Bill for Phone Encounters and Portal Messages
Your practice can bill for phone calls and portal messages.
Read the procedure below to learn how to chart and bill for a phone encounter (or portal message thread). Next, you can review the other sections below to learn about configuration and tips for turning phone calls and portal messages into billable telemedicine encounters.
Watch a Video: You can watch an example of how a practice charts and bills for a phone call (or portal message): Bill for Phone Encounters and Portal Messages.
Schedule a Telemedicine Encounter Instead: The article below talks about documenting a phone note or portal thread so you can bill for it. However, PCC recommends that you schedule, chart, and bill a telemedicine appointment instead.
Contents
Chart a Phone Note and Then Bill For It
Read the procedure below to learn how your practice can treat every call as though it may be billable, and then how to bill for it.
Follow This Procedure for a Portal Message As Well: The procedure below shows billing for a phone call. Portal Messages follow the same workflow and use the same set of tools.
Create a Phone Note
When your practice takes a call or receives a message, you record information on a new phone note.
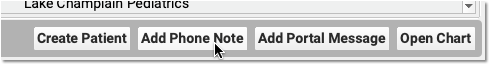
You can click “Add Phone Note” from the PCC EHR search results or from inside a patient’s chart. A triage nurse or front desk might take the initial call, create the phone note, and then assign it to a clinician to make a followup call.
Billable Phone Encounters Must Be Initiated by the Patient or Parent: If your practice makes the initial call to schedule or begin a phone encounter, that phone or portal message encounter can not typically be billed.
Document the Phone Encounter on the Phone Note
Next, a clinician at your practice documents the phone encounter with enough detail to cover telemedicine requirements.
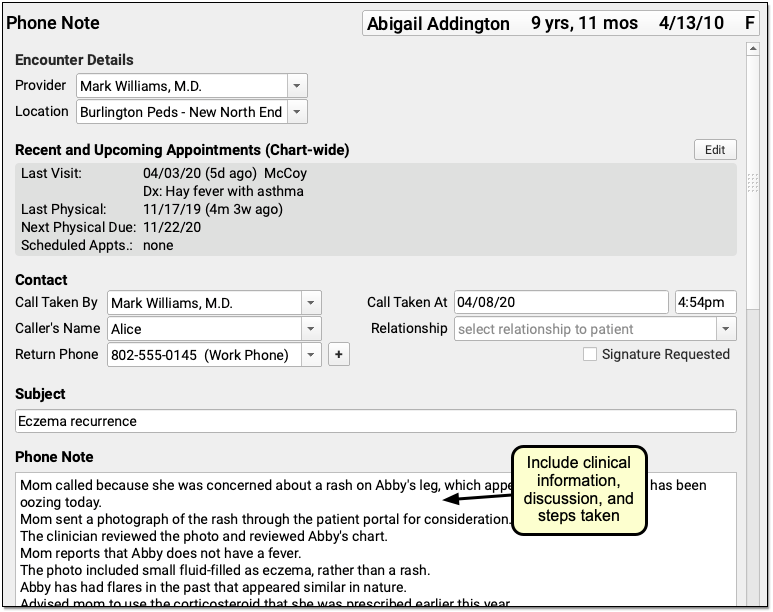
For example, use the Subject field to reflect the main topic of the encounter. Include enough clinical information in the phone note to make a diagnosis. Make note of all questions asked during the call, and all clinical information given. Include any reassurances offered. Include all topics covered during the conversation.
Record the Duration of the Call
Record the duration of the call, in minutes, on the phone note.
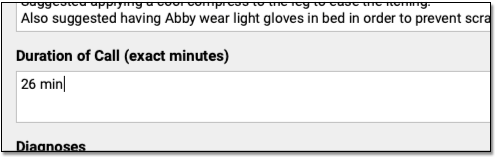
By entering the exact duration, you chart an important element of the encounter. The duration is used to support the encounter’s billing code(s).
How Do I Code the Duration of a Phone Call?: For help understanding how duration affects the coding level for a phone encounter, check out PCC’s Telemedicine Billing Code Time Table
Select Diagnoses
Chart one or more diagnoses on the phone note. Optionally, you can simultaneously add a diagnosis to the patient’s chart-wide Problem List.
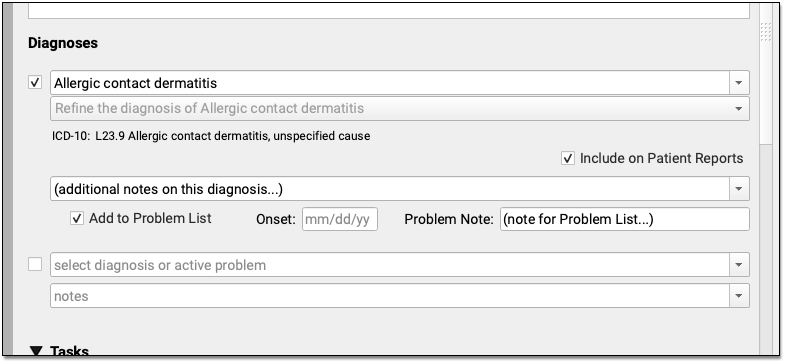
When you select a diagnosis description, PCC EHR automatically adds an appropriate ICD-10 code to the phone note’s Electronic Encounter Form.
Optional: Order Labs, Referrals, Procedures, and Other Orders
During the course of the call (or later when charting), you can create orders. Your practice can add orders components directly to the phone note protocol and make common orders available from a single click.
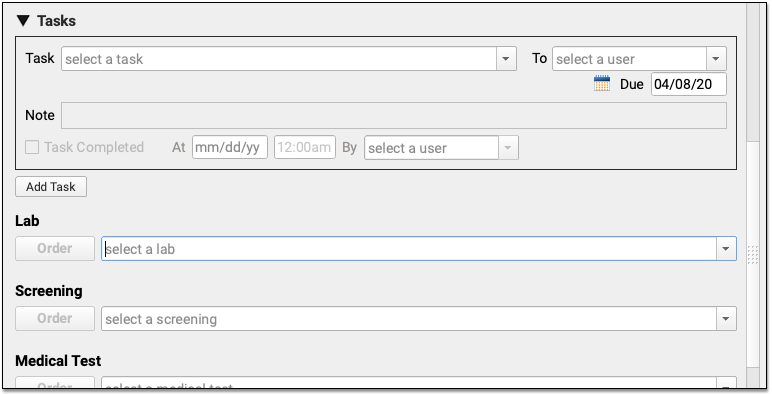
Can I Bill This Order From a Phone Encounter?: Orders that you create during a phone or portal message are not always billable. When you click “Order”, PCC EHR can automatically add appropriate diagnoses and procedures to your electronic encounter form, and your biller will need to be aware of limitations and make changes when they post charges.
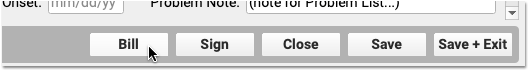
Click “Bill” and Select a Visit Code
Next, click “Bill” to review and select codes on the Electronic Encounter Form.
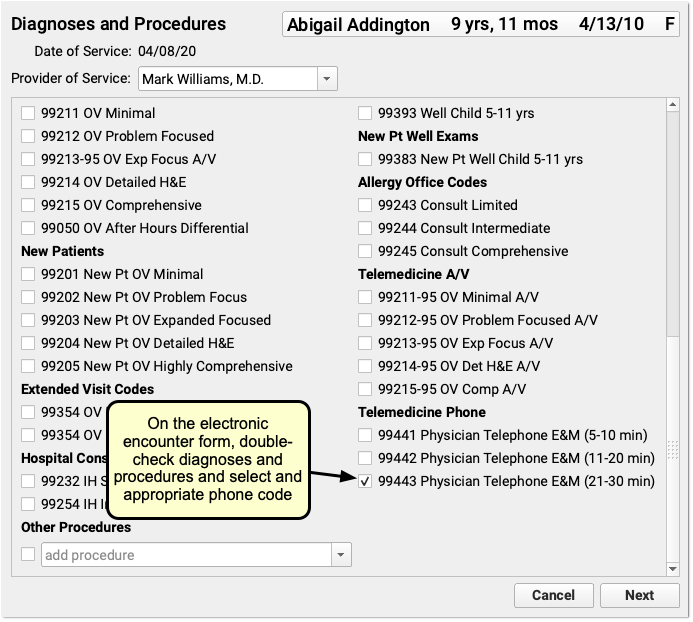
The Electronic Encounter Form displays all diagnoses and procedure codes from items the clinician selected on the phone note. They will typically select a visit code manually.
Your practice can configure what encounter codes appear on the Bill window. For example, for a telemedicine visit you might select a -95 code for a live audio and video E&M visit. For a phone-only visit, you might use time based codes 99441-99443. PCC does not recommend specific codes, you should check your CPT manual and consult with your payors for billing requirements.
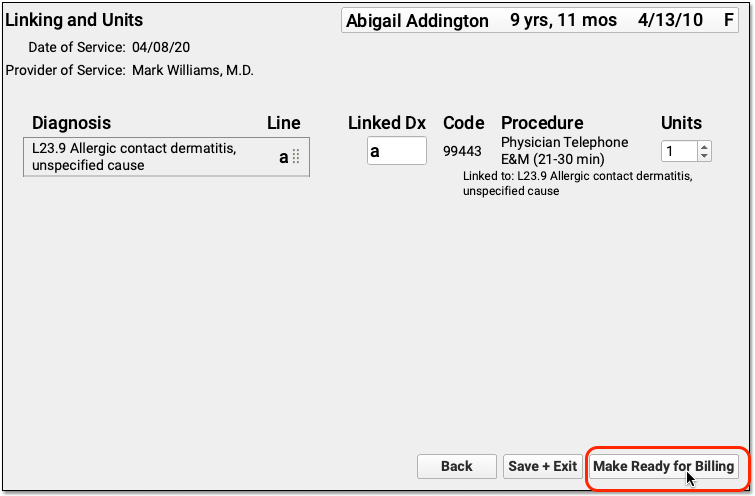
Update Units and Diagnosis Linking and Make the Visit Ready for Billing
After you review and add codes, you can review units and which diagnosis is linked to each procedure. Next, make the visit ready for billing.
Sign the Encounter
Complete your notes and click “Sign” to sign the phone note, just as you would for other encounters.

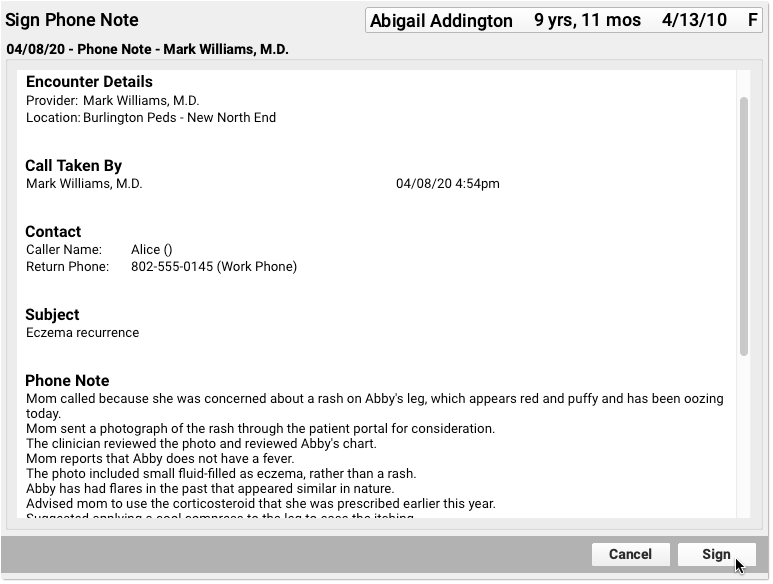
PCC EHR supports cosigning providers if needed.
Monitor the Messaging Queue for Billable Messages
A biller at your practice can check the Messaging queue to find phone and portal messages that may be billable.
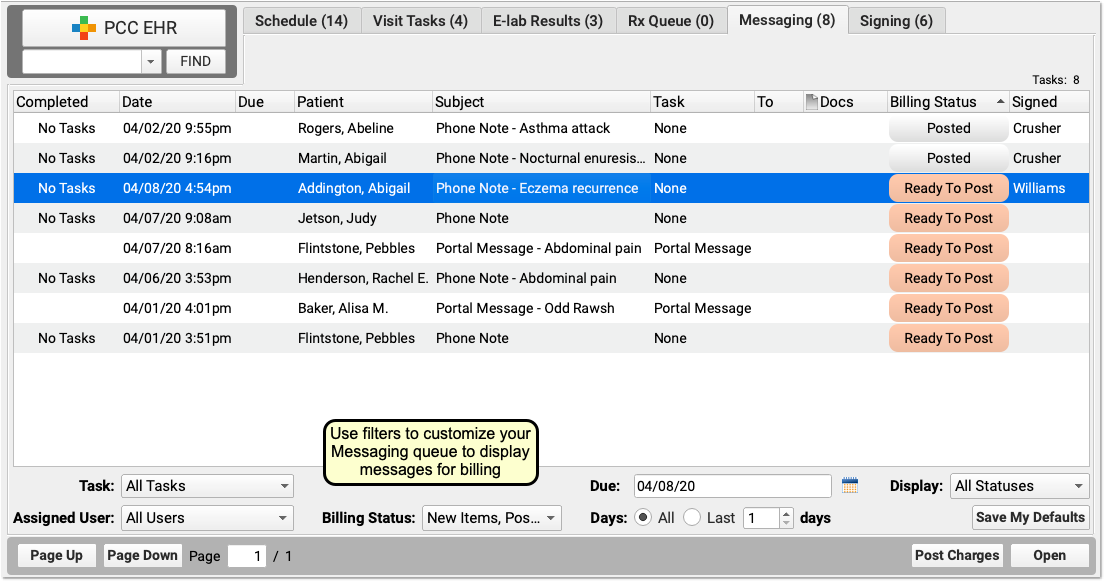
Sort the Messaging queue and use filters to limit the list to appropriate items for the biller to review.
For example, a biller can use the Billing Status filter to limit the list of messages to phone notes and portal messages that are “Ready to Post”, “Posted” and that may have “New Items” to post.
The 'Due' Filter Can Hide Messages: Practices can use due dates on tasks to hide a message until it becomes due–for example, to schedule a call back or a followup about test results. If you use the “Due” filter on the Messaging queue, be aware you could hide message encounters that are ready to bill today.
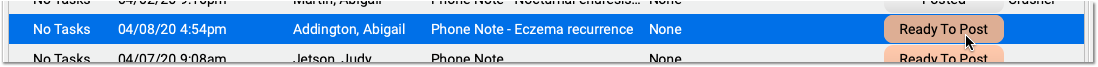
Click “Ready to Post” to Open a Message Encounter
When you are ready to review an encounter and post charges, click “Ready To Post”.
Assess Whether an Encounter is Related to Another Appointment
Use the patient’s Visit History, Encounter Details, and other chart sections to find out if the encounter is billable.
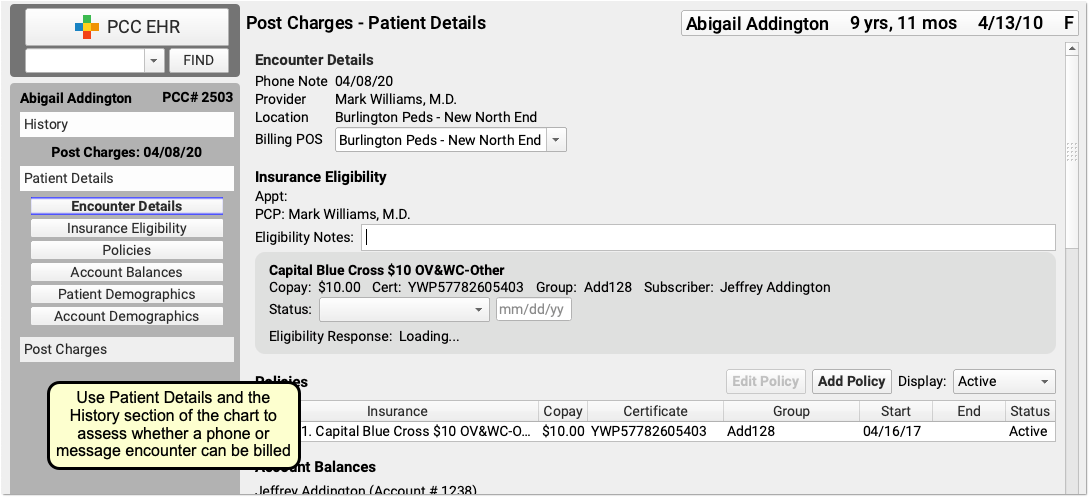
For example, a phone call might be a followup for a previous E&M visit within 7 days prior, or the call may have resulted in a visit the following day. Whether or not you can bill for an encounter depends upon specific rules for each visit code.
If the patient has an in-office E&M (for example) near the time of the call, you can open the chart note and check the reason. If the visit reason was not related to the phone call, then both that visit and the phone call may be billable.
For precise guidance on the restrictions for each billing code, check your CPT manual. In general, if a phone call is within 7 days of an E&M visit for a related reason, you may not bill the call and should instead incorporate the work performed into the claim for the in-office E&M visit.
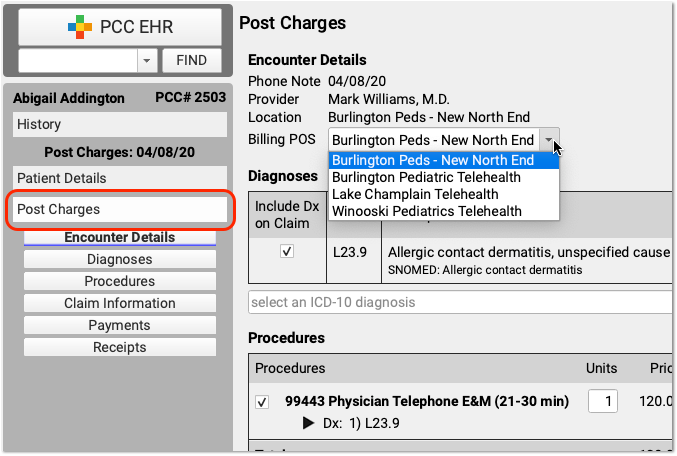
Update the Billing Place of Service
If your payer requires a specific telemedicine place of service, you can change it along with other details in the Post Charges protocol.
Update Diagnoses, Procedures, Claim Information, and Payments
Next, the biller can make any required adjustments to diagnoses, procedures, claim information, or payments.
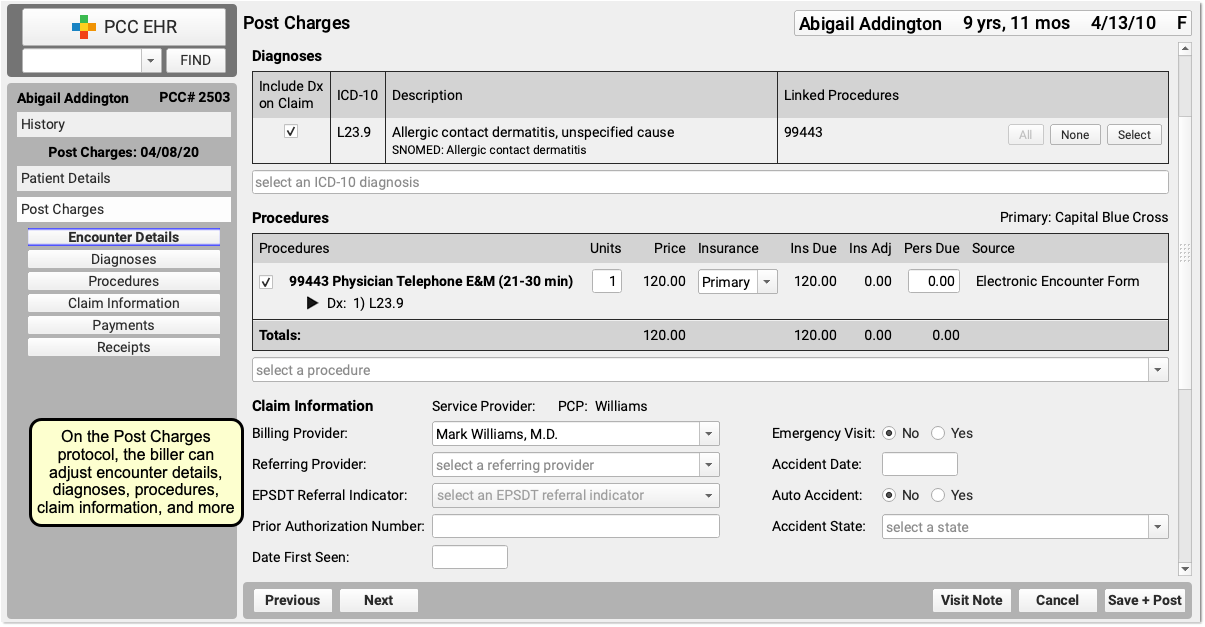
Billing for telemedicine is a rapidly evolving issue. PCC hosts web labs and a COVID-19 Coding Guide which we update regularly.
Click “Save + Post” to Queue Up a Claim
Finally, the biller clicks “Save + Post” to post the charges and queue up a claim.
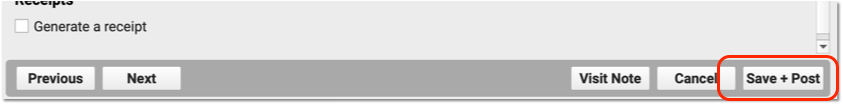
Later, the biller can come back to Post Charges if they need to add additional items.
Configure PCC EHR for Phone Note Billing
In order to get paid for telemedicine services provided over the phone, you may need to adjust how you chart phone notes. Review the items below to learn more.
Revise the Phone Note Protocol
If you are not already tracking call duration within your phone notes, you can add it to your existing Phone Note Protocol. You can also add the Diagonses component, orders components, and any other component your practice would use for a phone encounter.
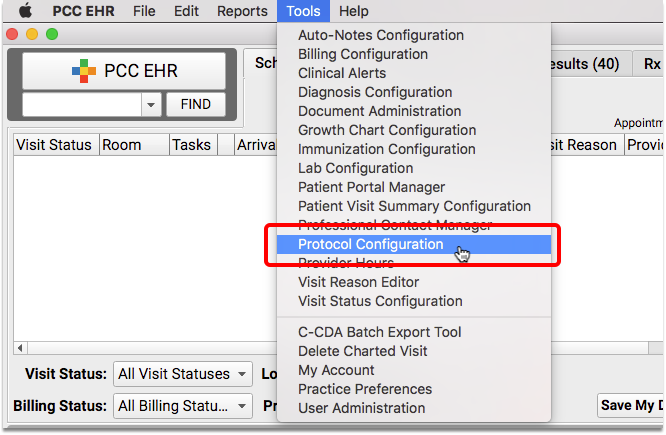
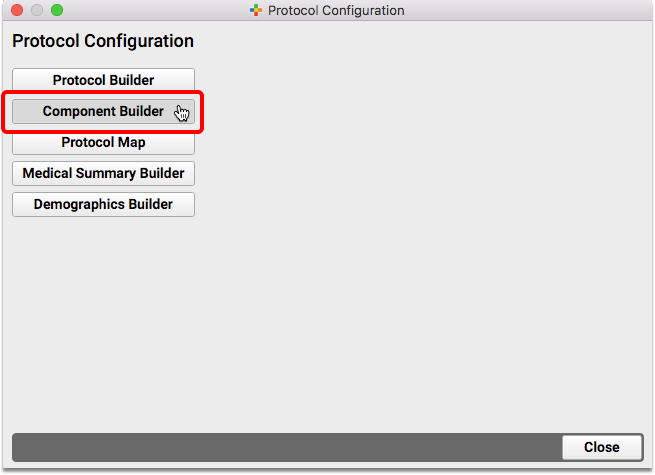
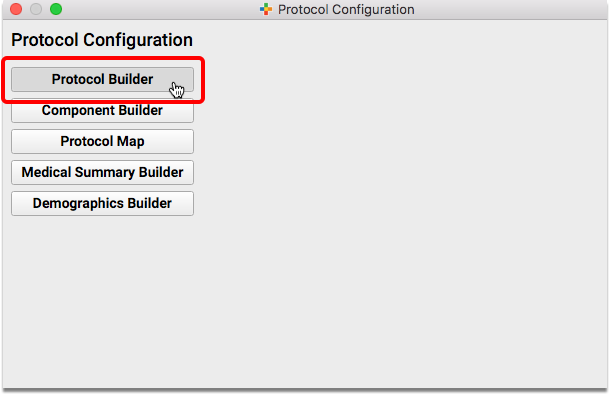
Open the Component Builder
Navigate to the Protocol Configuration tool and select the Component Builder.
Create a Duration Component
Add a new custom entry field for “Duration of Call (exact minutes)” to your Component Builder.
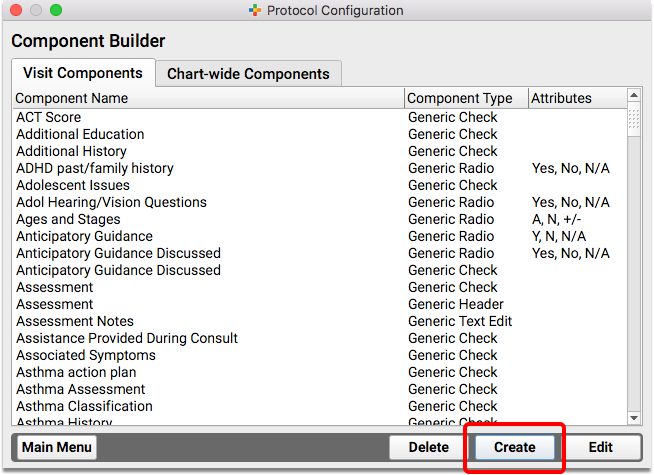
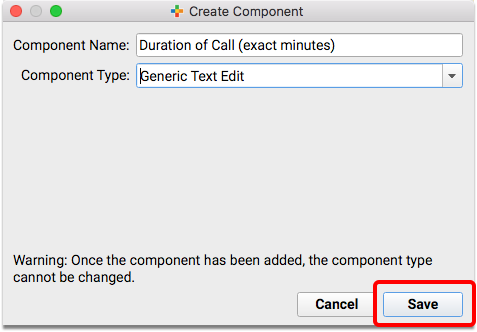
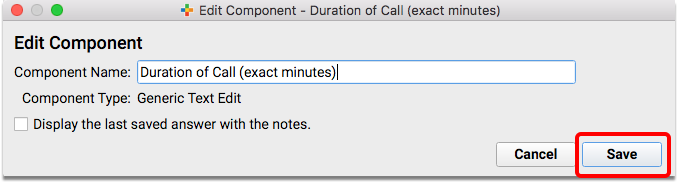
Duration vs Start/Stop: If you prefer, create two fields to track the Start Time and Stop Time of the call, rather than one Duration field. You just need a way to track the total minutes spent on the call.
Edit the Phone Note Protocol
Return to the Protocol Configuration and open the Protocol Builder to edit your existing Phone Note Protocol.
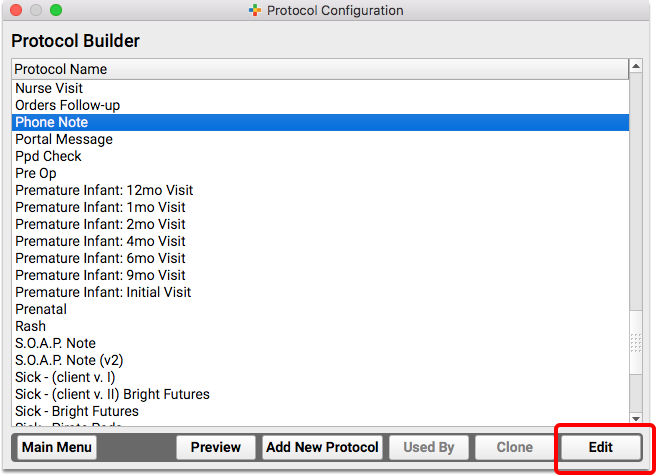
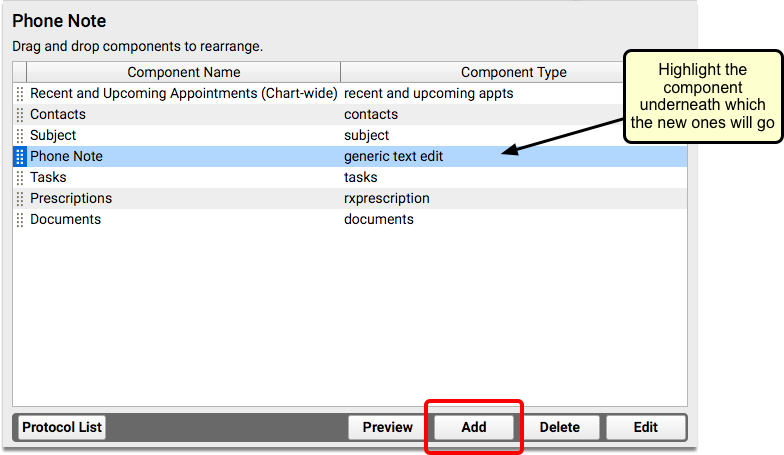
Add Components to the Phone Note Protocol
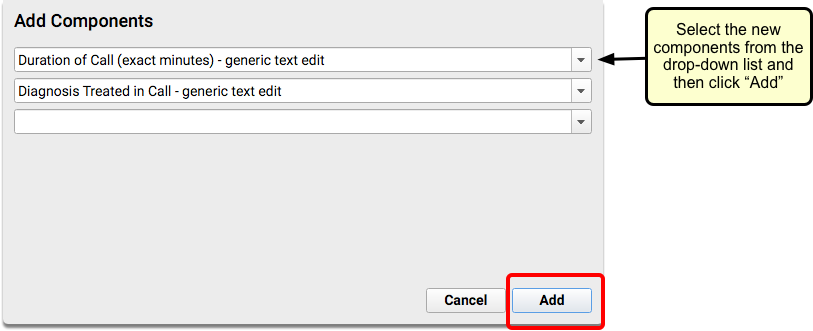
Review the components on your practice’s Phone Note and/or Portal Message protocol. Consider adding your new duration component, the Diagnoses component, and any other component that will help you chart on the phone note or portal message.
Create a Telemedicine Procedure Group and Add Telemedicine Procedures
To learn how to set up procedures, codes, and prices on your PCC system, read Configure PCC EHR for Telemedicine Encounters.
For more help in setting up new procedures, contact PCC Support.
Will Payers Pay for Phone Calls and Portal Message Encounters?
When you care for patients and families over the phone or a portal message, you provide a valuable service. PCC recommends that you treat every phone note as though it could be a billable service, unless it is for scheduling or clearly related to another appointment.
PCC has heard from pediatric practices that the smart move is to submit claims for telephone services to all of your insurance carriers–even if you know they won’t pay. The industry is changing, and the COVID-19 pandemic changed the landscape for telemedicine payment.
As always, check with your insurance providers to review their policies and requirements.