Reciprocal Billing Arrangements, Locum Tenens, and Incident-To Billing
When a clinician sees a different physician’s patient, there are a few limited circumstances that would allow the encounter to be billed under the primary physician. Read below for a brief overview of the conditions and considerations for each model.
Contents
Reciprocal Billing Arrangements and Fee-For-Time Compensation Arrangements
CMS now refers to short-term substitution for an absent physician as a “Reciprocal Billing Arrangement” or a “Fee-For-Time Compensation Arrangement”. CMS no longer uses the term “Locum Tenens”.
Various state, Medicaid, and carrier requirements may restrict how and when this billing arrangement is allowed, and a practice should consult with specific payors to understand what is required.
For example, a specific Medicaid plan might designate a time period limit, specify how the claim should be billed (a primary physician receiving payment for a substitute’s services), and what coding modifiers must be reported. Q5 and Q6 are required for Medicare, for example, which designate either a reciprocal billing arrangement or fee-for-time compensation arrangement.
Incident-To Billing
Under limited circumstances, an NP/PA or other clinician can bill under a physician’s name even though the physician did not participate in the encounter.
CMS limits this strictly to when the clinician carries out plans that the physician has written. (No new patients, no new problems!)
Additionally:
- The staff member must be employed by the physician directing the care.
- The supervising physician must have documented an order for the service rendered.
- The person administering the care must be qualified: the service is within their scope of practice as defined by state regulations.
In addition, various state, Medicaid, and carrier requirements may restrict how and when this billing arrangement can occur, and a practice should consult with specific payors to understand what is required.
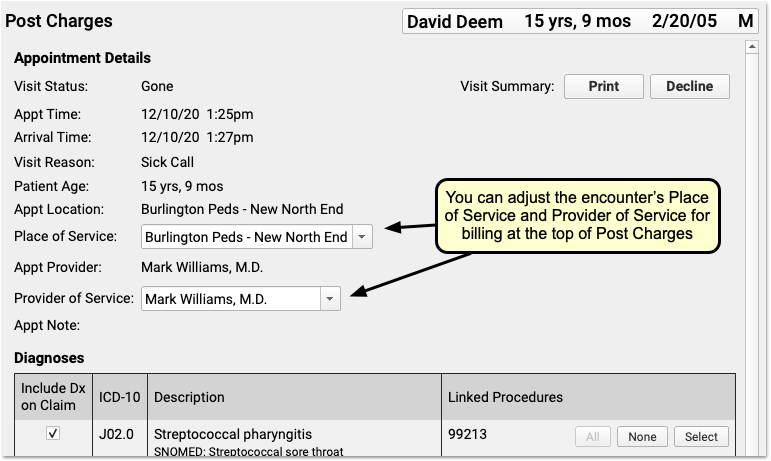
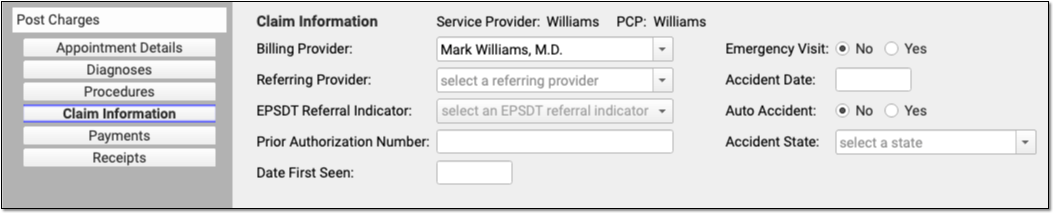
Change Provider of Service or Billing Provider When You Post Charges for Encounters
When posting charges in PCC EHR, users can adjust the Provider of Service and the Billing Provider separately. These providers can also be different from the scheduled Appointment Provider.
To learn more about adding a new user and clinician to your PCC system, read Add and Configure a New Clinician to Your PCC System.
To learn more about posting charges, read Post Charges in PCC EHR
Contact PCC for help adjusting billing configuration as needed.
