Report on Productivity in the Report Library
Practices can report on provider and practice productivity over time using the Total Charges and Payments by Provider and Month report. This report is helpful for practices using a revenue-based compensation model for clinicians. Practices looking to minimize unpaid charges can use this report to compare payments by procedure group as well.
To get an overview of productivity trends at your practice, visit the Practice Vitals Dashboard productivity page.
Contents
Run the Total Charges and Payments by Provider and Month Report
To view provider or practice productivity, or to get an overview of charges and payments by month, you can run the Total Charges and Payments by Provider and Month Report in the Report Library.
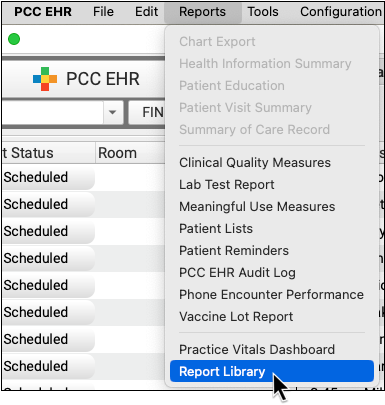
Open the Report Library
Open the Report Library from the Reports menu in PCC EHR.
Select the Report
In the Financial Oversight category, select the Total Charges and Payments by Provider and Month report.
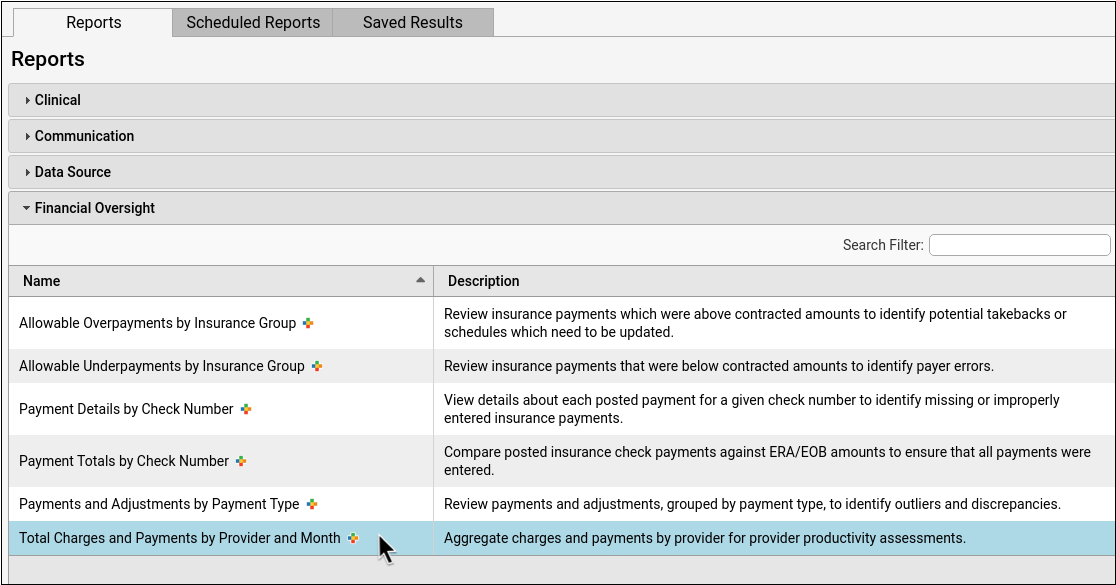
Limit Access to This Report: Users with permission to manage categories in the Report Library can edit the Financial Oversight category in the Manage Categories window and uncheck roles to remove access. See Restrict Access to Reports in the Report Library for more information.
Select Your Criteria
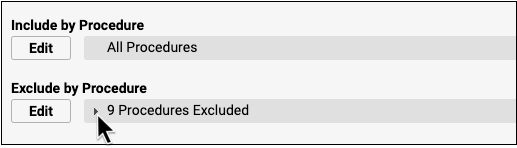
You can select criteria to control the results that display on your report output. For practices using this report to identify revenue generated, or for clinician compensation models, common procedure exclusions for this report are immunizations, injections, and miscellaneous office fees.
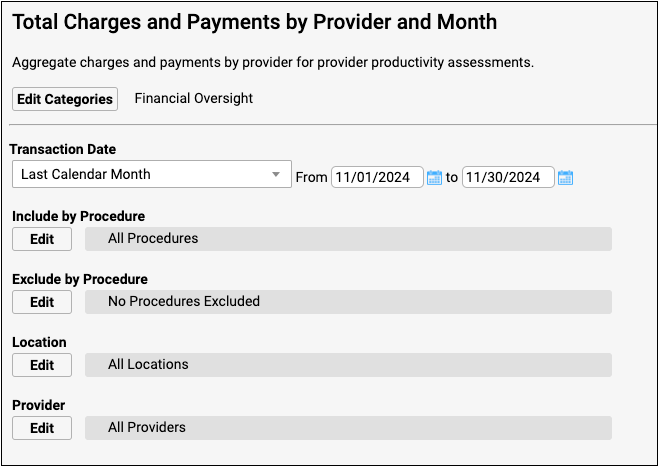
To explore your options for this report’s criteria, read the Select Criteria Options section below.
View the Report Results
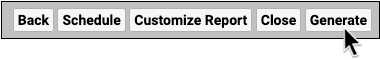
Click “View Results” to run the report.
Adjust Output
You can sort, arrange, and filter your report output in a variety of ways.
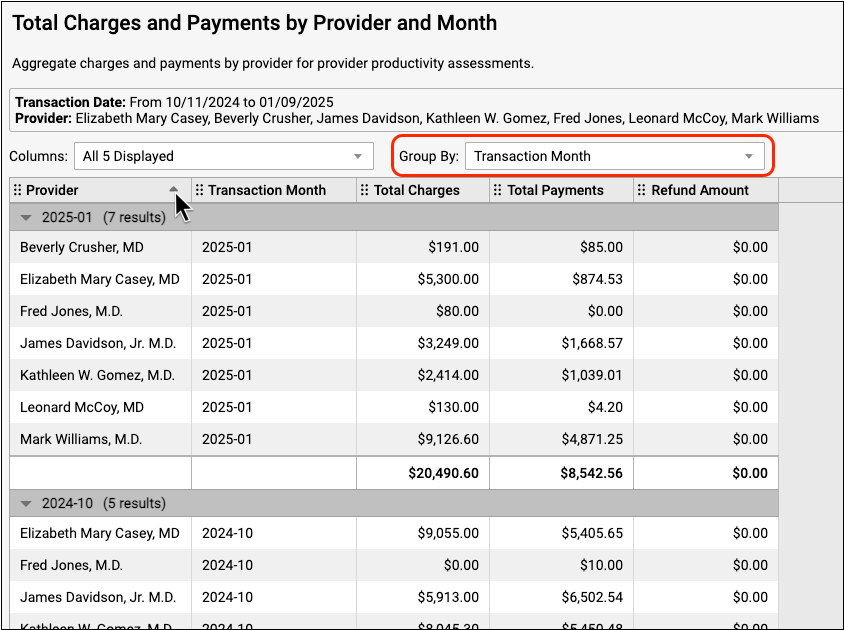
The Group By drop-down will group entries by the criteria that you select. If you group by transaction month, for example, the report data will be organized by month. Numerical columns subtotal at the bottom of each group.
You can further organize each section by clicking the column headers to sort the information by the column of your choice.
To learn more about navigating and working with report output, read Run Reports in the PCC EHR Report Library.
Optionally Export or Print
You can choose your output format and print or export your report to PDF or CSV.

20,000 Row Limit: Exports from the report output (View Results screen) in the Report Library are currently limited to 20,000 rows. If your output appears to be exactly 20,000 rows long, it may not contain all of the information that you are looking for. If this occurs, return to the report configuration screen and click “Export Report” to get your full report. Read Export Large Data Sets from the Report Library to learn more.
Select Criteria Options
Use the section below to understand your financial oversight criteria options.
Choose Your Transaction Date Range
You can choose your date range using the drop-down list, the date fields, or the calendar icon.
You may wish to compare the final report output to the payments deposited into your bank account during the same transaction date range that you chose to display on the report.
Transaction Date Range Covers Both Payments and Charges: The default, recommended version of this report runs by transaction date for both payments and charges.
Payment Transaction Date: Payment Transaction Date is the date found on the check, EOB, or ERA. Payments will display on this report when they have a payment transaction date that falls within your selected transaction date range.
Charge Transaction Date: The charge transaction date is the Date of Service (DOS). This is the date on which the patient received care. Charges will display on this report when they have a charge transaction date that falls within your selected transaction date range.
What About Posting Dates?: You may be used to seeing charge posting dates and payment posting dates on some of your financial reports.
PCC does not recommend running this particular report by posting date, but the option is available during customization.
For reference, the charge posting date is the date the charge was posted (entered) on your system and the payment posting date is the date that the payment was posted (entered) on your system.
Transaction Date Example for a Single Patient Visit
A patient came in for a well visit on January 31st. This is the Date of Service (DOS) and the charge transaction date. The practice’s biller posted the encounter charges on the following business day, February 3rd. This is the charge posting date. After processing the claim, the payer sent a check or ERA on March 8th. This is the payment transaction date or Electronic Funds Transfer (EFT) date. Finally, the biller posted the payment on March 12th. This is the payment posting date.
The Total Charges and Payments by Provider and Month report displays payments organized by the transaction date. If you chose a transaction date range for only the month of March, the report output would display the payment from the example visit, but not the charge from the example visit. If you chose a transaction date range of January through March, the report output would display the charge as well as the payment from the example visit.
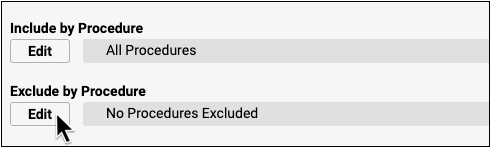
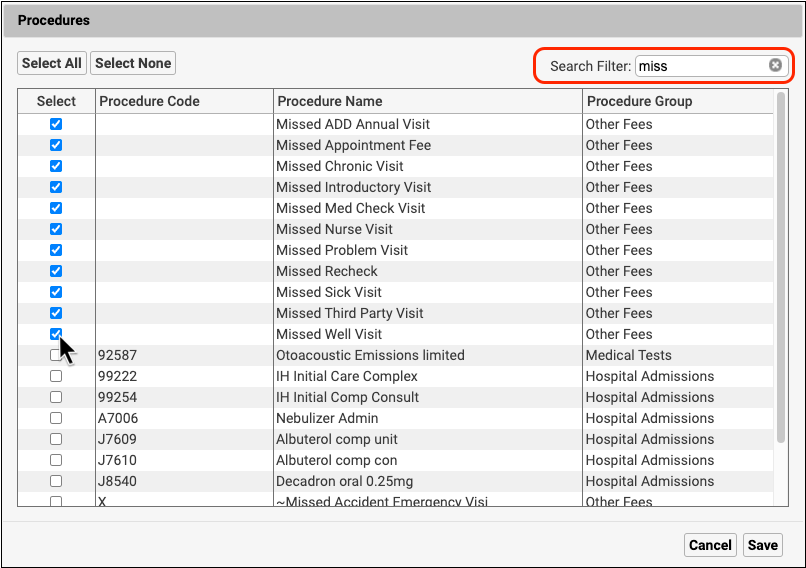
Include by Procedure
The default for this report is to include all procedures. Click “Edit” and use the search filter to find and select procedures by name, group, or procedure code.
To run a report for a specific procedure or procedure group, select the procedures from the Include by Procedure list. Your report will only include the charges and payments attributed to the procedures you chose, so you do not need to exclude any procedures.
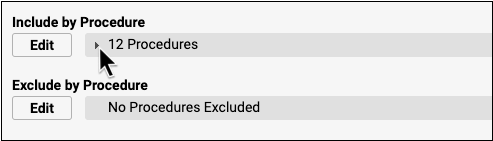
To run a report including charges and payments attributed to all procedures except a few, leave the Include by Procedure default of All Procedures. Then exclude the procedures you don’t want included by selecting them on the Exclude by Procedure list.
To learn more about including and excluding criteria in reports, visit Run Reports in the PCC EHR Report Library
Exclude by Procedure
The default for this report is to exclude no procedures. Click “Edit” and use the search filter to find and select procedures by name, group, or procedure code.
Select Locations
The default setting for this report includes all locations in the report output. If you select a location to include before you generate the report, only that location’s data will be included in the report output.
Select Providers
The default setting for this report includes all providers of service in the report output. If you select a provider to include before you generate the report, only that provider’s data will be included in the report output.
Provider of service is set when charges are posted or entered manually during payment posting.
Customize to Identify Additional Columns and Criteria
The Total Charges and Payments by Provider and Month report uses aggregate data that can be organized by including columns during report customization and by sorting the report output.
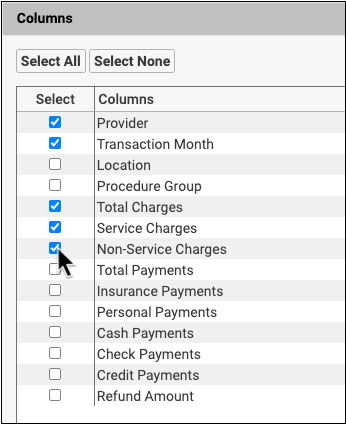
When you customize this report to include additional criteria, such as location and procedure, you must select the criteria as well as the column in order for the criteria to display as a column in the report output. To learn more about customizing a report, read Create a Custom Report.
Optionally Add a Column to Subtotal by Location
To display location and other additional columns in your report output, customize your report and select the columns you wish to include.
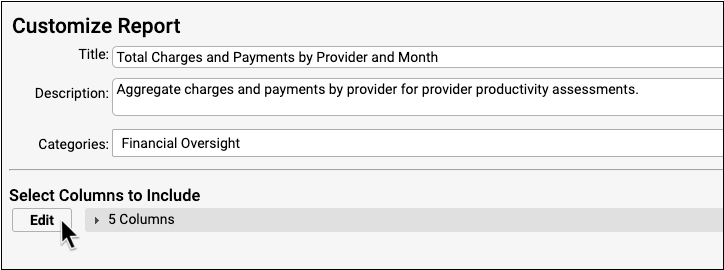
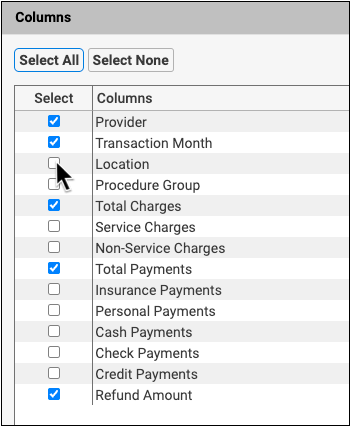
You can group the report by location so that the total charges and total payments subtotal within each location.
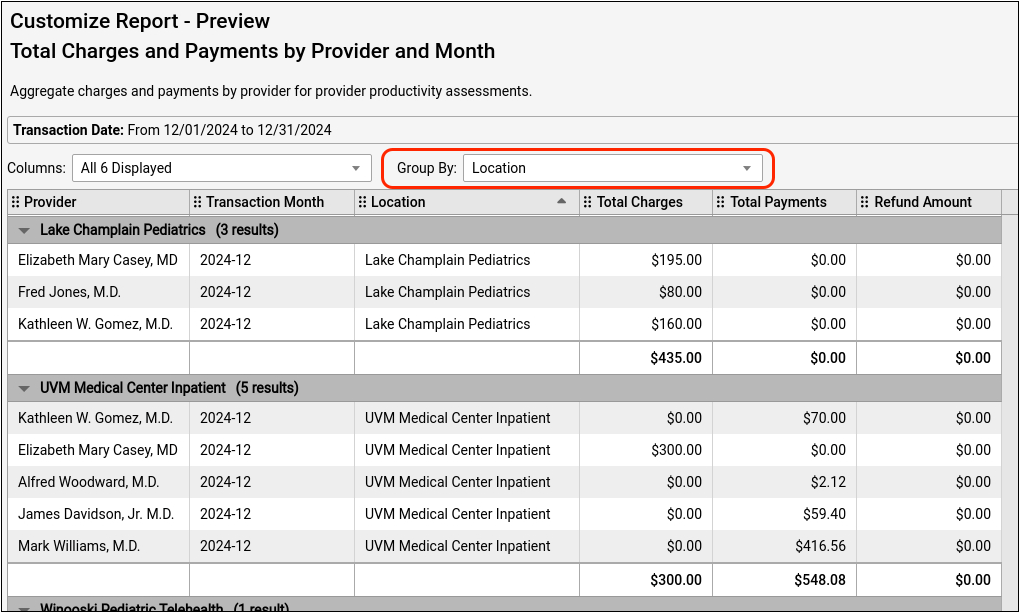
For more information on how to work with your report output read Run Reports in the PCC EHR Report Library.
Optionally Include Service Charges and Non-Service Charges
To see your practice’s service and non-service charges totaled separately, select these columns during customization.
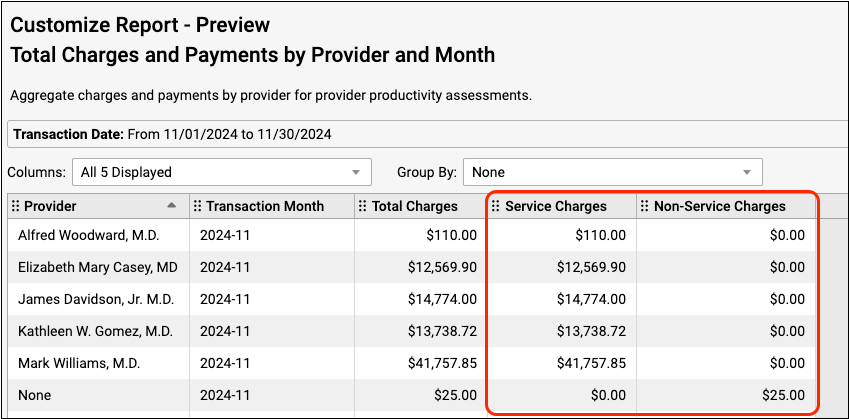
Whether a charge is considered service or non-service depends on the assigned accounting type for the charge’s procedure as defined in your practice’s list of billable procedures. To find out more about configuring accounting types for procedures, read Configure Adjustment Fees and Refunds with an Appropriate Accounting Type.
- Service charges are procedures that have an accounting type of “Revenue”. These are typically clinical procedures, such as office visits, immunizations, and screenings. The Service Charges column does not include credit write offs.
- Non-service charges are procedures that do not have the accounting type of “Revenue”. Some examples are non-clinical service fees, capitation payment offsets, and insurance interest or incentive payment offsets. The Non-Service Charges column does not include credit write offs.
The Total Charges column displays charges with the accounting type of Revenue (which includes Credit Write Off, Service, and Non-Service accounting types). The sum of the Service column’s total and Non-Service column’s total may not equal the Total Charges column total, as the Total Charges column does include credit write offs and the Service and Non-Service columns do not.
Provider None: If a non-service charge, insurance payment reversal, or other line item is not associated with a provider, the Provider column will display “None”.
Interpret Report Results
This report displays a snapshot of all charges and payments within a given payment transaction date range.
Your report output is based on the criteria you selected. The default report criteria present a simple overview of your providers’ productivity by transaction month. Customized reports present a more detailed, and more complex, organization of the data.
Interpret the Default Report
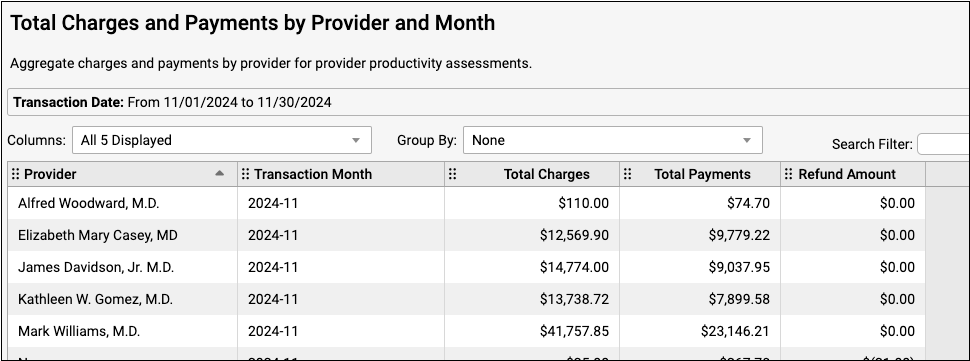
The default report output is sorted by provider and then by transaction month. Total charges and total payments subtotal within each row.
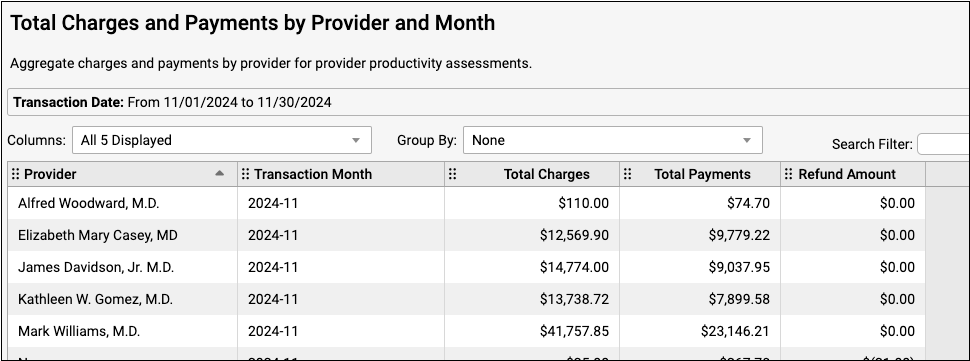
The report output displays all locations by default. If you selected locations while setting criteria on the default report, your selected locations will be the only locations included in the report output. To display chosen locations in a column, create a custom report.
The Transaction Month column displays the months included in your selected transaction date range. See Choose Your Transaction Date Range above for more information on selecting a transaction date range.
The Total Charges column displays charges with the accounting type of Revenue (which includes Credit Write Off, Service, and Non-Service accounting types). You can configure your accounting types in the Procedures table in PCC EHR. To find out more about accounting types, read Configure Adjustment Fees and Refunds with an Appropriate Accounting Type.
The Total Payments column displays total insurance and personal payments with assigned payment class of Insurance, Check, Cash, or Credit card. Adjustments do not display on this report.
The Refund Amount column displays charges with accounting types of Refund, Receipt, or NSF.
Interpret a Custom Report
Custom reports can provide a more detailed view of your data. If you selected location and procedure group during customization, for example, this additional information will display on your report. If you selected many criteria during report customization, the aggregate data will be broken down into even greater detail. Each unique combination of criteria displays on its own row.
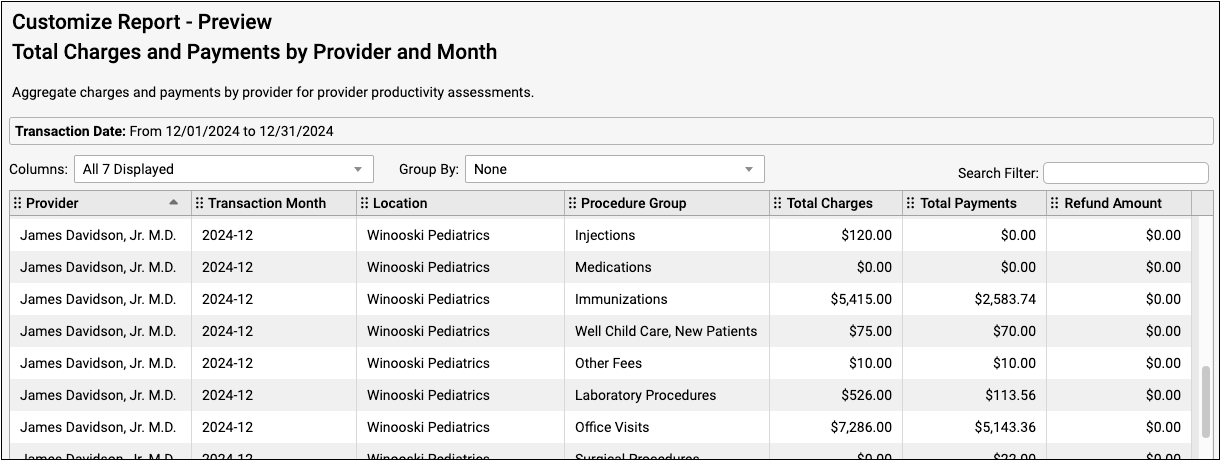
You can group and sort this output to further organize your data. Once you group the report, you can sort further by clicking on a column header. To sub-sort with other columns, hold the “Shift” key and click the column headers for your secondary sort, tertiary sort, and so on.
Interpret the Refund Amount Column
Refunds and reversed insurance payments (also known as “takebacks”) display in the Refund Amount column.
The charges, payments, and refunds displayed on this report are not necessarily associated with each other, except that they share the transaction date range of the report. If a payment and a refund occur within the same selected transaction date range, they will both display on the same report.
The example below shows a charge, a payment, and a refund that were all made on the same day.
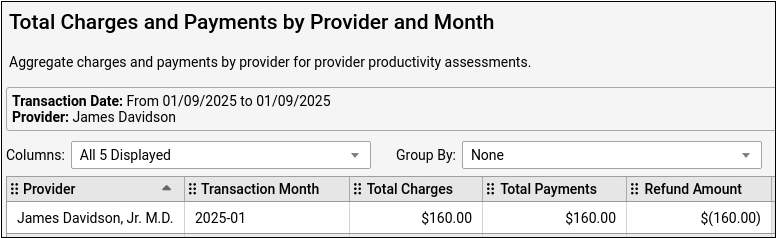
If an insurance payment reversal or other line item is not associated with a provider, the Provider column will display “None”.
