Edit Your Practice’s Procedures, Codes, Adjustments, and Prices
When you need to add a new CPT code to your PCC system, create a new version of a code that includes modifiers, or adjust your practice’s prices for procedures or adjustment types, use the Table Editor found in PCC’s under-the-hood Practice Management window.
Watch a Video: Watch Edit Your Prices and Billing Procedure Codes for a video tutorial of these steps.
Procedure Code Guidance: The procedure codes discussed in this article are intended only as examples. You should consult the AMA’s current CPT Coding Guide and work with your insurance payers to verify what codes you should report. Your practice updates and maintains your procedure list, codes, and prices in the Procedures table in the Table Editor on your PCC system.
Updates Procedure Names, Codes, and Prices
Follow the procedure below to learn how to add or update procedure billing codes, prices, and other procedure information (such as dose amounts for an injection procedure).
Add an Immunization: The procedure below covers how to edit prices and add or update billing codes for any medical procedure. You can also read a specific guide: Add and Configure Immunizations.
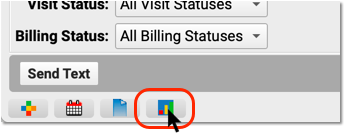
Open the Practice Management Window
Click on the Practice Management icon to open the Practice Management window.
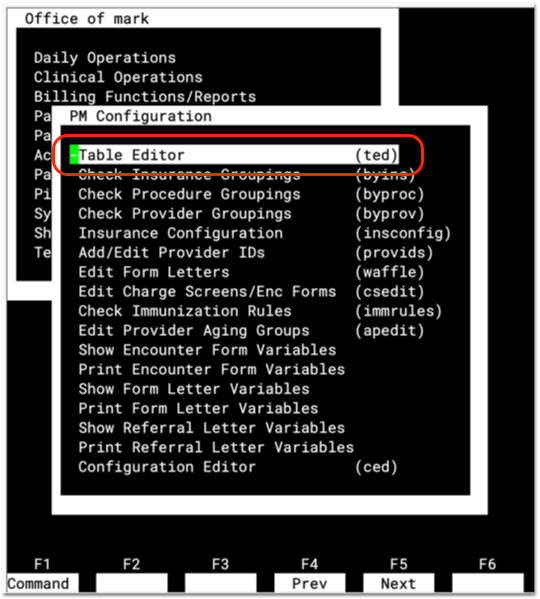
Run the Table Editor (ted)
Run the Table Editor (ted) from the Partner Configuration window.
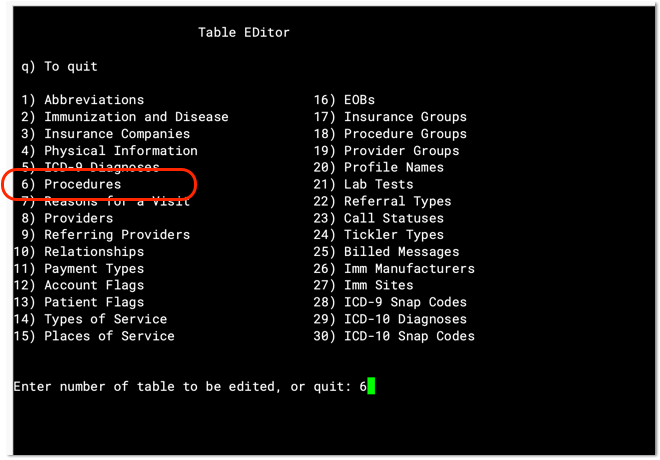
Select Table #6, Procedures
Open table #6, the Procedures table, to look at your practices list of procedures.
Review Existing Procedures
Press Page Up and Page Down to review the list of all billing procedures on your PCC system.
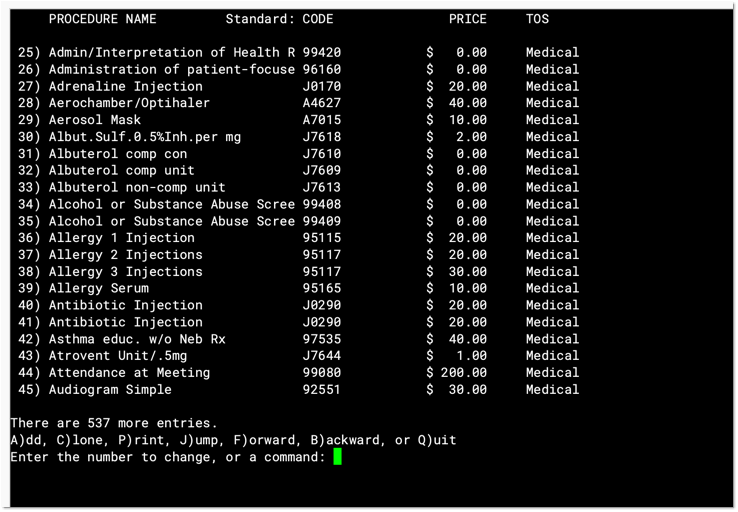
For each entry, you can see your practice’s custom procedure name, the default billing code (usually a CPT code), your default price, and the type of service.
Enter the number next to a procedure and press Enter to see details about any procedure.
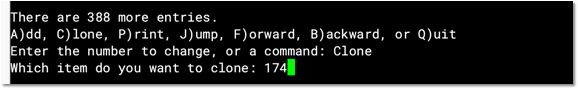
Clone (or Add) to Create a New Procedure
To create a new procedure, find a similar procedure and press C to clone it. Or press A to start from scratch.
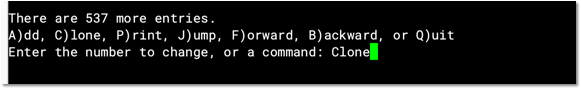
Do Not Overwrite an Existing Entry: Never edit and overwrite an existing procedure entry, as this may affect your billing history. Even if a procedure has been retired and replaced with a new CPT code (for example), always clone and create a new entry.
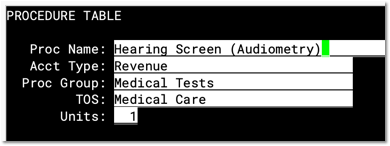
Update the Procedure Name, Group, and Related Fields
Edit the fields in the upper-left corner of the screen to indicate a procedure’s name, accounting type, procedure group, type of service, and units.
-
Procedure Name: You can name a billing procedure anything that will be useful for your practice. Your clinicians, billers, and the patient’s family will see this name in various contexts, such as a receipt or bill. Insurance payers do not generally review or verify a procedure’s name, relying instead on the billing procedure code.
-
Accounting Type: Billable procedures you perform in your practice should have an accounting type of “Revenue”. Other Account Types, such as “Receipt” and “Revenue – Non-Service” are used for refunds, insurance write offs, and other less common accounting situations.
-
Procedure Group: The Procedure Group field is a customizable value used for reporting purposes; it does not usually affect billing or how a procedure is ordered or completed. Select an appropriate Procedure Group.
-
Type of Service: The Type of Service field was originally used to indicate a code on claims, but it is no longer part of the claim standard. For most procedures performed by your practice, use “Medical Care”. If the procedure is a lab, select “Diagnostic Laboratory”. When your PCC system formats claims, it includes an appropriate CLIA identifier for procedures with a type of service “Diagnostic Laboratory”.
-
Units: If you always bill a procedure as a set number of multiple units, you could adjust the Units field. Normally, units are selected when your practice bills an encounter, and this field is set to “1”.
Update Drug or Injectable Related Fields
If the procedure is an immunization or another injection, enter the injectable-related information on the right.
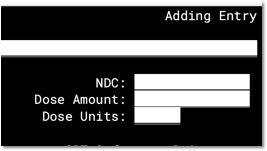
Read Add and Configure Immunizations to learn about specific details and tips for filling out the NDC, Dose Amount, and Dose Units fields. Always enter the NDC code found on the smallest administered dose. In other words, use the NDC code from the vial, not the box or carton.
Update the Billing Code
Enter the procedure billing code in the Schedule A “CPT” code field. Then press F4 – Duplicate Codes to copy the code to all schedules.
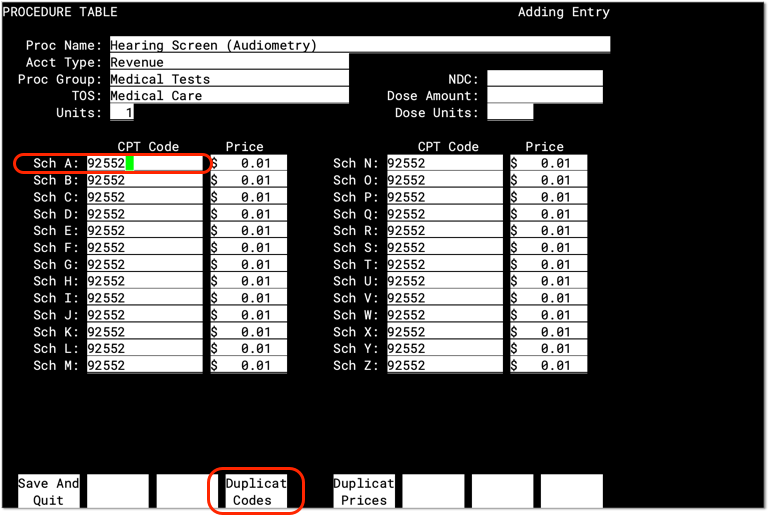
PCC does not provide or distribute CPT billing codes.
What About Billing Codes for Administrative Fees?: When your practice posts charges, PCC’s software will require a linked diagnosis for any procedure that has five or more characters, such as a “99213”. If you are creating or updating your practice’s administrative fees (or other charges that do not require a diagnosis), use a billing code with fewer than five characters. For example, if you are creating a “Forms Fee” or “Missed Appointment Fee”, you could use a billing code of “X” or “FEE”, or whatever would be clearest for your practice.
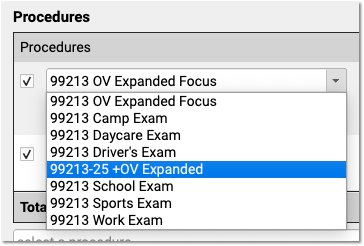
Code Modifiers: If your practice needs a code with one or more modifiers, such as the common -25, you should clone an existing procedure table entry and adjust the clone to include the modifier(s) in all code schedules. Common modifiers include -25, -26, and -59, but the CPT standard and payer requirements sometimes use more complex modifiers, such as -Q6, and CMS has developed HCPCS Level II Modifiers, such as -E1, -TC, and -XS. (See AAPC.) When your practice adds a modified version of a code, it becomes available to all users when they Post Charges.
When Would I Use a Different Code Schedule?: Normally, you will enter the same code for all schedules. PCC supports optional schedules due to deprecated “local codes”, which are no longer part of the claim standard used in the U.S. If your practice has a schedule specifically configured for Medicaid billing, and your state Medicaid program requires a modifier, you can enter the full code and the modifier into a CPT field for that schedule. PCC can then help configure which claims will use the custom schedule. Alternatively, your practice could clone a Procedure entry and create a specific version of the procedure for Medicaid billing.
Update Your Price for the Procedure
Enter a price for the procedure in the Schedule A “Price” field. Then press F5 – Duplicate Prices to copy the price to all schedules.
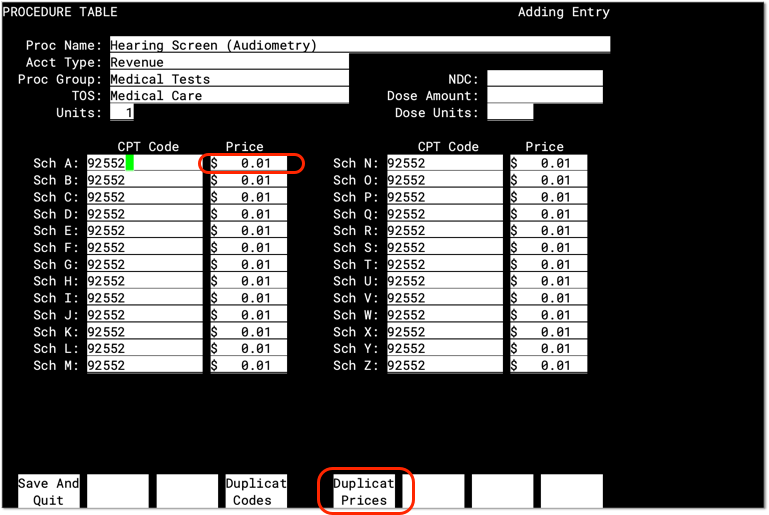
PCC does not provide pricing recommendations. The pediatric benchmark in the U.S. is to charge above 200% of Medicare reimbursement amounts, which are publicly available per-relative value unit for each region. The example above is for illustration only and is not a fee suggestion.
When Would I Use a Different Price Schedule?: A procedure’s price should be identical in all schedule fields, except where your practice uses a different fee schedule. For example, many pediatric practices use a fee schedule for medicaid plans, where they enter a $0 (or a reduced price) for immunizations, ensuring that VFC procedures are billed correctly. Read Add and Configure Immunizations in PCC EHR to learn more. If your practice needs a separate fee schedule, work with PCC Support to ensure that the correct insurance policies are configured to use the custom schedule.
Press F1 to Save
Press F1 – Save and Quit to save any changes to your procedure. Alternatively, press F12 to go back to the list without saving your changes.
Configure Your New Procedure Orders
After you add or update a billing procedure code and price, you may want to create one or more orders and add them to specific chart note protocols (found in Protocol Configuration tool), and link procedure codes directly to orders (in the Billing Configuration tool) so the codes will be added to an encounter whenever an order is created for an encounter. See the sections above to learn more.
Configure Adjustments and Accounting Types
In addition to billable clinical procedures, the Procedures table also includes adjustments. These include accounting adjustments, fees and charges, and other items that result in an increase to an account’s balance.
When you edit these procedures in the Table Editor (ted), the Accounting Type field indicates their purpose. Various PCC reports include or exclude different accounting types, or put them in special columns, in order to provide your practice with a better understanding of your accounts receivable.
The table below describes different categories of these procedures, their related “Accounting Type” in the table, and how they are used for each accounting operation.
What Are These For?: For examples of how you would use the procedures with these accounting types, see Refund Personal Credits and Reverse a Payment.
| Procedures | Accounting Type | Explanation and Usage |
|---|---|---|
| All clinical procedures performed in a practice | Revenue | Billable procedures you perform in your practice should have an accounting type of “Revenue”. Office visits, immunizations, and more are examples of revenue procedures. You can post these procedures as charges in the Post Charges window. |
| Non-Clinical service fees | Revenue – Svc Chg | Tasks you perform for a family that are non-clinical, and have a charge, have an accounting type of “Revenue – Svc Chg”. Examples include record transfer fees, form fees, rebilling fees, and similar. |
| Fines or other non-service fees | Revenue Non-Service | When your practice charges a bounced check fee, a forms fee, or some other fee that is not billed to an insurance payer, you use a procedure with an accounting type of “Revenue Non-Service”. The procedure will appear like any other charge on the account. |
| Capitation, incentive payment, insurance interest, overpayment, or withhold payment adjustments | Revenue Non-Service | When an insurance company sends you a capitation payment, interest payment, or other type of less-common payment, you post an adjustment procedure with an accounting type of “Revenue Non-Service” to indicate what the payment is for. Then you post the payment. For more information see Post Capitation Checks, Incentive Payments, Interest Payments, Overpayments, and Withhold Payments. |
| Write off a credit that you will not refund | Revenue Credit W/O | When you wish to classify a credit on an account as income, you can offset it with an adjustment procedure with an accounting type of “Revenue Credit W/O”. This means you are classifying the credit as income to the practice, and you do not intend to refund it. |
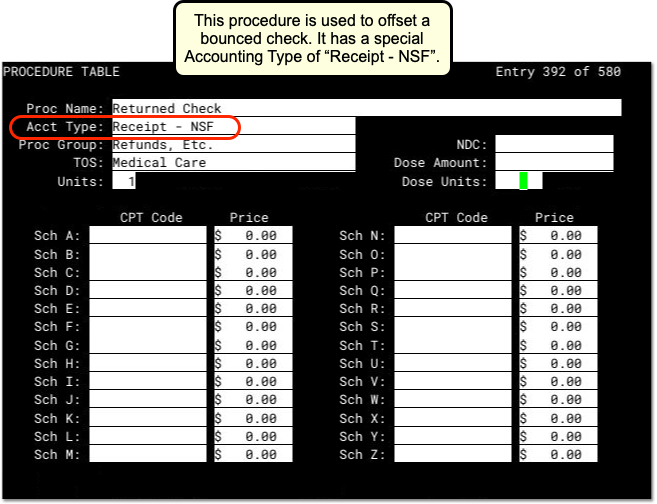
| Returned check or other stopped payment adjustment | Receipt – NSF | When a check bounces or another type of payment is stopped, your practice negates the payment by linking it to an adjustment procedure with an accounting type of “Receipt – NSF”. You might also post a fee. |
| Credit refund adjustments | Receipt – Refund | When you refund a credit to a family, you post an adjustment procedure to the account with an accounting type of “Receipt – Refund”. |
| Insurance takebacks and other insurance refund adjustments | Receipt – Refund | When you need to issue an insurance refund, or an insurance company issues a “takeback” for a payment you already posted, you post an adjustment procedure with an accounting type of “Receipt – Refund”. Then you link the original payment to that adjustment procedure. |