Check Prescription Pricing and Insurance Coverage While You Prescribe
When you prepare a prescription, you can see how much it will cost out-of-pocket, whether it requires prior authorization, and if there are more cost-effective alternatives.
Video: Watch Check Prescription Pricing and Insurance Coverage While You Prescribe to see it in action.
Contents
Overview
When you prepare a prescription, PCC eRx instantly displays pricing and insurance coverage information. The information is provided in real time by the pharmacy benefit manager that administers the patient’s prescription insurance plan.
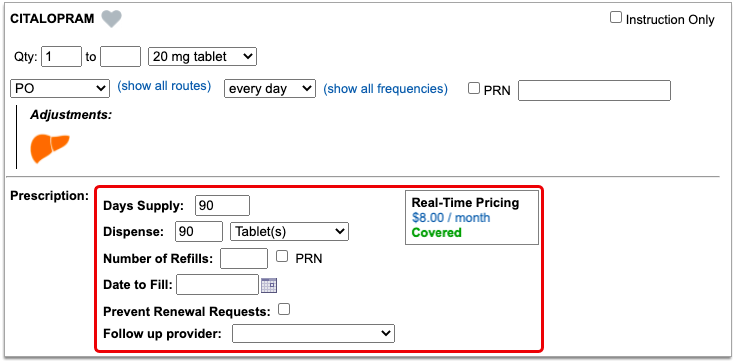
First, PCC eRx displays Real-Time Pricing.
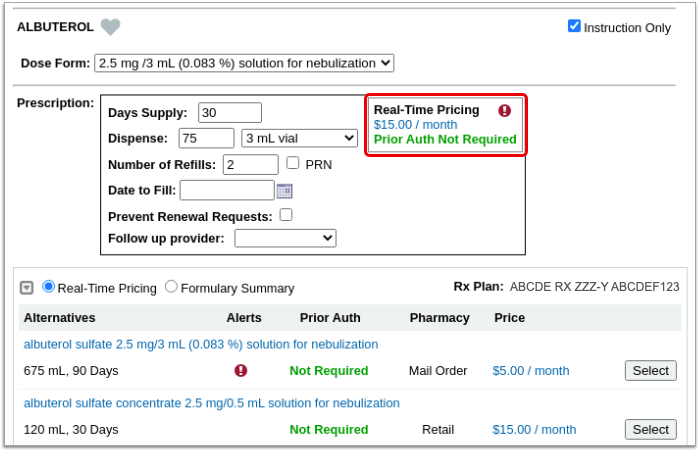
Real-Time Pricing: Real-Time Pricing can tell you exactly how much a prescription will cost out-of-pocket, whether it requires prior authorization, how much of it will apply to the patient’s deductible, and more. Real-Time Pricing displays on the prescription editing screen once you pick a medication and define a quantity, days supply, and pharmacy. These details are routed to Surescripts, the entity that enables electronic information exchange between PCC eRx and other organizations. Surescripts then asks the pharmacy benefit manager that administers the patient’s prescription insurance plan for pricing and coverage information and passes those details back to PCC eRx.
If the prescription does not contain enough information for the pharmacy benefit manager to provide Real-Time Pricing, or the plan is not set up for Real-Time Pricing, PCC eRx automatically displays a Formulary Summary instead.
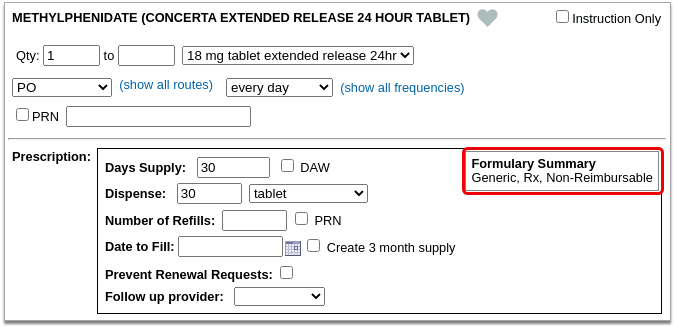
Formulary Summary: A Formulary Summary can generally tell you the copay tier for a prescription, whether the drug is on- or off-formulary, its preference level, and a dollar-sign rating as to how expensive it is out-of-pocket. The Formulary Summary displays as soon as you pick a medication and arrive at the prescription editing screen. The prescription details are routed to Surescripts, which asks the pharmacy benefit manager that administers the patient’s prescription insurance for formulary-level coverage information, then passes it back to PCC eRx. The Formulary Summary may not reflect the patient’s exact prescription benefit status, but can give a sense of how a prescription is covered under the general rules of their prescription insurance plan.
If both Real-Time Pricing and a Formulary Summary are available, you can switch between the two.

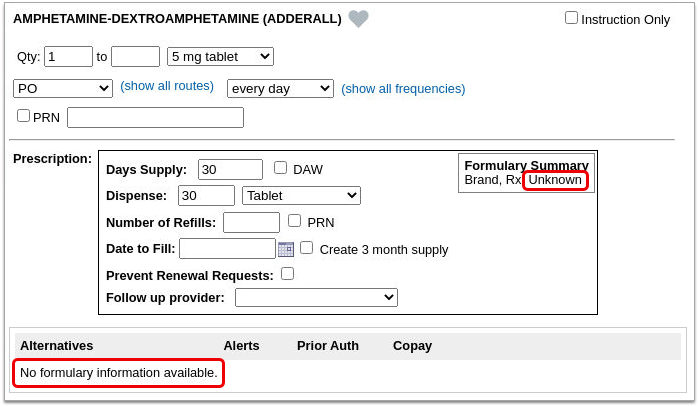
If the patient’s prescription insurance sends neither Real-Time Pricing nor a Formulary Summary, PCC eRx makes it clear that there was no response.
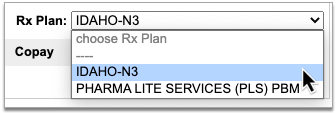
If the patient has multiple prescription insurance plans, you can switch between them to see how the prescription is covered under each one.
No Need to Change How You Collect Policy Information: PCC eRx receives the patient’s prescription insurance plan information directly from Surescripts, which relies on basic demographic details in the patient’s chart, not the information recorded in the Policies component, to find the patient’s coverage.
Each plan may suggest alternatives to your original prescription. You can switch to any alternative at the click of a button.
If you switch to an alternative or edit the original prescription, PCC eRx automatically runs a new prescription benefit check.
Usually, Real-Time Pricing and the Formulary Summary contain helpful and clear information, but sometimes they can be difficult to interpret. For help navigating confusing responses and scenarios, read What to Do About Poor or Confusing Responses.
Check Prescription Pricing and Coverage
When you prepare a prescription, you can see how much it will cost out-of-pocket, whether it requires prior authorization, and if there are more cost-effective alternatives.
Start a Prescription
Start a prescription in PCC eRx.
There are many ways to start a prescription. You can create one from scratch in the patient’s visit, renew an historic medication, or prescribe a favorite.
For detailed instructions about how to start a prescription, read Prescribe Medications.
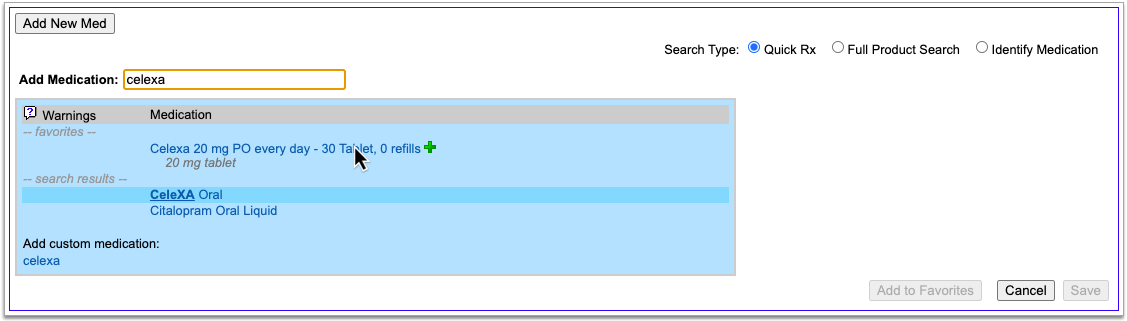
Select a Medication and Strength to See Formulary Summary Information
As soon as you choose a medication and strength for your prescription, PCC eRx starts checking how much it will cost out of pocket and how it’s covered under the patient’s prescription insurance. The results display in a box beside the prescription.
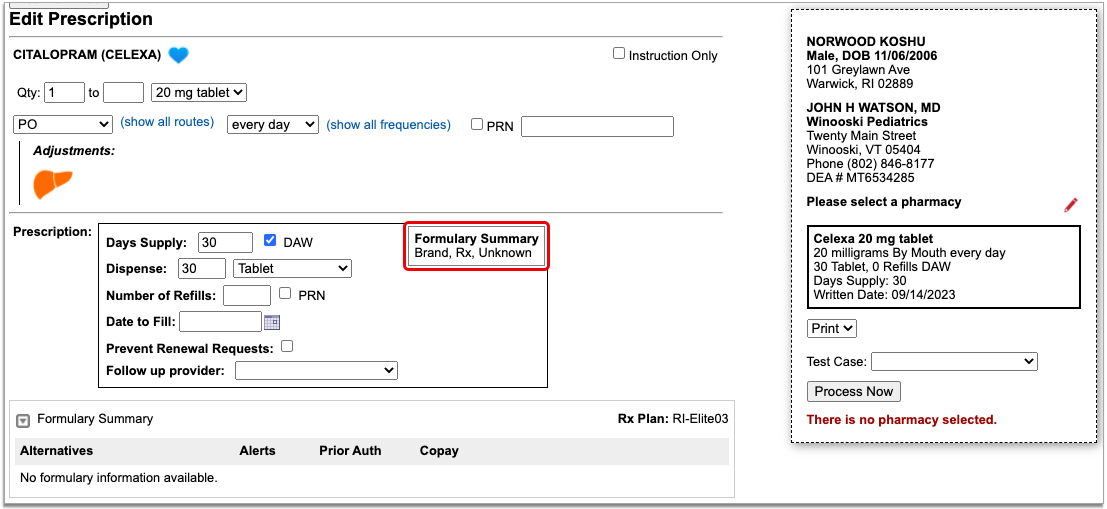
With only a medication and strength, PCC eRx can usually display a Formulary Summary result from the patient’s prescription insurance. The Formulary Summary can tell you the copay tier for the medication, whether it is on- or off-formulary, and provide a dollar-sign rating as to how expensive it is out of pocket.
Enter a Quantity, Days Supply, and Pharmacy to See Real-Time Pricing and Alerts
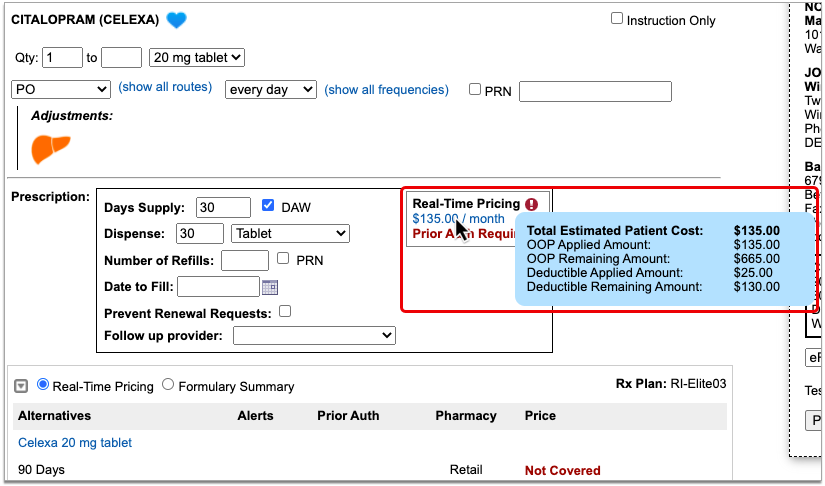
Once you enter a quantity, days supply, and pharmacy for the prescription, PCC eRx can usually display a Real-Time Pricing result from the patient’s prescription insurance.
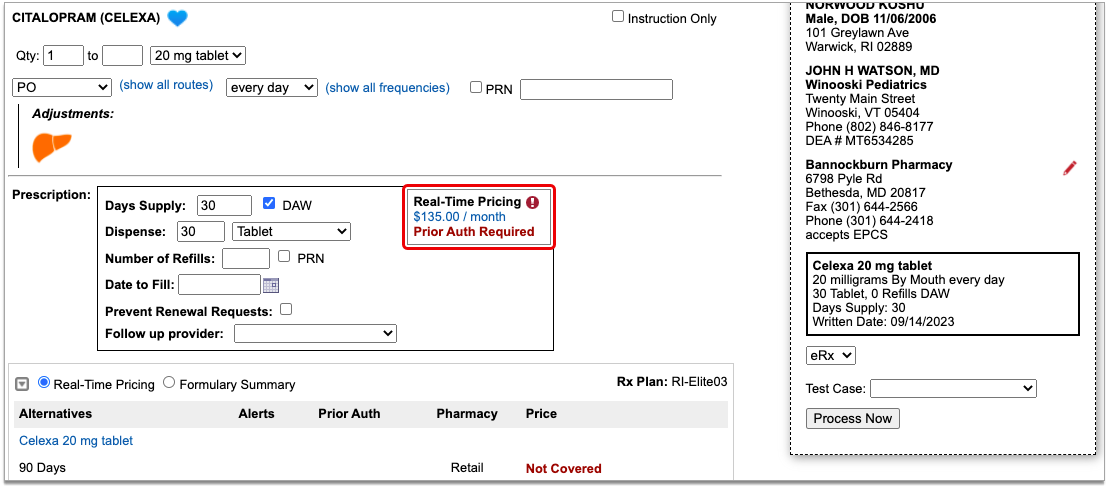
Real-Time Pricing can tell you exactly how much the prescription will cost out of pocket each month, how much of that cost will apply to the patient’s deductible, whether the medication requires prior authorization, and more.
Price
If the Real-Time Pricing response includes a price, hover over it to see if the insurance company shared how it will apply to the patient’s deductible.
Coverage Alerts
An alert icon indicates that there are coverage alerts for the prescription. Hover over the icon to view the alerts.
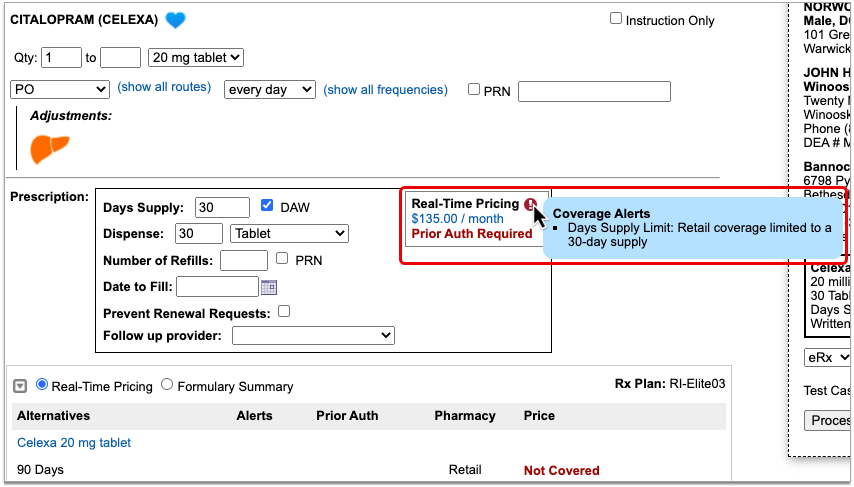
Coverage alerts may include information such as days supply limits, next fill dates, and coverage limitations based on age and sex.
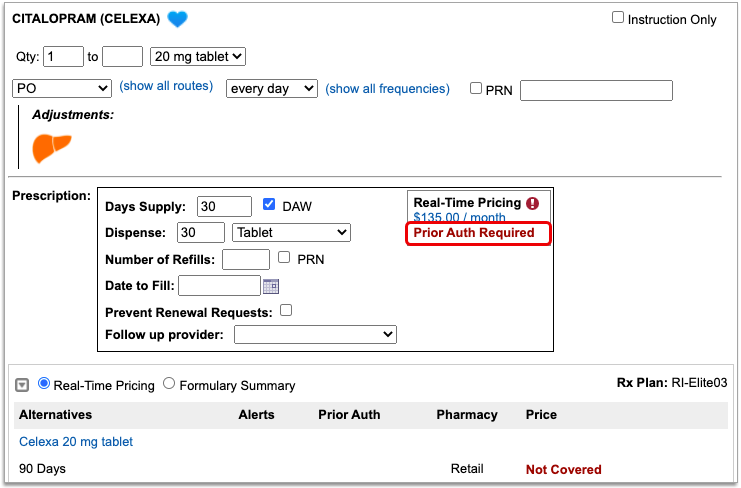
Prior Authorization and Coverage Status
The insurance plan may also send a prior authorization or coverage status, which displays in green if the medication is covered or does not require prior authorization, or in red if the prescription is not covered or does requires prior authorization.
Optionally, Check a Different Plan
The name of the plan that provided the pricing and coverage information displays in the “Rx Plan” field beneath the prescription. If the patient has multiple prescription insurance plans, the Rx Plan field becomes a drop-down and you can switch between them.
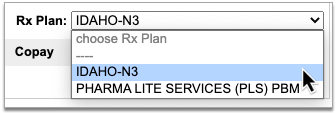
When you switch to a different plan, PCC eRx checks it for pricing and coverage information and displays those results beside the prescription.
Optionally, Switch Between Real-Time Pricing and Formulary Results
The radio buttons beneath your prescription indicate which types of responses the patient’s prescription insurance sent. If you see a Formulary Summary in addition to the Real-Time Pricing response, you can select it to see what it contains.
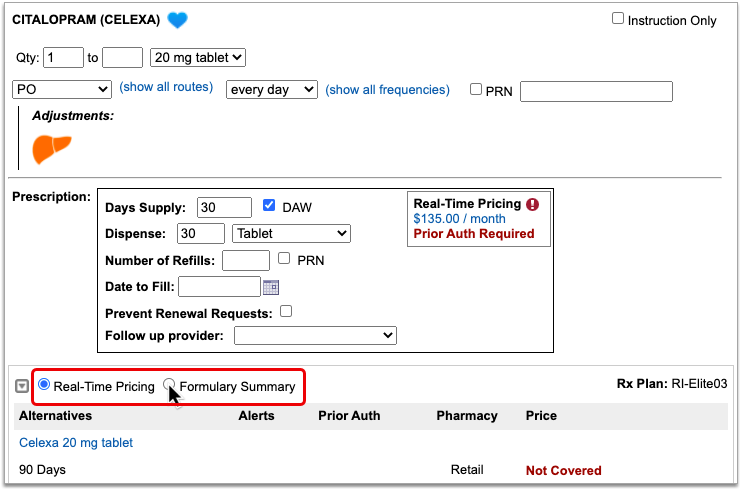
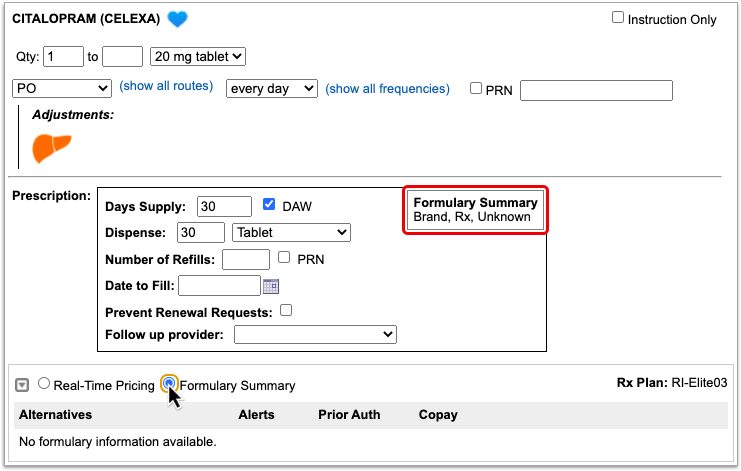
PCC eRx defaults to displaying Real-Time Pricing, since that response usually contains more concrete and actionable information. If the plan could not provide any response at all, PCC eRx indicates that there was no coverage information to be found.
Prescription pricing and coverage information is provided in real time by the pharmacy benefit manager responsible for administering the patient’s prescription insurance plan. PCC eRx connects with the pharmacy benefit manager through Surescripts, the vendor who enables electronic information exchange between PCC eRx, pharmacies, and other entities.
Surescripts and the pharmacy benefit manager use demographic information — not the insurance policy details recorded in PCC EHR — to find the patient’s prescription insurance plans.
Check Alternatives
Prescription insurance plans can send alternatives for you to consider instead of the prescription you wrote. Those alternatives display in a table beneath your prescription.
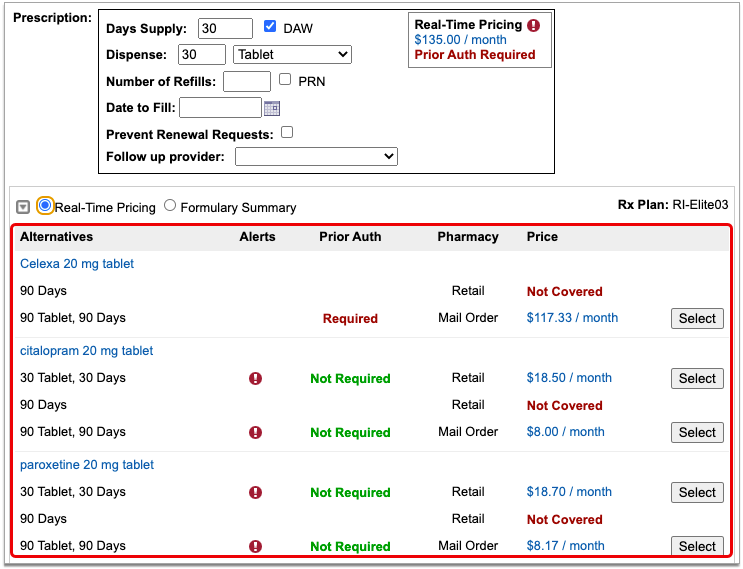
Alternatives may be cheaper for the patient, have fewer restrictions, or be covered without prior authorization.
If the original prescription you wrote is expensive, not covered, or requires prior authorization, see if one of the alternatives could work instead.
Alternatives may specify a different quantity, pharmacy type, or medication than the original prescription. Use your best clinical judgment to determine if one of the alternatives might be appropriate for your patient.
Easy Price Comparison: To ease comparison between the original prescription and alternatives, all prices are expressed as a cost per month.
Optionally Hide Alternatives: Click the gray disclosure triangle in the top left corner of the Alternatives section to hide it from view. Click the disclosure triangle again to show hidden alternatives. If you want the Alternatives section to be collapsed by default, update your Real-Time Pricing and Formulary display preference on the My Settings page.
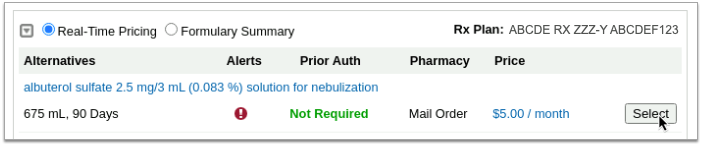
Optionally, Prescribe an Alternative
If one of the alternatives suggested by the patient’s prescription insurance proves to be a good option, click the “Select” button to switch to it. As soon as you click “Select,” PCC eRx replaces the original prescription with the selected alternative and displays the pricing and coverage information for it.
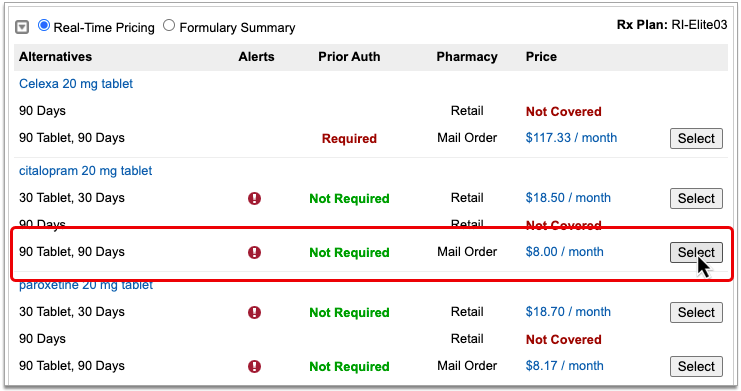
If you select an alternative that lists Mail Order as the pharmacy type, PCC eRx automatically updates the prescription to use the mail order pharmacy suggested by the insurance plan. If the patient prefers to use a different mail order pharmacy, you can manually update the pharmacy on the prescription to reflect the patient’s preference.
Double-Check Before and After You Select: Before you select an alternative, double-check the drug, quantity, duration, and other details to ensure that it is clinically appropriate for your patient. After you select an alternative, verify that the dosing instructions for the prescription are accurate, especially if the alternative is in a different form than the original medication. Edit the prescription for the alternative as needed until the instructions are correct for your patient.
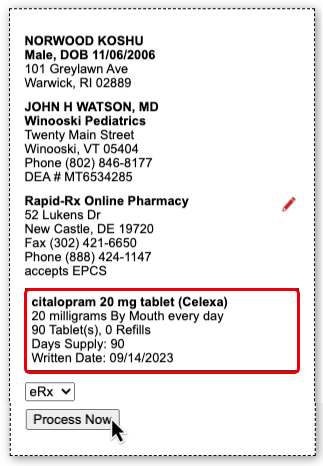
Process the Prescription
Once you are satisfied with the prescription, process and send it to the pharmacy.
What to Do About Poor, Confusing, or Nonexistent Responses
Not all prescription insurance plans respond the same way to prescription benefit checks, and sometimes the responses that do come through are unhelpful, sparse, or confusing. While PCC does not control the messages that come from prescription insurance plans and cannot provide definitive interpretations of their responses, there are some common cases that have relatively straightforward solutions. Read on to learn about those cases and how to navigate them:
-
'No Matching Coverage Details Provided' Message: When you see the message “No matching coverage details provided” in a Real-Time Pricing response, it indicates that the patient’s prescription insurance did not provide comment on the prescription as written and likely wants you to prescribe an alternative. This is most common when the total dispense quantity indicated on your prescription is less than the minimum standard package size that can be dispensed by the pharmacy. Review the alternatives suggested by the patient’s prescription insurance to see how standard package sizes are covered and optionally select one that is appropriate for your patient.
-
'Pharmacy Not Found' Message: Certain prescription insurance plans only cover prescriptions that route through mail order pharmacies and reply with the message “Pharmacy not found” when assessing a prescription that indicates a retail pharmacy. You can ignore the message if the prescription is covered under one of the patient’s other plans, or consider switching the prescription to a mail order pharmacy.
-
No Coverage Details and Only One Alternative: If no coverage details are provided for a prescription that you wrote and the prescription insurance plan only suggests a single alternative in a quantity that cannot cover the entire course of the patient’s treatment, it usually means that the plan only covers that lesser quantity of medication for the indicated timespan.
-
Not Covered and No Good Alternatives: If the prescription is not covered, has a coverage alert, and none of the suggested alternatives match what you are trying to prescribe, hover over the alert to see if it contains a description in words about what the prescription insurance plan will cover. For example, if the coverage alert indicates that a different quantity would be covered, try changing your prescription to match that advice, then wait to see if Real-Time Pricing updates with a more useful response.
-
Albuterol Inhalers: To reduce clicks and prescribe the most cost-effective option when your patient needs an albuterol inhaler, consider the following: 1) Many prescription insurance plans appear to prefer 6.7g albuterol inhalers to the larger, 18g ones. 2) If you write prescriptions for a total number of inhalers rather than a total number of grams, prescription insurance plans may not be able to provide coverage details.
-
Contradiction Between Real-Time Pricing and the Formulary Summary: If you notice a contradiction between the Real-Time Pricing and Formulary Summary for a prescription, defer to the Real-Time Pricing.
Nonexistent Responses
Some pharmacy benefit managers do not share real-time pricing and coverage insights. PCC and Surescripts have prepared a letter template that you can use to encourage them to do so (shown below).
PCC can review your practice’s specific Real-Time Pricing response rate and let you know which prescription insurance plans are not currently sharing real-time pricing and coverage insights. Contact PCC Support for help customizing this letter and learning to whom it would best be addressed.
