Read EDI Responses to Claim Submissions
After you submit claims, your office receives many different electronic responses. Your PCC system logs submission activity, PCC’s central server sends your system a daily summary, claim clearinghouses and other vendors send back acknowledgment reports, and payers send back rejections and ERAs.
Read the sections below to learn what kinds of responses are sent to your practice, which you should review, and where you can go to research responses when you run into a billing problem.
What is "EDI"?: EDI stands for “Electronic Data Interchange.” When you submit electronic claims or receive any kind of electronic reports, you are using EDI. PCC has several different dedicated teams working on EDI, and you can contact PCC Support with any questions.
Learn All Steps for the Biller Role: This article is part of the New User Training for Billers. You can use that outline to learn how to complete all billing tasks in PCC EHR.
Contents
What EDI Responses Are Sent To Your PCC System?
PCC, claim clearinghouses, ebill vendors, and payors all send your practice various electronic communication.
Electronic personal bills are fairly straightforward: Your PCC system logs what went out on the bills, and the ebill vendor sends back an acknowledgement that bills were received.
Claims, however, result in a series of logged information, responses, and reports:
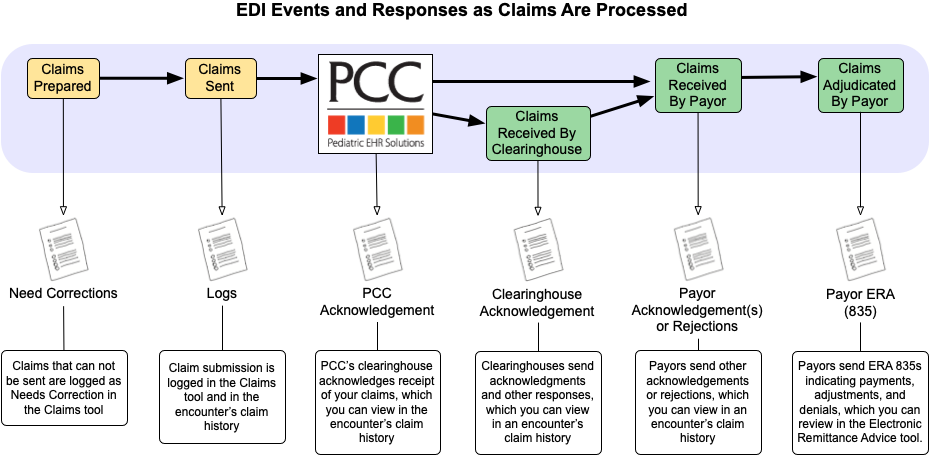
For most of these responses, your PCC system automatically receives the report, parses it, and adds appropriate items to each family’s account history. You don’t need to review the full report file, because the information is recorded for each encounter and (in some cases) for each charge. However, the full report file is archived on your system, should you need it.
Which EDI Responses Should a Practice Review?
Which electronic responses are important to review, and which are just for reference? There are three claim responses in the chart above that your practice will always respond to:
-
Need Corrections: When you process claims, your PCC system spots claim problems that need to be addressed before the claim can go out the door. You can review the “Need Corrections” claims in the PCC EHR Claims tool. Claims that are stuck also appear on the SRS Billing Error Report. Read Work on Claims That Cannot Be Submitted to learn more.
-
Rejections: Claim clearinghouses and payors will sometimes send your practice rejections, which indicate that the payor will not adjudicate the claim. You can find rejected claims in the Insurance Balances tool or review them in the encounter’s Claim History in the Billing History in the chart. Read Work on Claim Rejections to learn more.
-
835s (ERAs): After a claim is adjudicated, payers typically send an 835 ERA file, which explains payments, adjustments, and denials. These ERAs replace a traditional paper EOB. Your practice can automatically post most of these payments, and then manually post any that did not match expectations. Read Post Insurance Payments to learn how to post your ERAs. Later, you can review archived responses in the Electronic Remittance Advice tool.
How Do I Review the Archived Copy of any EDI Response?
As described above, PCC includes tools and reports for addressing claim and billing problems as part of your daily workflow. You can also read EDI responses for any encounter.
-
Claim History: You can review original acknowledgements and other responses using the Claim History for any encounter. The Claim History is available on the Posting Exceptions detail view, but you can find it at any time for any encounter in the Billing History section of the patient’s chart.
-
All ERAs: As described above, you can read the full ERA in the Electronic Remittance Advice tool.
-
System Archive: If you don’t know the patient, check number, or payor you can also read archived EDI communication that arrives on your PCC system in the under-the-hood EDI Reports (ecsreports) program. In addition to claim responses, the archive includes acknowledgements from your third-party bill printing service, batch reports for a day’s submission, and copies of other archived output from electronic transactions.
