Check Patient Insurance Eligibility
PCC automatically checks insurance eligibility for all upcoming appointments. You can also review a patient’s eligibility as you schedule, during Patient Check-In, or at any time.
Do You Trust Automated Electronic Eligibility in PCC EHR, or Do You Have to Visit a Payer's Web Site?: PCC wants automated eligibility to be 100% reliable, the perfect tool to give billers a heads-up about upcoming encounters. If you encounter an eligibility status in PCC EHR that doesn’t match a patient’s status on a payer’s web site, please notify PCC Support at 802-846-8177 or 800-722-7708 or support@pcc.com. Let us know so we can track down and correct the issue.
Contents
Insurance Eligibility Highlights
Here are some important notes about verifying eligibility in PCC:
-
Not All Carriers: Not all insurance carriers support electronic eligibility, and different payers support it to varying degrees. PCC keeps track of your carriers and will configure your practice for all that are available. To request help setting up an EDI connection with a payor, contact PCC Support.
-
Automatic Real-Time and Nightly Eligibility Reports: PCC checks eligibility as soon as a patient is scheduled or whenever you change demographic information or update an active insurance policy for a patient with an appointment. If you schedule a sick visit today or change appointment information, PCC will immediately check eligibility.
-
Check Manually at Any Time: You can also request an instant eligibility update at any time. If you haven’t scheduled an appointment, PCC will request eligibility for today’s date. If you’re working in the context of an appointment, you can recheck eligibility during Patient Check-In or in the Insurance Eligibility tool. (Note that if an insurance company does not support instant eligibility requests, PCC displays a batch request result, usually answered from the previous evening.)
-
Who Will Check Eligibility?: Your practice can confirm eligibility a day or two early, and/or your front-desk staff can recheck eligibility at checkin. You can work with your New Client Implementation specialist or PCC Support to figure out the best eligibility workflow for your practice.
Review Eligibility for Upcoming Appointments
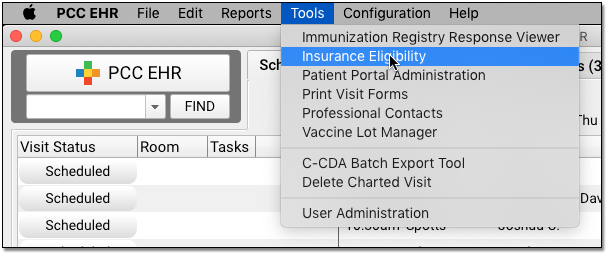
Use the Insurance Eligibility tool to review and confirm eligibility for upcoming patient encounters. You can find it in the Tools menu.
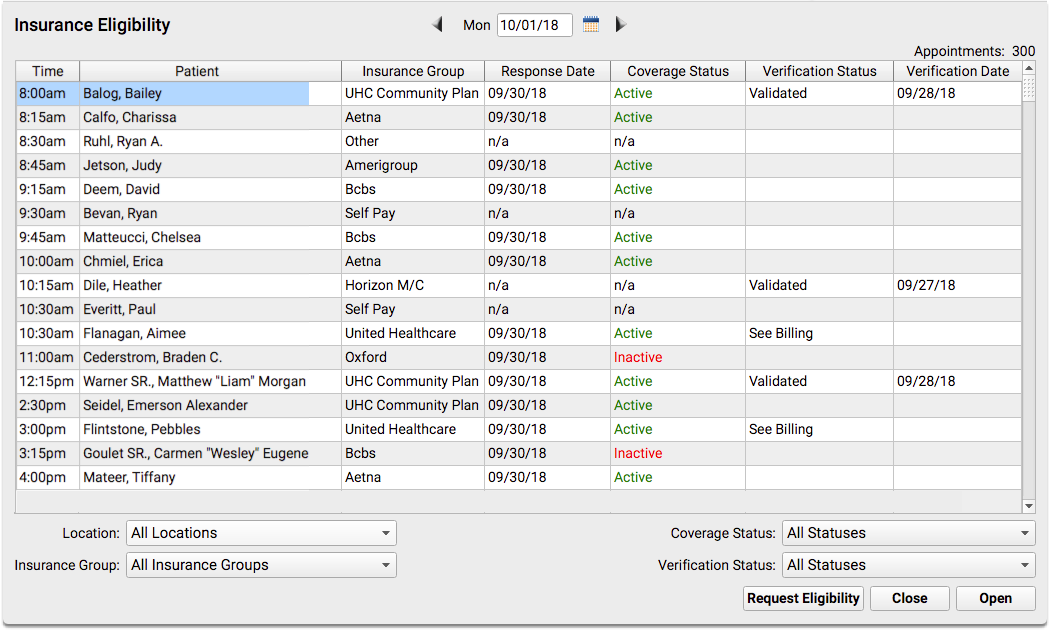
The Insurance Eligibility appointment list shows all scheduled appointments for the next day, but you can select any date.
You can see if a patient is active or inactive in the Coverage Status column. You will see an “n/a” if eligibility is not available electronically for an insurance carrier or if the patient is not insured (self-pay). “Unknown” means that an error occurred when eligibility was last checked, or the payer returned an uncertain reply. If the field is blank, eligibility has not yet been checked.
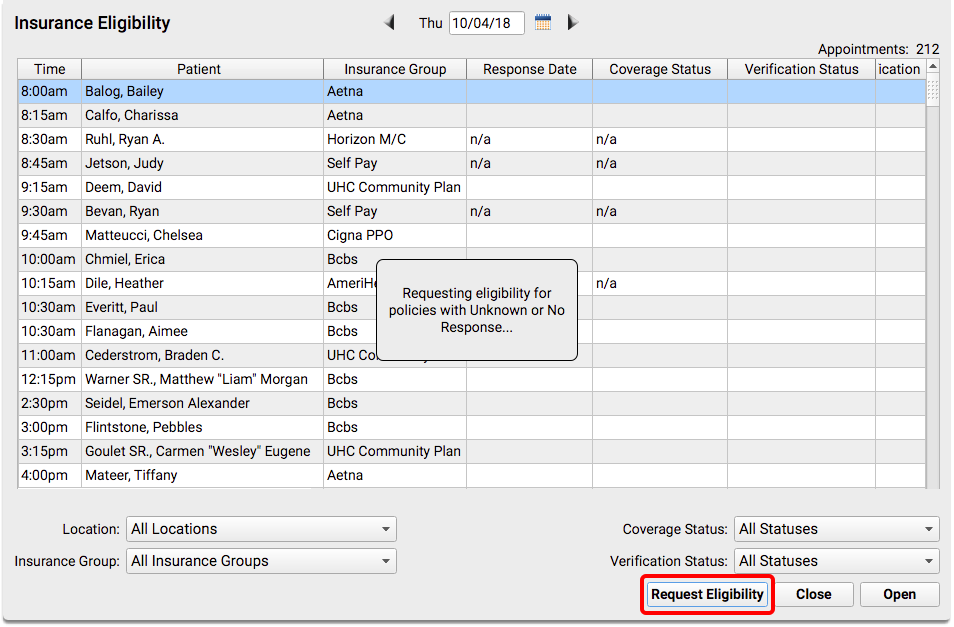
Click “Request Eligibility” to request an eligibility update for all visits that either have not yet had eligibility checked, or that received an error when the request was previously made.
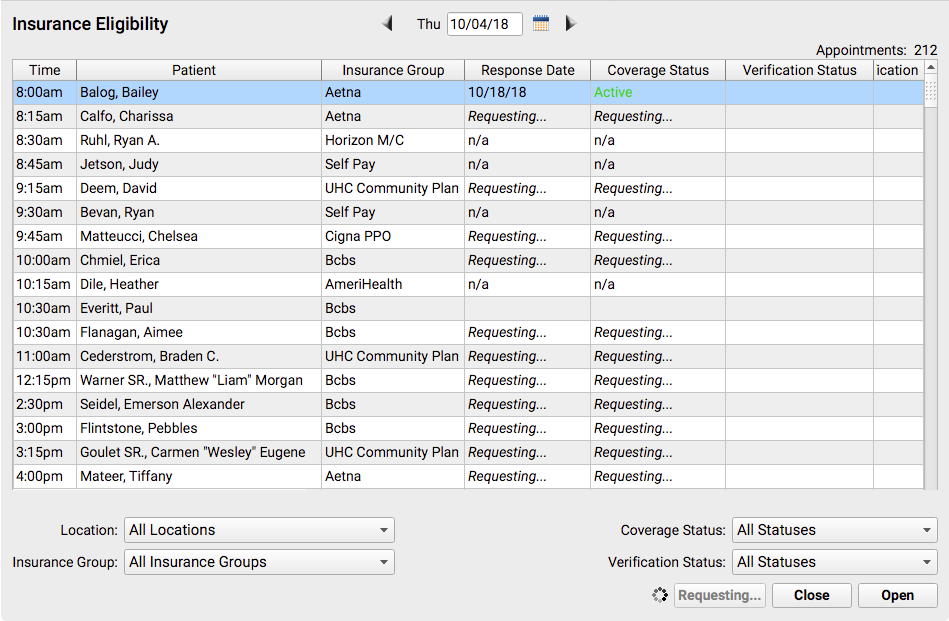
After responses arrive, you can work with individual records. Double-click on an encounter to open the Review and Verify window.
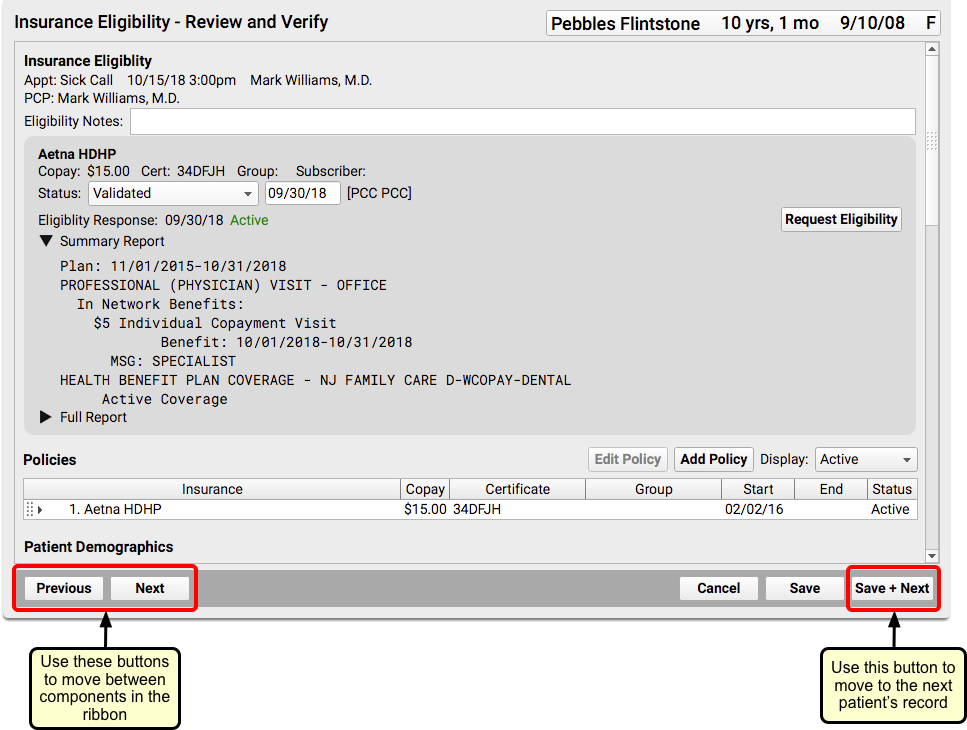
On the Review and Verify window, you can review information sent back from the insurance payor along with general information about the patient’s policy and demographics.
Select a “Status” to mark the encounter’s eligibility status as reviewed. Enter a note if needed. Then click the “Save + Next” button to move to the next patient.
Read the Understand Eligibility Responses, Errors, and Reports section below to learn how to read the payer’s response and any eligibility errors you may encounter.
Configure Your Custom Review and Verify Ribbon: The Insurance Eligibility – Review and Verify window includes the Insurance Eligibility component, Policies, and other useful components. You can add other components to this ribbon in the Insurance Eligibility Builder within the Protocol Configuration tool.
Where Else Can My Practice Confirm Eligibility?
In addition to using the Insurance Eligibility tool (which shows each day’s encounters) your front desk staff, clinicians, and billers can review patient insurance eligibility at other times.
Check Insurance Eligibility Without an Appointment
You can check a patient’s insurance eligibility before you schedule using the Insurance Eligibility component. When you are scheduling an appointment, for example, you can use the component in the Patient Details ribbon.
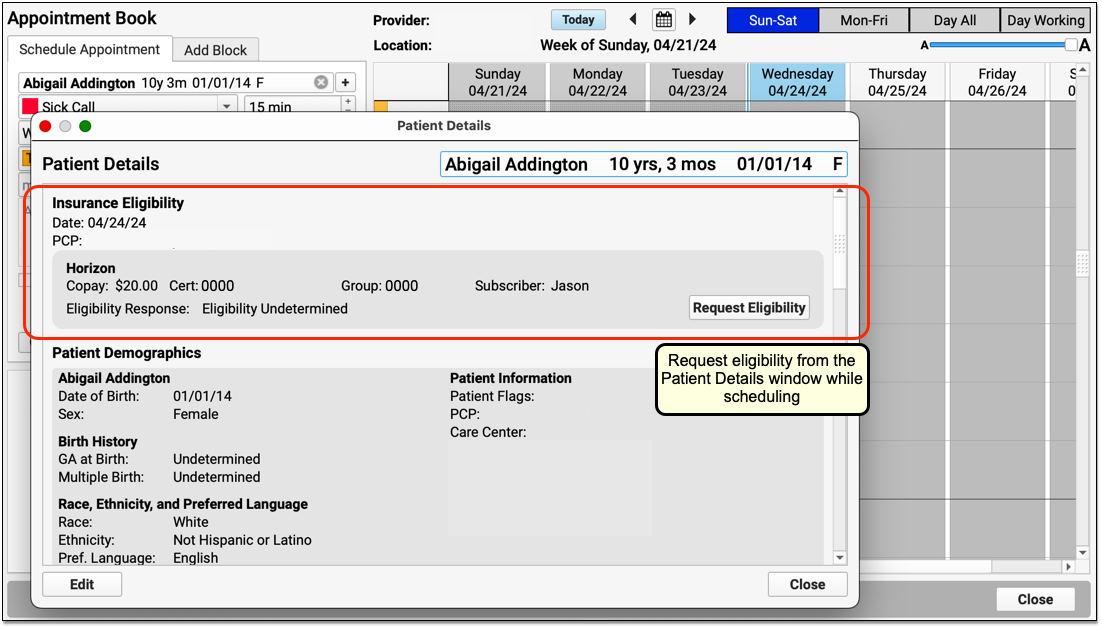
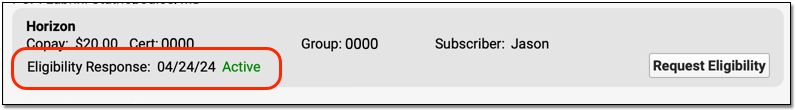
When you click “Request Eligibility”, PCC will contact the payor and retrieve any available eligibility responses using today’s date as the date for the encounter. If the payor responds, PCC EHR will display the “Active” or “Inactive” result.

If you wish to review the complete eligibility report from the payor, click “Edit”.

Eligibility For Future Appointments: When you request eligibility without a scheduled appointment, the payor returns eligibility information for today’s date. The patient may not be eligible for future appointments.
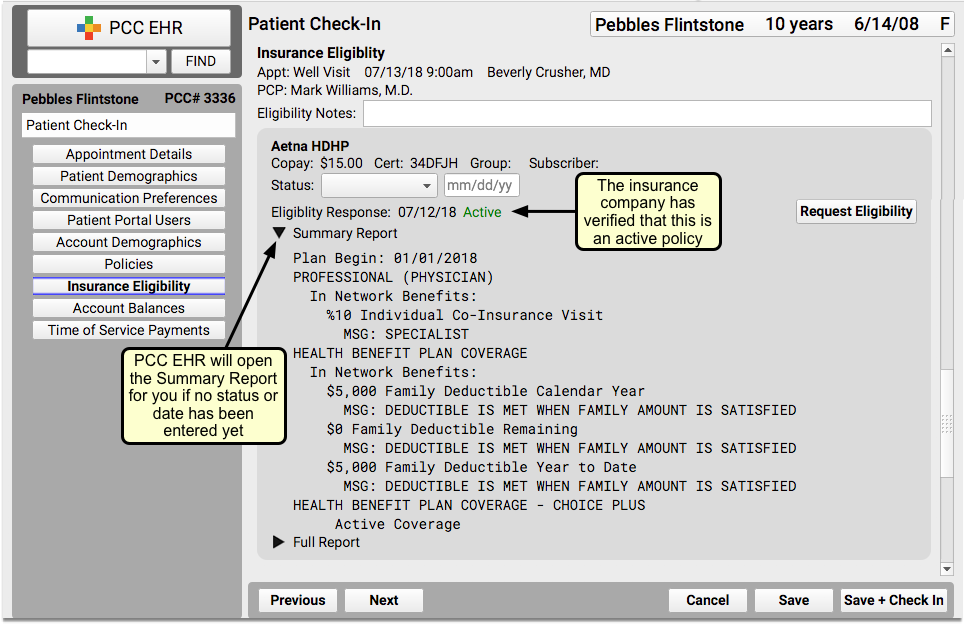
Confirm Eligibility During Patient Check-In
Your front desk staff can verify eligibility when a patient checks in. By default, an Insurance Eligibility component appears on the Patient Check-In ribbon.
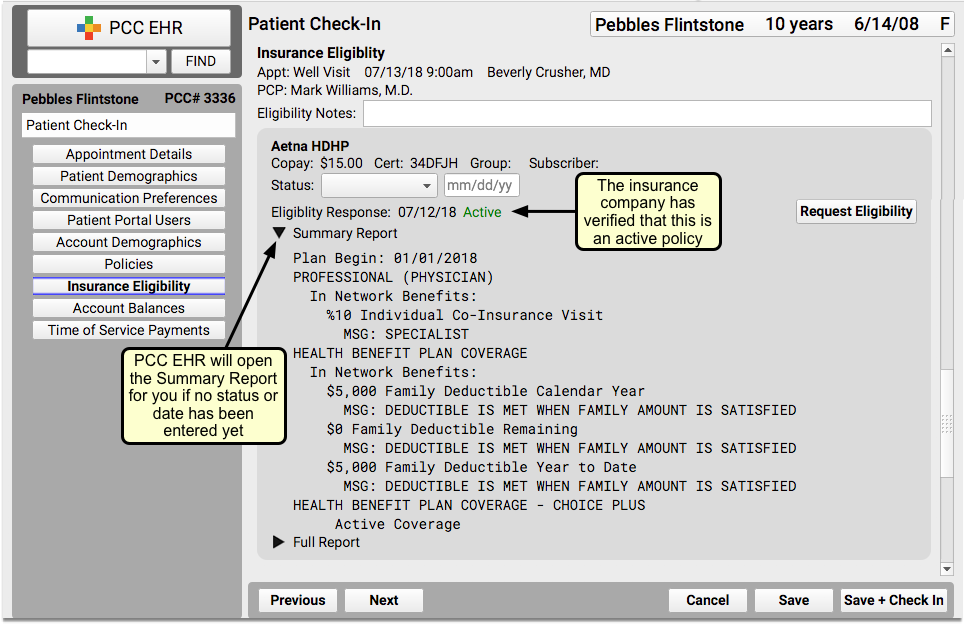
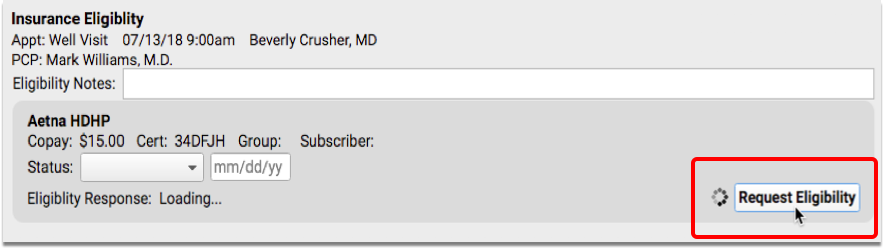
When you first open Patient Check-In, PCC EHR will automatically check eligibility. If your front desk adds a new policy to a patient, PCC EHR will check eligibility automatically. You can also click “Request Eligibility” to manually refresh eligibility (for example, if you changed the Date of Birth or other information about the policy or patient).
Read the Understand Eligibility Responses, Errors, and Reports section below to learn how to read the payer’s response and any eligibility errors you may encounter.
Check Eligibility While Charting
Your practice can add the Insurance Eligibility component to chart note protocols. Then a clinician can review eligibility during the context of working with the patient during an encounter.
When the chart note is opened, Insurance Eligibility is displayed in view mode. You can make changes by clicking the “Edit” button.
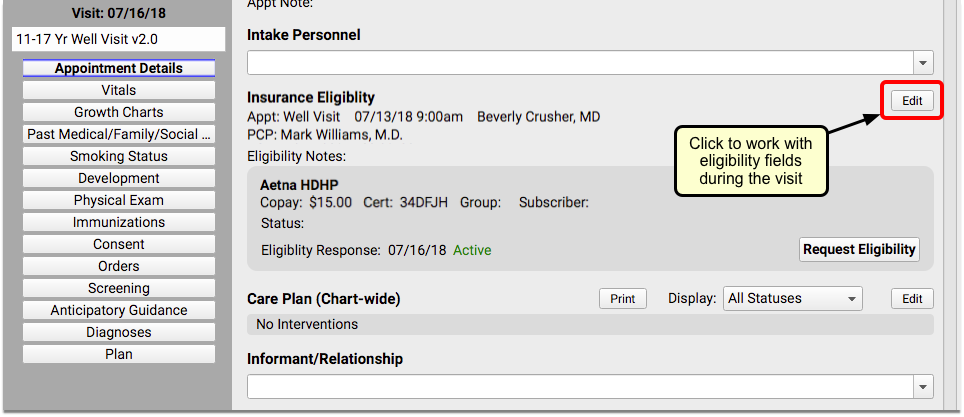
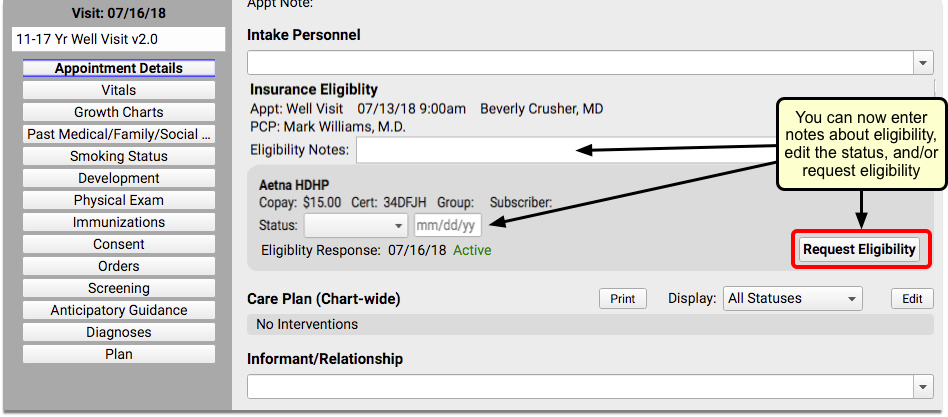
Read the Understand Eligibility Responses, Errors, and Reports section below to learn how to read the payer’s response and any eligibility errors you may encounter.
Check Insurance Eligibility While Posting Charges
When the biller posts charges for an encounter, they can review and update a patient’s insurance eligibility on the Patient Details section of Post Charges in PCC EHR.
Billers can check insurance eligibility for scheduled appointments, as well as billed phone note and portal message encounters.
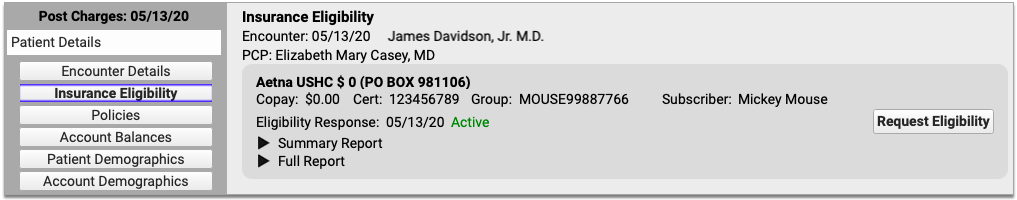
Post Charges is the only place where it is possible to verify insurance eligibility information for billed phone note and portal message encounters. It is not possible to record eligibility notes or verification statuses for phone note and portal message encounters.
Read the Understand Eligibility Responses, Errors, and Reports section below to learn how to read the payer’s response and any eligibility errors you may encounter.
Select an Eligibility Status
Whenever you review the eligibility information for a patient’s encounter, you can optionally select a Status and enter a date.
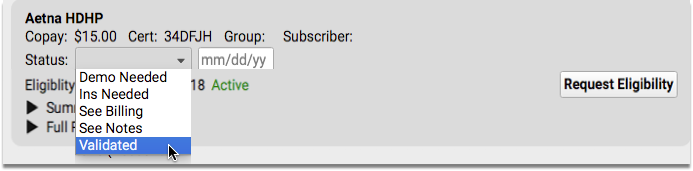
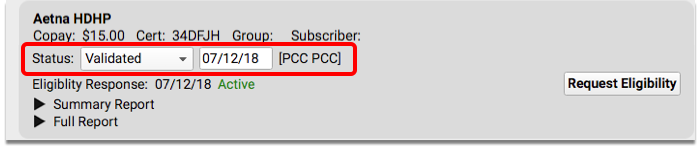
This “Verification Status” is a useful note to your practice that you’ve reviewed eligibility for the encounter. It will appear wherever your practice sees eligibility information for the encounter. It also appears in the “Verification Status” column in the main Insurance Configuration tool in PCC EHR.
Resubmit After Making Changes
If you update a patient’s insurance information or other demographic information, click “Request Eligibility” to submit a new request to the insurance carrier. The request will run in the background, so you can continue to work on the screen while the eligibility request is processing.
Understand Eligibility Responses, Errors, and Reports
You can use the information and tools inside the Insurance Eligibility component to review the response from the insurance payer and then mark the encounter’s eligibility with a status.
Whether you are looking at the Insurance Eligibility component inside the Review and Verify window, during Patient Check-In, during Post Charges, or on a patient’s chart note, the tools are the same.
When a patient has multiple insurance plans, each plan will be displayed within a separate bubble. Each eligibility request is performed independently.
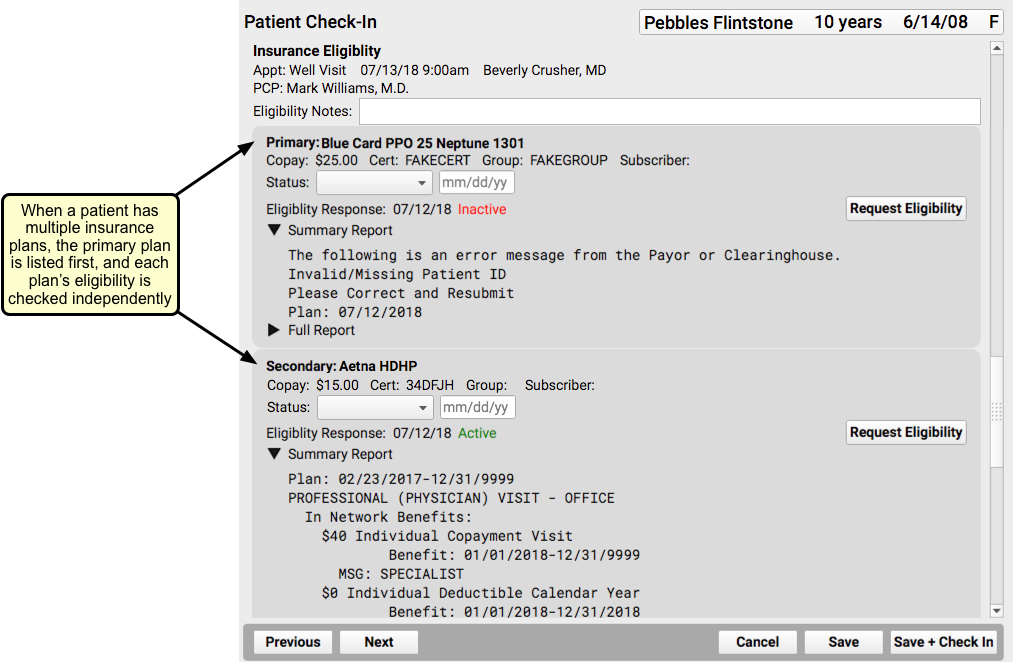
Eligibility Response
The Eligibility Response field will display “Active” in green, to indicate that the patient is covered, “Inactive” in red, meaning that the patient is not currently covered, or “Eligibility Undetermined” if the payer’s response is not sufficient to make a determination.
In some cases, such as when the eligibility request could not be submitted, you might also see a response of, “The eligibility request cannot be submitted.”
Whatever the Eligibility Response, you can read Alerts, Explanations, and Actions to know what to do next, and click to review the payers Summary Report and Full Report, when available.
Alerts, Explanations, and Actions
When an error has occured, PCC EHR explains the error and gives you action steps to fix the problem.
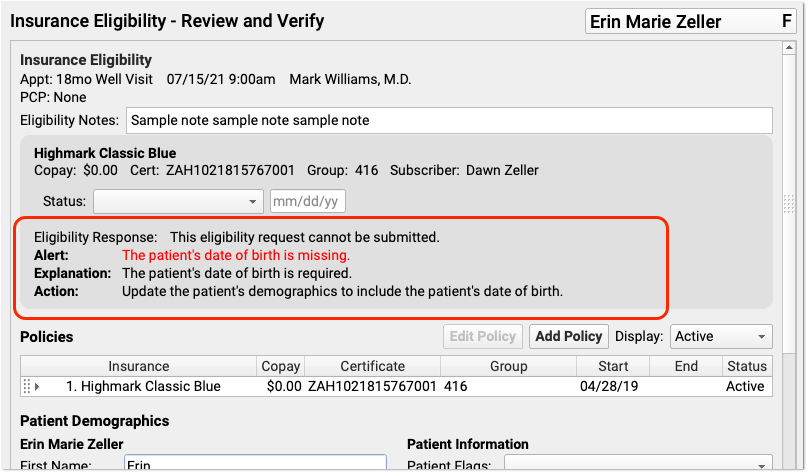
If the underlying issue is missing patient or policy information, you can quickly correct the problem and click “Request Eligibility” to try again.
If eligibility isn’t working due to underlying configuration, PCC EHR will provide you with useful information so you can contact PCC Support.
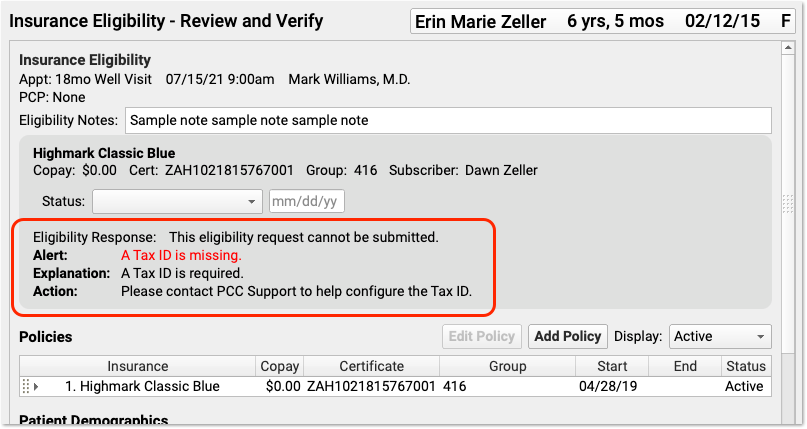
PCC EHR also summarizes more complex responses from the payer, and then provides the full payer report, when available.
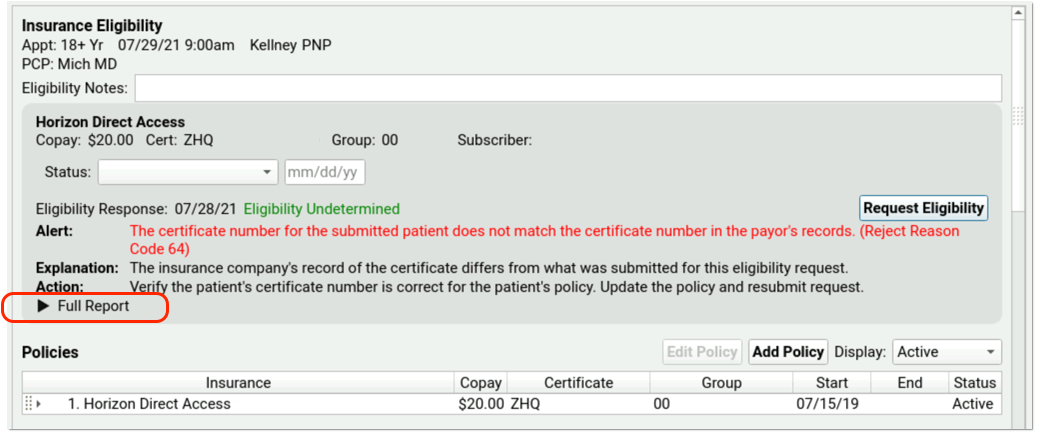
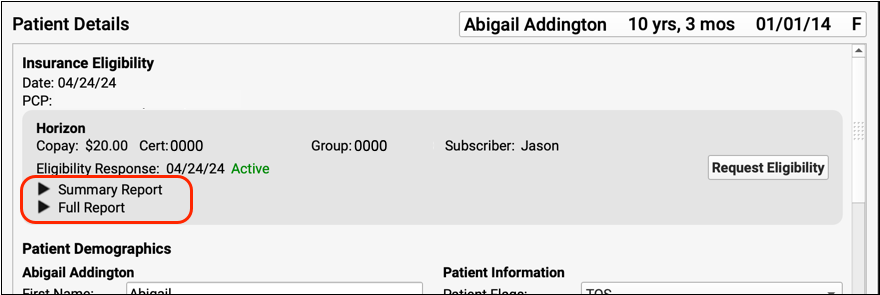
Summary and Full Report
If the payer has responded to the eligibility request, you can usually read a Summary and/or Full Report.
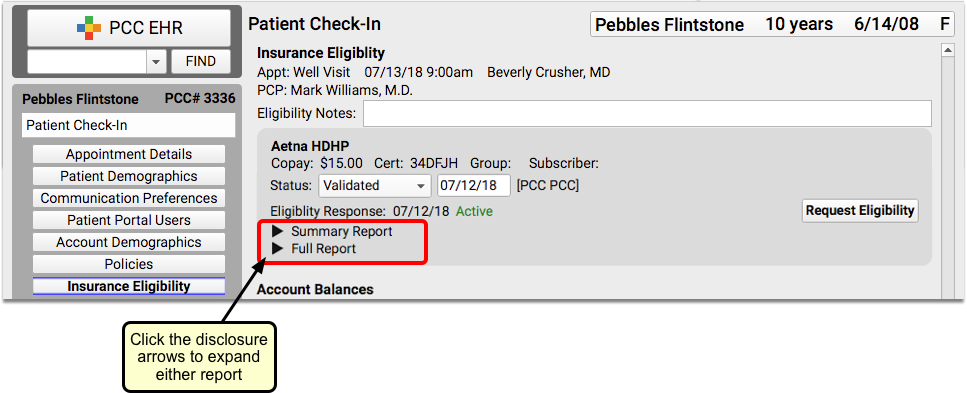
Click the disclosure triangles to see full details from the payer.
