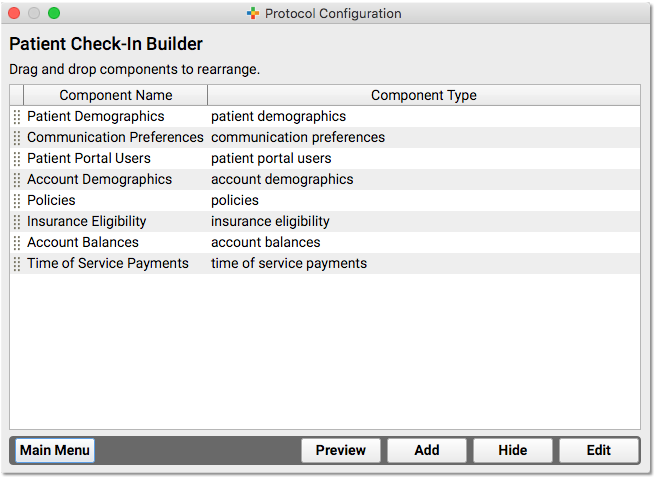
The default Patient Check-In components are shown in the image above. They include Patient Demographics, Communication Preferences, Patient Portal Users, Account Demographics, Policies, Insurance Eligibility, Account Balances, and Time of Service Payments.
You can click and drag the handle on the left to rearrange components, or click “Hide” to remove a component.
Click “Add” to add a new component.
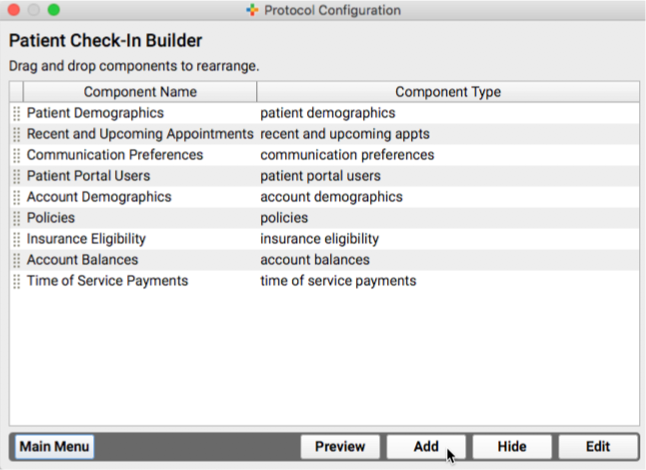
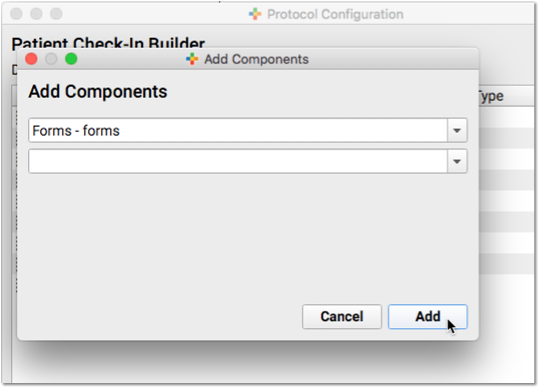
Double-click or select and click “Edit” to adjust any available configuration options for a component.
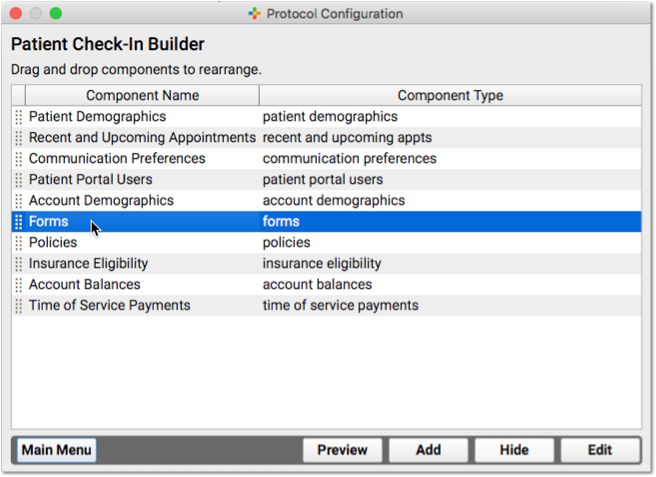
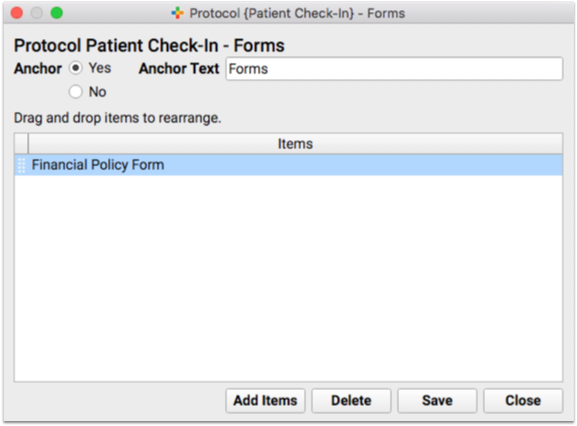
For example, you can change the contents of some components and change the anchor button text.
Create a Custom Headline and Notes Field in Patient Check-In
Do you want a custom component, featuring a headline and a notes field that your front desk staff will see every time they open the window? You could use this record any persistent, chart-wide information for the patient or family.
You can add a headline and notes field by creating a new chart-wide component.
First, open the Component Builder and visit the “Chart-Wide” component list. Create a new component.
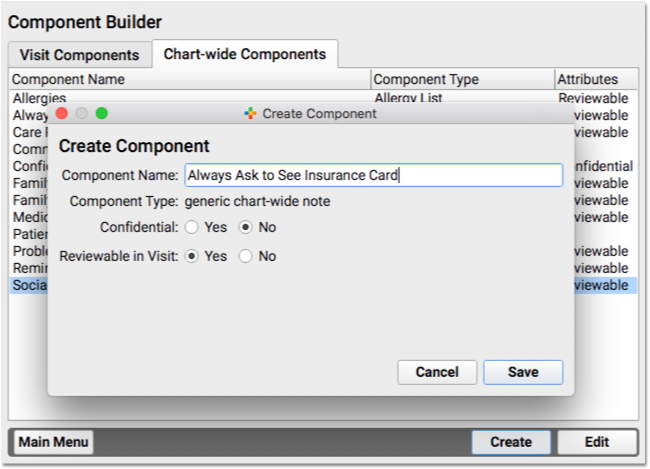
Next, use the Patient Check-In Builder to add the component to your Patient Check-In protocol.
The component will appear when you check in a patient.
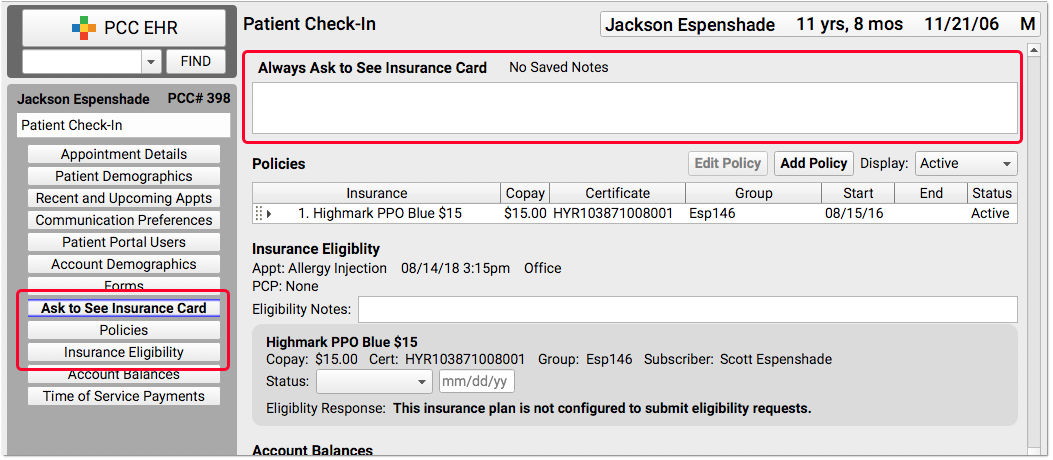
For more information about available components, read the PCC EHR Component Reference. For more examples of how to edit protocols, read the Edit Protocols article.
Custom Alerts During Patient Check-In
What kinds of things do the front desk staff need to know when they check in a family? Billing issues, incomplete forms, important announcements and reminders? Maybe you track a patient’s preferred pronoun, when it is different from the sex in their chart record?
Your practice can create Clinical Alerts to inform them of these issues. When you create a Clinical Alert, you can indicate whether it should appear when a chart is opened or saved, and/or when the patient is checked in.
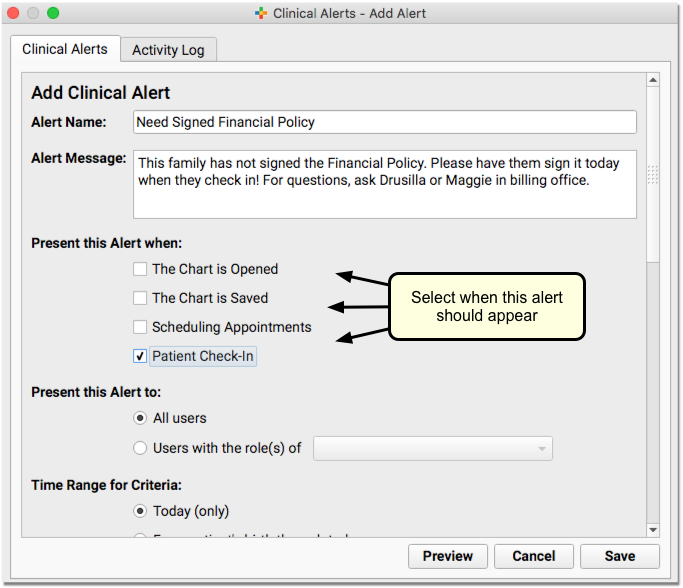
You can base the alert on a wide range of available criteria, including patient or account flags, demographics, or other details. This is the perfect tool for common patient and family status flags, like Billing Problem, Privacy Notice, or other clerical needs.
All Staff Alerts: If it’s important that the entire staff see an alert, make sure you check each appropriate box. Opening and saving the chart are not the same as Patient Check-In, for example.
For a guide to creating and editing Clinical Alerts, read the Clinical Alerts help article.
When someone checks in a patient who matches the criteria for an alert, it will appear along with your message about the topic.
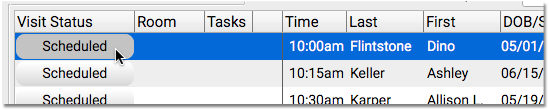
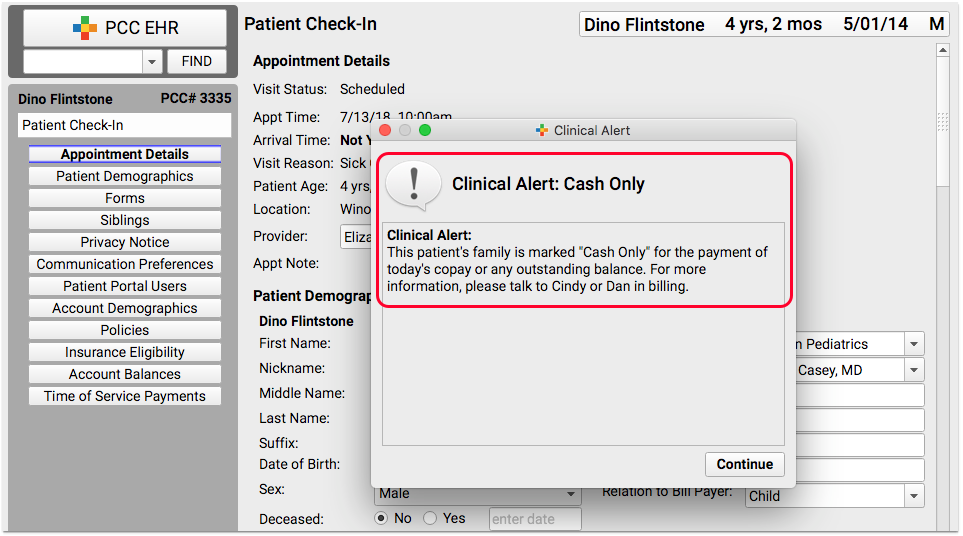
Check In a Patient
When a patient arrives at your practice, use Patient Check-In to check them in. Patient Check-In will help you review the family’s demographic and insurance information, check insurance eligibility, review outstanding balances and post payments, and more.
Watch a Video: You can learn how to check in a patient by watching Patient Check-In Video. The video covers the topics in this article.
How to Check In a Patient
When a patient checks in, do you review their address, update their policy information, and collect copay? What else do you say when you greet the parent? Your practice can customize the Patient Check-In protocol to meet your needs.
Follow the procedure below to learn about a typical Patient Check-In, including a number of useful tools.
Find the Appointment and Click on the “Scheduled” Status
When you are ready to check in a patient, click on their appointment’s “Scheduled” status on the Schedule queue.
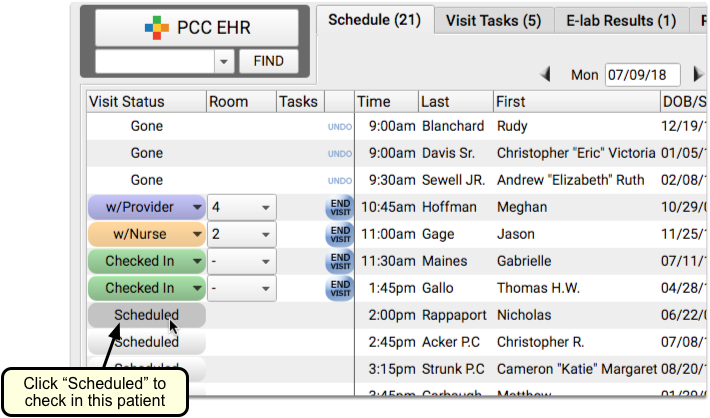
Alternatively, you can highlight the appointment and click on the “Patient Check-In” button.
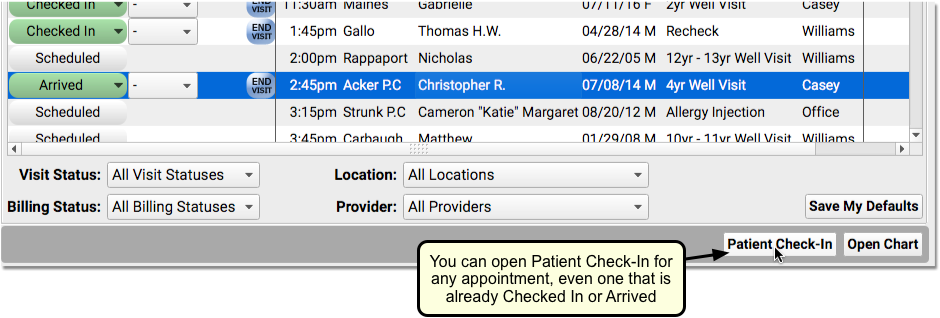
Optional: Review Patient Check-In Alerts
Your practice’s custom Patient Check-In alerts may appear when you begin to check in a patient.
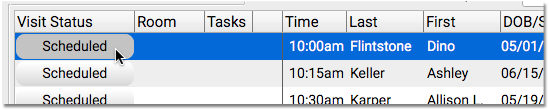
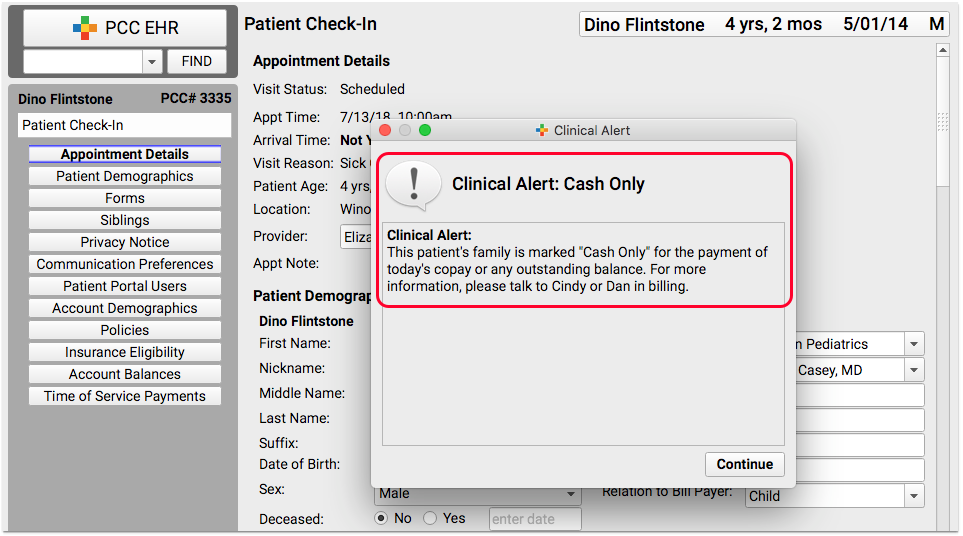
Review these alerts. They may include important details that you need to follow-up on with the family.
Review Demographics, Insurance Policies, and Other Components
Use the “Next” button, or the anchor navigation buttons, to review important information with the family.
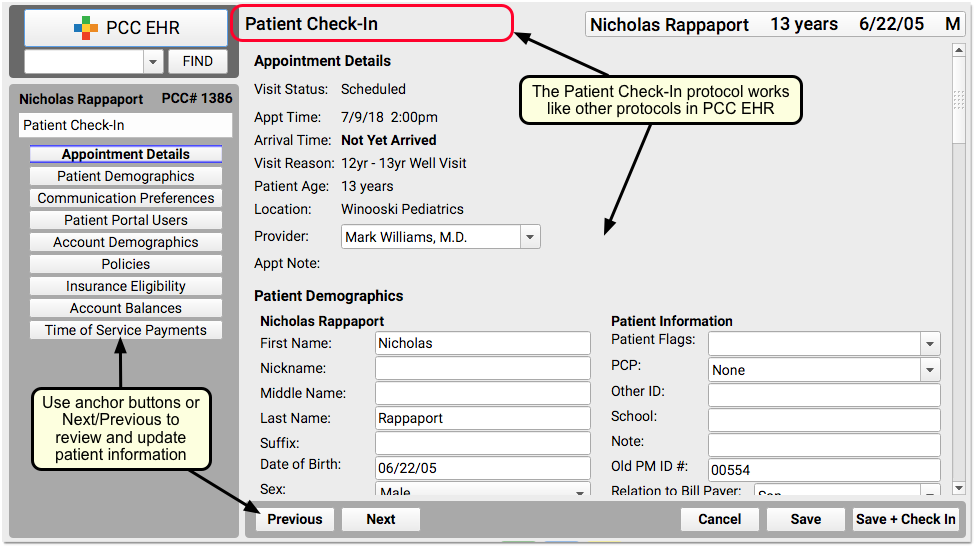
At each visit, do you confirm patient name, appointment information, demographic information, and insurance policies? Use each component on the ribbon to check over these details with the family.
Update Patient and Family Information
Make changes for the patient or the family account right on the Patient Check-In ribbon. For example, you might ask, “Do you still live at 54 Elmwood Road?” and update the account address if it has changed.
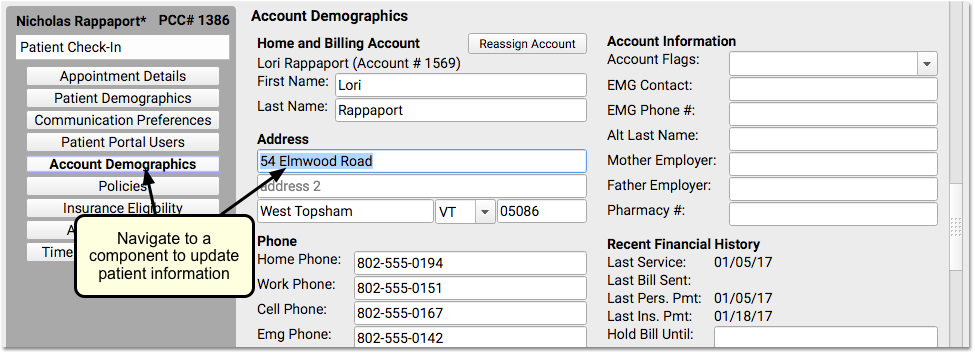
Similarly, you can use the Policies component to add, edit, or expire an insurance policies.
For more information about common demographics components, like Communication Preferences (and Immunization Registry Communication Preferences), Account Demographics, Personal Contacts, and more, read Review and Update Patient and Family Demographics.
Review Insurance Eligibility
Look at the Insurance Eligibility component and check that the patient is validated for today’s visit.
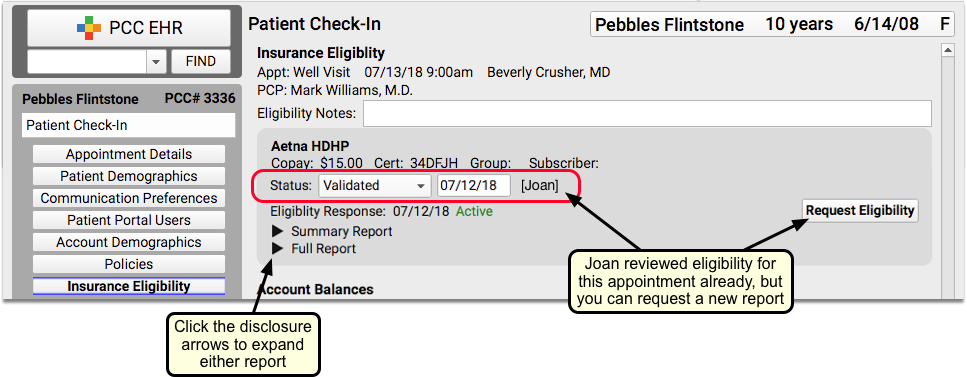
Optionally, you can click a disclosure triangle to look at the Summary Report or Full Report from the insurance carrier. If you just updated or added a new policy, you may want to click “Request Eligibility” to request a new report from the carrier. You can then set a new Status, based on what you learn.
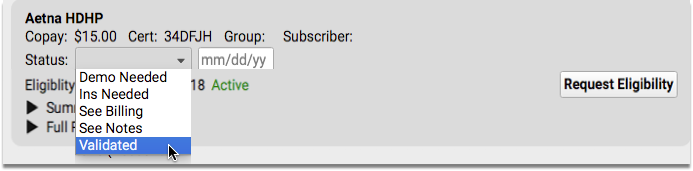
For more information about the Insurance Eligibility component, read Patient Insurance Eligibility with PCC.
Confirm Family is Using the Patient Portal, Help Them Sign Up
Use the Patient Portal Users component to quickly review portal information and help the family with patient portal access.
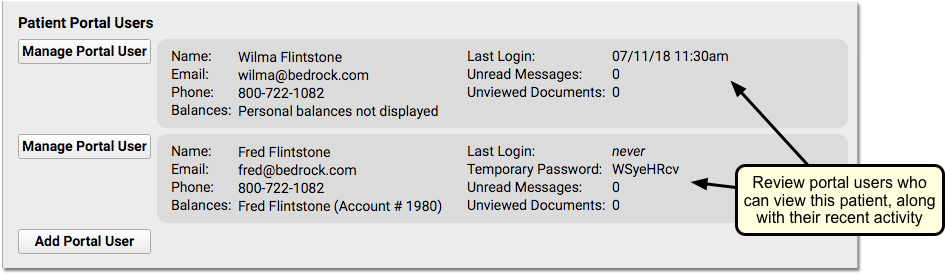
You can see if mom, dad, or another guardian has access to the patient’s records. If the patient has no portal account users, you can click “Add Portal User” to jump into the Patient Portal Manager.
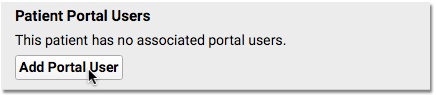
If the family has not logged in, doesn’t have a linked billing account, or needs their password reset, you can click “Manage Portal User” to open up the Patient Portal Manager and help the family with their accounts.
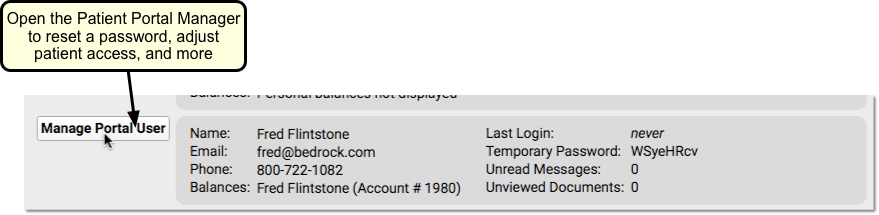
For more information, read Patient Portal User Account Administration.
Review Outstanding Account Balance
Review the Account Balance component to understand outstanding personal charges.
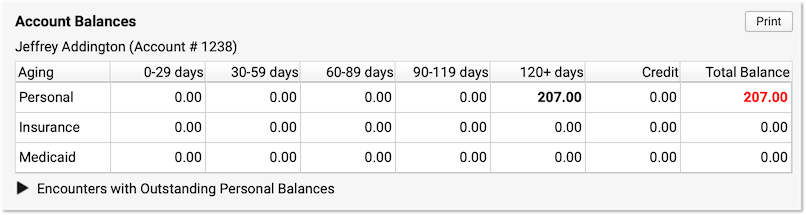
Balances are account-based, so you can see total overdue amounts for this patient and any siblings who share the same billing account. Unpaid balances are broken down into Personal, Insurance, and Medicaid charges. They are aged across aging categories (0-29 days, 30-59 days, etc.), with the total personal balance due displayed in red.
Does the family want to know where the balance comes from? Click the disclosure triangle to view a summary of the charges that have an outstanding personal (non-insurance) balance.
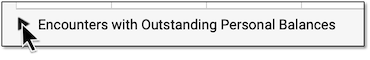
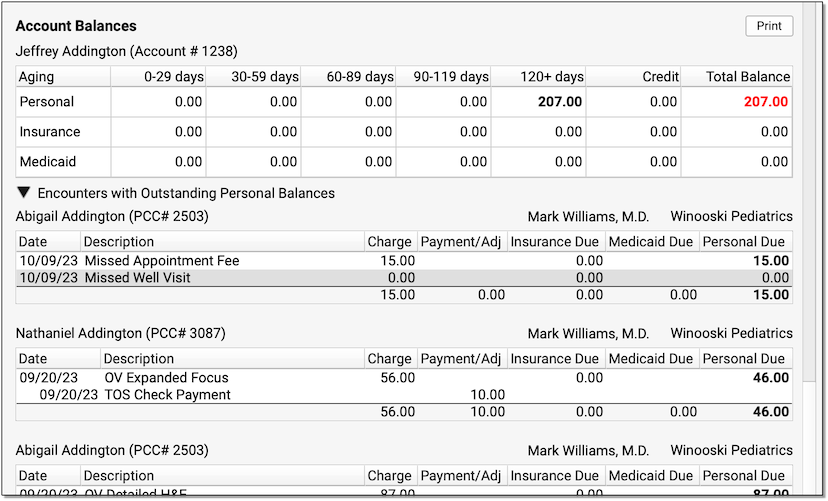
You can see the patient, the date of service, each charge, and a record of all payments or adjustments applied toward the charge so far. You can use these details to explain outstanding charges to the family.
Collect Payment
Use the Time of Service Payments component to post today’s copay, or other amount, toward the account balance. The amount due today will appear in a ledger.
Select a payment type, enter an amount, and if appropriate enter a check number and select a provider. The provider will default to the provider for today’s encounter. As you enter payment details, you’ll see the payment amount appear in the ledger above. You can see the new expected balance before you save the payment.
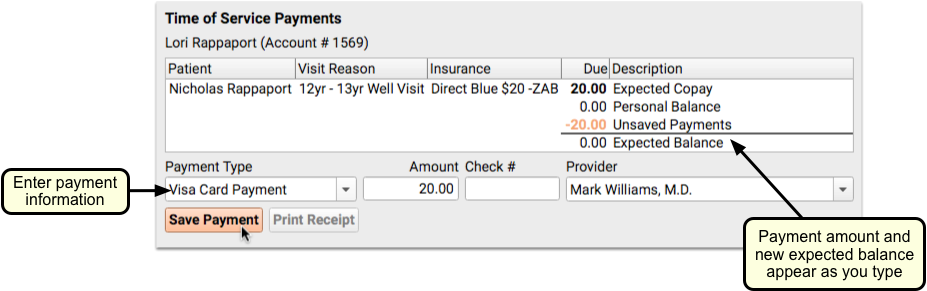
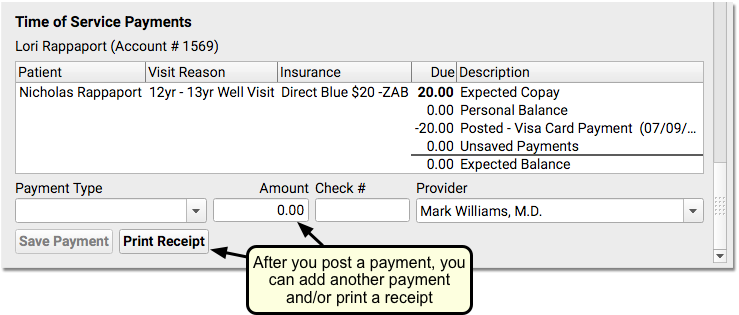
For an account with past-due balances, you can post a single payment for past charges and today’s copay.
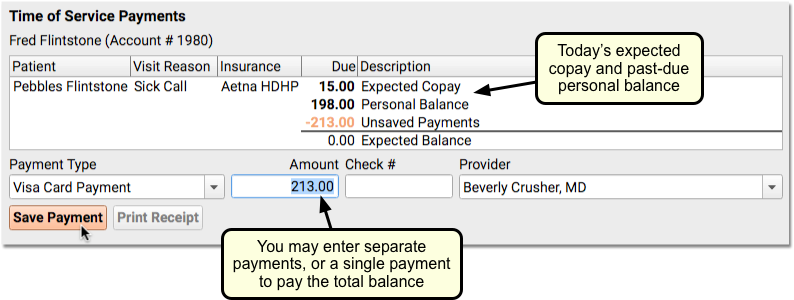
If the account has balances due for encounters related to a sibling, you can clearly see the totals of their copays and outstanding balances. You can post a single payment toward all of the family’s current and past-due balances.
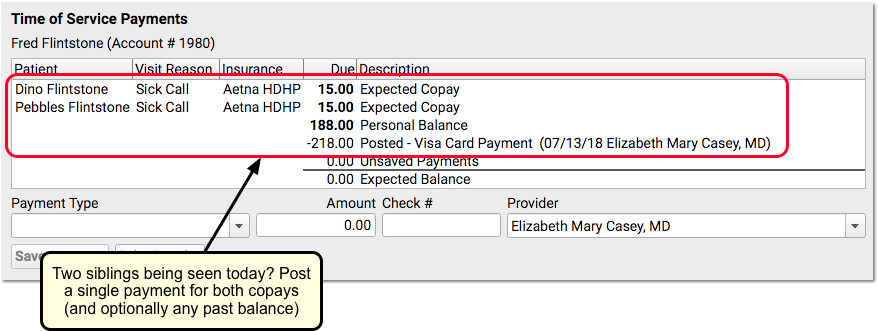
When you check in the next sibling, you’ll see the payment details from when you checked in the first sibling.
Optionally, Print a Receipt
After you post one or more payments, you can click Print Receipt to print out a receipt.
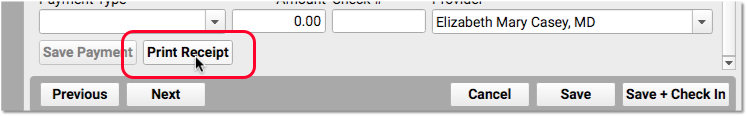
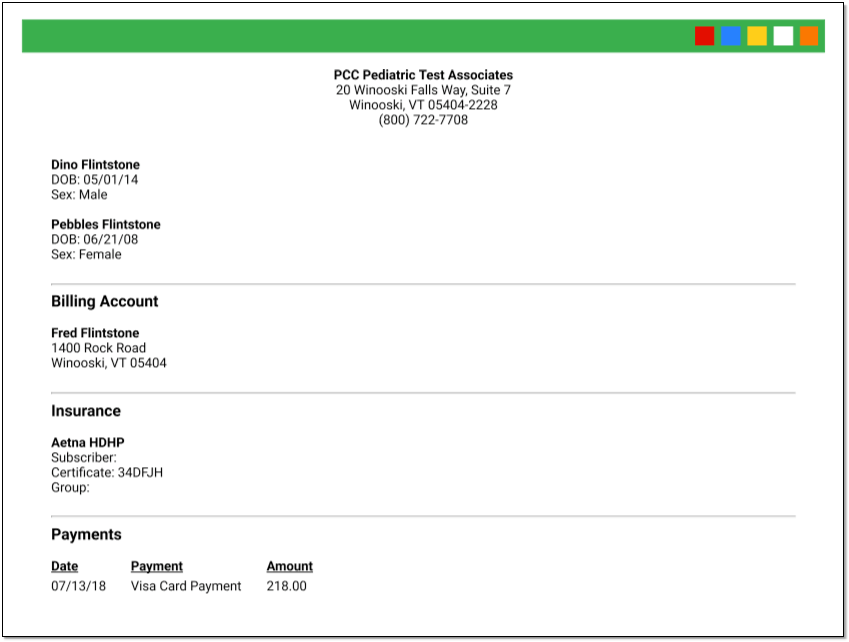
You can make changes and reprint the receipt if you need to, and you can always retrieve the receipt if you need it later by returning to the Patient Check-In protocol.
Click “Save + Check In”
When you are finished checking in the patient, click “Save + Check In”.
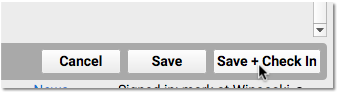
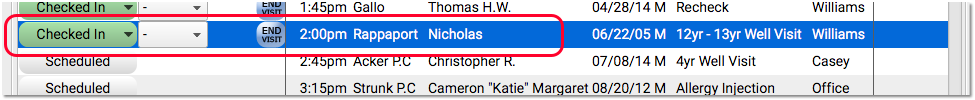
PCC EHR will update the patient’s status to Checked In, increment the Visit Status Counter for Arrived/Checked-In patients, and you’ll be ready to greet the next patient.
Undo Check-In (Revert Visit Status Back to “Scheduled”)
If a patient is checked in (or “arrived”) by mistake, you can easily revert the visit status back to “Scheduled”.
Simply highlight the visit that was checked in by mistake, click on the Edit menu from the top of the screen and select “Revert Status to Scheduled”.
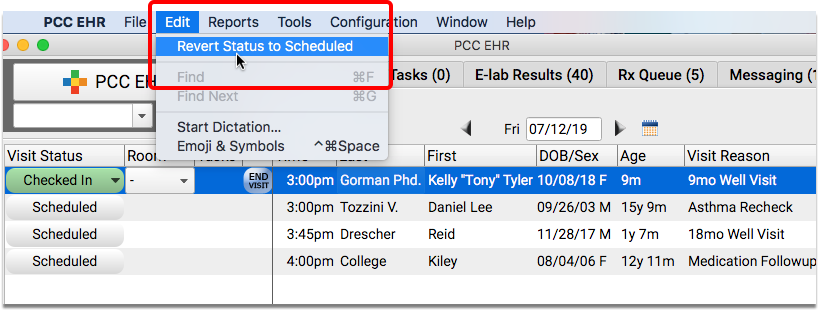
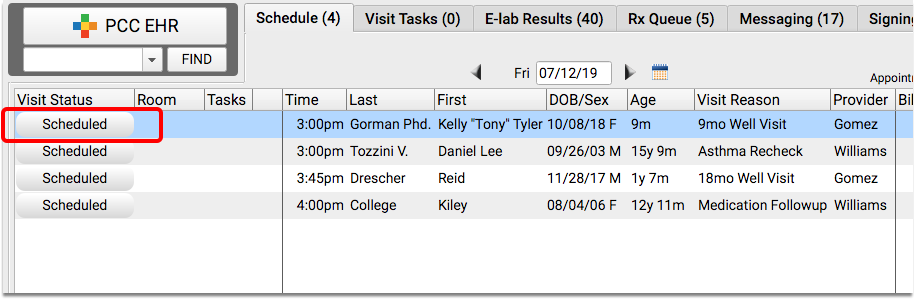
The appointment will revert back to “Scheduled”.
Orders Prevent Status Change: If you have created orders on the visit chart note, you will not be able to revert the visit status.
Open Patient Check-In Again to Reprint Receipt, Post Another Payment, and More
You may not complete all of the Patient Check-In steps right away. For example, the parent may return to the desk to ask for a receipt. Or you may need to post an additional payment or update policy information later.
You can reopen the Patient Check-In ribbon for any appointment by selecting the appointment and clicking “Patient Check-In”.
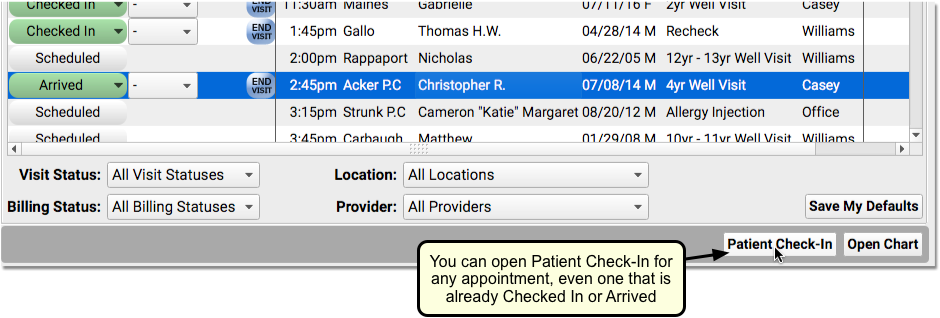
Who Checked a Patient In? Who Posted a Payment?
PCC EHR tracks which user at your practice performed various functions. This can help when there’s confusion at the front desk or when you need to balance out your cash drawer.
You can see who checked a patient in by reviewing the Appointment Details component.
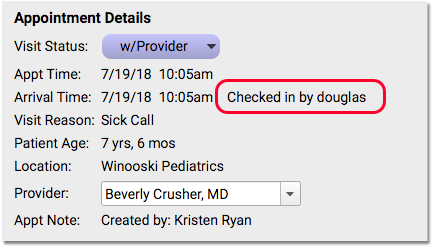
You can find that component at the top of a chart note or in Patient Check-In. So, for example, if you wanted to know who checked a patient in, you could highlight the appointment on the Schedule screen and click “Patient Check-In”. Or, you could open the visit’s chart note and look at the top of the protocol.
You can see who posted a payment in the payment’s description in the ledger in the Time of Service Payments component. You can also see who posted a payment in the deposit report and in other Practice Management reports.
Are Your Staff Accounts Linked?: When you post a payment in PCC EHR, you want it to display appropriate attribution in your practice management reports. For this to work, your practice’s EHR user accounts should be linked up with their practice management user accounts. Your Client Advocate or New Client Implementation specialist will help you with this.
You can also review the PM Username column in the User Administration tool, and enter practice management account information for your staff.
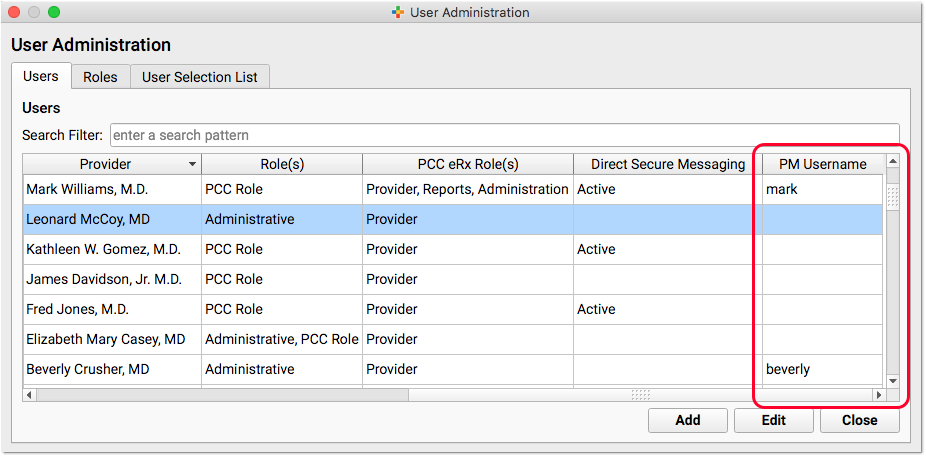
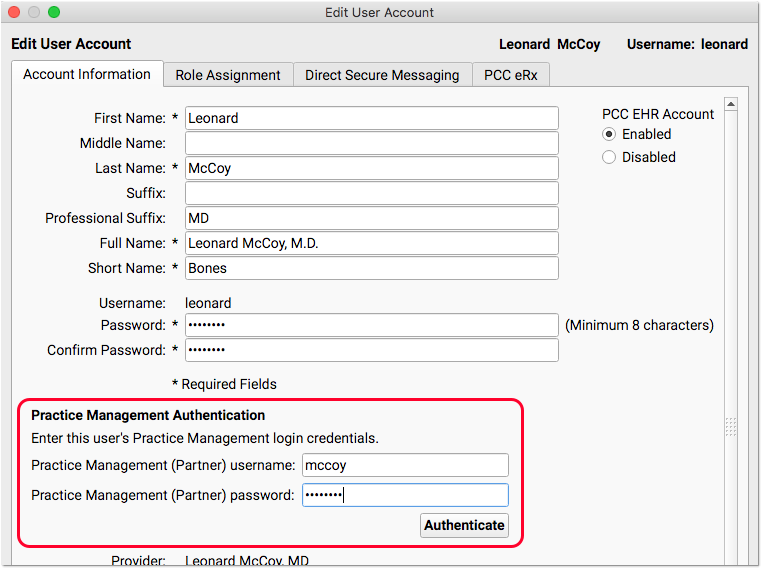
Check In or Arrive Patient, Visit Status Counters
Patient Check-In is a great tool for reviewing and updating patient information and for performing other front desk tasks. However, you can optionally just mark a patient as having arrived, without checking them in.
PCC EHR has an “Arrive Patient” button, which you can see when you open a chart for a patient who has not been checked in.
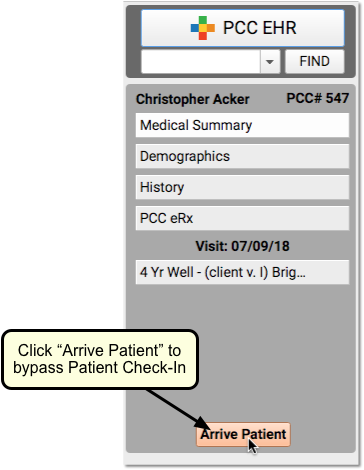
If a provider wants to create an appointment and begin working with the patient immediately, for example, or if your practice decides not to use Patient Check-In, you can click to “Arrive” a patient instead.
Keep in mind that when you “Arrive” a patient, you skip the Patient Check-In protocol, which includes important components such as a patient’s policies and eligibility. (You can optionally complete Patient Check-In later, using the “Patient Check-In” button on the Schedule.)
Your green Visit Status Counter (at the bottom of the screen) will display a total of all patients on your Schedule screen who are either Checked In or Arrived.
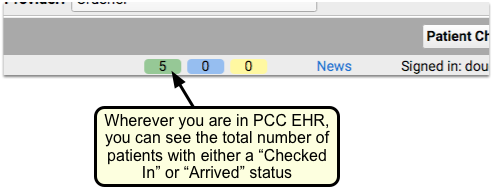
Configure Patient Check-In for Your Practice
You can adjust what components appear in Patient Check-In, create custom components, and create custom Patient Check-In Clinical Alerts.
To learn how to customize your practice’s Patient Check-In workflow, read Configure Patient Check-In.
Optional: Pre-Check-In
Pre-Check-In is an optional function in PCC’s patient portal. Your patients and families can add, confirm, and update patient, billing and insurance information through the patient portal in advance of their visit, so your practice can quickly update patient data and reduce wait times for your patients.
When Pre-Check-In is enabled, a status icon appears in the Visit Status column in PCC EHR’s Schedule queue.
![]()
Visits indicated with an orange clipboard icon have Pre-Check-Information waiting to be reviewed and imported by your practice. This can be completed before or during check-in.
When a portal user completes Pre-Check-In in PCC’s Patient Portal, the submitted information appears in a Pre-Check-In component in Patient Check-In
For more detailed information on configuring and using Pre-Check-In, click here.
Moving Your Practice to a New Location
So your practice is moving. Maybe you have outgrown your current space, or want to move to a more affordable location, or your lease is up, or you want to buy a building as an investment? Moving can be complicated. There are many moving pieces, and PCC is eager to make your move successful, with as little interruption to routine and as few surprises as possible.
Contact PCC
When you make the decision to move please contact PCC Support. Your Client Advocate and/or a PCC project coordinator will arrange a “kick-off” meeting with you and a team at PCC. Ideally you’ll let PCC know about your move at least three months before your projected move date, but the more lead time we have the easier and less stressful the process will be. PCC will work with you to ensure all the i’s are dotted and t’s crossed for your move.
Moving Checklist
Many small things have to happen for your transition to go smoothly. PCC has developed a checklist you can use to track your outstanding tasks while you get ready to move. Download it here.
Guide for Start-up Practices
Opening a new practice is a complex process. One important element is selecting the EHR and Practice Management System you want to use, but, before your practice can open its doors, certain things must be in place.
Physical Space
Location
Your practice location is of critical importance. Selecting a location, signing a lease or purchasing a property, and interior fit-up take time.
Certificate of Occupancy:
Before you can begin seeing patients, you must receive a Certificate of Occupancy from your state or local government to certify that your physical space meets building code requirements.
Internet Access
Having a connection with enough bandwidth to support your patient volume and practice operations is critical. Before you can start using your EHR, the right internet connection needs to be up and running, provided by the local internet service provider (ISP) of your choice. PCC strongly recommends fiber or business-class cable for internet. Your PCC representative will provide specific requirements and review your current or planned internet connection.
Equipment Room
Will your practice host your data locally, in a physical server on the premises, or in the cloud? PCC provides both solutions, and can work with your practice to decide on the best choice. We also provide network equipment to practices that need them, such as a firewall, UPS battery, and network switch.
If you will have a server running locally on the premises, or if you use PCC to supply and manage your network equipment, PCC requires that this equipment have adequate space, power, and ventilation. Many pediatric practices use a ventilated closet or storage room, one that is not used for other storage needs. To ensure that proper security is maintained, this equipment should be locked when not attended.
Network Cabling
Your office must have network cables to connect hardware throughout your practice. Speak to your PCC representative for help determining what kind of cabling will work for your practice. Please note that PCC does not do premise cabling and cannot cut holes in your walls, ceilings, or furniture for cabling. You are responsible for arranging such work to be completed before the PCC Server is installed.
Floor Plan
A floor plan of your physical space allows you to determine how many exam rooms you will have, where your front desk will be, where to house your PCC equipment, and where to place wireless network access points.
Recommended Hardware
Before you can go live with PCC, you’ll need to set up the printers, scanners, and workstations to support your practice. Clinical, front desk and billing staff will need workstations that meet PCC’s hardware requirements.
Set Up Billing Workflow
One of the biggest challenges for new practices is ensuring that their billing and collections are up and running from day one. Your billing is your revenue stream, and without proper coding, claims processing, and followup, your practice will have a difficult time getting paid fairly and on time. We recommend the following as a minimum to help you build a healthy billing workflow.
Get Your Providers Credentialed Properly
Without the right credentials, your providers can’t see patients, or bill for services. Identify who is responsible for getting the right paperwork completed to ensure that your providers can see patients and submit claims before you open your doors.
Hire an Experienced Biller or Billing Service
Billing is an incredibly detailed and complex process. It may sound straightforward, but insurance companies, coding practices and changing regulations require a great deal of attention. Hiring the right person will help you build strong billing practices from the start, saving you from potential trouble down the line. If you’d prefer to use a billing service, PCC has experience working with billing services.
Identify Claim Posting and Followup Responsibilities
Determining who posts charges, who follows up on personal balances, and who follows up with insurance companies is vital. Make sure each person understands and can handle their responsibilities.
Plan Out Your Front Desk and Encounter Workflow
Your patients and families need to quickly check in at your front desk, register for their visit, and pay their copays. When you start a new practice, you’ll be collecting a lot of information – names, addresses, insurance cards – and your front desk will be set up for success if they have clear responsibilities and proper workflow in place. How will your practice manage the flow of patients from check in, to the waiting room, to the exam room?
The best way to prepare for your go-live is to visit a pediatric practice in your area already using PCC. We’re happy to provide you a list of PCC clients near you. Visiting another office allows you to see how they have chosen to set up their system, observing their workflow and asking questions about what works best for them. This hands-on experience will give you an idea of how you’d like your practice to work and can help you make informed decisions as you go through the PCC online process.
Set Your Prices
Your practice needs to determine how much to charge for its services. This includes all of the different procedures and office visits you do, as well as lab tests, school forms, and other ancillary services. PCC has reporting tools you can use as a guide when making pricing decisions, but, your practice must decide how much to charge for each service you provide.
Determine Your Coding Practices
Pediatric billing is complicated, and your practice needs to become familiar with Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) coding. Use resources about pediatric coding to decide which CPT and ICD codes you will use and how your visits should be coded. Make sure this information is communicated clearly with staff members who are responsible for charting.