Review Electronic Claim Responses in oops
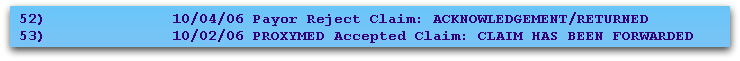
When Partner receives an electronic claim response from the insurance payor or the claim clearinghouse, a one-line message is added to oops. Here are two examples:
If the claims were sent through the Copario (MedAvant, ProxyMed) or Emdeon claim clearinghouses, you can review a more detailed response report from within the oops program. Press [fkey title=’F3′ subtitle=’See Claim Rpt/Bill’ display=’inline’ /] and then select any billing response item that begins with “Payor Response” or that indicates a rejection or acceptance.
Example 1
In the example below, you can see that the electronic claim clearinghouse (ProxyMed) sent several messages to Partner regarding William Amis’s visit on 01/06/06.
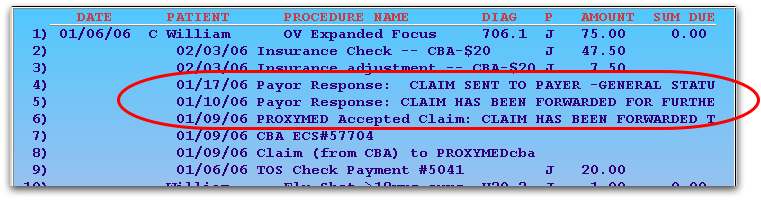
To read the full electronic report, press [fkey title=’F3′ subtitle=’SeeClaim Rpt/Bill’ display=’inline’ /] and then select any entry beginning with “Payor Response” or “PROXYMED Accepted Claim”:
Partner will open the relevant ECS report and display portions related to this patient that are on that report:
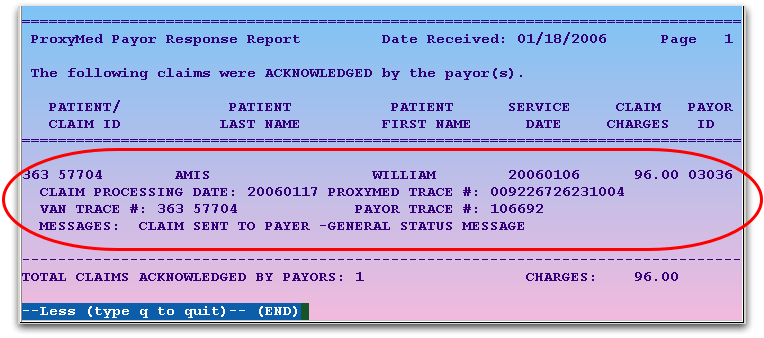
In the above example, the claim was accepted.
Example 2
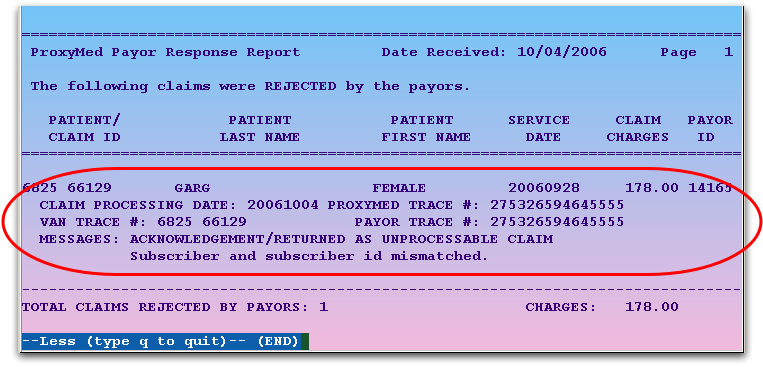
You can also review information about a rejected charge. In the next example, Female Baby Garg’s immunization administration charge was rejected by the MVP insurance company:
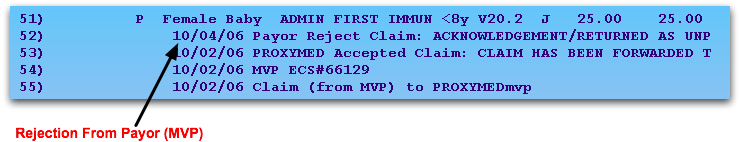
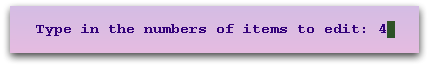
To find out why the claim was rejected, press [fkey title=’F3′ subtitle=’See Claim Rpt/Bill’ display=’inline’ /], enter the number next to the rejection, and press Enter:
Partner will display the segment of the report related to the patient, and you can read all the information that the insurance company (or claim processor) returned:
Using this feature, you can read your ECS reports from within the oops program. You can also read ECS reports in your e-mail or through the ecsreports program.
