Best Practices for Pediatrics in the COVID-19 Era
Pediatric practices around the country can continue to see patients, provide great care, and thrive as businesses during and following the COVID-19 pandemic.
PCC worked with practice managers and managing providers to develop this library of recommendations.
Contents
- 1 Recall Patients
- 2 Adjust How You Schedule Patients
- 2.1 Implement the PCC EHR Appointment Book
- 2.2 Maximize Portal Communication
- 2.3 Implement Appointment Requests in the Patient Portal
- 2.4 Update How You Handle Scheduling Phone Calls
- 2.5 Adjust When You Schedule, Your Scheduling Blocks, and More
- 2.6 Proactively Schedule Followups and Recurring Appointments
- 2.7 Ask: “Could This Be a Telemedicine Encounter?”
- 3 Improve Your Practice’s Pre-Visit Steps
- 4 Change How You Checkin and See Patients
- 5 Implement and Expand Your Telemedicine Services
- 6 Get Paid and Maintain Practice Revenue
- 7 Apply for a CARES Grant and Other Available Support
Recall Patients
PCC recommends that all practices launch a patient recall initiative. During the initial months of the COVID-19 pandemic, many practices experienced lower visit volume. Children’s developmental needs and other health concerns (diabetes, asthma, depression, and more) did not slow down, and this created an unmet need.
Consider contacting all families who have visited your practice in the past three years and schedule them for telemedicine or in-person appointments. Get your patients caught up on well visits, screenings, shots, and chronic problem and care plan management. As you provide much needed care, you will also be maintaining your practice’s relationships and your ability to help your community.
Read Why and How Pediatric Practices Should Launch a Recall Initiative Today to learn more.
Adjust How You Schedule Patients
When PCC spoke with pediatric practices, they shared changes they’ve made to patient scheduling during the COVID-19 era.
Implement the PCC EHR Appointment Book
The Appointment Book has built in Telemedicine features and can be configured with visit templates to help your schedulers. The close integration between the Appointment Book and the patient’s chart record make everything easier, from connecting to patients, to charting, to billing.
If your practice is not using the PCC EHR Appointment Book, PCC Support can help you get started.
Maximize Portal Communication
Contact your families and make sure they all have patient portal access. This will allow their initial contact with your practice to be asynchronous, which means your staff and clinicians can followup on questions and concerns whenever they are available.
By improving this initial point of contact, you can more efficiently triage issues and schedule appointments as needed.
Implement Appointment Requests in the Patient Portal
Your practice can create a patient portal template for appointment requests. Then, when the family wants an appointment, they can pick “Appointment Request” when they create a portal message.
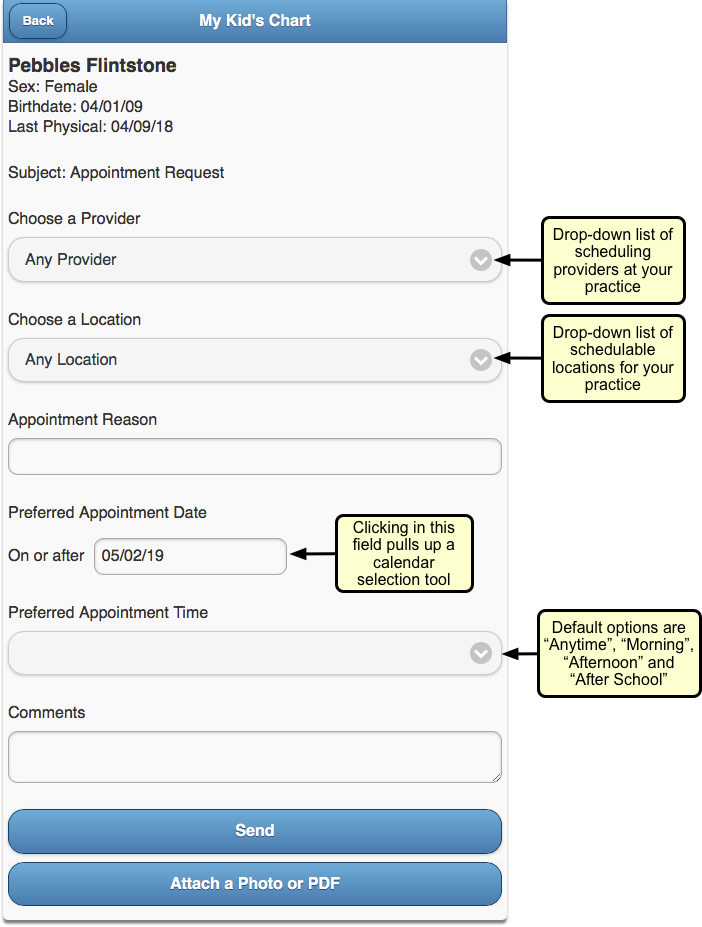
With an Appointment Request template, you can encourage families to provide the information you need to schedule them.
Read Configure Your Patient Portal Message Templates to learn more.
Update How You Handle Scheduling Phone Calls
When your practice schedules an appointment, what do you review and communicate to the family?
Develop a quick script that informs the family what to expect when they visit your practice, and confirm demographic, insurance, and other information when you schedule. For example, if your practice requires masks, no longer uses your waiting room, or performs a phone-based checkin prior to the appointment, set that expectation when you schedule.
If your practice is implementing practice-wide credit card on file for all families, you can collect that information when you schedule. See below for more tips on CCOF implementation.
Adjust When You Schedule, Your Scheduling Blocks, and More
Review when your practice schedules different visit types, and make adjustments that balance what your families need with your practice’s enhanced safety protocols and other changes.
-
Well Visits in the Morning: Some pediatric practices have implemented a “Well Visits in the Morning” schedule. That means all well visits are seen in exam rooms, normal cleaning takes place in between visits, sick visits happen in the afternoon, and the once-a-day more comprehensive cleaning happens after the office has closed.
-
Sick vs. Well Locations: Another pediatric practice has two locations, and they have changed one to a “sick only” location and one to a “well visit only” location.
-
Change Blocks, Stop Using Blocks: Some practices report that in 2020 they “threw out the visit template”, reworked their blocks based on daily trends, or no longer use visit blocks at all.
The above ideas may or may not suit your practice’s goals, but you might make other changes to how you schedule. In the COVID-19 era, pediatric practices need to stay agile as they tweak and adjust schedule blocks, hours, open time slots, and family expectations. As your community and culture rapidly changes in response to COVID-19, patient appointment needs will change too.
Proactively Schedule Followups and Recurring Appointments
When a followup appointment is appropriate, consider scheduling it at the same time as you schedule the initial visit, or during the initial visit. Rather than waiting the weeks or months before you contact a family to schedule, make the appointments when you have the family’s attention.
If your practice normally only schedules out six months, consider expanding that to 13 months so you can schedule annual well visits at the preceding visit.
Ask: “Could This Be a Telemedicine Encounter?”
Many practices schedule telemedicine encounters for sick visits and followup visits. Some are trying out partial well visits over telemedicine as well.
See the Telemedicine section below for ideas on expanding your practice’s telemedicine services.
Improve Your Practice’s Pre-Visit Steps
What does your practice do in advance of each appointment? During the COVID-19 era, you can examine your process and make changes that will make the visit itself easier and more efficient.
Your process might include:
-
Expand When and How You Check Eligibility: Especially if you are increasing telemedicine visits or offering new services, you should review eligibility for all encounters in advance. You can do that with PCC’s built in eligibility tools. Practices report that payers do not respond to eligibility requests until 5 days previous, and anecdotally some Medicaid payers only provide day-of or day-before eligibility information. Regardless, it’s important to check eligibility as employment status, insurance payer rules, and state rules about visit types are rapidly changing.
-
Implement Pre-Visit Questionnaires in the Patient Portal and/or With CHADIS: Since clinician in-person time now has additional constraints and challenges, you may want to implement or expand your pre-visit screenings or questionnaires. You can design your own questionnaires in the patient portal’s templates tool, or you could sign up for CHADIS or a similar service. PCC is working to enhance CHADIS functionality, and a partial CHADIS integration is in pilot test now. As you expand your pre-visit questionnaire use, keep in mind that you will need to adjust your workflow so the front desk or a nurse can send the families these materials or links.
-
Collect Copays in Advance: In order to make in-person and telemedicine encounters as smooth and “touchless” as possible, your practice can implement a policy of collecting copays in advance of an appointment. Since account balances and payments can be done through the patient portal, families will have transparency and can see their credit if the visit ends up not requiring a copay, for example.
Change How You Checkin and See Patients
When it’s time for the encounter, what changes will your practice make to accommodate the additional challenges of COVID-19? This section includes recommendations we heard from pediatric practices across the country.
Eliminate or Reduce Use of Your Waiting Room
Some practices have closed their waiting rooms or greatly reduced any time spent in them. They tell families:
-
Wait In Your Car: Your practice can instruct families to wait in their car until the time of their appointment.
-
Call When You Arrive: When a family pulls in, they can call your front desk to checkin. You can verify insurance, demographics, and collect the copay over the phone.
-
We Will Text You When Your Exam Room is Ready: PCC’s built-in text feature means your staff can quickly select an appointment and text the family when their room is ready.
As they make these transitions in their offices, some practices are changing their long term plans for their layout. For example, could you transition your waiting room into multiple exam rooms or office space?
Virtualize Your Checkin and Precheckin Processes
By using the patient portal, texting, and the phone, some practices have eliminated all parts of the in-person patient checkin.
To facilitate encounter management, some practices create a new Visit Status in PCC EHR, such as “Precheck”, so that everyone can understand when a family has completed their demographic updates, paid their copay, and are ready for the doctor.
At The Door: Take Temperature, Provide PPE
When a family enters the building, a practice can greet them at or near the entrance. They can use this opportunity to take temperatures and to review PPE guidelines for the practice.
If a patient or family member is not wearing a mask, a practice can optionally provide masks for them to wear.
Consider Car Visits and Shot Tents
PCC heard from practices that now see their patients right in their cars.
Instead of an exam room, the clinician visits the patient in the parking lot of the pediatric practice.
When an immunization or other medical procedure is needed, they can use a “shot tent” or station set up for that purpose.
Plan for Flu and Immunization Clinics
If your practice performs annual flu clinics, where you bring in patients en masse for their flu immunization, you can make adjustments to your usual procedures and do the same in 2020 and beyond.
Similarly, if you implement Telemedicine well visits (some practices are trying), you may have a backlog of kids who need to come in for immunizations. When COVID-19 vaccines are developed, pediatric practices may be an important part of distribution and administration.
Practices can work now to improve their “immunization-only” visit workflow and how they might run clinics while maintaining enhanced safety protocols.
Read More Here: Run a Pediatric Drive-Up Flu Shot Clinic
Implement and Expand Your Telemedicine Services
Telemedicine encounters can provide effective care without physical contact. During the COVID-19 era, practices across the country have expanded their use of phone, portal messages, and video telemedicine encounters. When a practice schedules a sick visit or a followup visit, they can stop to ask the both the family and themselves, “Could we do this as a telemedicine encounter?” The answer is often “Yes!”
You can learn how to use PCC EHR’s tools for these encounters here:
- Schedule, Chart, and Bill for a Telemedicine Encounter (Video, Article)
- Bill For Phone Calls and Portal Message Encounters (Video, Article)
Read below for an overview of tips and recommendations we heard from pediatric practices.
Schedule for Telemedicine Appointments
When you schedule a telemedicine encounter:
-
Actually Schedule Telemedicine Encounters: A telemedicine encounter is not just a phone call that you decide to bill for later. Schedule your Telemedicine encounters. Adjust your schedule’s visit reasons, blocks, and more to make telemedicine a real part of your practice’s offerings that you will bill insurance for.
-
Use the PCC EHR Appointment Book: When you schedule a telemedicine encounter in the Appointment Book, a telemedicine icon appears with the encounter for all users, additional fields are available for telemedicine connection information, and PCC EHR can optionally designate a telemedicine billing place of service based on your configuration.
-
Perform Precheckin When You Schedule: As with any encounter in the COVID-19 era, it is important to review and update information as soon as you can, to make the actual encounter run smoothly. Update patient information, verify insurance, and collect credit card information for the copay when you schedule.
-
Set Expectations: When you schedule a telemedicine encounter for a family, tell them exactly what to expect. For example, when will the practice call them for pre-visit questions? How will they receive telemedicine connection information? Let them know during scheduling.
Perform “Precheckin” Calls Before a Telemedicine Encounter
On the day of a telemedicine encounter, or the day before, your practice can call the family. At some practices, this call is made by the MA or nurse. During that call, they:
-
Update Patient and Family Information: Verify demographics, insurance, and other details.
-
Collect Money: Collect copays and payments for any outstanding balances. Since billing and collection for telemedicine visits are rapidly changing, some practices have made it their policy to always collect the copay ahead of time and issue a refund later once the EOB arrives.
-
Tell Them How to Connect: Provide technical instructions on how to connect to the encounter. The caller can provide the telemedicine link verbally, and also send a portal message or followup text message with the URL, using PCC’s direct text message feature.
-
Update Visit Status: When the precheck phone call is complete, the practice updates the Visit Status for the appointment so the practice can see it has been completed and the patient is ready for the telemedicine encounter.
Adjust Encounter Workflow, Charting, and Billing for Telemedicine
You can make changes to your workflow and PCC EHR configuration to help telemedicine encounters be successful.
For example, create additional Visit Reasons, Visit Statuses, and custom chart note protocols that include tools for recording information during a telemedicine encounter.
If some parts of a visit must be done separately, you must decide how you will chart and bill for the two different parts.
To help chart a telemedicine protocol, create one or more telemedicine protocols for your clinicians.
Get Paid and Maintain Practice Revenue
This section collects recommendations and tips for pediatric billing and collections during the COVID-19 era.
Here are some general recommendations:
-
Consider Billing For Other Encounter Types: Prior to 2020, you may not have billed for phone consultations or portal messages. Many practices now do, and PCC has a guide which can help.
-
Adjust Your Electronic Encounter Form: After a clinician is finished with an encounter, they click “Bill” to review diagnoses and procedures and select a visit code. You can customize your practice’s electronic encounter form to include phone consultations and telemedicine-related procedures to make it easier to bill for services.
-
Update Your Chart Note Protocols and Orders: When you click on a procedure or other order on a chart note, PCC EHR can automatically add the appropriate CPTs to your encounter form. Review your lab, radiology, referral, and other orders so that they appear by default on appropriate chart notes and will automatically queue up the correct codes for billing.
Streamline Personal Payment Collection
Across the country, pediatric practices are finding ways to make personal payment of copays and outstanding balances as quick and “touchless” as possible.
-
Implement Portal Payments: Families can pay their copay and outstanding balances in the patient portal. Read Get Started with Portal Payments to learn more. Once you’re set up, work with your schedulers and staff so that they can prompt families to use this service.
-
Implement Credit Card on File (CCOF) for All Families: Your practice can use a third-party service to securely store credit card information, and incorporate CCOF into your practice’s billing policies. When you use portal payments, credit card information is similarly stored by a third party, but by expanding CCOF to all families for other billing needs, you can streamline payment and avoid problems at the time of service. Ask your bank and your merchant services for information about CCOF service. If you are doing portal payments with PCC, you have an existing contract with BluePay, a company which also offers CCOF for other billing needs. You can use a CCOF account flag and clinical alerts in PCC EHR to both drive adoption (by checking if a family has CCOF yet) and inform staff. You can then also create a custom report for the current week’s appointments showing who has CCOF and who still needs it set up.
-
Collect Copays In Advance: As mentioned above, many practices have begun collecting copays during a pre-visit checkin call. For some encounter types, it may not be clear if a copay is needed. A practice can collect the copay for every visit and issue a refund later when the EOB arrives.
-
Set Default Telemedicine Places of Service: Your practice can set default telemedicine billing places of service per scheduling location.
-
Select Billing Place of Service When You Post: Your billers can select or change an encounter’s billing place of service when they post charges.
-
Change Billing Place of Service for Previously Posted Charges: If needed, your biller can even update the billing place of service for charges after they have been posted.
Get Paid By Your Insurance and Medicaid Payers
Are your insurance and medicaid payers paying you for Telemedicine visits in parity with your in-person sick visits? According to regulations in some areas, they should be. You can research this and other topics at the COVID-19 section of your Practice Vitals Dashboard.
For common coding topics during the COVID-19 era, read Code and Bill for a COVID-19 Related Encounter, or take a look at PCC’s quick COVID-19 Coding Guide.
As insurance companies learn to respond properly to changing circumstances, your practice may need to be extra vigilant as you review claim rejections and underpayments and resubmit.
Is Billing Place of Service Still an Issue for Telemedicine?
Early on in the COVID-19 era, some practices encountered challenges with the billing place of service used on claims.
Insurance payers have mostly improved how they handle this. PCC has seen good response in many states to telemedicine billing and other encounter changes that practices have needed to make.
However, just in case, your practice should know about the capabilities in PCC EHR:
Apply for a CARES Grant and Other Available Support
Pediatric practice across the country have participated in the federal government’s CARES program, which includes grants and money for small business loans. As the COVID-19 pandemic continues, every practice should stay abreast of these opportunities, and PCC will help keep you informed.