Code and Bill for COVID-19 Related Encounters
How does a pediatric practice code and bill for COVID-19 related encounters? Read below to learn about the SNOMED-CT, ICD-10, and CPT codes available for tests, diagnoses, and more. PCC Support can help you customize your chart note protocols, diagnoses, orders, and billing tools.
New Codes On Your System: Throughout 2020 and into 2021, PCC regularly updated your system to add vendor lab identifiers, SNOMED-CT descriptions, ICD-10 codes, and LOINC codes to help with COVID-19-related orders, charting and billing. Contact PCC Support if you have any questions or can’t find the code you need.
Procedure Code Guidance: The procedure codes discussed in this article are intended only as examples. You should consult the AMA’s current CPT Coding Guide and work with your insurance payers to verify what codes you should report on claims. Your practice updates and maintains your billable procedure list, codes, and prices in the Procedures table in the Tables configuration tool on your PCC system.
Contents
Code for Exposure or Other COVID-19 Related Symptoms
How do you code for exposure to COVID-19? What other diagnoses are used for a COVID-19 encounter, and how might you map those to SNOMED descriptions for use on a chart note?
Exposure
When you diagnose exposure to COVID-19, you can use:
- Z20.822 Contact with and (suspected) exposure to COVID-19
- SNOMED-CT Mapping Option: Exposure to SARS-CoV-2 (alternate title: Exposure to 2019 novel coronavirus)
History, Associated Symptoms, and More
What other ICD-10 billing codes, and corresponding SNOMED descriptions, are available for COVID-19 related encounters?
- B97.21 SARS-associated coronavirus as the cause of diseases classified elsewhere
- SNOMED-CT Mapping Option(s): Suspected disease caused by severe acute respiratory coronavirus
- Z86.16 Personal history of COVID-19
- SNOMED-CT Mapping Option(s): H/O: viral illness, H/O: infectious disease
- Z86.19 Personal history of other infectious and parasitic diseases
- SNOMED-CT Mapping Option(s): History of disease caused by Severe acute respiratory syndrome coronavirus
- Z03.89 Encounter for observation for other suspected diseases and conditions ruled out
- SNOMED-CT Mapping Option(s): Disease caused by Severe acute respiratory syndrome coronavirus 2 absent
- M35.81 Multisystem inflammatory syndrome (MIS)
- SNOMED-CT Mapping Option(s): Acute organ dysfunction due to systemic inflammatory response syndrome, Systemic inflammatory response syndrome, Systemic inflammatory response syndrome associated with organ dysfunction, Systemic inflammatory response syndrome without organ dysfunction
- M35.89 Other specified systemic involvement of connective tissue
- SNOMED-CT Mapping Option(s): Disorder of connective tissue co-occurrent and due to systemic disease
- J12.82 Pneumonia due to coronavirus disease 2019
- SNOMED-CT Mapping Option(s): (pneumonia diagnosis descriptions)
You might also use other diagnoses for common signs and symptoms:
- R051-R059 Cough
- R06.02 Shortness of breath
- R50.9 Fever, unspecified
Code for a Screening Encounter?: In December of 2020, the WHO added another related ICD-10: Encounter for screening for COVID-19 (Z11.52). During the COVID-19 pandemic, a screening encounter code is generally not appropriate. For encounters for COVID-19 testing, including preoperative testing, code instead as exposure to COVID-19.
Adjust Your PCC EHR Chart Note Protocols to Display COVID-19 Related Diagnoses
To make them easier to select, you can use the Protocol Configuration tool to add diagnoses directly to your practice’s chart note protocols.
When clinicians select a SNOMED diagnosis description, the mapped ICD-10 billing code appears on the Bill screen.
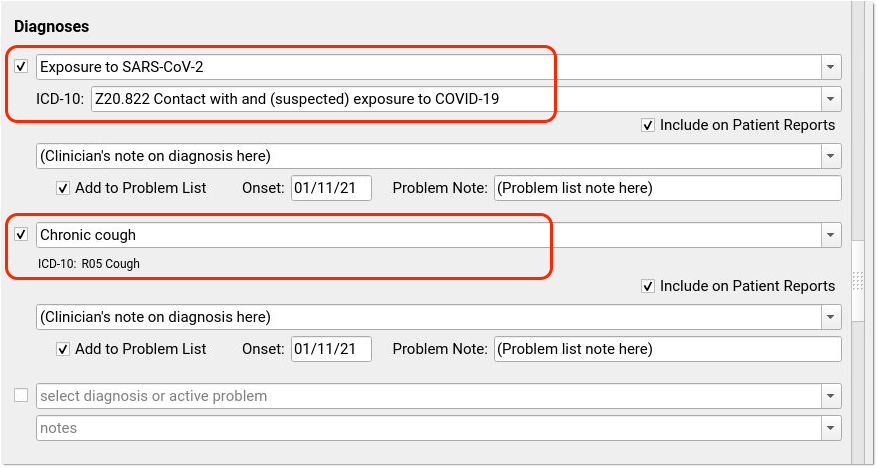
Many codes include pre-defined mapping. Use the Billing Configuration tool to adjust the mapping of SNOMED-CT descriptions to ICD-10 codes. Possible SNOMED to ICD-10 mappings are listed in the section above with each billing code.
Order and Code for COVID-19 Lab Tests
During an encounter, you may decide to order a COVID-19 test. When you order a COVID-19 test, your practice might collect the specimen and relay the test to a lab vendor for processing. Increasingly, pediatric practices are also completing tests in-house.
In PCC EHR, when you click “Order” next to a lab order, the appropriate LOINC will be part of the order, appropriate diagnoses and procedures can be queued up for billing, and optionally the lab test information can automatically be added to the chart note for incoming electronic results.
Set Up Your COVID-19 Lab Test Orders: You can learn how to create a COVID-19 lab test order on your system, add it to chart note protocols, and configure billing behavior by reading: Create a COVID-19 Test Lab Order. For additional details about Lab Configuration in PCC EHR, you can read Lab Configuration.
Billing Codes for COVID-19 Tests and Orders
When you gather the specimen for a COVID-19 test, you can bill:
- 99000: Handling and/or conveyance of specimen for transfer from the office to a laboratory
Depending on your lab configuration, and whether or not you perform the test in-house, you may use additional procedures for a COVID-19 test:
- 87635: Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
- 87426: Infectious agent antigen detection by immunoassay technique
- 86328: Immunoassay for infectious agent antibody(ies), qualitative or semiquantitative, single step method (eg, reagent strip); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19])
- U0002: 2019-ncov coronavirus, sars-cov-2/2019-ncov (covid-19), any technique, multiple types or subtypes (includes all targets), non-cdc
- G2023: Specimen collection for severe acute respiratory syndrome coronavirus 2 (sars-cov-2) (coronavirus disease [covid-19]), any specimen source. Note: This code is for use by independent labs, not private offices.
In PCC EHR, you can map your orders directly to the procedures you bill so they will automatically appear on your electronic encounter form automatically.
E-Lab Configuration Identifiers
You can configure lab orders so results will be sent back to your practice electronically, if your lab vendor supports e-lab integration.
Labcorp and Quest have provided the following vendor-specific identifiers, which PCC added to all practice systems:
- Labcorp COVID-19 Test: 139900
- Quest SARS-CoV-2 RNA, Qual Real-Time Test: 39433
Code and Bill a COVID-19 Diagnosis
During an in-person or telemedicine visit for a patient with a COVID-19 diagnosis, you would code both the COVID-19 diagnosis and related conditions.
When you indicate a COVID-19 diagnosis with a SNOMED description, use:
-
840539006 Disease caused by 2019-nCoV: This diagnosis has alternate, searchable names of “Disease caused by 2019 novel coronavirus” and “Disease caused by Wuhan coronavirus”.
In PCC EHR, you can select this diagnosis on a chart note and/or add it to a patient’s Problem List.
For all encounters that occured after April 1st, 2020, use this code when you bill for a visit with a patient with a positive COVID-19 diagnosis:
- U07.1 COVID-19
This code was added to all PCC systems with a 2020-03-23 update. By default in PCC EHR, when you select the SNOMED COVID-19 description, the ICD-10 COVID-19 code will appear:
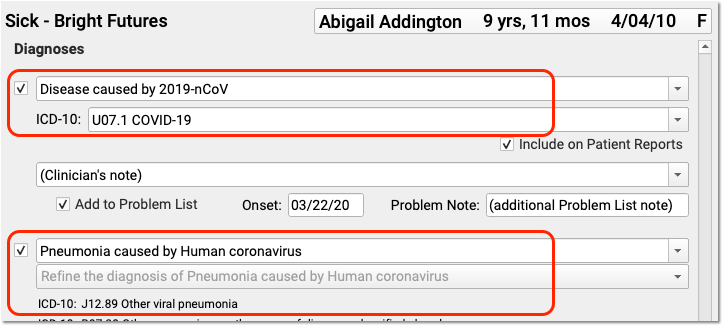
For services rendered prior to the April 1st effective date of U07.1 COVID-19, the CDC recommends you chart and code for the conditions of Pneumonia, Bronchitis, Lower Respiratory Infection, Respiratory Infection NOS, and ARDS, and then adding B97.29 Other coronavirus as the cause of diseases classified elsewhere. Before the specific COVID-19 ICD-10 diagnosis code is in effect, use the less specific B97.29 secondary to the manifestation code to indicate the patient has COVID-19.
Details May Change: The above scenarios and COVID-19 codes are new and payer response may vary. PCC keeps an up-to-date handout with COVID-19 coding and billing recommendations here: 2020 COVID-19 Coding Guide. We will update that PDF and this article as the situation changes and we learn more.
Use Other Procedure CPTs for COVID-19 Related Visits
In addition to the codes mentioned above, here are some other CPT codes you might use in relation to a COVID-19 related encounter.
Code for Telemedicine, Phone Calls, Portal, Email and Other Remote Services: What CPT visit code should your practice use for a video telemedicine encounter, a telephone call, a portal message consultation, or other remote service? PCC is maintaining a COVID-19 Coding Guide with descriptions of appropriate codes for different circumstances. You can also read PCC’s Schedule, Chart, Code, and Bill for Telemedicine Encounters.
Bill for COVID-19 Risk Counseling
Your practice may talk with a patient or parent at length about COVID-19 risk. You could use:
- 99401: Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual (separate procedure) approximately 15 minutes
- 99402: …approximately 30 minutes
- 99403: …approximately 45 minutes
- 99404: …approximately 60 minutes
You may use these codes for COVID-19 risk reduction and prevention counseling. You can add these codes onto a claim with other office visit codes, or they can stand alone.
Are These Codes Okay for Telemedicine?: Although these codes do not appear in Appendix P of the CPT manual, which lists telehealth or telemedicine codes, many states are currently mandating that all services, including the 99401-99403 codes, be billable in a telemedicine encounter.
Add-On CPTs for Urgent and Unusual Circumstances
If an emergency appointment disrupts your office’s schedule, such as the sudden arrival of a patient with Acute Respiratory Distress, you can use this additional code on the claim:
- 99058: Service(s) provided on an emergency basis in the office, which disrupts other scheduled office services, in addition to basic service
If you have to leave the office for an emergency visit that disrupts your schedule:
- 99060: Service(s) provided on an emergency basis, out of the office, which disrupts other scheduled office services, in addition to basic service
If you leave the office for an encounter at the request of the patient or family, you might add:
- 99056: Service(s) typically provided in the office, provided out of the office at request of patient, in addition to basic service
We're Seeing Kids in the Parking Lot. Is That a 99056?: If the patient or family makes a special request for you to come out to the parking lot to perform a visit, you may add this code. If your practice sees patients in your parking lot as your general office policy during the COVID-19 epidemic, this code may not apply.
Vaccine, Administration, and Counseling Codes
Payment for administration of COVID-19 vaccine varies among payers and states. You should consult your CPT resource for guidance, and speak with your payers.
Guide to COVID-19 Vaccines in PCC EHR: Read COVID-19 Vaccines: Plan, Configure, Order, Administer, and Track to learn about the MVX, CDX, NDC, and CPT codes needed for COVID-19 vaccine encounters.
How to code for COVID-19 vaccine-related encounters has continued to evolve and change during 2021. For example, in June of 2021, North Carolina Medicaid changed their payment policy for CPT 99401 (Preventative medicine counseling and/or risk factor reduction intervention) to allow for an additional 15 minutes to counsel about the benefits of receiving COVID-19 vaccine. They require a CR modifier on the code. When this change occurred, PCC reached out to North Carolina clients.
If you learn of similar updates to policy, please reach out to PCC and/or PCC Community to share!
