Review an Encounter’s Billing History
Use the Billing History in a patient’s chart to see full details of what was billed for an encounter, what payments were collected, when claims were sent, acknowledged, and received, and more.
Video: Watch Work With a Patient’s Billing History to learn more.
Contents
- 1 Visit the Billing History
- 2 Review the Billing History for a Specific Encounter
- 3 Review Charge and Payment History for an Encounter
- 4 Review Claim History for an Encounter
- 5 Read Claim Files, Acknowledgements, and Other Responses for an Encounter
- 6 Print an Encounter’s Complete Billing History
- 7 Edit Encounter Charges and Claim Details and Resubmit
- 8 Other Ways to Review What Was Billed for an Encounter
- 9 Look Up ICD-10 Codes for a Patient’s Diagnoses During an Encounter
- 10 Create a New Encounter
Visit the Billing History
Click the “Billing History” button inside the History section of a patient’s chart to review the billing history for any encounter.
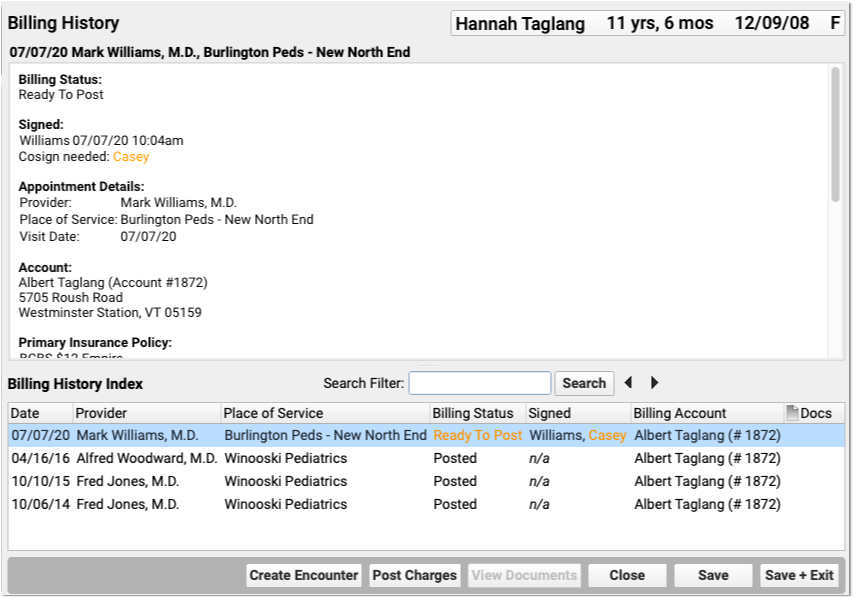
Office visits, telemedicine encounters, phone notes, portal messages, hospital charges, and administrative encounters that have been billed or may be billable appear in the index at the bottom.
When Do Encounters Appear in the History?: An appointment has a billing history entry as soon as an encounter’s status is set to “Arrived” or the patient is checked in. Phone notes and portal messages only have a billing history if the clinician clicked “Bill” and selected “Ready for Billing”. Hospital and administrative encounters appear after a user creates the encounter and posts the charges.
Review the Billing History for a Specific Encounter
Click on an encounter in the index to see details in the window above.
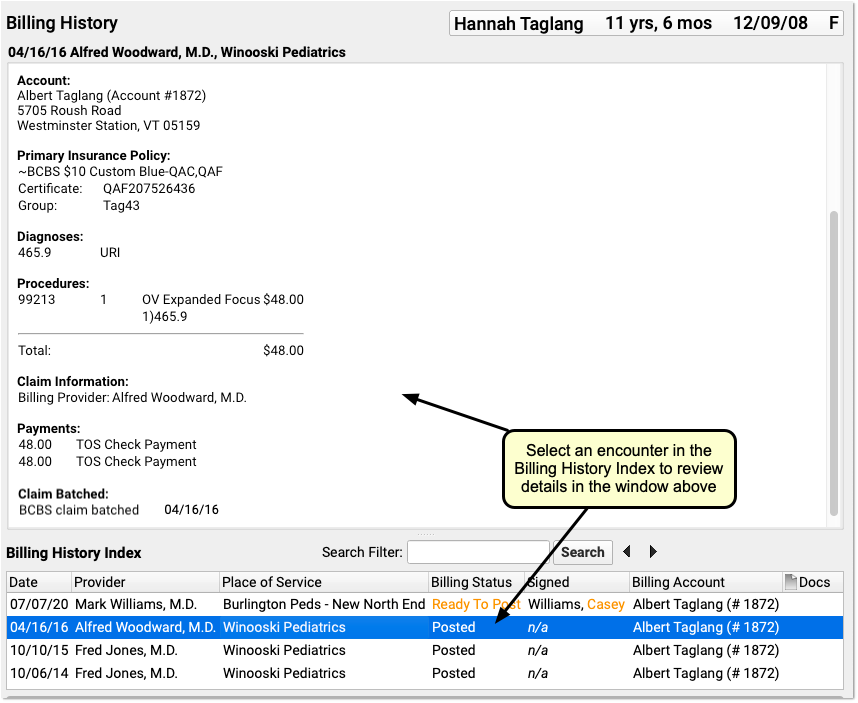
You can review encounter billing details, such as what diagnoses and procedures were posted, a payment history for the encounter, and a claim history for the encounter.
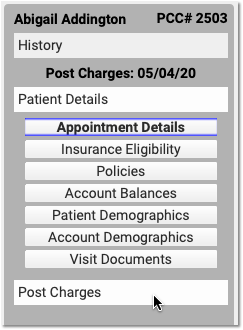
If an encounter still has the “Ready to Post” status, or has new items added to post, you can work with those encounters on this screen. Select the encounter and click “Post Charges” (or double-click on the encounter) to open up Post Charges.

Review Attached Documents: You can review any documents attached to an encounter in the Billing History section of the chart. For example, if a user attached a scanned insurance card, a hospital note, or other document to an encounter, you can double-click to open it.
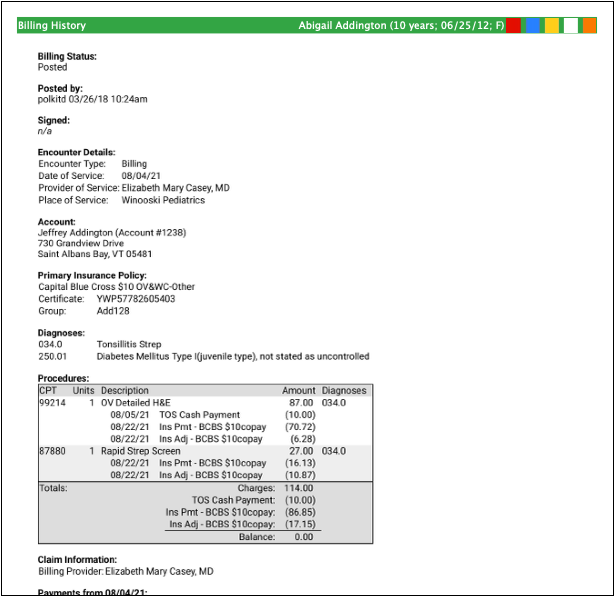
Review Charge and Payment History for an Encounter
In the Procedures section of an encounter’s billing history, you can review charges for the encounter and a history of all payments.
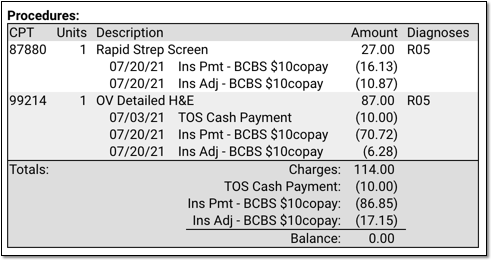
For each charge, you can see personal payments, insurance payments, and adjustments.
If any unapplied (or “unlinked”) payments on an account are paying off charges, you will see the “Payment (Unapplied)” amount indicated for each charge and in the totals section.
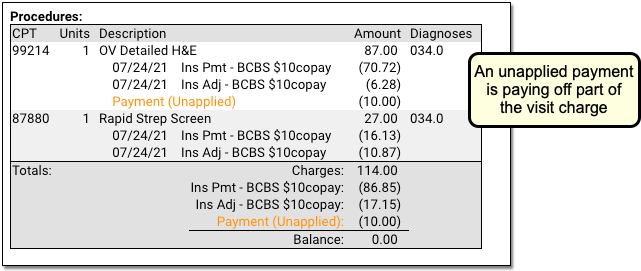
In the Payments section, you can review all payments posted on the same date as the encounter. To configure which payment types appear in this section, contact PCC Support.
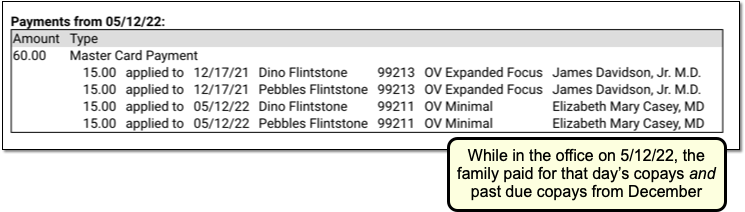
For each payment, you can review what charges the payment applies towards.
For more details about reviewing payment history, see Review Payment History and Edit Payments.
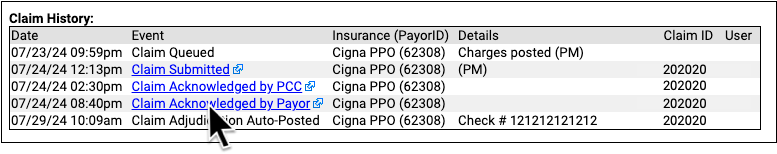
Review Claim History for an Encounter
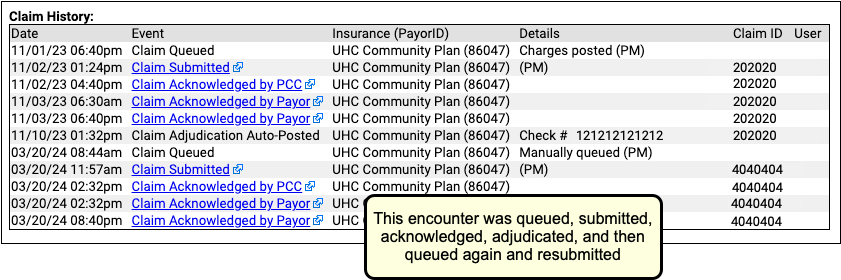
When you need to understand when a claim was sent, acknowledged, paid, or resubmitted, use the Claim History found in the encounter’s Billing History.
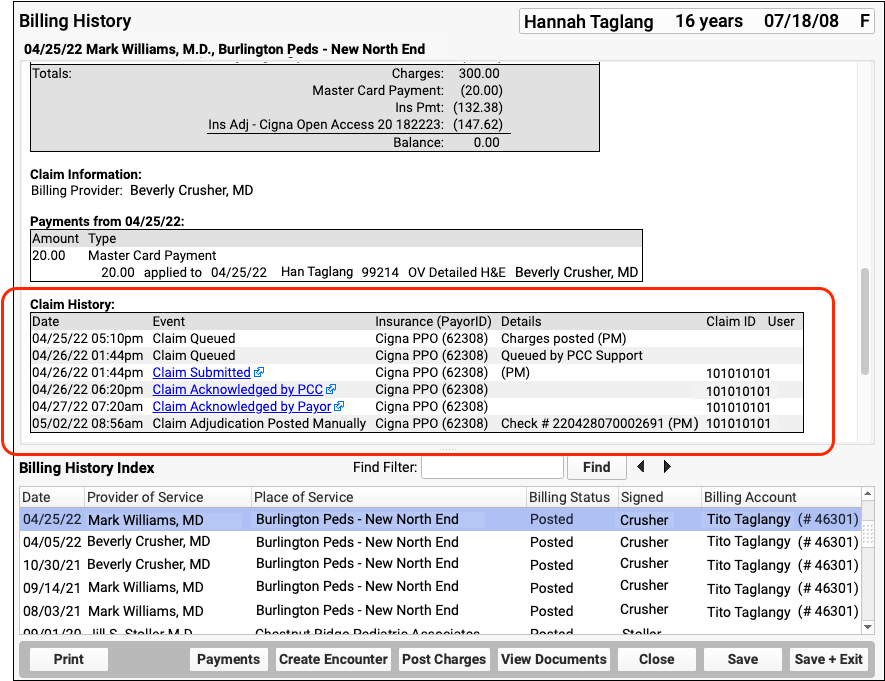
The Claim History shows the lifecycle of all claims for the encounter, from submission to resolution. You can see when a claim was queued, held, delayed, processed, received by PCC’s clearinghouse, acknowledged by the payor, and more.
For each event, you can see the date, the event, and the insurance plan. When available in your system’s records, the component displays additional details, the claim ID, and the user who performed the action.
If an encounter was submitted multiple times, the claim history will show you each submission along with claim acknowledgements and other events.
Read Claim Files, Acknowledgements, and Other Responses for an Encounter
When you need to dig deeper into a problem claim, you may want to review the claim submission log, acknowledgement, or other electronic response from a payor. When an electronic record is available for a claim event, you can click on a link to open it.
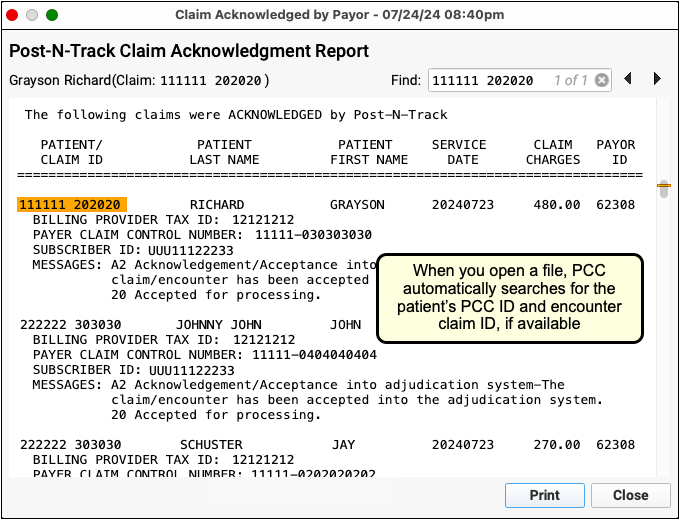
You can review the outgoing electronic claim file, claim acknowledgements, rejections, and most other responses for claims. (To review the ERA, use the Electronic Remittance Advice tool.)
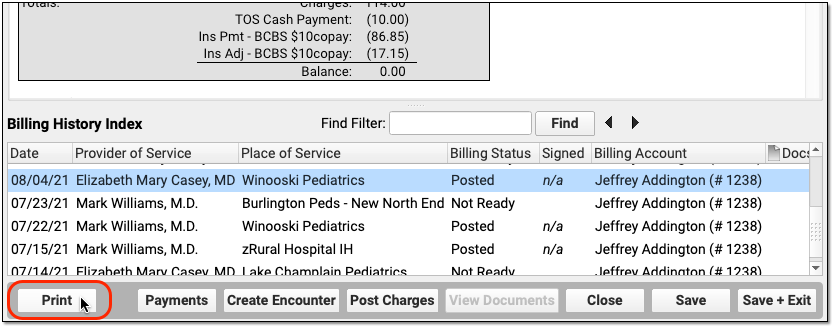
Print an Encounter’s Complete Billing History
Select any encounter and click “Print” to print the billing history. It will include all charge, payment, and adjustment information along with details about the claim.
Edit Encounter Charges and Claim Details and Resubmit
If you need to edit the charges on an encounter or claim details, such as the place of service or additional information submitted with the claim, select and encounter and click “Edit Charges”.
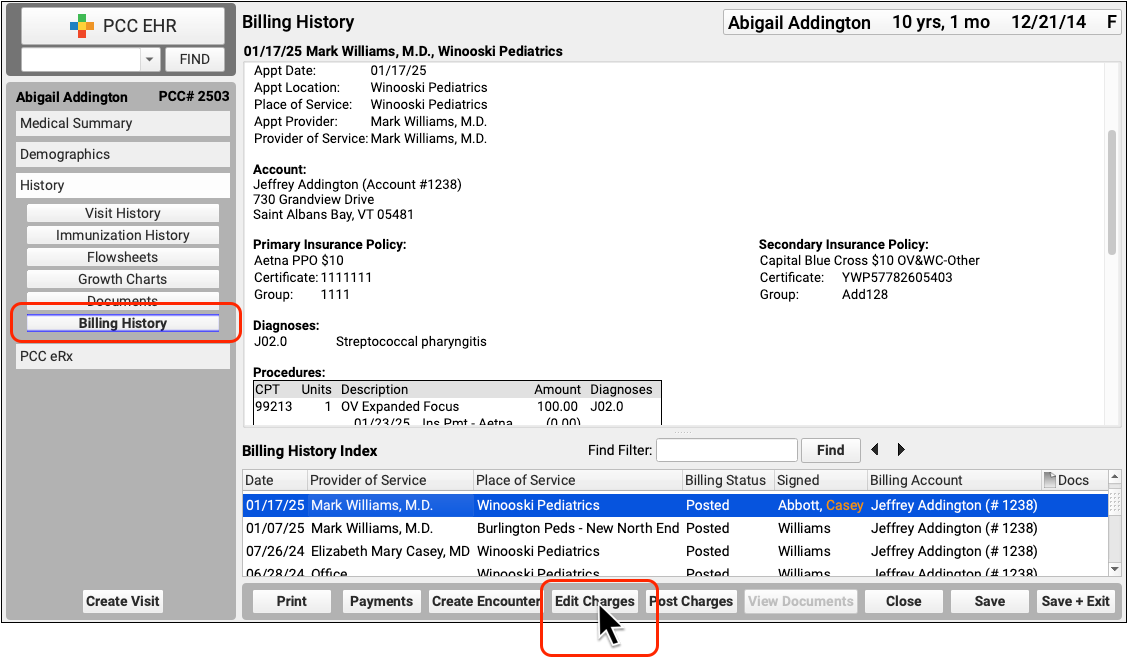
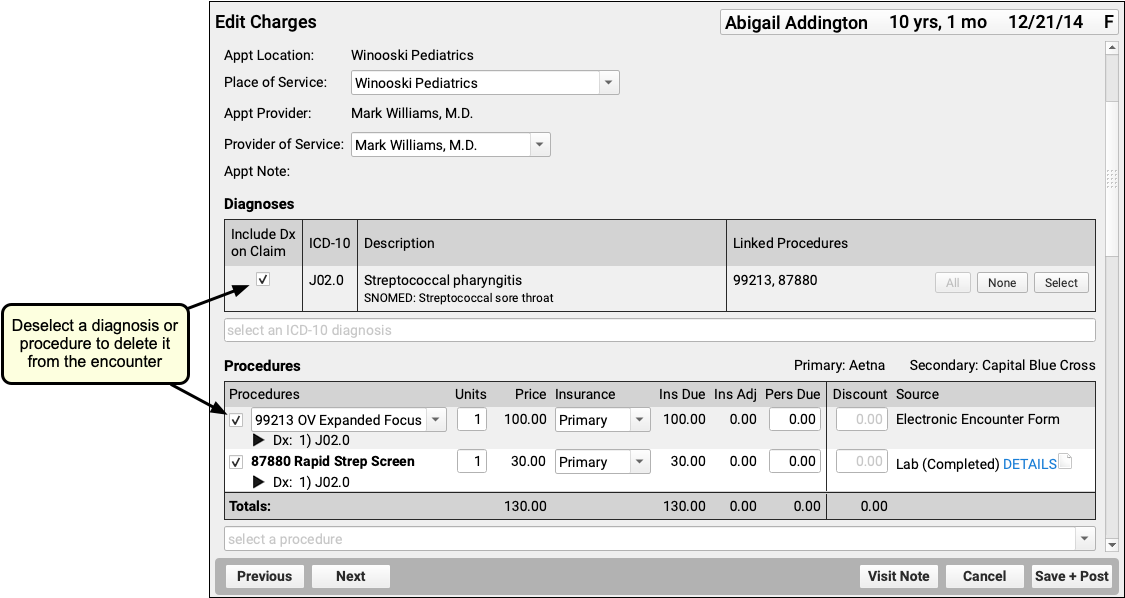
Read Edit Encounter Charges and Other Claim Information to learn more.
Other Ways to Review What Was Billed for an Encounter
In addition to the Billing History, there are two other ways to revisit the diagnoses and procedures for an encounter.
Open the Post Charges Workflow
You can reopen the Post Charges workflow after charges are posted. From there you can see what was posted and optionally add additional items to the claim. Reopen the Post Charges workflow from the patient’s Billing History as shown above or from the Schedule screen.
Click “Posted” or “New Items” on the Schedule screen to return to the Post Charges screen for an encounter your practice has already posted.
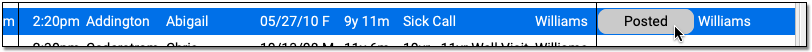
For information about the Post Charges window, read Post Charges and Check Out Patients in PCC EHR.
Review Diagnoses and Procedures on a Chart Note’s Electronic Encounter Form
You can also open a chart note’s “Bill” window and review the Electronic Encounter Form, which shows the selections originally made by the clinician.
Open the Patient Chart
Use the Find tool or double-click on an appointment to open a patient’s chart.
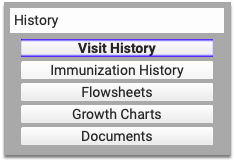
Click “Visit History”
Go to the Visit History section of the chart.
Find the Visit Date You Wish to Review
Use the list at the bottom to locate and select the visit you wish to review.
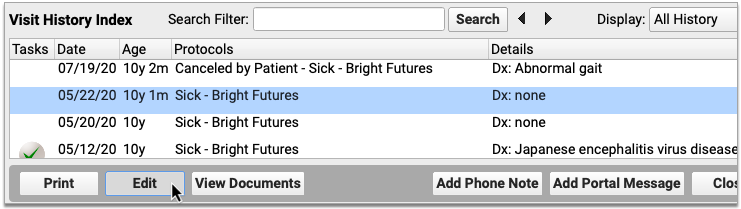
Double-Click or Click “Edit”
Click Edit to open the chart note. It will appear along with chart navigation buttons.
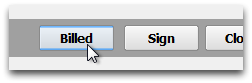
Click “Billed”
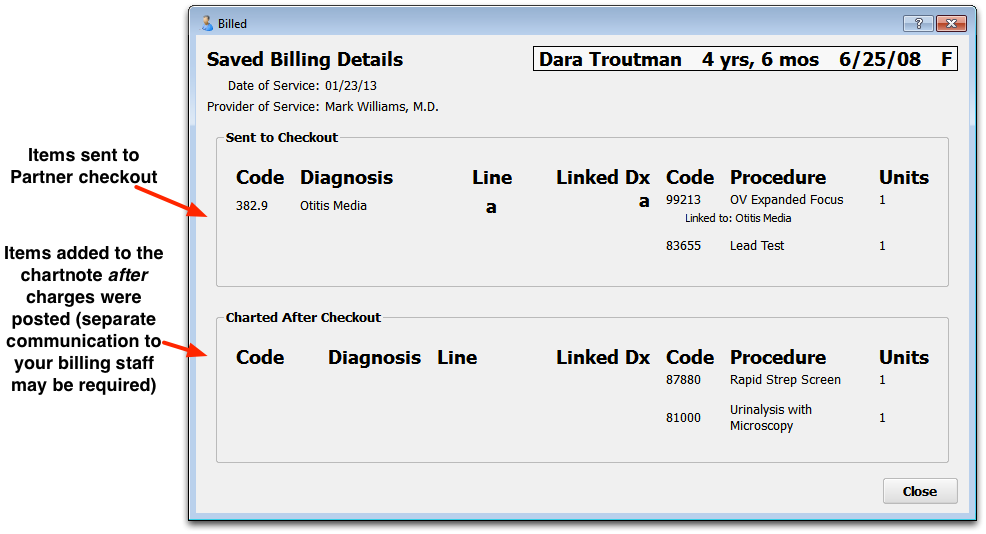
Click the “Billed” button at the bottom of the chart note to open the visit’s saved encounter form.
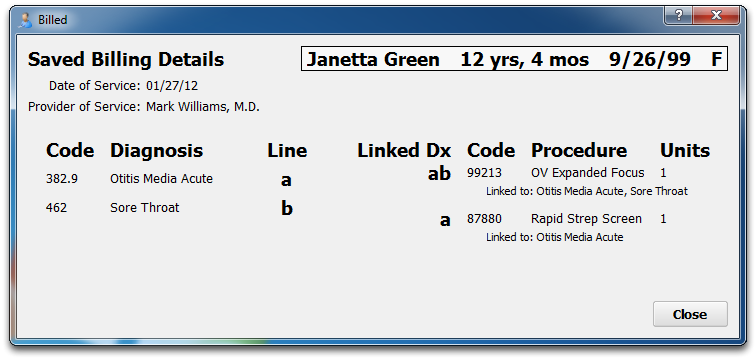
What Was Selected, Not What Was Billed: The Billed window retains a record of the procedures and diagnoses on the electronic encounter form, how they were linked, and how many units were indicated. After that information is made ready for billing, however, the biller can adjust that information when they post the charges and file the claim. The Billed window is a static record of what was made ready for billing by the clinician and does not reflect later changes.
Added After Posting: If a clinician added diagnoses or orders to the chart note after the visit was posted, those items will appear in a special section on the encounter form.
Look Up ICD-10 Codes for a Patient’s Diagnoses During an Encounter
If you are filling out a form or need the ICD-10 code billed for a patient’s diagnosis during an encounter, you can use the Diagnosis Flowsheet in a patient’s chart to quickly get the codes you need.
For more information, read the Look Up ICD-10 Codes for Referrals, DME, Requisitions, and Pre-Authorizations article.
Create a New Encounter
Billers typically post charges for appointments on the Schedule screen, or post charges for phone notes or portal messages from the Messaging queue. You can also create a new encounter in the Billing History section of a patient’s chart.
Click “Create Encounter” to post charges of any kind, without a scheduled appointment. For example, you may want to post a hospital encounter or administrative fees.
