Run the Meaningful Use Measures Report
The Meaningful Use Measures report in PCC EHR calculates your office’s performance on the Meaningful Use standards indicated in ARRA’s EHR Medicaid Incentive program and referenced in PCMH requirements. Use this report to see your office’s Meaningful Use statistics.
Follow the procedure below to run the report.
More About PCMH, CQMs, Meaningful Use Measures and Incentive Programs: For more information, check out the PCMH, CQMs, Measures, and Incentive Programs section of PCC Learn.
Configure Your System and Adjust Chart Policies
The Meaningful Use Measures report depends on charting and coding in PCC EHR. You may need to adjust how you code and chart visits in order for PCC EHR to properly evaluate your Meaningful Use percentages.
Read Meet Meaningful Use Measures with PCC EHR to learn more.
Time Period: After your practice makes configuration and workflow changes, you may need to wait 90 days in order for the report to fully reflect how your office addresses each measure.
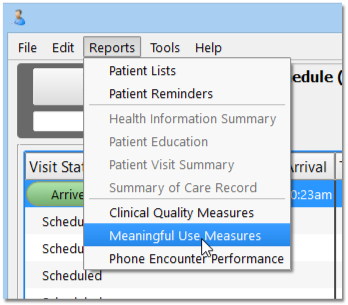
Click “Reports” and Select “Meaningful Use Measures”
The Meaningful Use Measures report is in the Reports menu.
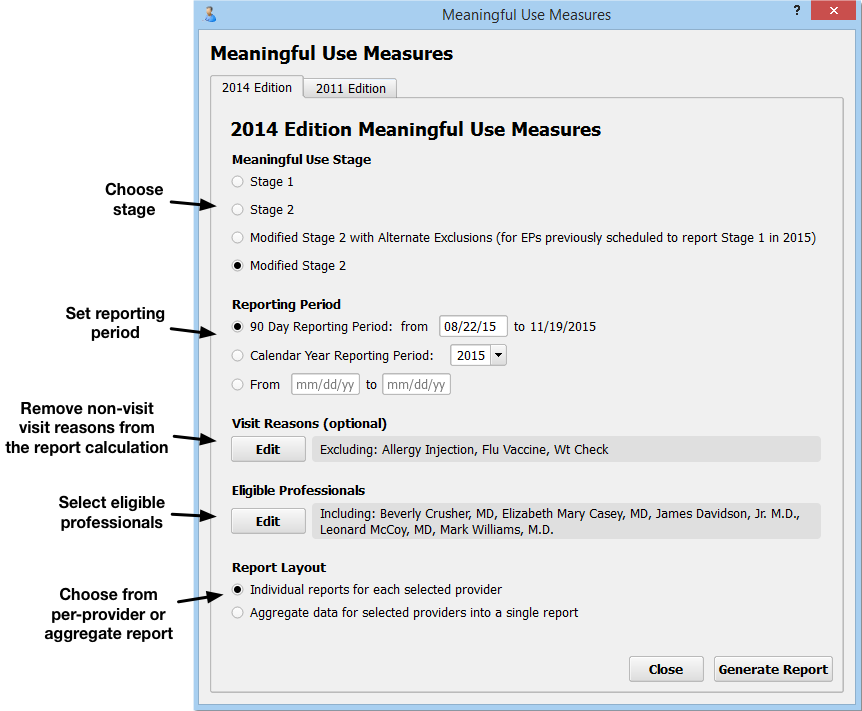
Select Stage, Reporting Period, Visit Reasons, Eligible Professionals, and Report Layout
On the Meaningful Use Measures report criteria screen, you can adjust options for output before you generate the report.
-
2014 or 2011 Edition: You can select either the 2014 or 2011 Edition Meaningful Use edition by clicking on a tab at the top of the screen. Note that the 2011 MU rules have been retired and that practices can no longer apply for the EHR Medicaid Incentive Program or a PCMH program using the 2011 rules.
-
Meaningful Use Stage: Select whether you wish to view your scores for Stage 1, Stage 2, or Modified Stage 2. Some of the 2014 PCMH standards align with Stage 2. The ARRA EHR Medicaid Incentive program now uses the Modified Stage 2 version of the measures, but also recognizes an Alternate Exclusions version of the measures.
-
Reporting Period: For 2015, your EHR Medicaid Incentive Program application or PCMH application will probably use a 90-day reporting period. For 2016 and beyond, a full calendar year may be required. You can set any 90-day period, any calendar year, or input a custom reporting period.
- Do not use a reporting period that extends before the date you went live with PCC EHR. Some of the data needed to properly calculate Meaningful Use Measures can not be obtained through data conversions.
- If you have added chart note components or made charting policy changes at your practice in order to record data for Meaningful Use, you should use a reporting period after you made those changes.
-
Visit Reasons: Click “Edit” in the Visit Reasons criteria section to select visit reasons you wish to exclude from the report. You could use this option to exclude visits where the physician typically does not see the patient, such as a lab-only or weight check visit.
-
Eligible Professionals: Click “Edit” in the Eligible Professionals criteria section to select providers for the report. For example, for the EHR Medicaid Incentive Program, you will run reports for professionals that perform at least 20% Medicaid visits. Contact PCC Support for help determining the Medicaid volume of the clinicians at your practice. For PCMH, you should select all providers (NP, PA, MD, DOs, etc.) However, for both PCMH and EHR Medicaid Incentive Program applications, you should use this criteria to exclude generic or “nurse” provider entries.
-
Report Layout: The ARRA EHR Medicaid Incentive application requires separate data for each eligible professional. A PCMH application requires a practice aggregate report.
Once you set the report criteria and generate the report, PCC will remember your settings and restore them each time you open the Meaningful Use Measures Report.
Who Did What in PCC EHR?: As you review data for each eligible professional, keep in mind that 2014 Meaningful Use Measure calculations use the “Provider of Encounter” for each arrived visit. The PoE appears at the top of each chart note, and by default is the scheduled provider. 2011 calculations were based on the clinician who signed the visit.
Click “Generate Report”
After you make your selections, click “Generate Report”.
The Meaningful Use Measures report examines details from hundreds or thousands of charts and may take several minutes to run. You may prefer to run it after-hours, when your system is less busy.
Review Report Results
The Meaningful Use Measures report will calculate and display your practice’s numbers for each measure, either as an aggregate report or per-provider.
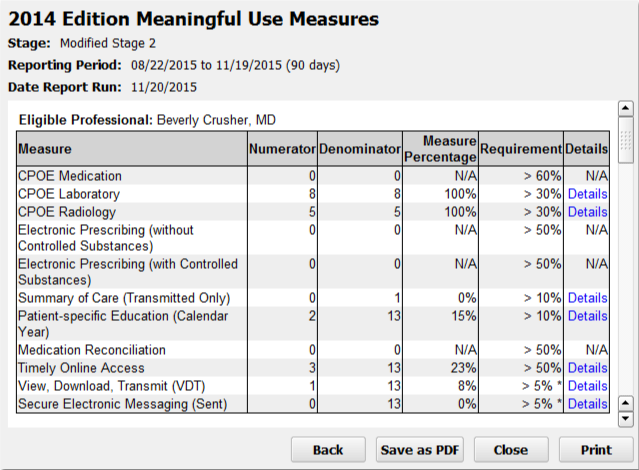
For each Meaningful Use Measure, you can see a description of the measure or alternate measure, followed by your practice’s results.
-
Numerator and Denominator: Most Meaningful Use Measure results display a number of patients who meet the requirements or goal of the measure (the “Numerator” column), as well as the total number of patients with relevant characteristics who had arrived visits during the reporting period (the “Denominator” column).
-
Measure Percentage: Next, the “Measure Percentage” column displays your practice’s percentage for the measure, calculated by dividing the numerator by the denominator.
-
Requirement: The final result column displays the threshold for successfully meeting the measure. For example, for the Modified Stage 2 version of the CPOE Medication measure, your practice needs above 60% to meet the measure. In October of 2015, CMS revised the requirements for meeting measures.
How Do I Chart and Configure PCC EHR to Affect Each Line? How Is Each Line Calculated?: Meaningful Use Measures look for certain activity in the chart for patients who visited your practice during the reporting period. For more information on how each line of the report is calculated, and to learn what changes you can make in your PCC workflow to improve your percentile score, read the Meet Meaningful Use Measures with PCC article, or review Tim Proctor’s handy Meaningful Use table.
Optional: Drill-Down to Per-Patient Details
Click “Details” for any measure to review patient-level details for the results.
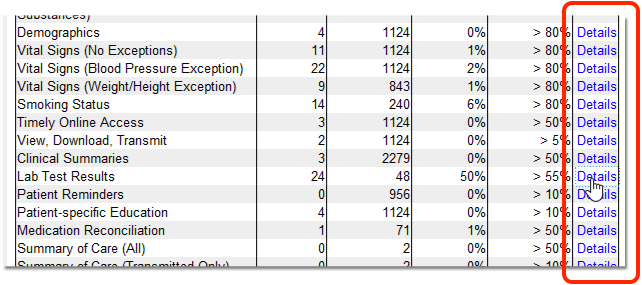
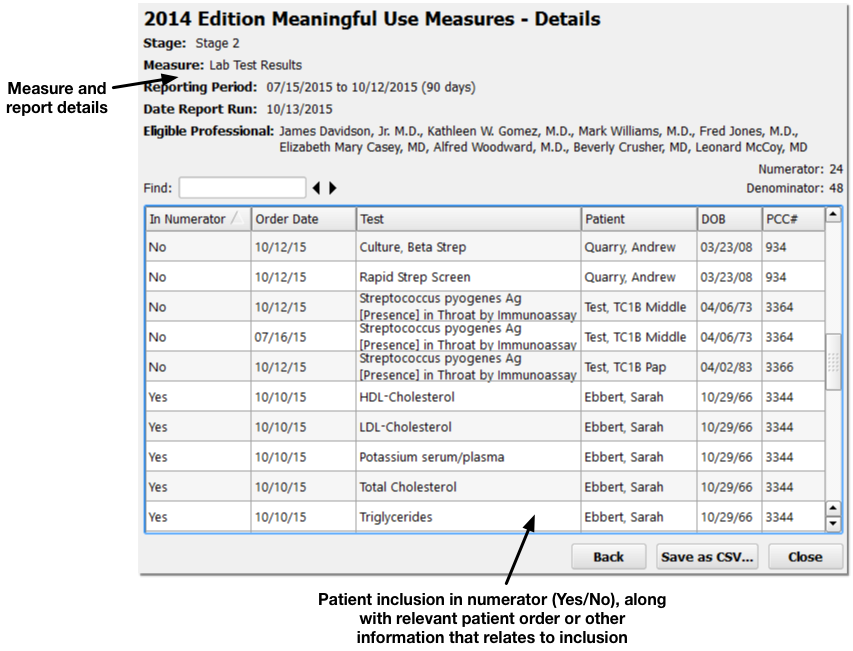
Details for the report and the selected measure appear at the top. Below, you can see a list of included patients. The table shows whether or not each patient was included in the numerator, along with any relevant patient details for the measure, such as an order, diagnosis, or other patient information.
By reviewing patient records to determine why they were or were not included in a measure’s calculation, you can address potential problems in your workflow or PCC configuration that may alter your final percentage.
Optional: Output the Report
Click “Save as PDF” or “Print” to output a copy of the Meaningful Use Measures results.