How to Chart for Clinical Quality Measures in PCC EHR
You can use PCC EHR to collect data for standardized measure reporting required by NCQA’s Patient Centered Medical Home (PCMH) Program or other external entities requiring clinical measure reporting from your practice. To learn more about NCQA’s standardized measure reporting, visit PCMH Standardized Measurement.
Read the article below to learn how to chart and configure your system in order to record medical information for each clinical quality measure. By following these recommendations, and training your practice on charting workflow for CQMs, you can make sure that PCC EHR records the correct data to calculate your CQM performance.
Contents
- 1 Run the Clinical Quality Measures Report to See Your Practice’s Current Results
- 2 Pediatric CQMs Overview Chart: Adjust Your Practice’s Configuration and Visit Workflow
- 3 CMS2: Preventative Care and Screening: Screening for Clinical Depression and Follow-Up Plan
- 4 CMS117: Childhood Immunization Status
- 5 CMS155: Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents
Run the Clinical Quality Measures Report to See Your Practice’s Current Results
Clinical Quality Measures (CQMs) are designed to evaluate certain patient populations and compare chart activity to coding. The overall goal of CQMs is to show improvement over time.
You can report on your practice’s numbers for certain custom measures in your Practice Vitals Dashboard.
Pediatric CQMs Overview Chart: Adjust Your Practice’s Configuration and Visit Workflow
For a quick understanding of each measure, use the table below. You can click the “More Details” or “Show Me How” links to jump directly to a longer description, accompanied by screenshots and examples.
| CMS | NQF | Measure Name | Calculation Description | Configuration in PCC | Clinician Workflow |
|---|---|---|---|---|---|
| 2 | 0418 | Preventative Care and Screening: Screening for Clinical Depression and Follow-Up Plan | For all patients seen for a qualifying encounter during the reporting period, who were 12 years old or older at the time of the qualifying encounter, who did not already have a bipolar diagnosis or contraindication, who did not refuse the screening, what percentage received a depression screening, and, if the result was positive, received additional follow-up care, such as a mental health care education or a referral to a behavioral specialist? (More Details) |
|
|
| 117 | 0038 | Childhood Immunization Status | For all patients seen by the eligible professional during the reporting period and turning two years old during the reporting period, what percentage had four diphtheria, tetanus and acellular pertussis (DTaP); three polio (IPV), one measles, mumps and rubella (MMR); three or four H influenza type B (HiB); three hepatitis B (Hep B); one chicken pox (VZV); four pneumococcal conjugate (PCV); one hepatitis A (Hep A); two or three rotavirus (RV); and two influenza (flu) vaccines by their second birthday, or had a documented history of the illness, seropositive result for the antigen, or a contraindication for a specific immunization? (More Details) |
PCC EHR’s standard installation includes most of the configuration required in order to chart for this measure.
|
|
| 155 | 0024 | Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents | For all patients seen by the eligible professional during the reporting period, who were between 3 and 17 years of age, what percentage had their height, weight, and BMI recorded, and what percentage received counseling for nutrition and/or physical activity? (More Details) |
|
|
CMS2: Preventative Care and Screening: Screening for Clinical Depression and Follow-Up Plan
This measure calculates the percentage of patients aged 12 years and older who are screened for clinical depression on the date of their encounter using an age-appropriate standardized depression screening tool AND if positive, a follow-up plan is documented on the date of the positive screen. (CMS at eCQI)
-
Denominator: PCC EHR calculates the denominator of this measure by counting all patients who had an eligible encounter code billed in the electronic encounter form during the reporting period and who were 12 or older before the reporting period. Eligible encounter codes include billed CPT codes for Sick (99202-99205, 99212-99215), Well (99384-99387, 99394-99397) Telephone Visits (98966-98968, 99441-99443), Psychotherapy (90791-90792, 90832-90837), or other counseling services.
-
Numerator: PCC EHR calculates the numerator of this measure by counting all of the patients in the denominator who had a LOINC test for depression screening, generally inside a Depression Screening order, with a positive or negative result, on the encounter date. If the result was positive, the patient must have additional care in the form of a completed LOINC test for suicide risk assessment, follow-up or additional evaluation for depression, and/or a referral for depression, and/or a prescription for a depression medication, on the same date as the depression screening, in order to be included in the numerator.
-
Exclusions: If a patient already had an active diagnosis for Bipolar Disorder on their Problem List (or in the Diagnoses component for the qualifying visit), they will be counted in the Exclusions for the measure. Some relevant codes to indicate bipolar disorder include ICD-10 code F30.— and F31.—, manic episode and bipolar disorder diagnosis codes that can used as a billed ICD-10 code. In addition, you can use SNOMED code 13746004 for bipolar disorder as a diagnosis code in the problem list or diagnosis component when charting a visit.
-
Exceptions: If a patient refused the screening, or had a medical contraindication for it being performed, such as an urgent medical situation or a lack of functional capacity to complete the screening, they are excepted from the denominator (and the numerator) for the calculation and will be counted in the Exceptions for the measure. Marking the screening as refused or contraindicated will count the patient as an exception.
Recommended PCC EHR Configuration for CMS2 Depression Screening
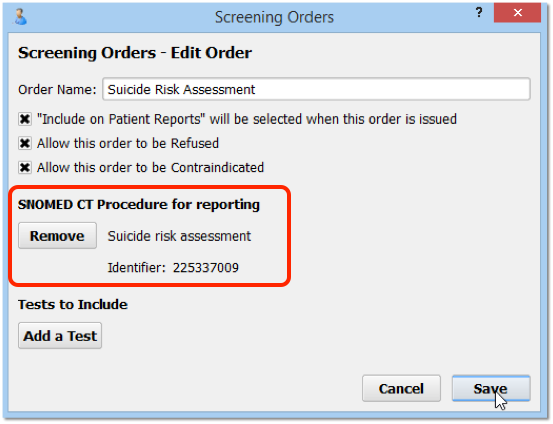
In order to chart depression screenings, follow-up, and suicide risk assessment, your practice can create screening orders and add the specified LOINC tests or SNOMED-CT descriptions to those orders. You can also configure referral orders so that they are recorded with an appropriate SNOMED-CT. Finally, you can add the orders to chart notes so they are easy to select at every visit.
For a step-by-step procedure on how to add codes to orders and add specific orders to chart notes, read Use Orders to Track Measures for Mandates.
Configure Your Depression Screenings
Add SNOMED-CT and LOINC codes to your adolescent depression screening orders in PCC EHR.
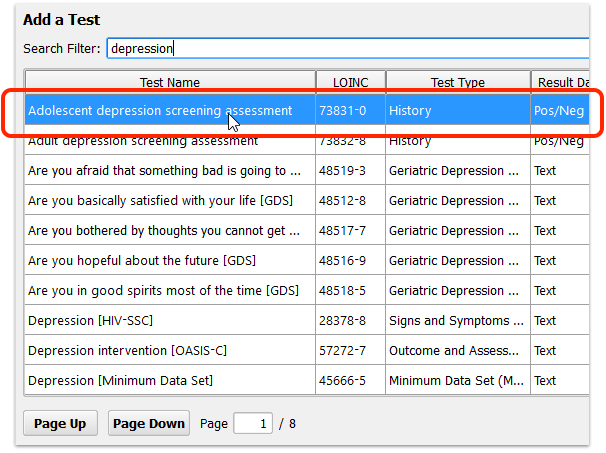
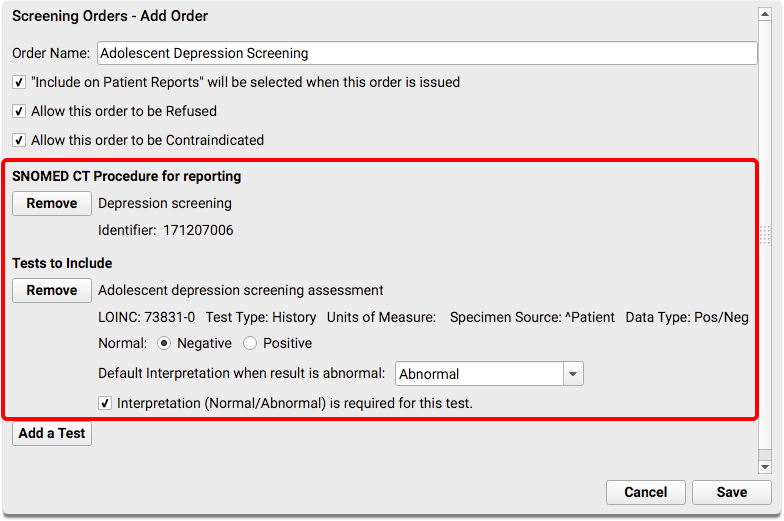
For the initial depression screening, you should add SNOMED-CT procedure code 171207006, and LOINC test code 73831-0, “Adolescent depression screening assessment”. (You could also add LOINC 73832-8, “Adult depression screening assessment” for an order for patients 18 years or older.) The test should have a Negative/Positive result.
| Code Set | Code | Description | Notes |
|---|---|---|---|
| LOINC | 73831-0 | Adolescent Depression Screening Assessment | Link this code to all adolescent depression screening orders |
| LOINC | 73832-8 | Adult Depression Screening Assessment | Link this code to all adult depression screening orders |
| SNOMED | 171207006 | Depression Screening | Link this code to all adolescent and adult depression screening orders |
Do you already have a specific LOINC code that works best for your office? You can add more than one test to a single order. Add your preferred code to the order so that you don’t have to compromise on workflow while still meeting the measure.
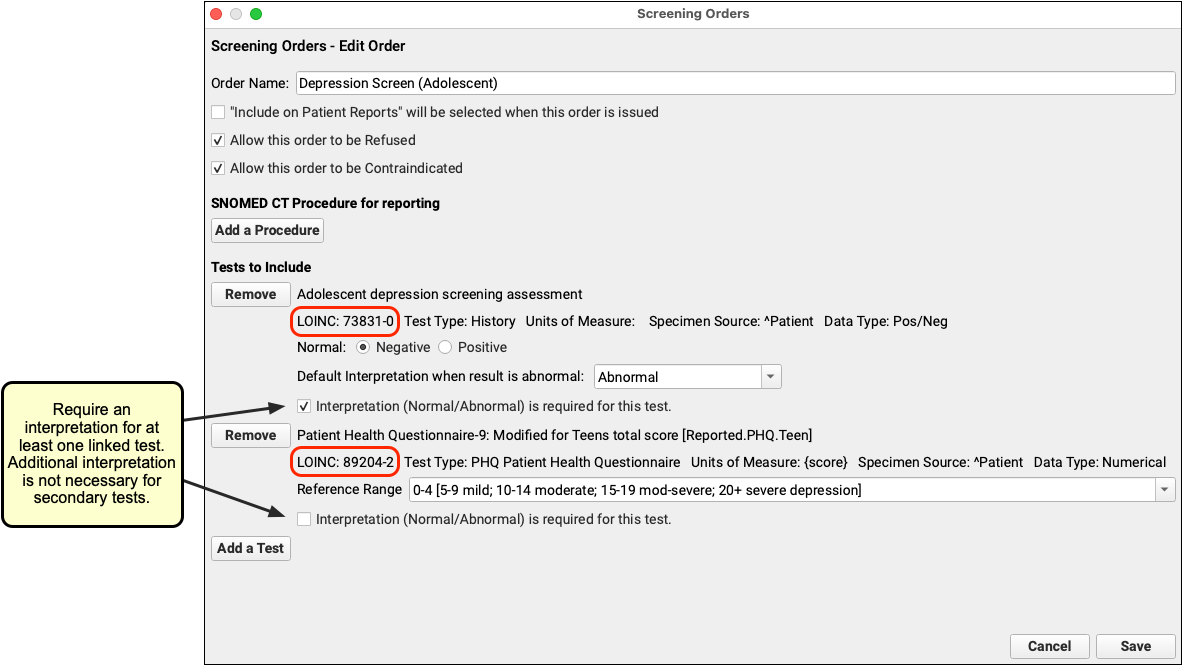
What About Other Depression Screening Tests?: Your practice might perform other depression screenings and use other LOINC tests to record discrete results. You can add more than one test to a single order. For example, if you perform a PHQ-9 at each visit, you might first add the “Adolescent depression screening assessment” test, which is used by the clinical quality measure, and then also add the “Patient Health Questionnaire 9 item (PHQ-9) total score” test in order to record the patient’s numerical result. Postpartum depression screening orders are usually billed in association with the newborn patient and are not be tracked by this measure.
Configure Follow-up Depression Care
When a patient has a positive result on a depression screening, your practice might perform one or more additional evaluations, follow-up orders, referrals, or mental health interventions.
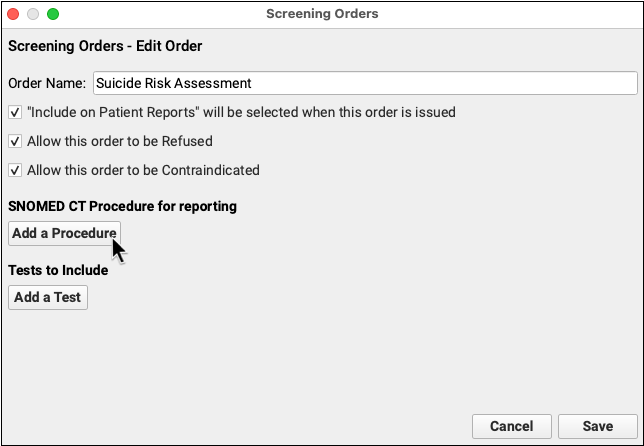
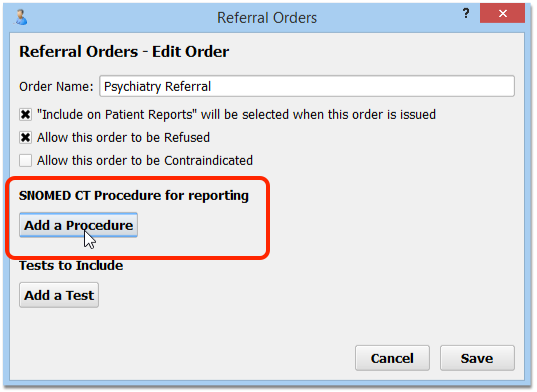
In order to affect the clinical quality measure for this additional evaluation, follow-up, or mental health intervention, your practice must also add SNOMED-CT procedures to the screening order. For each order, edit the order, click “Add a Procedure” and search for the appropriate SNOMED-CT description.
Examples:
-
Mental Health Care Education: When offering a patient mental health care education, add SNOMED-CT code 41022408, “Mental Health Care Education” to the order.
-
Follow-up For Depression: You could also create and add SNOMED-CT descriptions (and LOINC tests, if appropriate) for any number of depression follow-up orders, such as Completion of a Mental Health Crisis Plan, or Coping Support Management. Other options are included in the NIH’s Follow-up for Depression – adolescent value set, found on the VSAC website.
-
Additional Evaluation: For an additional evaluation for depression order, you could add one of the SNOMED-CT descriptions for psychiatric evaluation listed by NIH for Additional evaluation for depression – adolescent value set on the VSAC website.
Configure Depression Referral Orders
Add SNOMED-CT procedures to your Referral orders for Depression.
Your practice may have one or more referrals related to depression. For example, you may have referrals for an initial psychiatric evaluation or a specific depression referral. Click “Add” to create a new order, or double-click on an existing order to make changes.
In order for the referral to be tracked as part of a clinical quality measure, you must add a SNOMED-CT description from to the order. The table below contains several SNOMED codes that will work for this measure.
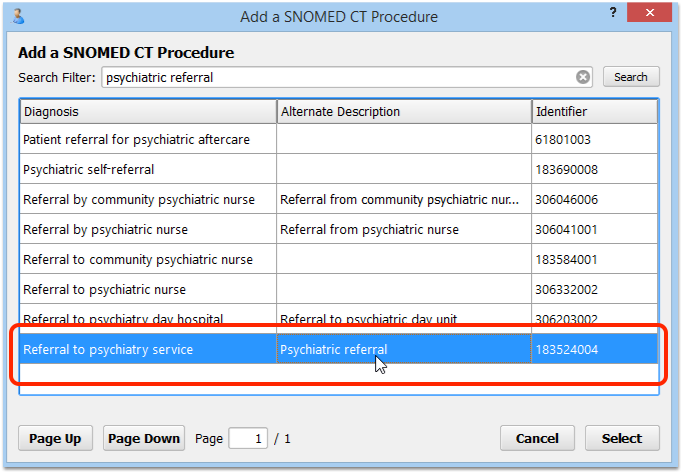
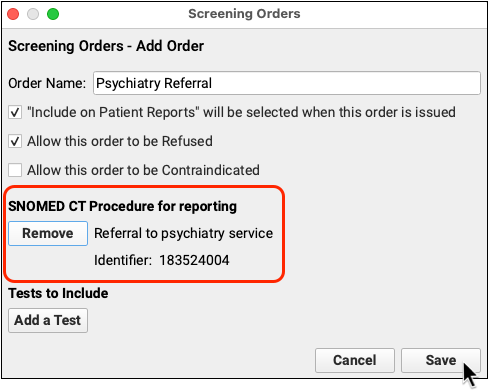
Your practice may have other referrals that may follow a positive depression screening. Add new orders, or double-click on an existing order to make changes. The following table contains generic SNOMED codes that you can link to your follow-up on depression screening orders.
| Code Set | Code | Description | Notes |
|---|---|---|---|
| SNOMED | 41022408 | Mental health care education | Link this code to an “Intervention provided for positive depression screening” follow-up or screening order |
| SNOMED | 81294000 | Patient referral for psychotherapy | Link this code to the relevant referral order |
| SNOMED | 306227000 | Referral for mental health counseling | Link this code to the relevant referral order |
| SNOMED | 75516001 | Psychotherapy | Link this code to the relevant follow-up or referral order |
| SNOMED | 385726000 | Emotional support education | Link this code to the relevant follow-up order |
Add Depression Screening, Mental Health Care Education, and Referral Orders to Your Chart Note Protocols
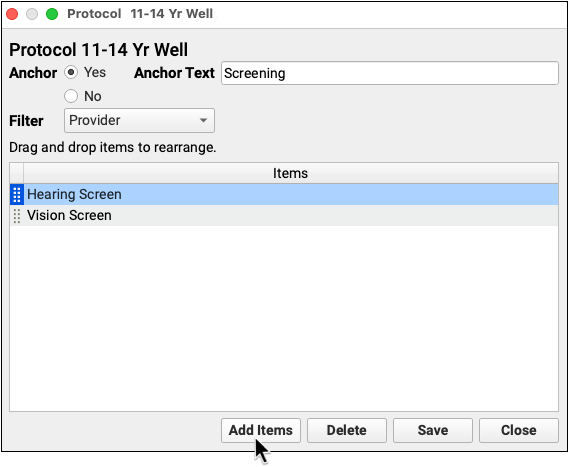
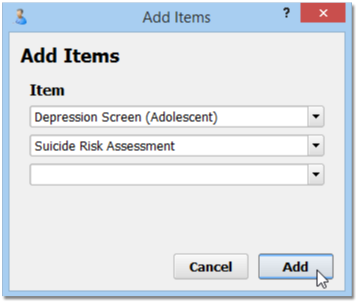
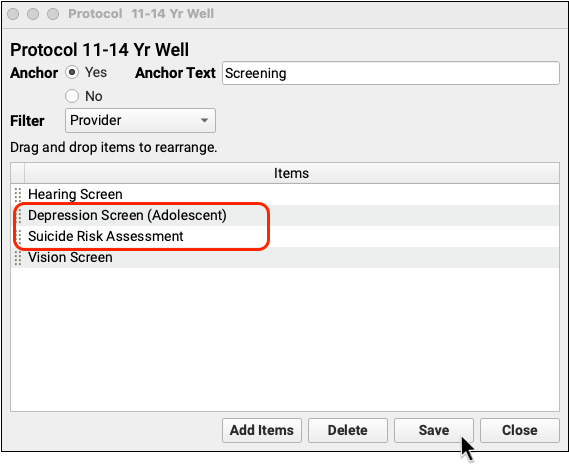
After you make changes to the various orders your practice uses, you can add them to chart note protocols to make them easier to order. Your clinicians will then see the “Depression Screening” order, for example, on every chart note.
For information on how to add specific orders to a chart note protocol, read Use Orders to Track Measures for Mandates.
Configure CHADIS Depression Screenings
If your practice uses CHADIS, add a LOINC code to the screening order so that the test is documented for CQM reporting.
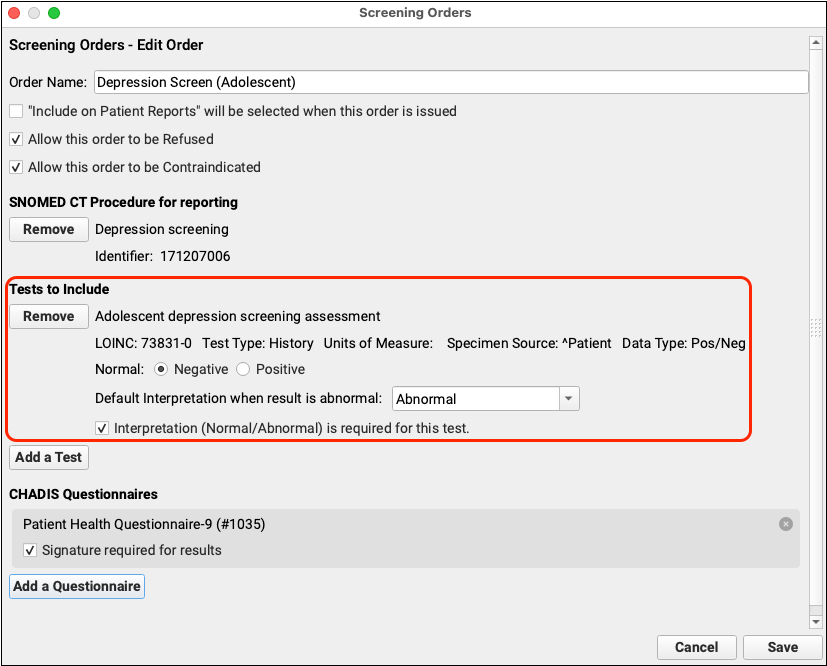
The CQM report looks for a positive result on the screening order and a subsequent follow-up action. Be sure to add a result to the order when your CHADIS questionnaires come in.
Adding a result to the order has the added benefit of making the result visible at a glance in patient flowsheets.
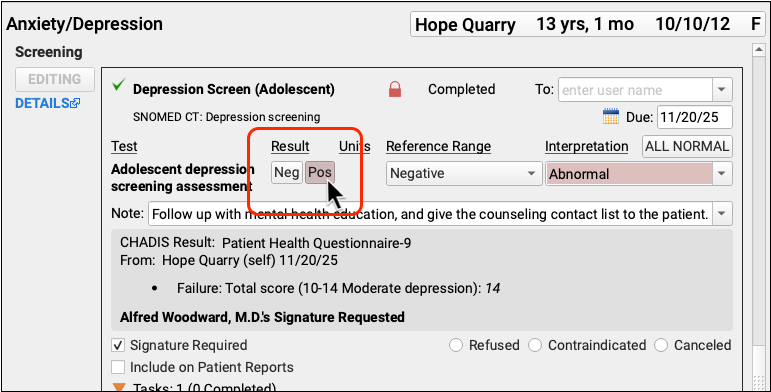
Recommended Charting and Workflow for CMS2 Depression Screening
When a patient twelve or older visits your practice, click “Order” to order a Depression Screening.
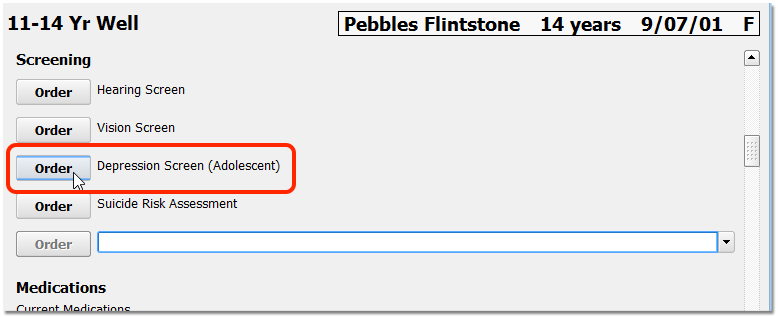
Optionally, you can assign the screening to another clinician, or complete the screening immediately. When the screening is complete, enter a result.
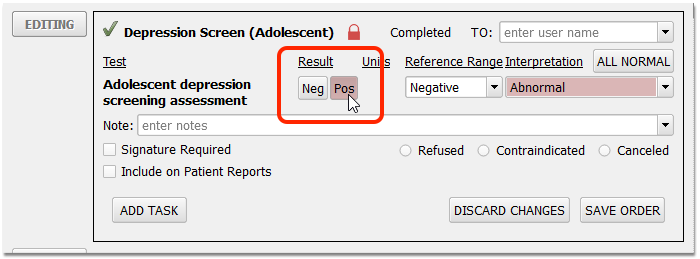
If the screening is refused, select “Refused” and add a note in the order. If the screening is contraindicated, select “Contraindicated” and add a note in the order. Marking the screening as refused or contraindicated will count the patient as an exception.
Unless refused or contraindicated, a positive or negative result is required. Result interpretation, in the Interpretation field, is not required for the clinical quality measure, though your practice may have configured it to be required for completion of the order.
If the result is positive, record whatever additional care follows. For example, you may prescribe appropriate medication, order an Intervention for Positive Depression screening, or order a referral.
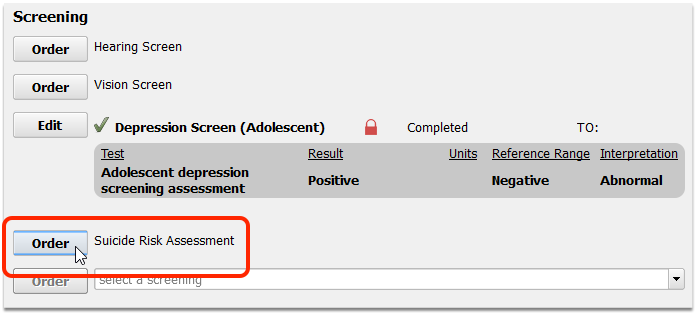
Enter results and take any other appropriate follow-up steps.
When you are finished charting, remember to click “Bill” and select an appropriate visit encounter code. In addition to billing, the visit encounter code is used to calculate the CQM.
CMS117: Childhood Immunization Status
This measure calculates the percentage of patients turning 2 years old during the reporting period who have a visit during the reporting period and have four diphtheria, tetanus and acellular pertussis (DTaP); three polio (IPV), one measles, mumps and rubella (MMR); three H influenza type B (HiB); three hepatitis B (Hep B); one chicken pox (VZV); four pneumococcal conjugate (PCV); one hepatitis A (Hep A); two or three rotavirus (RV); and two influenza (flu) vaccines with evidence of administration prior or on their second birthday.
-
Denominator: PCC EHR calculates the denominator of this measure by counting all patients who turned 2 years old during the reporting period, who had an eligible encounter code entered on the electronic encounter form during the reporting period. Eligible encounter codes include billed CPT codes for in-person and virtual sick (99202-99205, 99212-99215), well (99381-99384, 99391-99394), telephone visits (98966-98968, 99441-99443), or home healthcare visits (99341-99350).
-
Numerator: PCC EHR calculates the numerator of this measure by counting all of the patients in the denominator who have the full series of recommended vaccines within the appropriate schedule by age two. This measure counts both historical and administered vaccines, and patients must show evidence of meeting all the immunization requirements, either ordered, added manually to the patient record, or billed.
- Special inclusions: There are numerous reasons for a patient to be included in the numerator even if they did not have a particular shot.
- For the MMR, hepatitis B, VZV and hepatitis A vaccines, numerator inclusion criteria include: evidence of receipt of the recommended vaccine; documented history of the illness; or, a seropositive test result for the antigen.
- For the DTaP, IPV, HiB, pneumococcal conjugate, rotavirus, and influenza vaccines, numerator inclusion criteria include only evidence of receipt of the recommended vaccine. Patients may be included in the numerator for a particular antigen if they had an anaphylactic reaction to the vaccine. Patients may be included in the numerator for the DTaP vaccine if they have encephalopathy. Patients may be included in the numerator for the IPV vaccine if they have had an anaphylactic reaction to streptomycin, polymyxin B, or neomycin.
- Patients may be included in the numerator for the influenza, MMR, or VZV vaccines if they have cancer of lymphoreticular or histiocytic tissue, multiple myeloma, leukemia, have had an anaphylactic reaction to neomycin, have Immunodeficiency, or have HIV. Patients may be included in the numerator for the hepatitis B vaccine if they have had an anaphylactic reaction to common baker’s yeast.
-
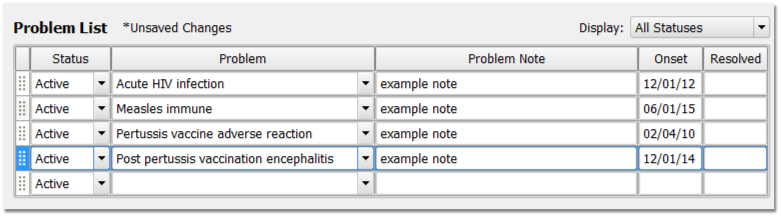
Exclusions and Exceptions: This measure will exclude children who are diagnosed as being in hospice care for any part of the measurement period as well as children who are diagnosed with any of the following conditions on or before the child’s second birthday: Severe Combined Immunodeficiency, Immunodeficiency, Human Immunodeficiency Virus (HIV), Lymphoreticular Cancer, Multiple Myeloma or Leukemia. Intussusception. For any immunization status exclusions, PCC checks the patient’s diagnosis history, Problem List, and Allergies List.
Recommended PCC EHR Configuration for CMS117 Childhood Immunization Status
When your practice implemented PCC software and services, the initial setup and configuration was sufficient to allow clinicians to chart in order to meet this CQM.
For more information on CVX and MVX codes in your PCC system, read CVX, MVX, VIS and NDC Codes in PCC.
What CVX Codes Are In Use?: Different combination vaccines and different formulations have different CVX codes. To review what CVX codes you administer, visit your immunization refrigerator. PCC Support can also help you compare the CVX codes in your PCC system with the CDC’s library of CVX codes. Common CVX codes for each immunization as of 2019 are as follows: DTaP 20, IPV 10, MMR 03, HIB 49, Hepatitis B 08, Varicella (chicken pox) 21, Prevnar 13 (pneumococcal conjugate PCV) 133, Hepatitis A 83, Rotavirus 116, Influenza (Flu) Preservative Free 140.
Add Age-Appropriate Immunizations to Your Custom Chart Notes
Do all of your custom chart notes have age-appropriate immunization orders ready, easy for your clinicians to click?
If not, follow the procedure below to update your chart note protocols.
Add Age-Appropriate Immunizations to Your Custom Chart Notes
Recommended Charting and Workflow for CMS117 Childhood Immunization Status
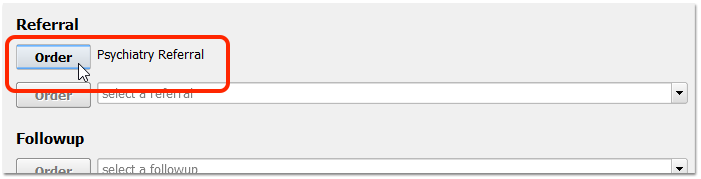
When a patient visits your practice, review their immunization history in the chart note or in the Immunization History section of the chart.
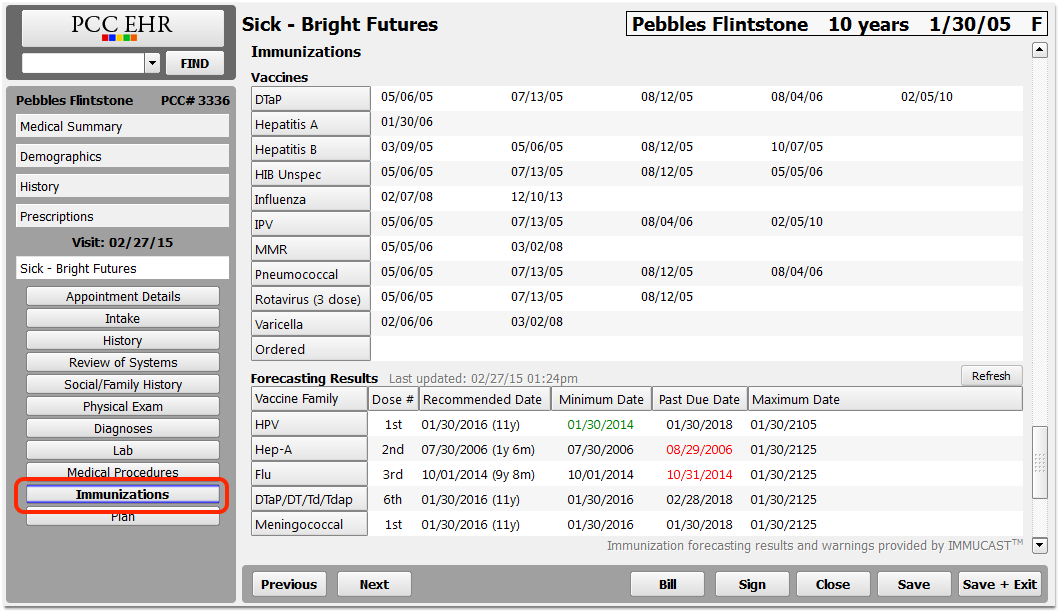
Optionally, you can review Forecasting Results and Forecasting Warnings to see what immunizations a patient may be missing.
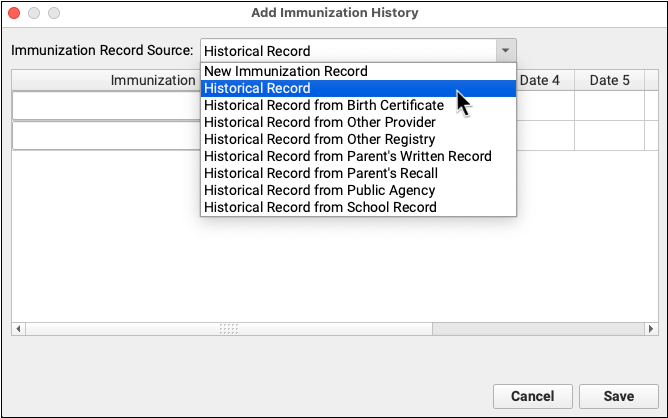
If you need to update a patient’s past immunization history, visit the Immunization History section of the chart, click “Add Imms” and add any immunizations they received that are not in the chart record.
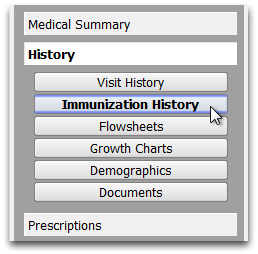
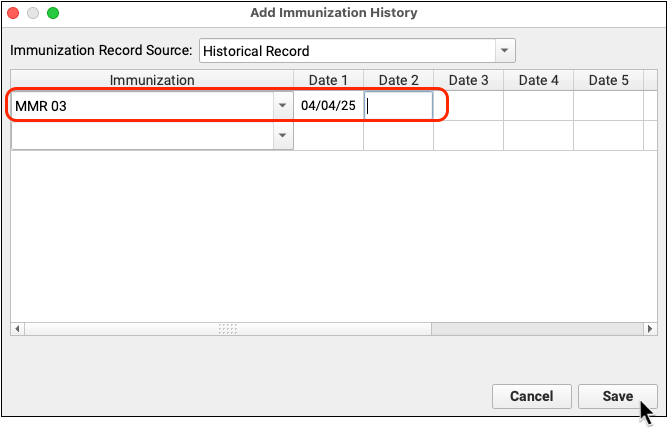
Use the Immunizations component on the chart note to order any age-appropriate immunizations.
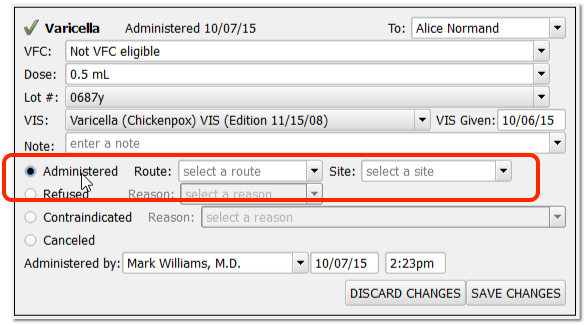
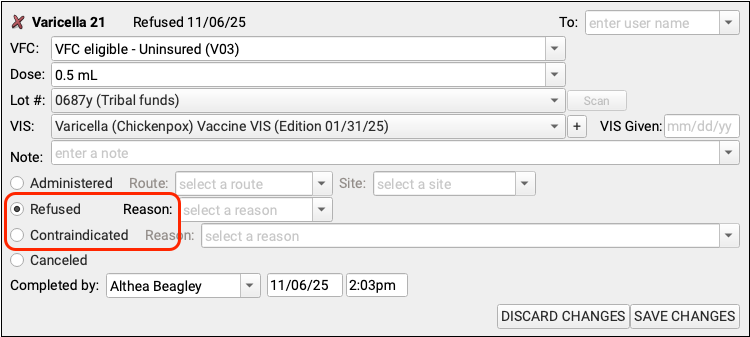
Use the same component (or “Edit Orders” orange indicator tool on Schedule screen) to record that the immunization is administered, refused, contraindicated, or canceled.
When Should Each Shot Be Given?: PCC EHR can display Immunization Forecasting, with results and forecasting calculated by STC’s implementation of the ACIP immunization schedule guidelines from the CDC. Your practice may have their own set of standards for how these guidelines are implemented, and CMS has their own published clinical recommendation based on ACIP’s guidelines. The rules for reporting for the Childhood Immunization Status CQM, however, are much simpler, only requiring the correct number of shots, given more than a day apart.
If you make a decision not to give an immunization, chart the reason in the following manner:
-
Contraindications: If a patient has a contraindication for an immunization, click “Contraindicated” in the order, and add the appropriate diagnosis description to the Diagnoses component in the chart note and/or to the patient’s Problem List or Allergies list. For example, if a patient has acute HIV infection, or an allergy to an immunization component, you should record that information in the Problem List and the Allergies List respectively.
-
Refused: If a patient or family refuses an immunization, click “Refused” in the immunization order. Marking a vaccine as Refused will remove the patient from the numerator in your Immunization Tracking CQM report. This is not an exclusion or exception.
-
History of an Illness: If a patient has a history of an illness for which an immunization would otherwise be administered, add that illness to the patient’s Problem List or chart it in the Diagnoses component.
-
Evidence of Immunity: If your practice performs titers, or receives a test result showing that the patient is seropositive for an antigen, record that result as a diagnosis or on the Problem List.
When you are finished charting, remember to click “Bill” and select an appropriate visit encounter code. In addition to billing, the visit encounter code is used to calculate the CQM.
CMS155: Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents
This measure calculates the percentage of patients 3-17 years of age who had had a visit during the reporting period, and had their height, weight, and body mass index (BMI) documented, and/or received counseling for nutrition, and/or received counseling for physical activity. (CMS at eCQI)
-
Denominator: PCC EHR calculates the denominator of this measure by counting all patients who had an eligible encounter code billed on the electronic encounter form during the reporting period and who were between 3 and 17 years old. Eligible encounter codes include billed CPT codes for sick (99202-99205, 99212-99215), well (99381-99384, 99391-99394), telephone visits (98966-98968, 99441-99443), or other counseling services.
-
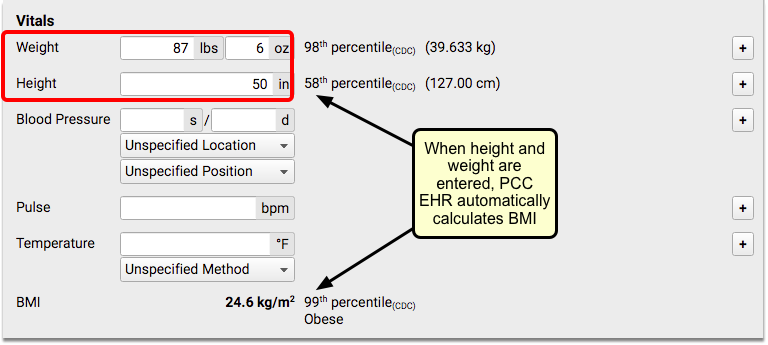
Numerator 1: PCC EHR calculates the first numerator of this measure by counting all of the patients in the denominator who had a height, weight, and BMI percentile recorded at least once during the measurement period. To meet this measure, track each patient’s height and weight (on the same day) during eligible encounters. This measure does not reference ICD-10s, or SNOMED codes.
-
Numerator 2: PCC EHR calculates the second numerator of this measure by counting all of the patients in the denominator who received counseling for nutrition during a visit that occurred within the measurement period. To indicate that counseling for nutrition was completed, you can use the following codes:
-
Numerator 3: PCC EHR calculates the third numerator of this measure by counting all of the patients in the denominator who received counseling for physical activity during a visit that occurred within the measurement period. To indicate that exercise counseling was completed, you can use the following codes:
-
Exclusions and Exceptions: This measure will exclude children who are diagnosed as being in hospice care, as well as patients who have an active diagnosis of pregnancy during the measurement period.
| Code Set | Code | Description | Notes |
|---|---|---|---|
| SNOMED | 11816003 | Diet education | Link this code to a nutrition counseling screening order |
| SNOMED | 441041000124100 | Counseling about nutrition | Link this code to a nutrition counseling screening order |
| SNOMED | 61310001 | Nutrition education | Link this code to a nutrition counseling screening order |
| Code Set | Code | Description | Notes |
|---|---|---|---|
| SNOMED | 281090004 | Recommendation to exercise | Link this code to an exercise counseling screening order |
| SNOMED | 304507003 | Exercise education | Link this code to an exercise counseling screening order |
| SNOMED | 41028900 | Exercises education, guidance, and counseling | Link this code to an exercise counseling screening order |
Recommended PCC EHR Configuration for CMS 155 Weight Assessment and Counseling
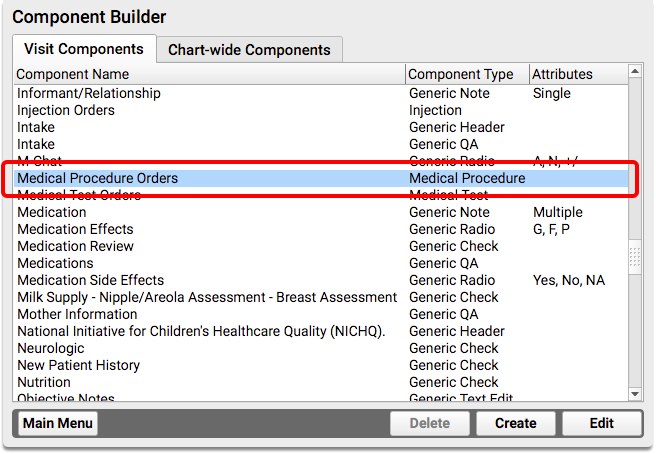
In order to chart counseling for nutrition or physical exercise, your practice can create screening orders and add the specified SNOMED-CT procedures to those orders. Then you can add the orders to chart notes so they are easy to select at every visit.
For a step-by-step procedure on how to add codes to orders and add specific orders to chart notes, read Use Orders to Track Measures for Mandates.
Configure Your Nutrition Counseling Order
Create or edit a screening order for nutrition counseling.
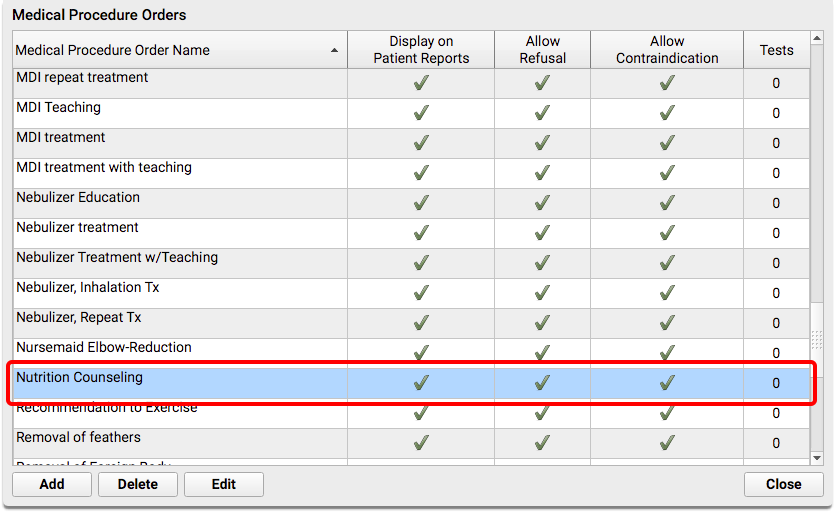
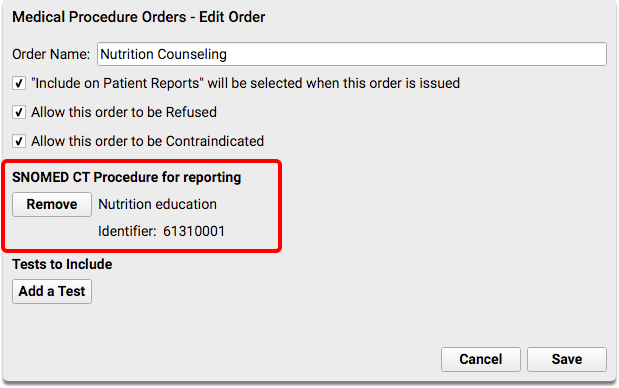
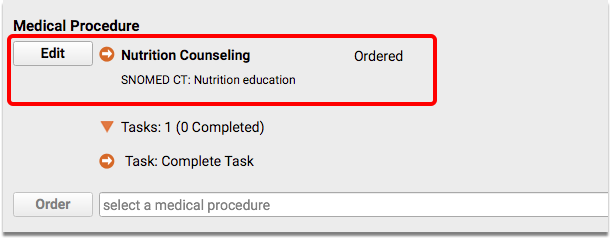
For the nutrition counseling order, you should select SNOMED-CT code 61310001, “Nutrition education”.
Configure Your Physical Activity Counseling Order
Create or edit a screening order for physical activity counseling.
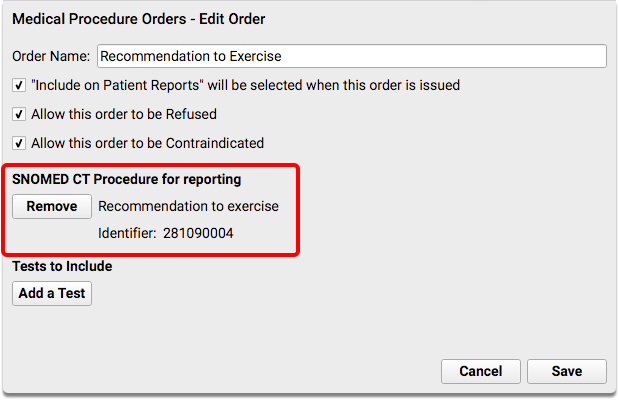
For the physical activity counseling order, you should select SNOMED-CT code 281090004, “Recommendation to exercise”.
Use the Specified SNOMED Codes: Please note that the 2018 ICD-10 code Z71.82, “Exercise counseling” will not work with PCC EHR reporting.
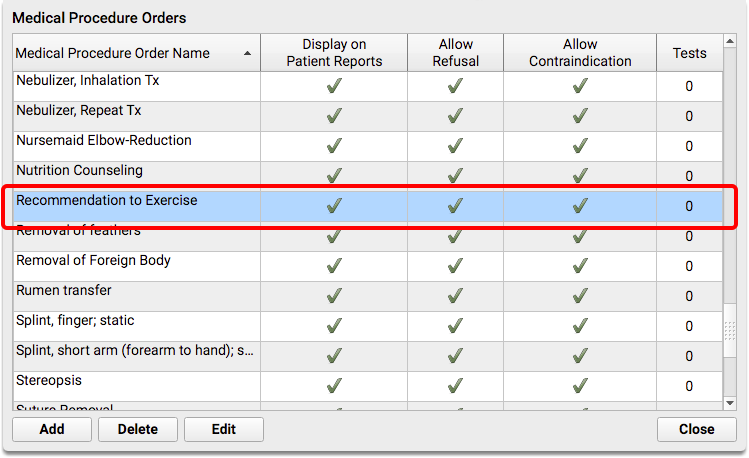
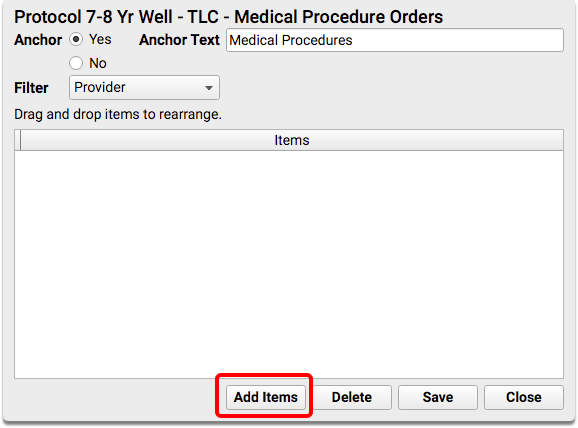
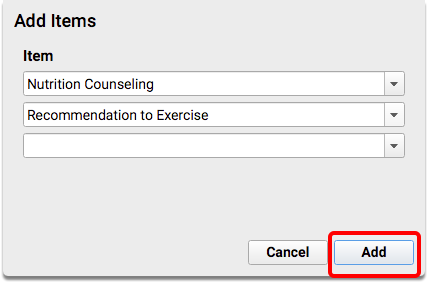
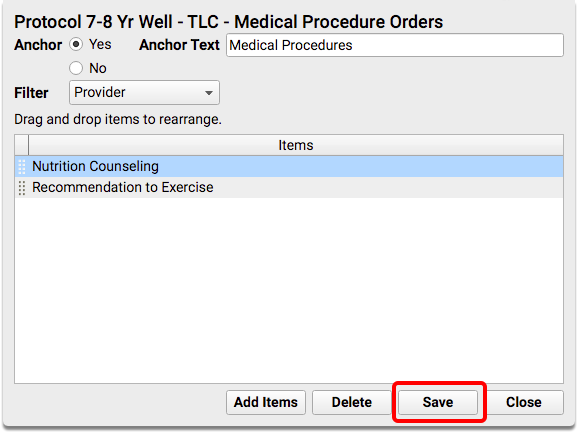
Add Nutrition and Physical Activity Counseling Orders to Your Chart Note Protocols
After you create the new orders, you can add them to chart note protocols to make them easier to order. Your clinicians will then see the “Nutrition Counseling” order, for example, on every chart note.
For detailed instructions on how to add orders to a chart note protocol, read Use Orders to Track Measures for Mandates.
For each protocol, find or add the Screening Orders component, and then add the nutrition and physical exercise orders.
Recommended Charting and Workflow for CMS 155 Weight Assessment and Counseling
Collect height and weight during normal office visits, well exams and other appropriate visit types.
When appropriate, order your practice’s nutrition and/or physical activity counseling screening order.
When you are finished charting, remember to click “Bill” and select an appropriate visit encounter code. In addition to billing, the visit encounter code is used to calculate the CQM.
