Track Newborn Charges and Delay Billing the Family
Does your practice delay newborn billing until the family updates their insurance? Your practice can add a newborn patient to your PCC system, track newborn hospital and office encounters, and delay billing until the family has updated their insurance information
Contents
Define Your Practice’s Grace Period
Your practice decides on a grace period, or how long you delay billing for newborn charges. Your grace period is how much time you allow for parents to enroll their newborn. Before the end of that period, they need to circle back with you so that claims can be filed to insurance.
For example, you could decide to delay billing for newborn services for 30 days. Use your grace period value in the steps below.
Add the Patient and Post Newborn Encounter Charges
When you add the newborn patient to your PCC system, give them a “Newborn” policy with an end date and enter a Hold Bill Until date.
Add the Newborn Policy to the Patient
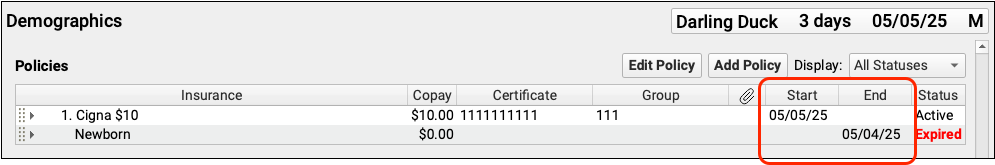
Add the “Newborn” insurance policy to the patient’s policies. Enter an “End Date” equal to the patient’s DOB plus your practice’s grace period.
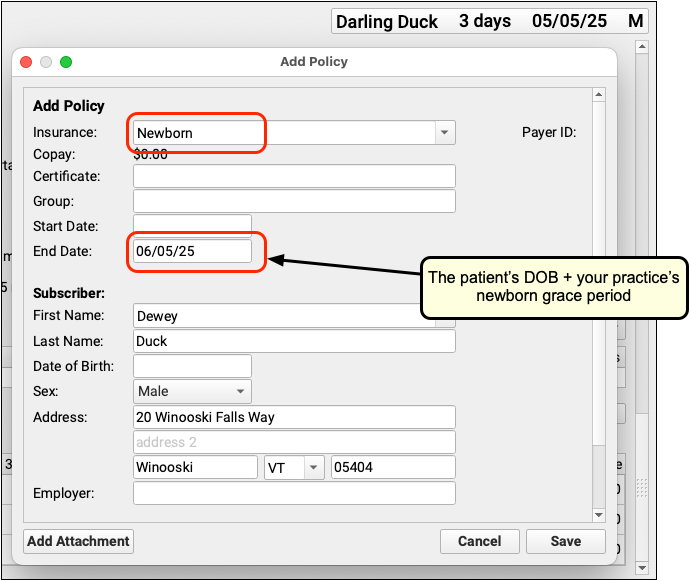
Can't Find the Newborn plan?: If your practice does not have a Newborn insurance plan on your PCC system, contact PCC Support.
Enter a Hold Bill Until Date for the Family
In the Demographics section of the chart, enter the same date in the billing family’s Hold Bill Until field.
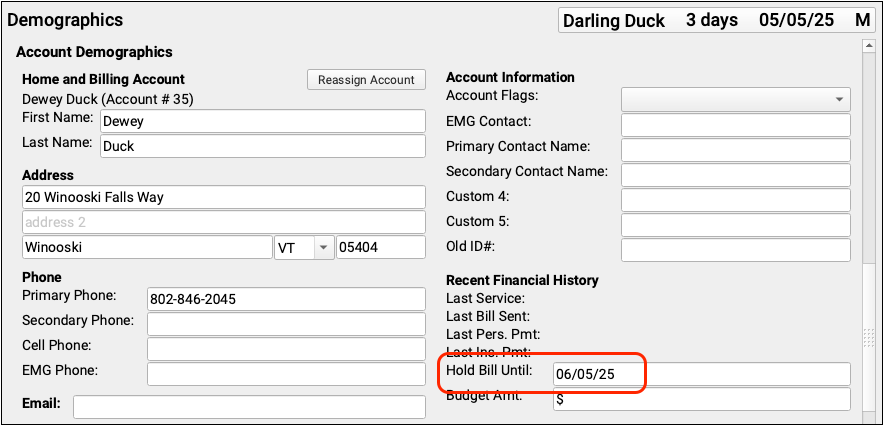
The Hold Bill Until date will prevent statements from being sent home until that date has passed.
Post Newborn Encounter Charges
For hospital encounters, use the “Create Encounter” button in the Billing History. For an in-office encounter, you can click “Ready to Post” on your Schedule screen.
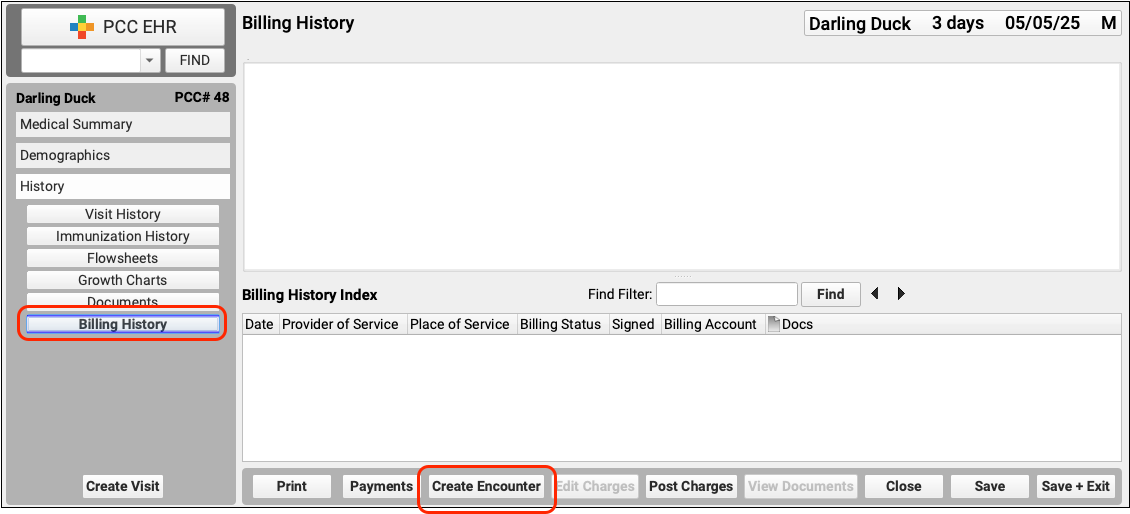
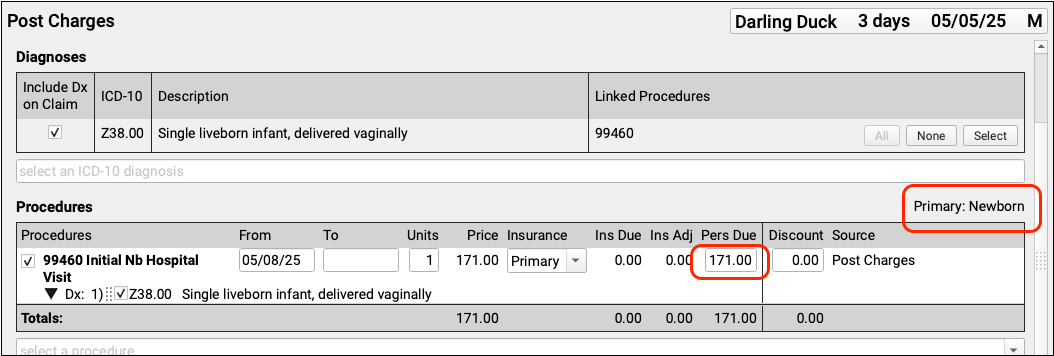
Because the patient has the Newborn insurance policy and the account has a Hold Bill Until date:
- The encounter charges will pend to the Newborn insurance policy but will not generate a claim.
- Unpaid encounter charges will be the billing account’s responsibility. However, the family won’t receive a statement until the Hold Bill Until date.
- The family has time to obtain insurance coverage and contact you to update the patient’s record. If they fail to do so before the end of your practice’s grace period, they’ll receive a statement for the amounts due.
Follow Up With Families
You can use PCC tools to follow up with the family and update their insurance information.
You can track all charges pending the Newborn insurance group in the Insurance Balances tool. Details about the amounts due will appear in the Account Balances component found in the Payments tool and in the patient’s chart.
You could also use a flag to mark accounts with outstanding newborn charges. Then your practice could use the Report Library to create custom lists. You could create a Clinical Alert so that your staff will remember to ask the family for updated insurance information at each encounter.
Update Records and Send Claims When You Receive Updated Insurance Information
Once the family has verified their newborn’s coverage, update the patient’s polices, edit each encounter to make it the payor’s responsibility, and queue up a claim.
Update the Patient’s Policies
Add the new insurance information to the patient’s policies. For the “Start Date”, enter the policy’s effective date.
Expire the Newborn insurance by entering an end date before the patient’s date of birth.
Edit Charges for Each Encounter
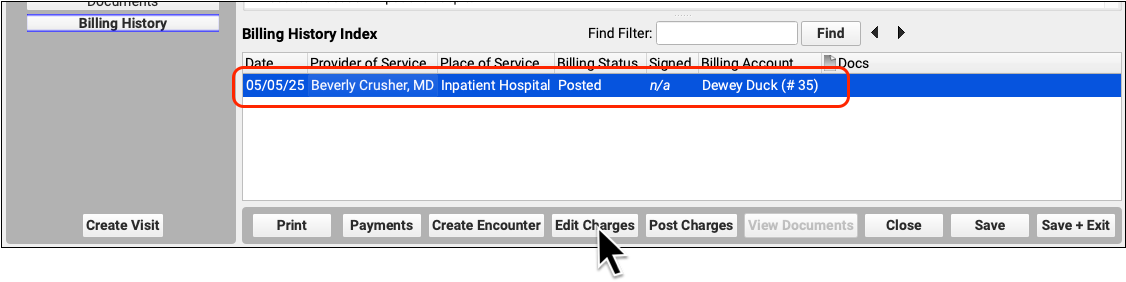
In the patient’s Billing History, select each encounter that needs a new claim and click “Edit Charges”.
Update Responsible Party and Personal Amount Due
Ensure that the new policy is now listed as primary and, if needed, adjust the “Insurance” for each charge to be “Primary”.
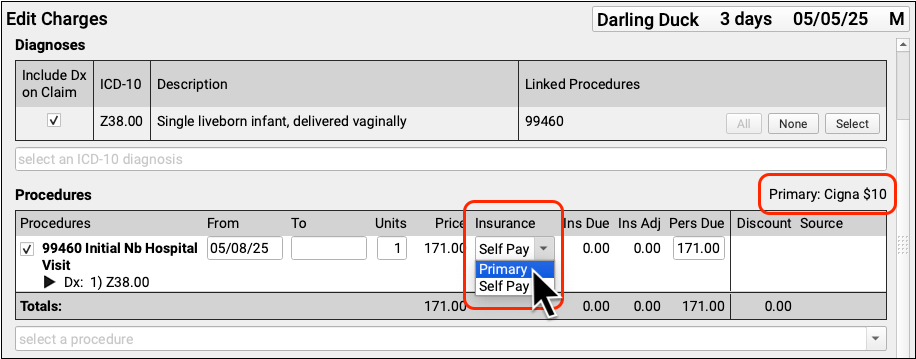
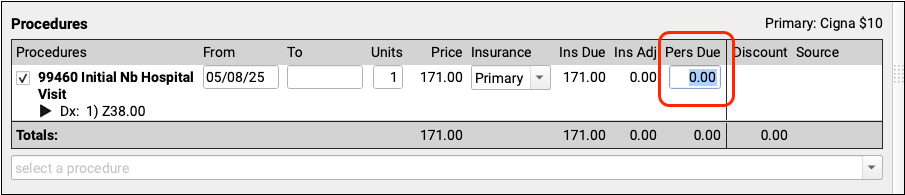
For each charge, change the Personal Due amount to zero.
Queue Up a Claim and Save Changes
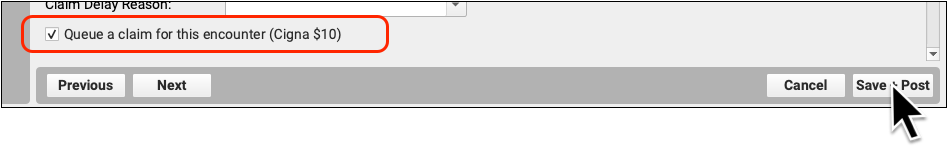
Double-check that the “Queue a claim for this encounter…” box is checked and then click “Save + Post”.
Edit Charges and Queue a Claim For Any Subsequent Encounters
Repeat these steps for any other encounters in the patient’s Billing History that should now be billed to the family’s insurance.
When you next run claims, your PCC system will process and submit the claims to the insurance payer.
