The Claim Journey Explained
How is a claim created, and what happens in the background to make sure your practice is paid? Read below to learn some of the “under the hood” workings of claims with PCC.
Your Practice Posts Charges for Each Encounter, Creating a Claim Tag
First, a clinician sees a patient. They create orders and enter diagnoses on the chart note, and they also add billing details and select visit codes on the Bill screen in PCC EHR. (learn more)
Next, either the front desk or a biller reviews those diagnoses and procedures and posts them as charges. PCC queues up those charges and creates a claim tag, an under-the-hood entry which contains a collection of charges that are ready to be turned into a claim. (learn more)
Your practice creates claim tags in other ways, too. When you fix a problem with a charge, such as changing the responsible party, you also generate a new claim, which creates a new claim tag. As another example, a new claim tag is created automatically when you post payments and adjustments and the remaining balance pends the next responsible party.
Your Practice Prepares and Submits Claims, Which PCC Sends to Clearinghouses and Payers
Next, your practice uses the Claims tool in PCC EHR to transform claim tags into outgoing claims. (learn more)
Your PCC system sorts the tags, checks for errors, filters out claims that should be delayed or held, routes certain claims to be printed on paper (when needed, learn more), provides you with a list of stuck claims that need corrections before they can be sent out (learn more) and then sends electronic claims to PCC for routing.
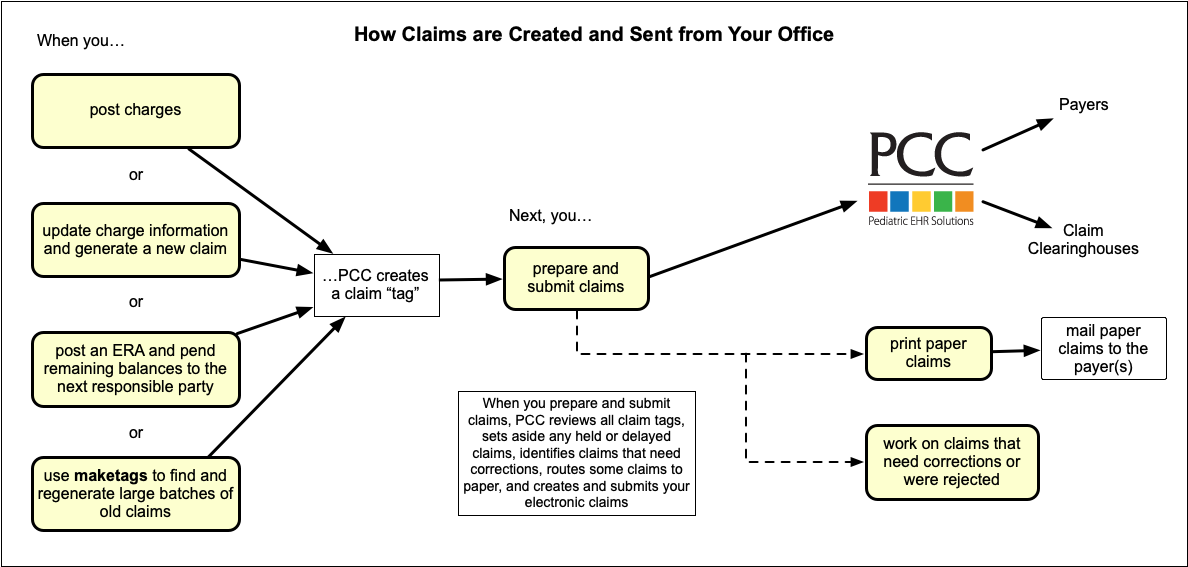
Claims travel through additional verification on PCC’s servers. Then we route them either directly to the payer or to a claim processing clearinghouse, which then directs the claim to the payer.
Usually, the clearinghouse and payer acknowledge receipt of the claim, which your practice can see in the encounter’s claim history (learn more).
Next, the payer adjudicates the claim. They send payment and adjustment details back through PCC and into your system as an ERA (electronic remittance advice). You can post most ERAs automatically and enter any denials or unusual responses manually. (learn more).
During the above steps, your PCC system logs errors, acknowledgements, rejections, and other reports sent by claim clearinghouses and payers. Your practice’s billers review those logs and other “EDI responses” (learn more).
Finally, billers use PCC tools to respond to rejected claims (learn more). If the payer never responds to a claim or an appeal, or an encounter was not billed correctly, billers can track the entire insurance A/R and create custom worklists of all unpaid encounters with insurance balances. (learn more).
For more information, or for help understanding how claims are created or why a claim can be rejected, contact PCC Support at 802-846-8177 or 800-722-7708. PCC also hosts free interactive drop-in sessions where you can ask billing, coding, and practice management questions.
PCC's Pre-Submission Claim Error Scrubbing: When you process claims, PCC “scrubs” them, checking for common errors that would prevent the claim from being accepted and paid. Your system stops those claims and lets you correct the problems before they are sent. Check out the Claim Error Reference to learn what claim details are verified on claims during processing.
Under-the-Hood Vocabulary: When you speak with PCC’s EDI teams, you may hear references to tags (which are queued up claims on your PCC system), and the underlying tools that manage tags, interface with your practice’s custom needs, and turn tags into claims (preptags, tagsplit, splitconfig, and consorttags). If you want to know the true nerdy side of what these words mean: when you process claims, PCC’s preptags program calls the tagsplit program according to your practice’s settings. The tagsplit program processes queued-up claims (“tags”) and sorts them by insurance batch while doing a number of other validation checks, all of which refers back to your practice’s custom splitconfig configuration. The preptags program automatically runs the ECS program, which is the underlying software which sends your claims out the door through a secure internet connection to PCC.
