What is a Claim ID Number?
Every insurance claim in your PCC system has a unique identification number. The number appears in various reports and programs, and you can use it to improve claim tracking and payment posting.
Claim ID Creation and Tracking
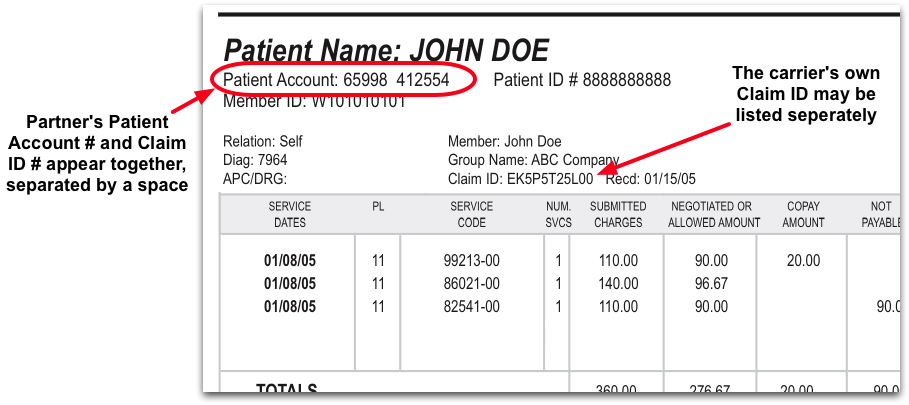
As soon as a claim is submitted, your PCC system creates a unique claim ID. The number is submitted on the claim, along with the patient’s account number. It should appear on all resulting claim communication, though some insurance carriers have trouble distinguishing the numbers.
When you work to track down a problematic claim, you can see the claim ID number in the Claims tool, when you read ERAs as well as on many other screens.
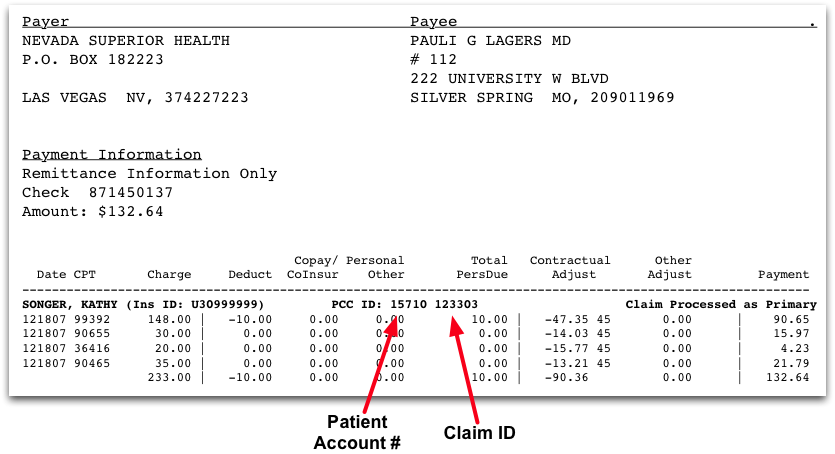
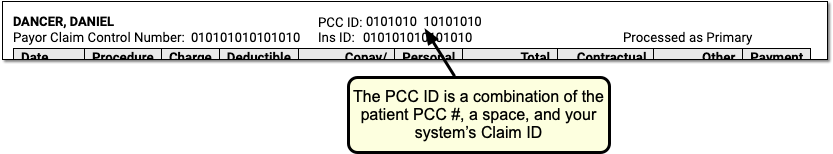
Find the Claim ID on Reports and EOBs
While your PCC system can identify the Claim ID quickly and easily, different reports and EOBs may display the claim ID in different ways. Below are some examples.
Use the Claim ID to Post Payments and Adjustment
For most claims, your PCC system automatically identifies the claim ID and can post incoming payments and adjustments automatically. When you need to post a payment or adjustment manually, you can use the claim ID to select it quickly.
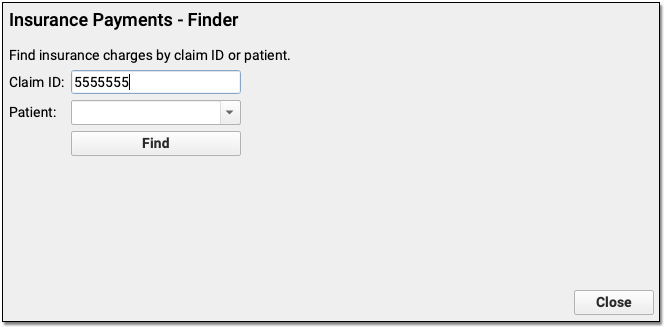
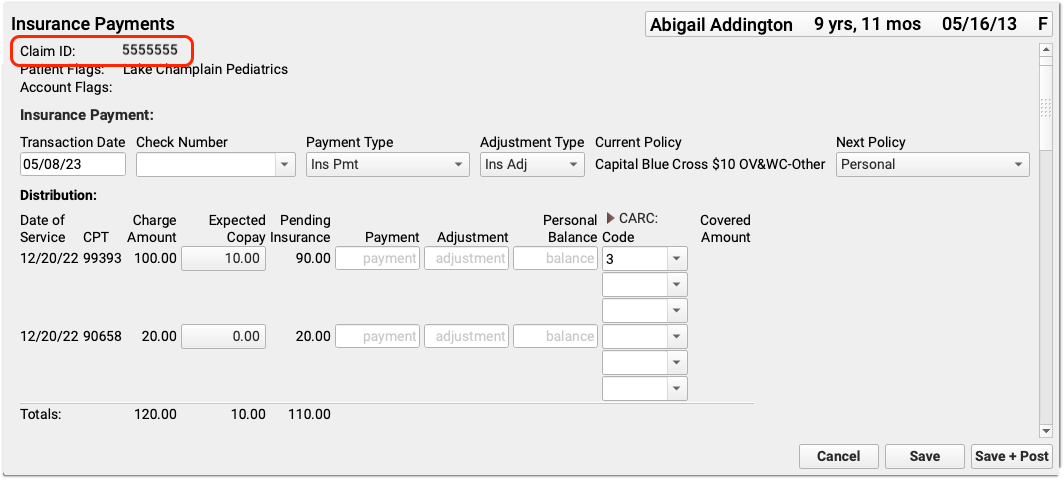
If you can not find a claim ID for some reason, you can also search by patient name, birthdate, phone number, or other information. See Post Insurance Payments to learn more.
