Troubleshoot a Specific Rejection Snippet
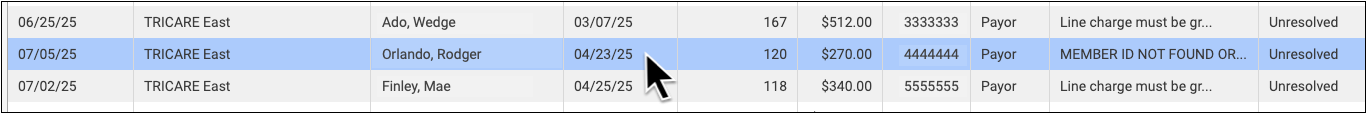
Double-click on a rejection to review more details.
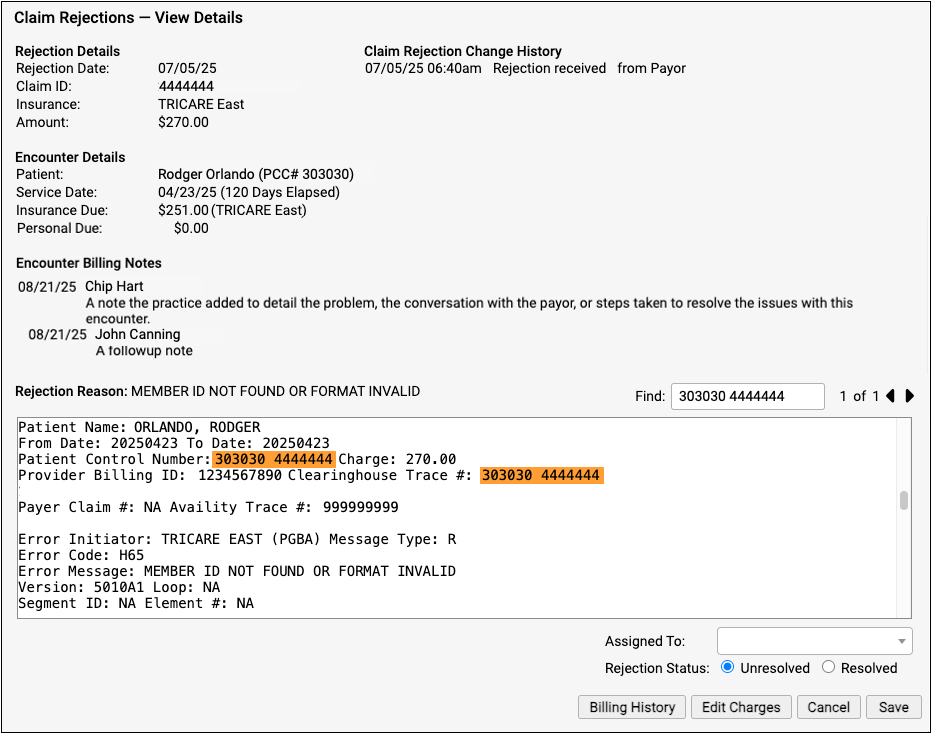
The Claim Rejections – View Details screen provides information and tools that will help you understand and respond to the rejection.
-
Rejection Details: The Rejection Details section indicates when your PCC system received the rejection, the claim ID indicated by the payer, the plan, and the amount on the claim.
-
Encounter Details: The Encounter Details section shows the patient, date of service, and how much is currently due from insurance and the family. If the “Insurance Due” amount is now $0.00, the rejection may already be resolved or else your practice may have changed the responsible party for the charges.
-
Claim Rejection Change History: Any time anyone at your practice assigns or changes the status of this claim rejection, it is logged in the Claim Rejection Change History.
-
Encounter Billing Notes: If you or someone at your practice has entered encounter billing notes (sometimes called “visit billing notes” or “oops notes”), the Encounter Billing Notes section will display those notes. If you’ve contacted the payor and submitted a claim multiple times, you can review your practice’s notes to better understand the history of the rejection.
-
Rejection Reason: When your PCC system receives the rejection from the payor or clearinghouse, it attempts to extract a reason summary from the data. That summary is listed on the screen as the “Rejection Reason”, and the complete rejection data file is shown so you can review it.
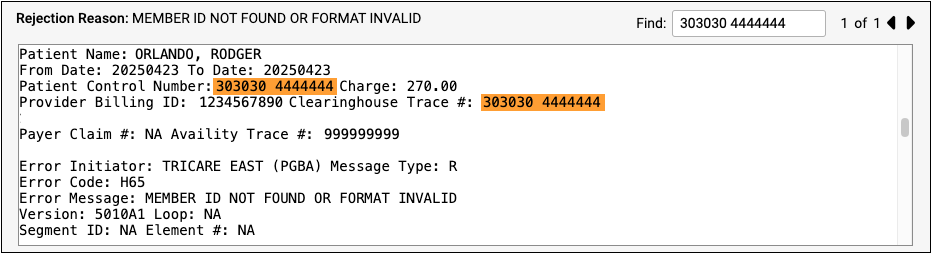
Different payors and clearinghouses send different types of electronic communication. A single file may include responses to many different claims, so the search field of the Rejection Reason is automatically filled with the Claim ID, making it easier to navigate the electronic file from the payor. If the claim ID appears multiple times in the electronic file, you can use the Find field’s next and previous buttons to review the details.
