PCC 10.0 Migration Considerations
The PCC 10.0 release includes new features that may need configuration and for which you may want to do extra planning or training. Read below to learn more, and share relevant details with your physicians and staff.
Read the PCC 10.0 Release article for complete details on these features.
Contact PCC Support for help implementing features in PCC 10.0.
Contents
- 1 Set Chart Export Permissions
- 2 Add, Move, or Remove the Insurance Eligibility Component
- 3 Consider Limitations of Autoposting in PCC EHR 10.0
- 4 Configure Your Autopost Payment and Adjustment Types
- 5 Adjust Permissions for Claim Configuration and Working with ERAs
- 6 Review Your “No Show” Workflow and Billing Procedures
Set Chart Export Permissions
The Chart Export tool in PCC 10.0 makes it easy to export sensitive information that could harm patients, their family members, and your practice if shared inappropriately. As a result, it is protected by a new permission.
Nobody at your practice will receive the Chart Export permission with the PCC 10.0 update. An authorized user at your practice must enable this permission for the appropriate user roles – or create a new role – before anyone can start using the new tool.
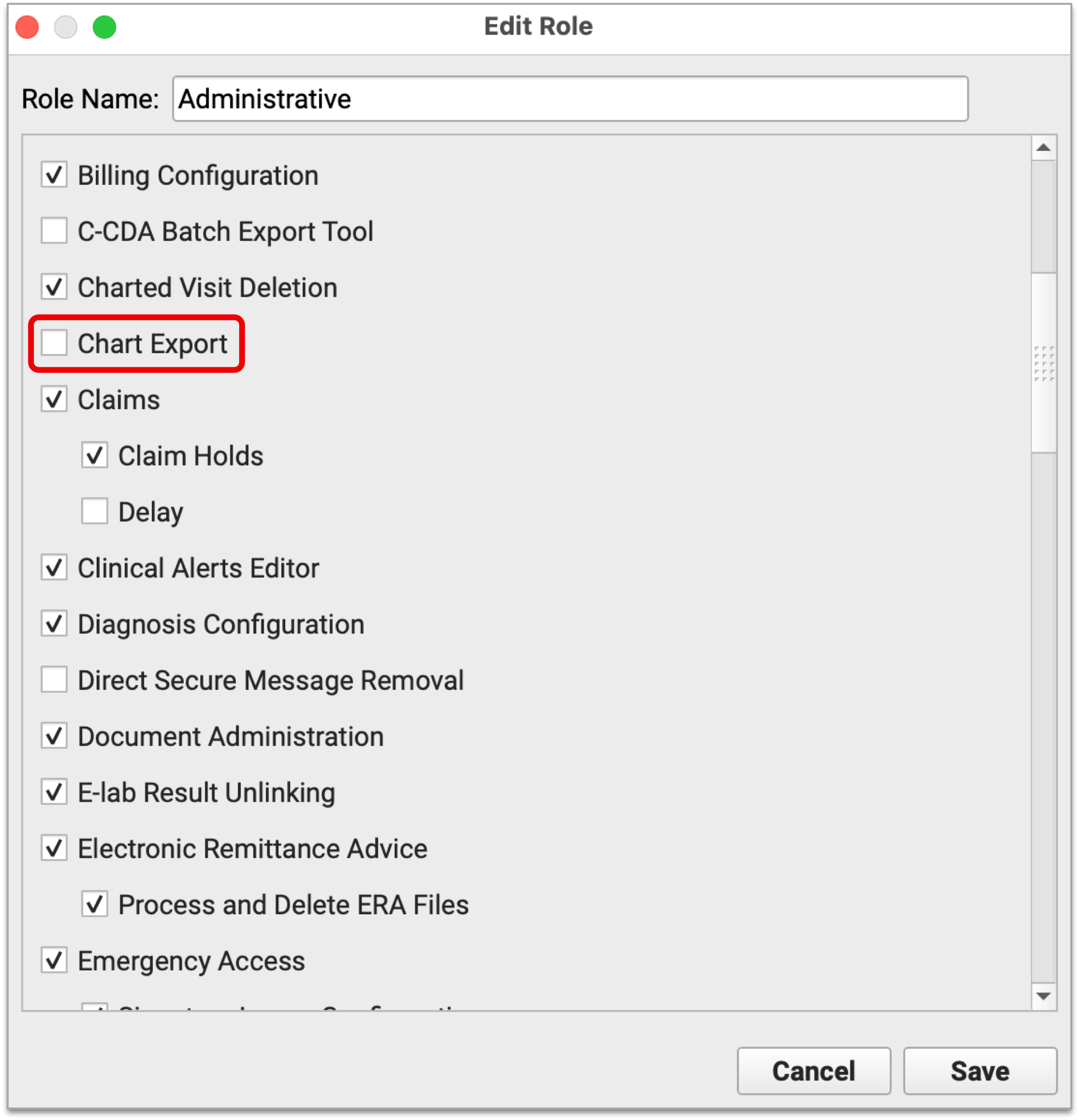
To learn more about user roles and permissions, read Set User Roles for Permissions and Security.
Add, Move, or Remove the Insurance Eligibility Component
After your PCC 10.0 update, your practice may want to move the Insurance Eligibility component on your Patient Details protocol and/or add the component to other screens in PCC EHR.
The PCC 10.0 update automatically adds the Insurance Eligibility component to the top of your Patient Details window.
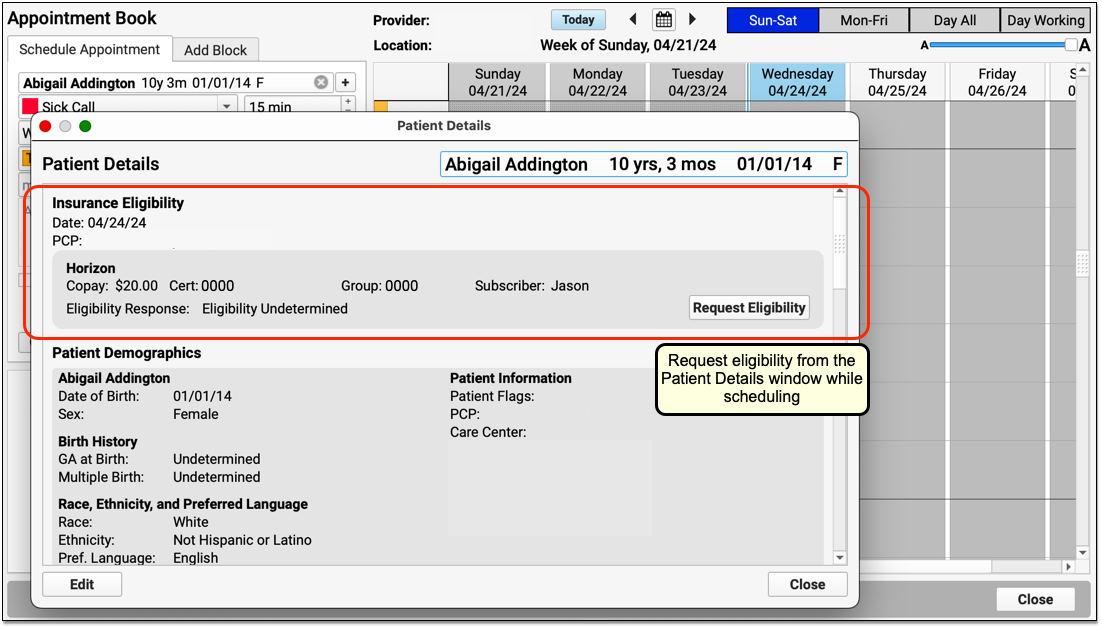
You can use the Protocols Configuration tool to move the component down to a new location in the window, remove the component, or add the same component to the Demographics section of the patients chart or other locations.
The Insurance Eligibility component acts differently depending on where it appears. It requests eligibility information for today’s date when it is not associated with an encounter. When the component appears in Patient Check-In or a chart note, for example, it uses the date of the encounter.
Consider Limitations of Autoposting in PCC EHR 10.0
Autoposting in PCC EHR 10.0 is a new feature, and PCC has received feedback and found issues which may need addressing before the tool meets your practice’s needs.
-
Provider Level Adjustments: In the rare circumstance when an EOB includes provider level adjustments that are not associated with an encounter, PCC EHR does not display them in the Electronic Remittance Advice tool. You can review these details in the previous ERA Reports tool. PCC plans to improve how these appear in PCC 10.1.
-
Specifying the Transaction Date: When you autopost in PCC EHR 10.0, the payor’s remittance date is used as the transaction date for the payment. While this typically corresponds to when the funds were transferred to your bank, many users have requested the ability to specify a custom transaction date when they autopost. PCC plans to include this functionality in PCC 10.1.
-
Autopost's Copay Changing Behavior May Interfere With a Medicaid Work-Around: When you autopost an ERA, PCC EHR can automatically change the expected copay on a charge to match the copay reported back by the payer. This is useful when your practice did not have the correct copay amount on file for the family, but it may interfere with a common work-around used by some practices. When a patient has Medicaid as a secondary policy, practices sometimes assign them a $0 copay version of their primary plan to avoid billing them for the copay later. Since autoposting in PCC EHR tries to “fix” incorrect copay amount, it may undo this work-around. PCC is considering solutions for this issue in an upcoming release.
-
Matching Modifiers: In rare cases where your practice always uses a modifier for a given procedure, the ERA tool in PCC EHR may not be able to recognize the root code. These items will appear as payment exceptions for manual attention. PCC will address this issue in PCC 10.1.
Configure Your Autopost Payment and Adjustment Types
When you automatically process ERAs in PCC EHR, what payment and adjustment types will PCC use?
You can review and update these types in Practice Preferences. By default, PCC will post payment types named “Ins Pmt” and “Ins Adj”. To post an insurance reversal, it will use an accounting procedure named “Insurance Takeback”.
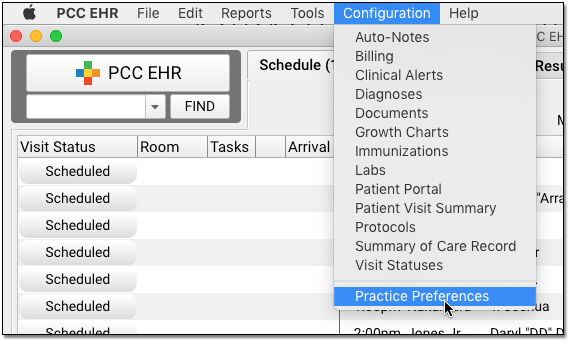
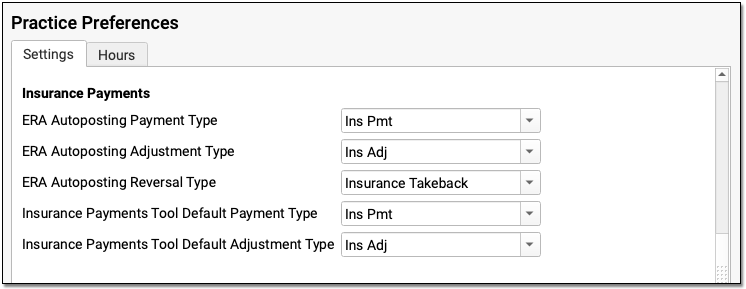
If you need to edit or adjust your available payment and adjustment types, you can do so in the Payment Types and Procedures tables in the Table Editor. Contact PCC for assistance.
Adjust Permissions for Claim Configuration and Working with ERAs
Your practice can control which users have access to new claim configuration options and ERA processing.
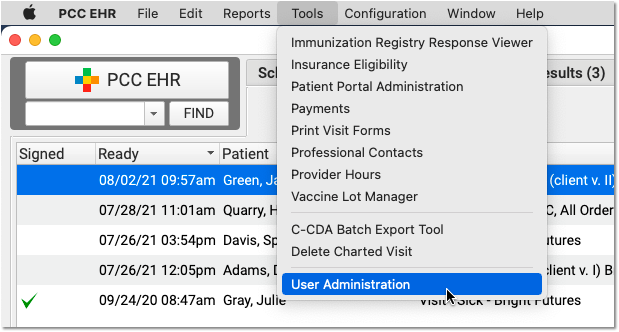
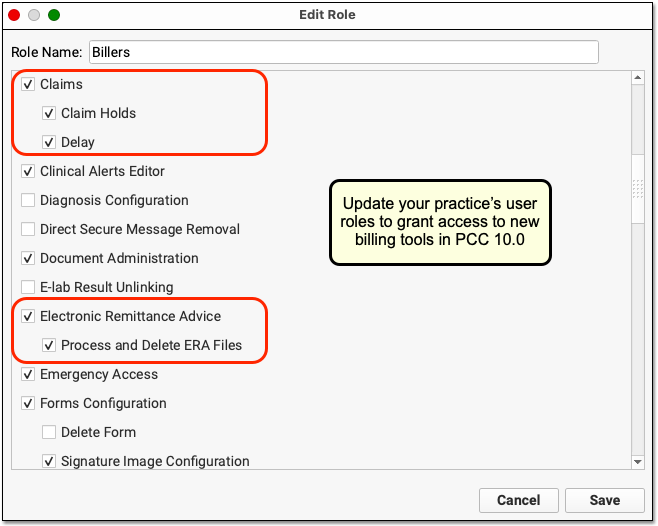
Your PCC 10.0 update will automatically grant access to ERA processing and ERA deletion to your practice’s administrative users. No users will be granted the ability to edit your practice’s claim delay. After your PCC 10.0 update, you can review these settings and grant appropriate users permission. Read Set User Roles for Permissions and Security to learn how.
Review Your “No Show” Workflow and Billing Procedures
The latest update to SNOMED-CT deprecates some common “missing a visit” descriptions: “Did not attend” and “DNA – Did not attend outpatient appointment” are no longer part of SNOMED-CT. Some pediatric practices use diagnoses to signal to the biller that the patient did not show up for the encounter. If your practice relied on those descriptions in the chart note to record no-shows, you may need to revisit your practice’s “no show” workflow.
Your practice can use PCC’s tools in various ways to record when a patient misses an appointment. For example, your front desk can mark appointments as missed and your biller can later use the Report Library to list all no shows and create administrative encounters to bill a fee. Reach out to PCC Support or the PCC Community to discuss options.
