Add an Attachment Code to a Claim
If a claim requires an attachment, such as an EOB from the primary, a certificate of medical necessity, a discharge summary, or other clinical documentation, use PCC EHR to add attachment information to the claim.
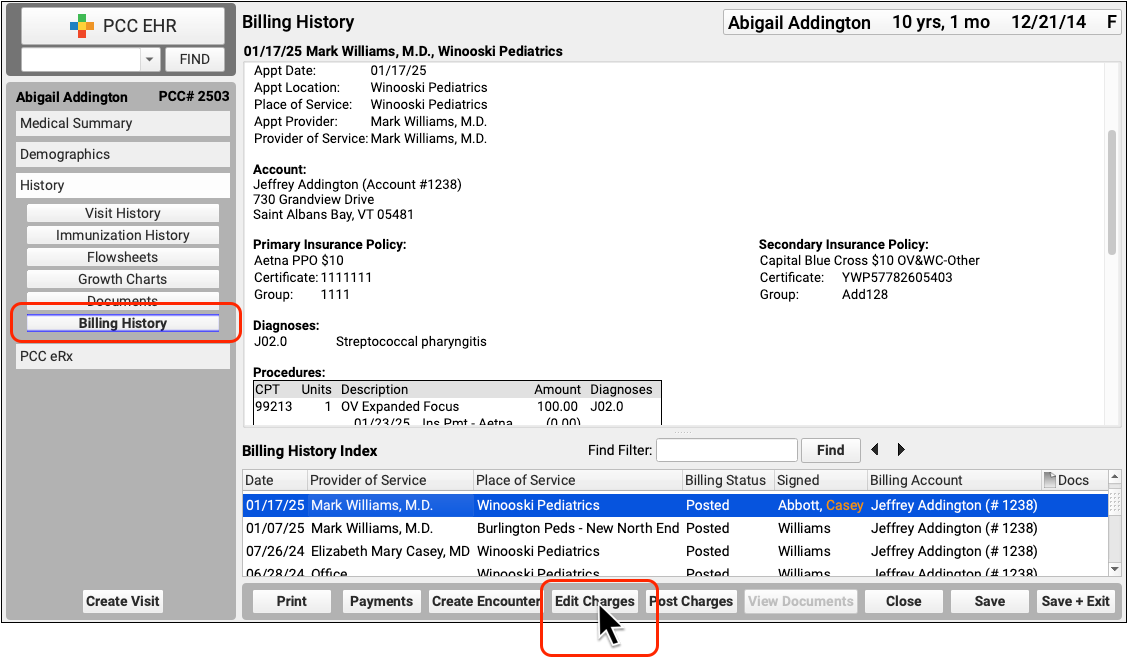
Whenever a claim requires an attachment, select the encounter in the Billing History section of the chart and click “Edit Charges”.
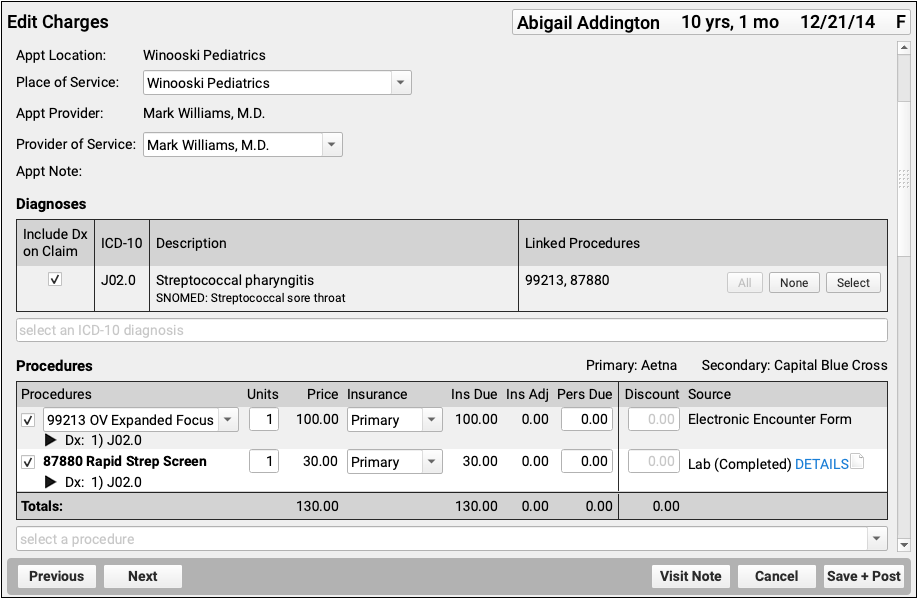
Depending on the circumstances, you may need to make other changes to the encounter or the charges. For example, if you’ve already processed a payor response, you should check the Procedures component to make sure the charges are currently pending the correct responsible party for the claim you wish to send.
Next, visit the Claim Information section and click “Add Attachment”.
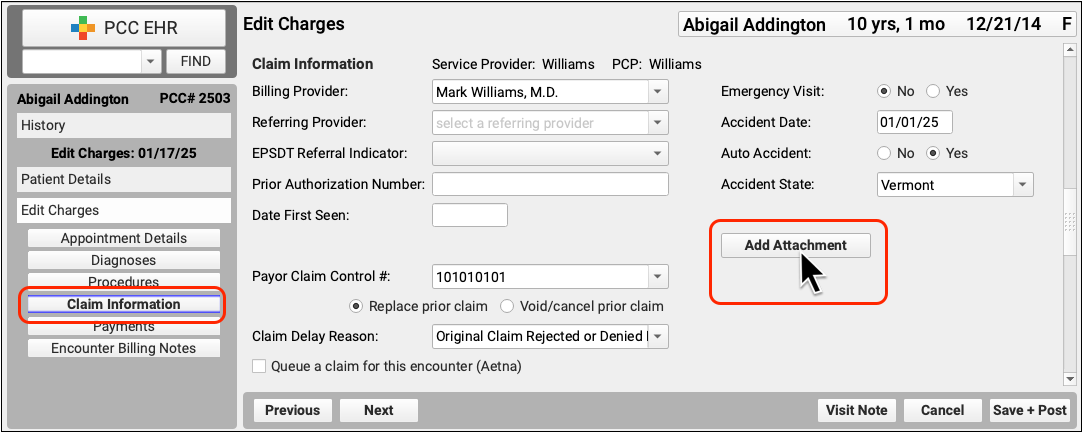
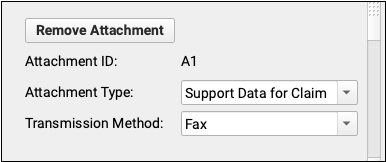
PCC EHR will create a unique attachment ID. You can then set the Attachment Type and Transmission Method. These values will be submitted on the electronic claim.
Double-check that the checkbox for claim submission is checked, and that it is for the correct payor.
Then click “Save + Post” to save the attachment information and queue up a new claim.
For more details about editing charges and encounter and claim details, read Edit Encounter Charges and Claim Information.
Claim Attachment Information is Per Claim: When you add attachment information to an encounter, it is added to the next claim queued up for that encounter. If you later need to resubmit or send the claim to a different payor, for example, you should use the Claim Information section to add a new attachment.
