Review Claim Rejections Worklist Snippet
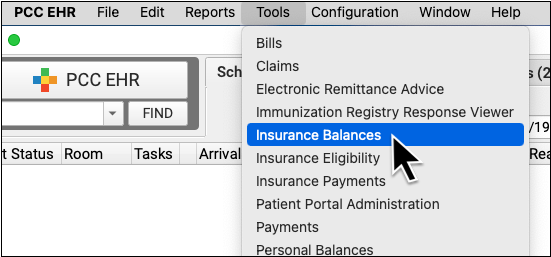
To review claim rejections sent to your practice from payors and clearinghouses, open the Insurance Balances tool and visit the Rejected Claims tab.
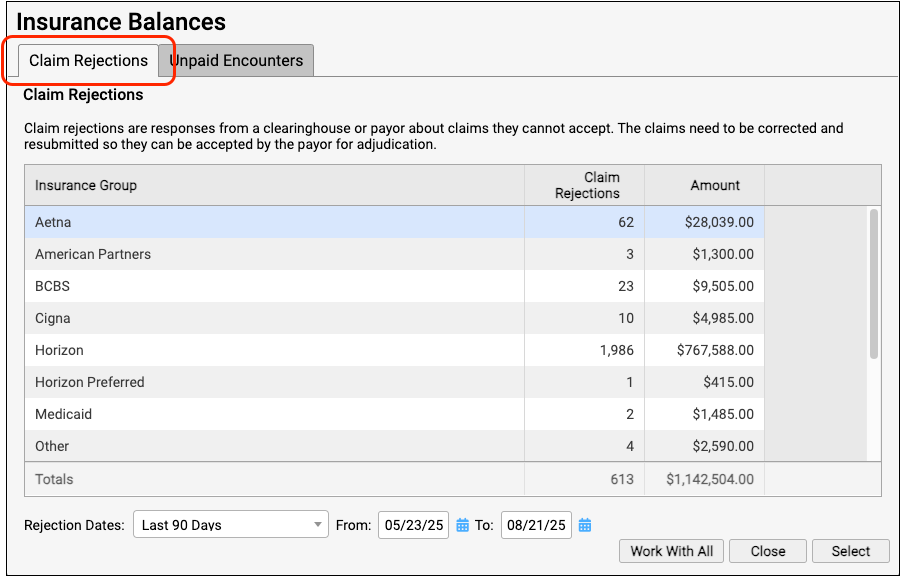
The Claim Rejections overview summarizes unaddressed rejections sent to your practice. Totals are aged and shown for each insurance group.
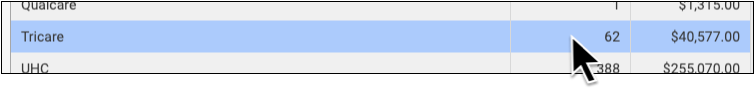
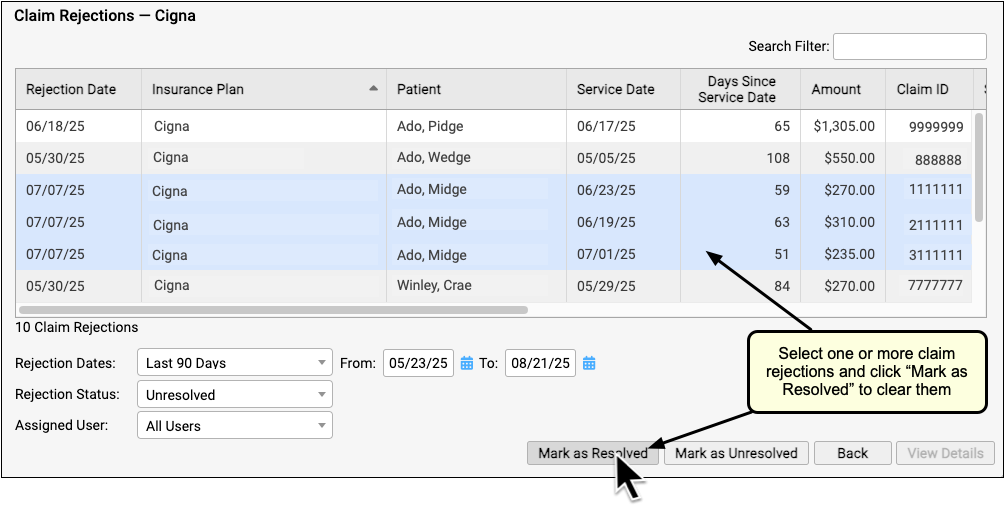
Double-click on a single insurance group or click “Work With All” to view the rejections worklist.
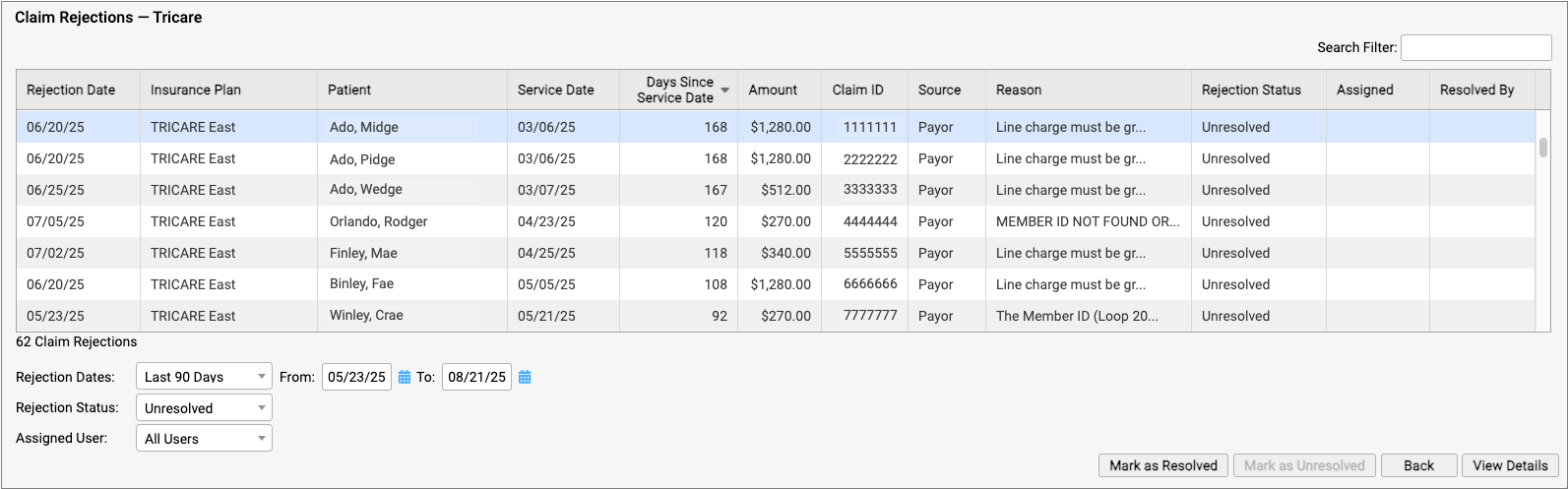
For each rejection, you can see key details about the rejection and the claim, including the number of days since the date of service and the rejection reason. You can also see a Rejection Status (which defaults to “Unresolved”) and whether the rejection is assigned to a user and who resolved it.
You can filter the list to isolate rejections you need to work on. You can select an age or enter a date range, limit the list to resolved or unresolved rejections, or filter by assignee. You can enter a search term in the Search Filter field to find rejections based on a patient name or claim ID, for example.
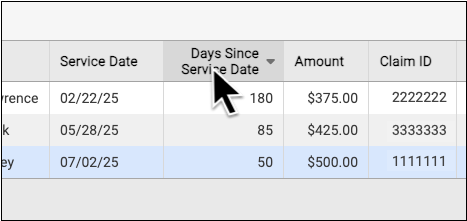
You can also sort the list by any column, making it easy to target rejections based on age or the amount on the claim.
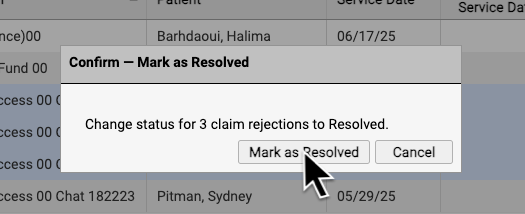
If you are certain a rejection or rejections are now resolved, you can select them and click “Mark as Resolved”.
By reviewing and resolving every claim rejection sent to your practice, you can ensure that no claims slip through the cracks.
Each Rejection is a Point-in-Time Response: Rejections are similar to email messages or other incoming communication. Your practice might handle a billing problem for an encounter using a different tool, and an encounter’s balance may already be paid off. The rejection from the payor remains on the Rejected Claims worklist for your review until you mark it as resolved.
