Post Insurance Payments and Adjustments
With PCC, you can automatically post most payments and adjustments sent to your practice as an ERA. Next, if a response requires manual attention or you receive a paper EOB, you can manually post the payments and adjustments.
Video: Watch Post Insurance Payments and Adjustments to learn more.
As you post insurance payments, you can enter CARC adjustments, record non-payment, pend the remaining balance to the next responsible party, and automatically queue up a subsequent claim or personal bill.
Contact PCC (1-800-722-7708, support@pcc.com) if you need to configure what ERAs require manual attention, need a custom payment type, or need help configuring your system for capitation checks, overpayments, or any other special circumstances.
Contents
Autopost Insurance Payments and Adjustments That Arrive on an ERA
Most ERAs that arrive on your PCC system do not require direct manual attention. Follow the steps below to autopost your incoming insurance payments and adjustments that arrive on electronic remittance advice (ERAs).
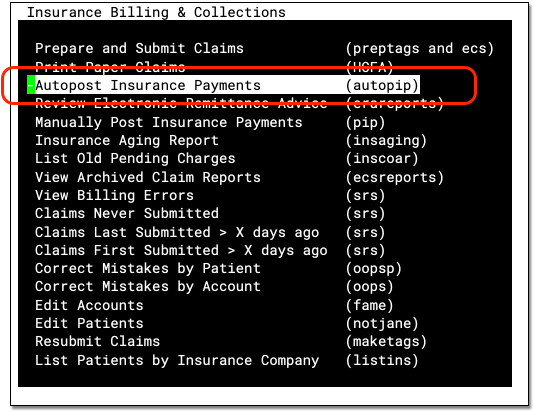
Run Autopost
Run Autopost from the Insurance Payments window in Practice Management.
Review Your List of ERA “Check” Files
PCC sorts incoming electronic EOBs into checks. If an ERA consists of multiple checks, it will be broken into individual entries. On the first Autopost screen, you will see a list of check files.
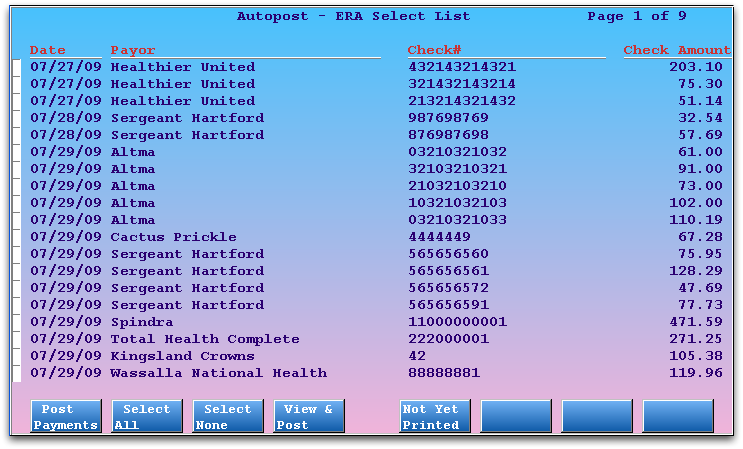
The oldest incoming check files are at the top of the screen. For each entry, you can see the Date of the ERA, the Payor, the Check # or reference #, and the total Check Amount.
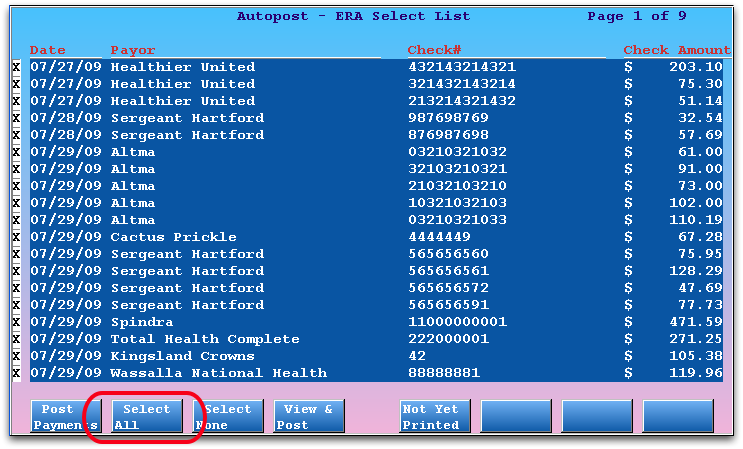
Select All (or Some) ERA Check Files and Press F1
Press F2 – Select All to select all the ERA checks your system has received, and then press F1 – Post Payments to continue. If you prefer, you can use the arrow keys and type X to select individual checks and then press F1 to continue.
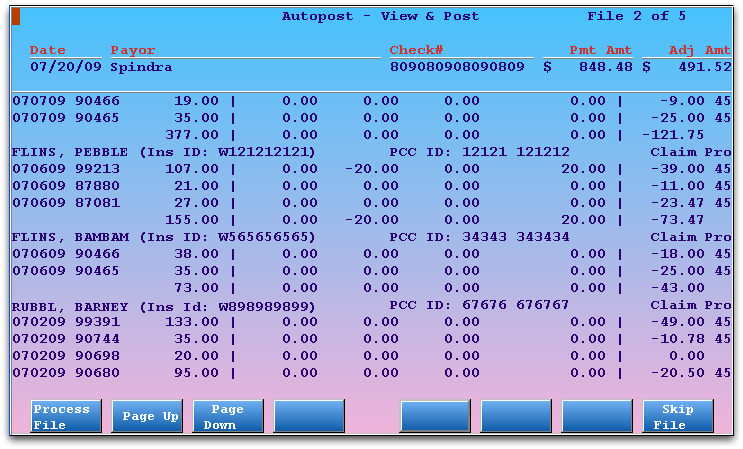
Work and Post "Check-by-Check": If you wish to review what will be posted for each check as you post the payments, press F4 – View & Post instead of F1. Autopost will show a brief summary of what will be posted for each check, and you can then post or skip each one.
Specify the Transaction Date for Payment
Next, choose whether Autopost should post the ERAs using the ERA’s issue date, today’s date, or a custom date. (You can configure your practice’s default in the Configuration Editor (ced).)
For example, you may want to specify that the transaction date should be the date you received the direct deposit. You can enter that date on this screen. Then press F1 – Process to continue.
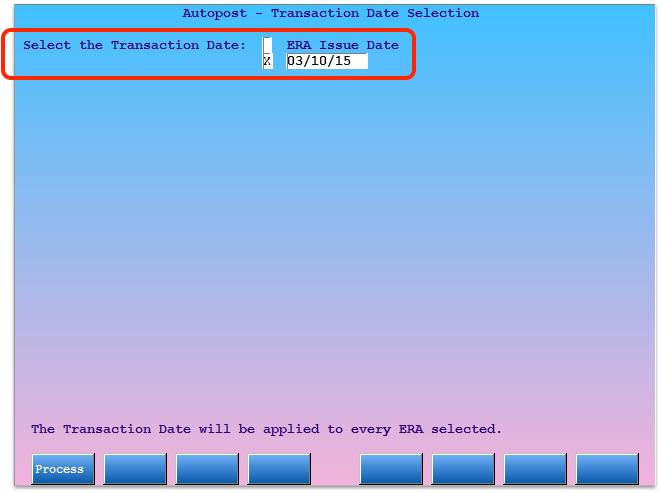
Posting Several?: If you selected several ERAs, your Transaction Date choice will be applied to each one. When you make your selection, make sure your choice is appropriate for all selected ERAs.
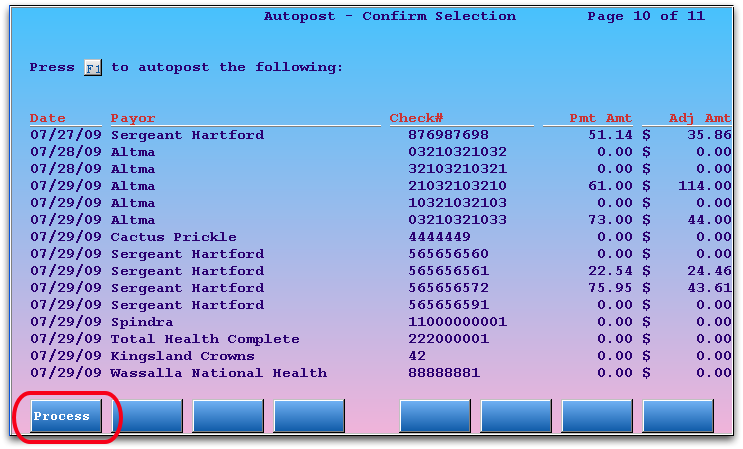
Review Your Selection and Press F1
On the Confirmation screen, double-check that you selected the correct checks and press F1 – Process to continue.
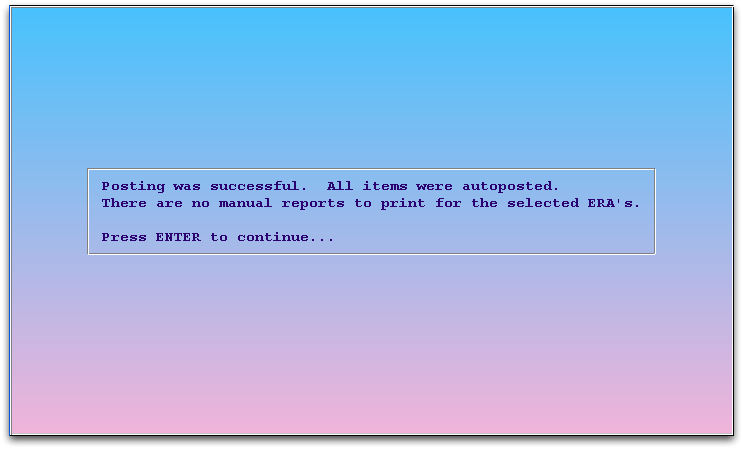
Press Enter and Quit
If all the payments and adjustments were ordinary, and no allowable amount was missed and everything matched the outgoing claims, you will be prompted to press Enter to return to the ERA Select List screen. You can then press F12 to quit autopip.
Review “Unpostable” Manual Items
If any encounter in the ERA does not match the claim you sent, or requires attention for a mismatched copay or other reason, then the Autopost program will not post payments and adjustments for that encounter. Instead, Autopost creates a Manual Post Report and you will be prompted to review or print that report.
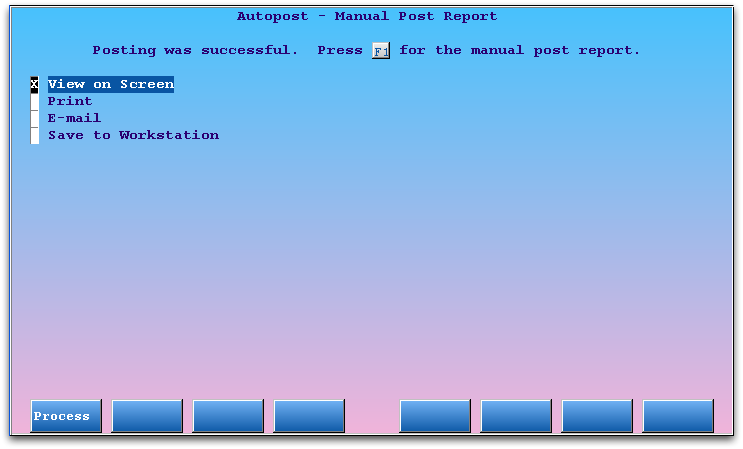
You can press F1 – Process to review the report immediately on the screen, or print, e-mail, or save it.
Why Do I Need to Print, E-Mail, or Save the Manual Reports?: ERAs may contain denials, reversals, and insurance interest payments. After Autopost finishes, any items in an ERA that autopip was unable to post are placed in a “Manual” report. A biller needs to review each Manual report and follow up on the included remittance information for the claims. For example, your practice may need to resubmit a claim or change the copay amount as you manually post the payments and adjustments.
Review Unprinted Manual Reports
If you or other users at your office do not print, e-mail, or save a copy of the Manual report, it will remain on a special list. Press F5 – Not Yet Printed from the main screen in autopip to review that list.
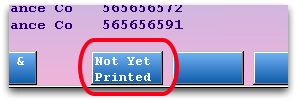
The Manual reports listed on this screen require attention. You can select multiple reports and then print, save, or e-mail them in order to remove them from this list.
Daily View: Press F7 – Daily View to review all Manual reports, whether they were printed/saved/e-mailed or not. You can use the Daily View history to find old manual reports and review daily Autopost activity.
When Needed, Use ERA Reports to Review Your Autoposting History
Run the erareports program to review all the Manual reports, details of all the autoposted items, or the full, original ERA check information. Read the section on ERA Reports for more information.
For more information about each screen in the Autopost program, read the Autopost Reference section below.
Manually Post Insurance Payments and Adjustments in PCC EHR
Use the Insurance Payments tool in PCC EHR to manually post payments, adjustments, and CARC information. Many ERAs can be posted automatically, but when a payor sends a paper EOB or an ERA with an unusual denial or adjustment, you can enter details manually while also reviewing and updating patient information.
Video: Watch Post Insurance Payments and Adjustments to learn more.
Open Insurance Payments
Open the Insurance Payments tool from the Tools menu in PCC EHR.
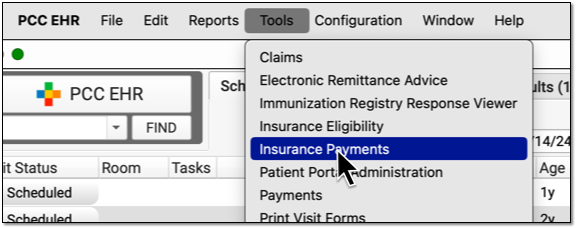
Your practice can configure which users have access to this tool.
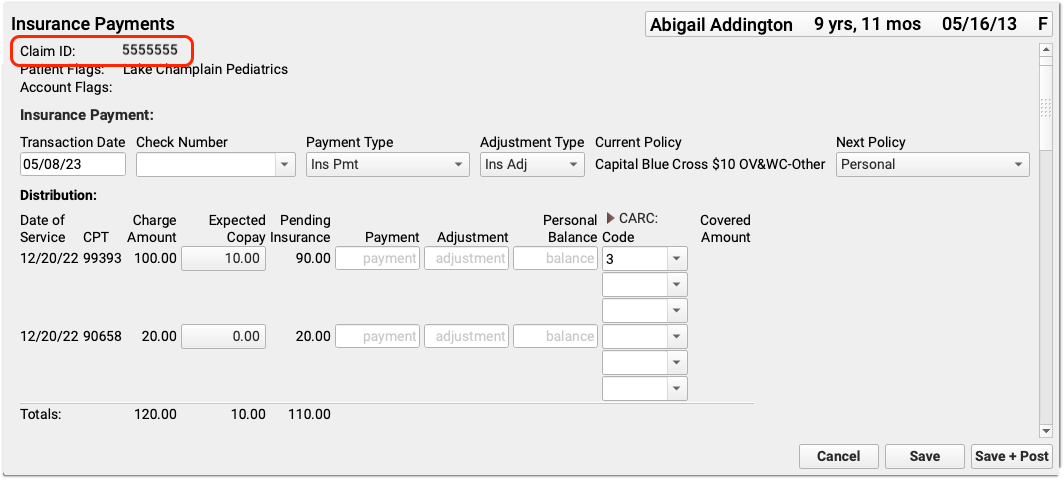
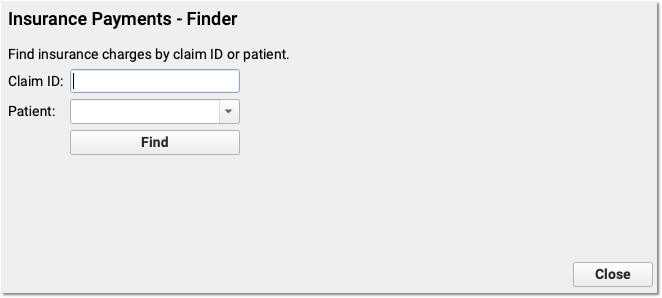
Enter the Claim ID
Enter a claim ID. When you press Enter or click “Find”, PCC EHR will find all charges from that claim that have a balance pending insurance.
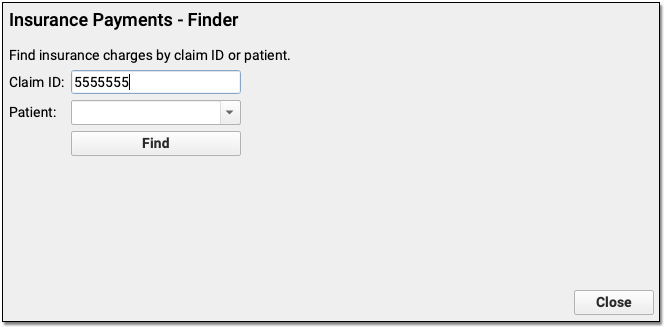
Optional: Find a Patient and Select an Encounter
If you don’t have a claim ID, you can first find a patient and then select an encounter.
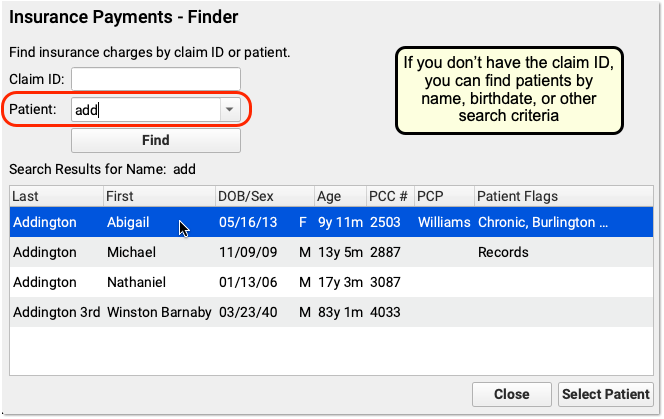
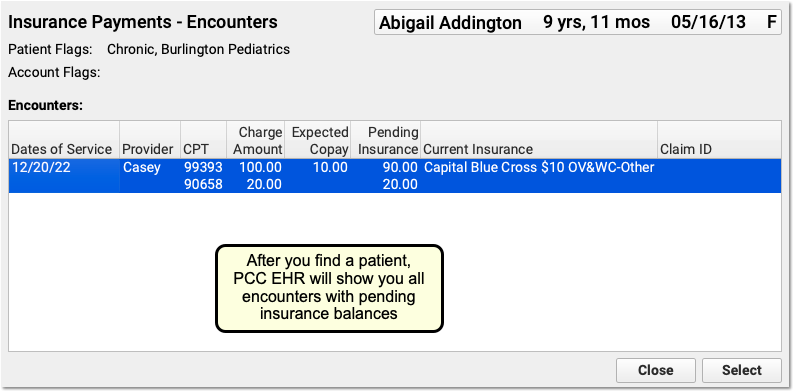
After you find a patient, PCC EHR will display all encounters with charges that have an amount due pending insurance. Double-click on an encounter to select it.
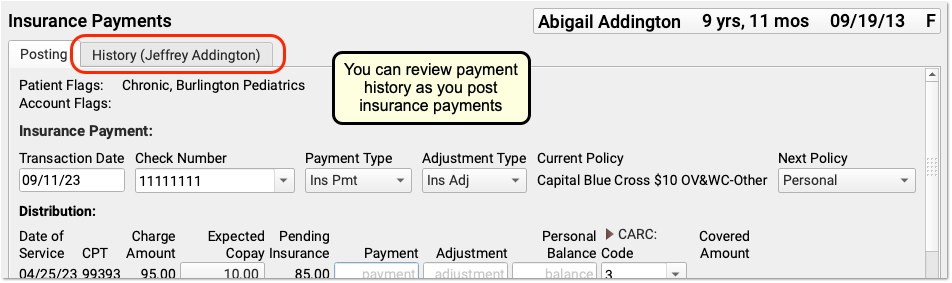
Optional: Review Payment Histories
As you work with a patient or an encounter in the Insurance Payments tool, you can click on an account history tab to review all past payments.
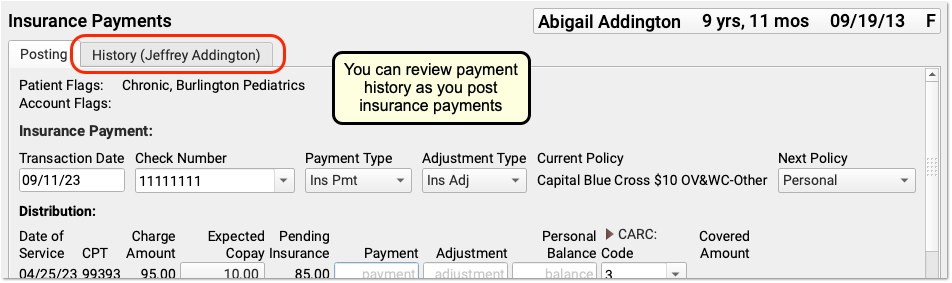
If a patient has had more than one billing account while at your practice, you may see more than one History tab.
Enter a Check Number, Review Other Details
Whenever you post payments, enter a check number.
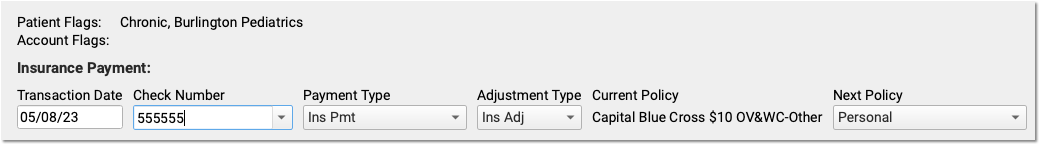
You can also use the fields at the top of the screen to: review patient and account flags, adjust the transaction date, change the payment or adjustment types, double-check that the payment came from the current policy, and change the next responsible party for any remaining amount due.
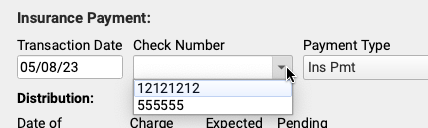
PCC EHR will remember and automatically select your most recent transaction date, check number, and payment and adjustment types.
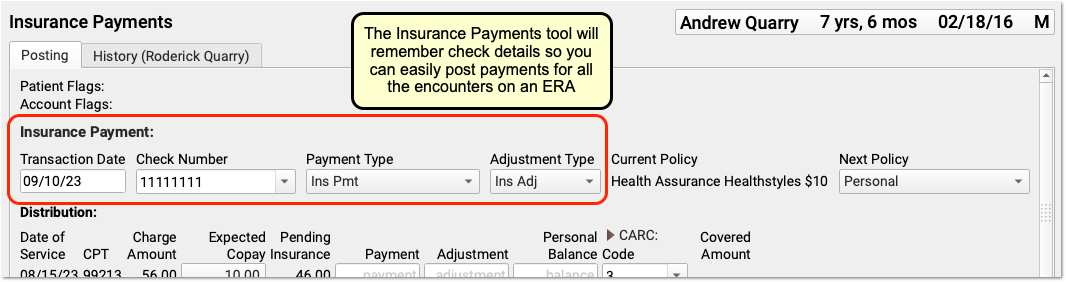
If you close and reopen the Insurance Payments tool, it will reset these values to their defaults. You can also select from your ten most recent check numbers.
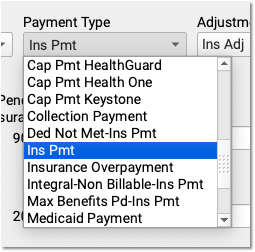
By default, PCC EHR posts payments and adjustments as “Ins Pmt” or “Ins Adj”. You can optionally select from your practice’s custom payment and adjustment types.
Enter Payment and Adjustment Amounts
For each charge on the encounter, enter the payment or adjustment amount found on the payor’s response.
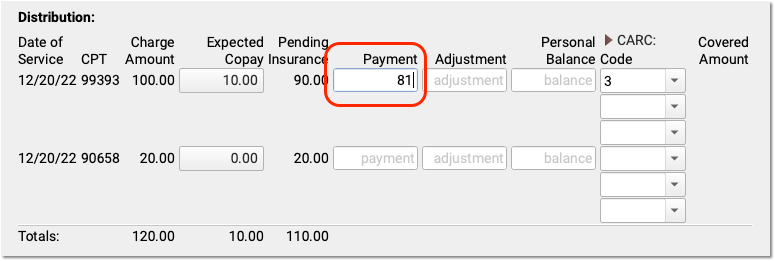
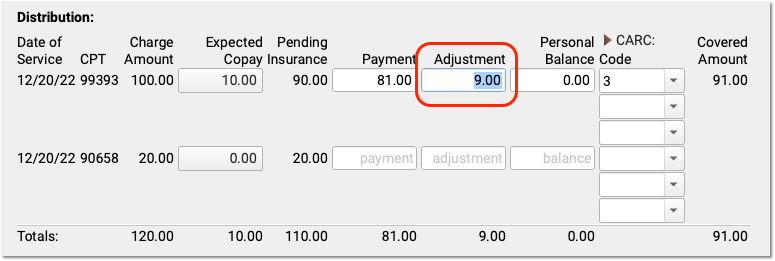
When you enter a payment amount and press Enter, PCC EHR will automatically calculate the likely adjustment amount. If the ERA indicates that the remaining balance is not adjusted off, you can make changes. You can also enter a remaining balance amount, and PCC EHR will recalculate the amounts for each field.
Optional: Change the Expected Copay Amount
Sometimes a claim is submitted with the wrong copay amount. The payor may respond with less or more than expected, and indicate the correct copay amount. You can change the expected copay for any charge as you enter payments and adjustments.
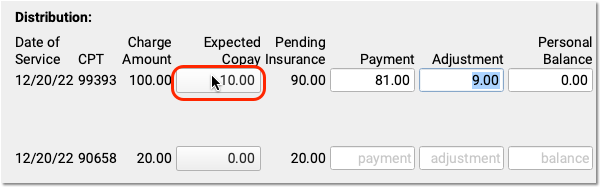
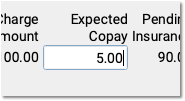
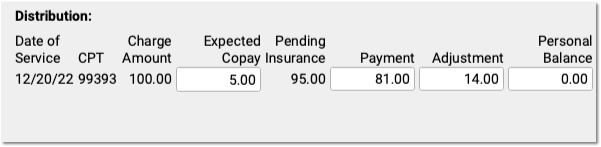
Automatic Calculation and Payment Relinking: When you change the expected copay, PCC EHR recalculates the adjustment amount on the screen for you. Also, if the family already paid the copay, then when you save and post, PCC EHR will automatically apply that payment correctly and (if appropriate) credit the account. For example, if a parent already paid $10 and now only $5 is expected, the remaining $5 will be a credit on their account.
Enter CARC Codes, Groups, and Amounts
As you enter payments and adjustments, you can also add Claim Adjustment Reason Code (CARC) information.
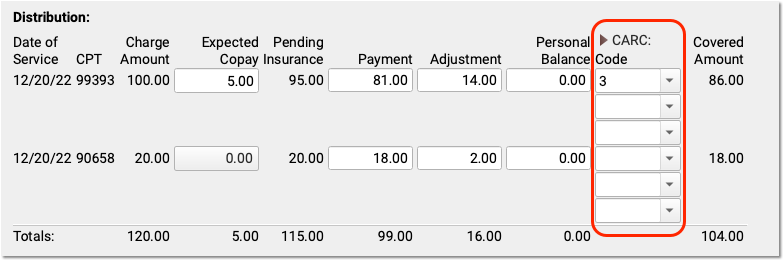
Payors use CARC codes, groups, and amounts to explain the adjudication of a claim. This information can be important for families as well as when you need to submit a secondary (or tertiary, etc.) claim.
When the next responsible policy is “Personal”, PCC EHR displays only the first CARC field by default, as shown above. If the patient has additional policies, however, then three Code, Group, and Amount columns will appear by default. You can click the CARC field label disclosure arrow to show or hide these extra CARC fields at any time.
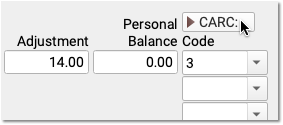
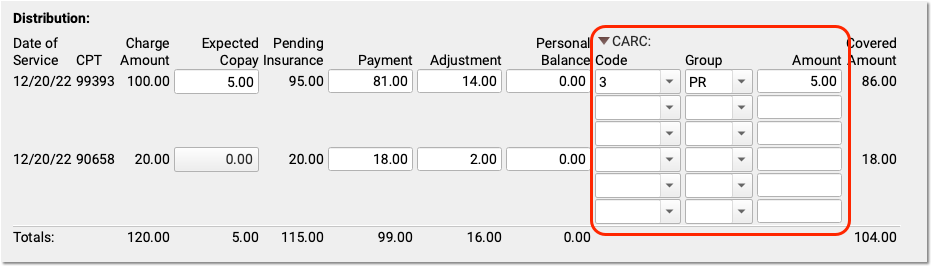
Automatic Copay CARC: If a copay is expected for a charge, PCC EHR automatically adds the CARC code “3” for “Co-payment amount”, with a Group code of “PR” and the amount of the expected copay as the adjustment amount.
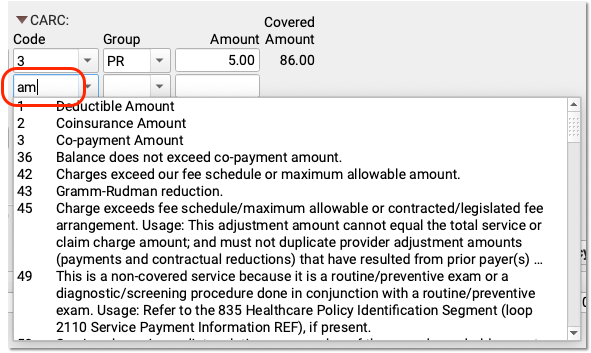
You can enter additional CARCs, and even search for a CARC adjustment using text from the adjustment reason, which typically appears in the payor’s response.
CARC Adjustments and Insurance Payments May Not Exceed the Charge Amount: CARCs explain adjustments. For that reason, the CARC amounts for a charge cannot exceed the original charge amount minus payments. PCC EHR will prevent you from entering more than the total possible amount, as that could result in a rejected claim from a secondary payor.
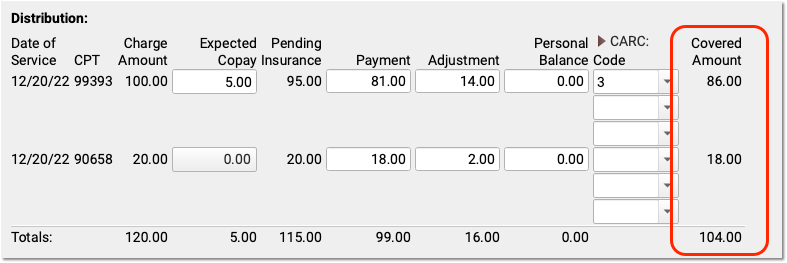
Optional: Review Covered Amount and Negotiated Rate
After you enter payments and adjustments, you can see the amount of the charge that the payor adjudicated as “covered” in the Covered Amount column. This displays the original charge amount minus adjustments.
If your practice tracks insurance contracts in PCC, and you’ve entered allowable amounts for these procedures for this insurance, then you will also see a “Negotiated Rate” column to the right.
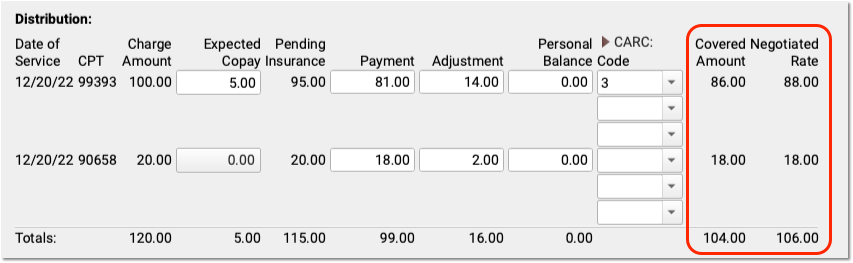
You can quickly compare the Covered Amount with your practice’s Negotiated Rate.
Optional: Review and Update Policies, Account Demographics, and More
As you enter payments and adjustments, you can scroll down to review patient policies, patient and account demographics, account balances, and account notes.
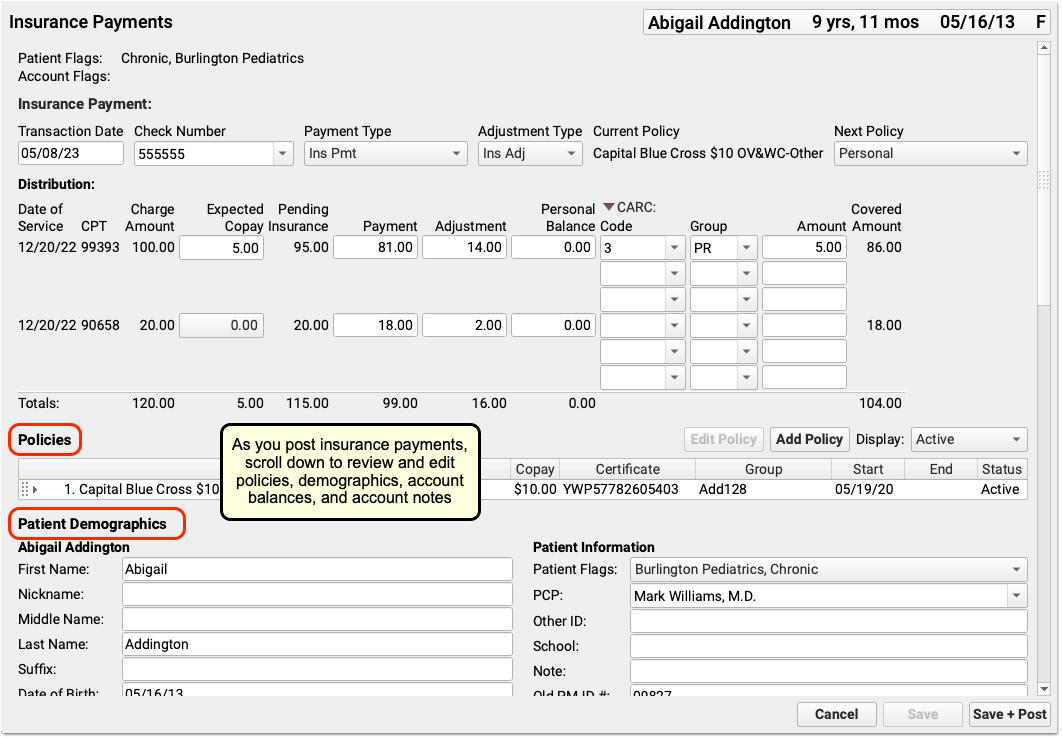
Use these components to update the patient’s policies, contact the family, or add a note explaining issues with the encounter.
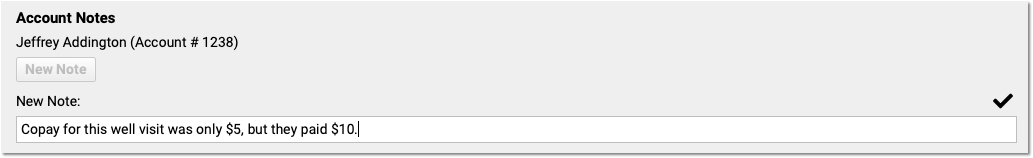
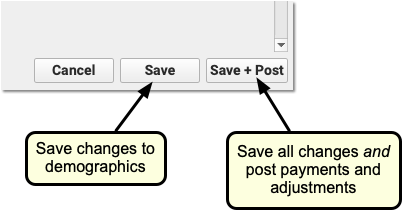
As you work, click “Save” to save patient and account demographics. Policy changes and Account Notes save automatically, but changes to other fields won’t be saved until you click “Save” or “Save + Post”.
Double-Check the Next Policy
Is there a remaining amount due on the charges for this encounter? Before you save and post payments and adjustments, PCC recommends you double-check the next policy, which indicates the next responsible party for these charges.
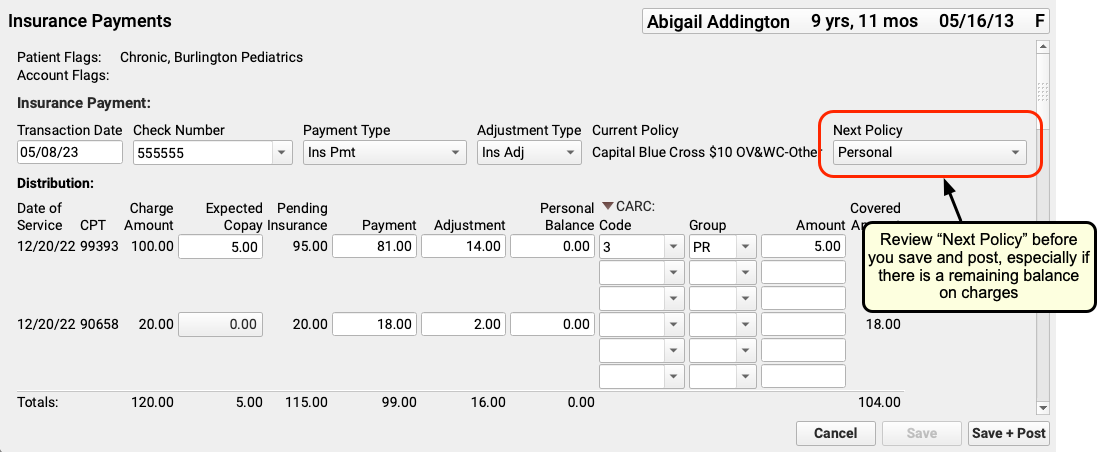
If the next policy is a payor, then PCC will automatically queue up a claim when you save and post your payments and adjustments. If it is “Personal”, then the remaining amount will become a personal balance.
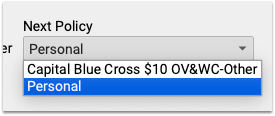
You can change the next policy. For example, if you added a new patient policy to the Policies component, you can select that new policy. When you save and post, PCC EHR will queue up a claim for the remaining encounter balances.
Click “Save + Post”
When you click “Save + Post”, PCC enters the payments and adjustments into your system, saves any changes you made to demographics, updates balances, and queues up a claim for the next insurance if appropriate.
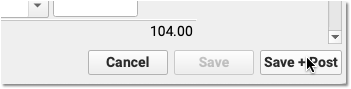
PCC EHR will return you to the first screen of the Insurance Payments tool so you can continue on to the next encounter.
Review Posted Insurance Payments and Adjustments
After you post insurance payments and adjustments, where do they appear?
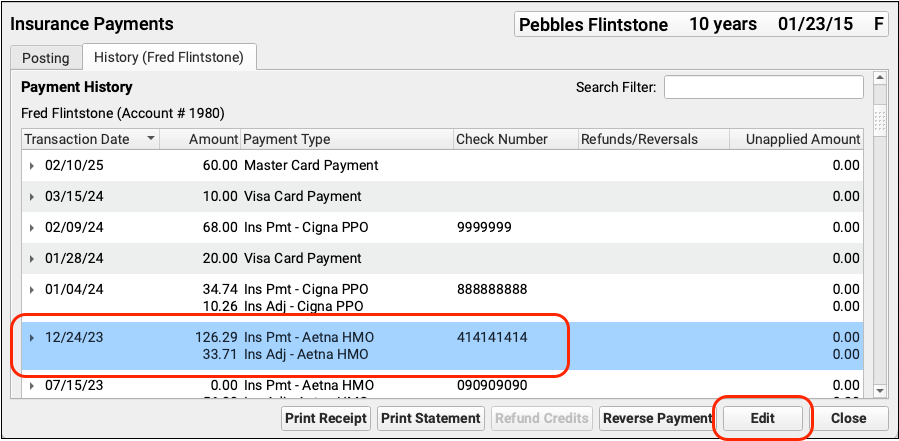
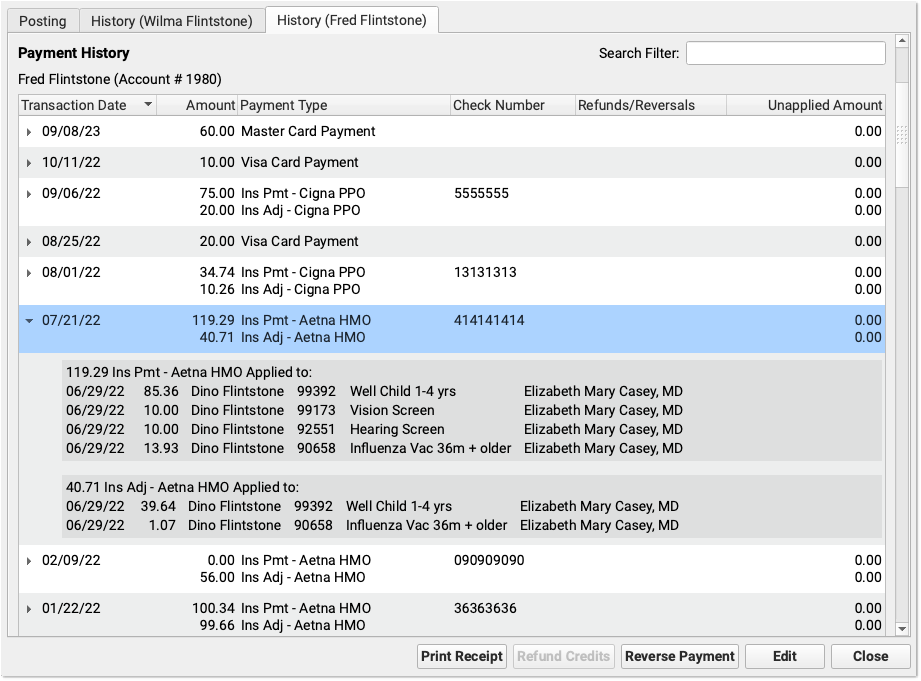
Review An Account’s Payment History
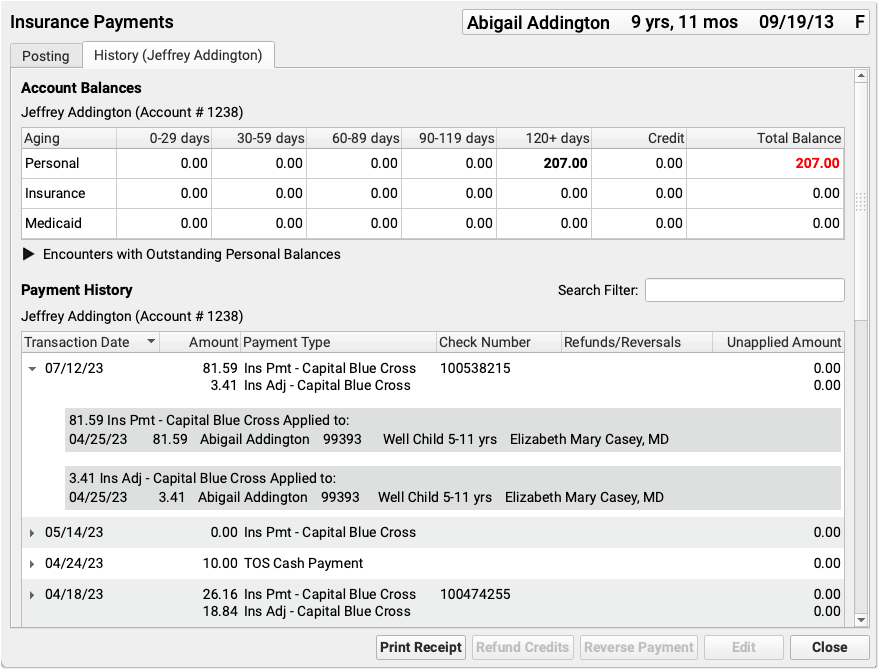
Click on the History tab in the Insurance Payments tool to review the complete payment history for the patient’s billing account.
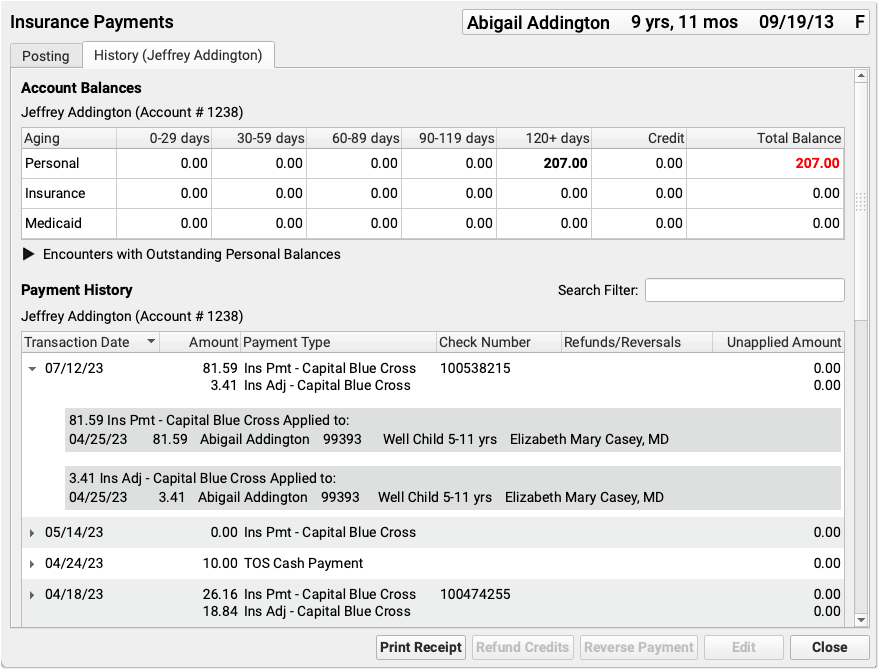
If a patient has had more than one billing account, you may see more than one History tab.
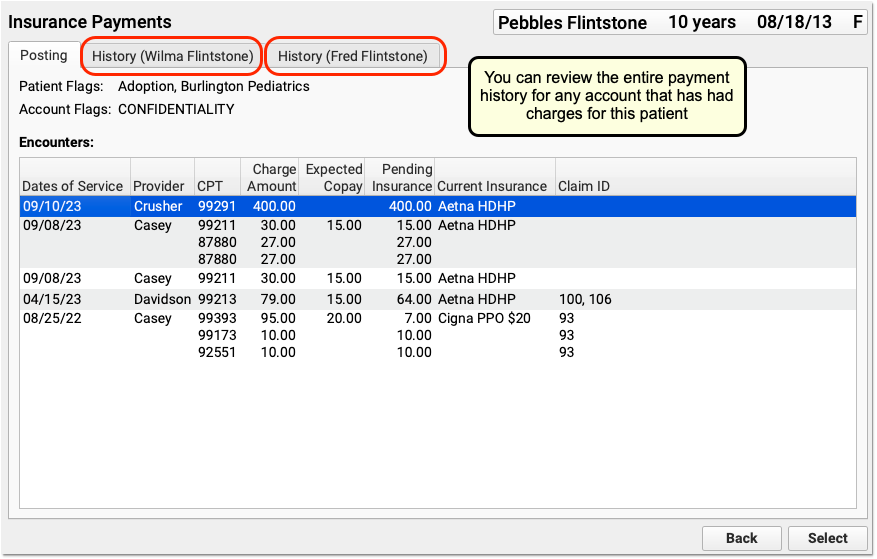
You can review the entire payment history for any account that has had charges for this patient.
The History tab is also available in the PCC EHR Payments tool:
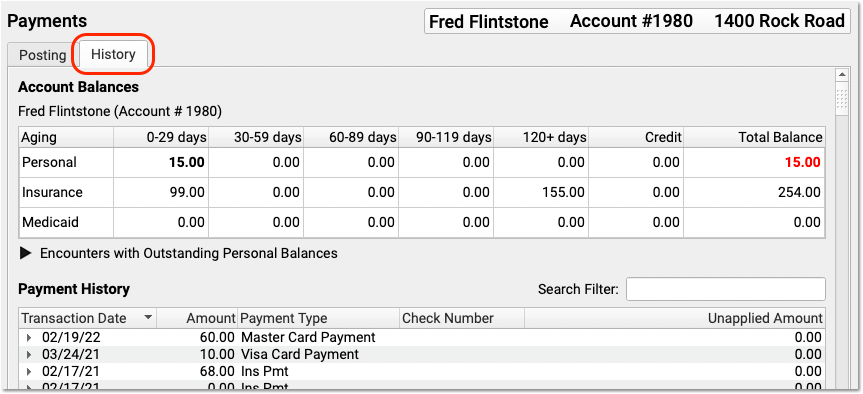
PCC EHR groups insurance payments and adjustments together, making it easier to review and work with payment history.
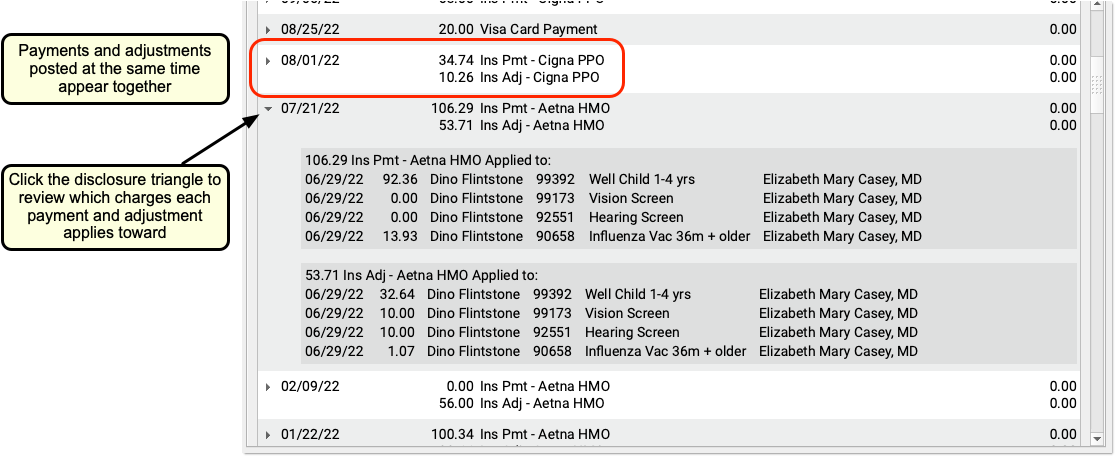
Note that if you unlink or delete parts of a payment or adjustment, the Payment History may display items on multiple lines.
Review An Encounter’s Payment History
You can review the history of all charges for an encounter in the Billing History section of a patient’s chart.
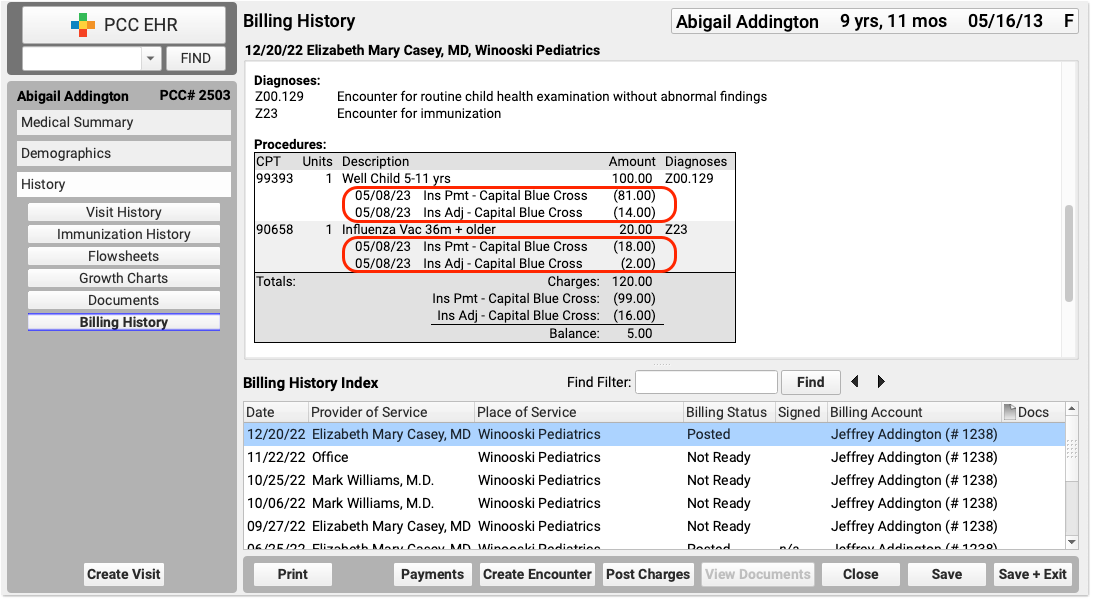
The encounter’s billing history includes more information about what diagnoses and procedures were posted and how claims were sent. For viewing and adjusting other claim history and claim information, use the Correct Mistakes (oops) program.
Review Insurance Payment Totals and Other Trends
PCC includes reports for reviewing what your practice posted, examining insurance reimbursement trends, and more. Visit your Practice Vitals Dashboard to get started, and contact PCC Support for help with specific reporting needs.
Edit Insurance Payments and Adjustments
When you need to edit an insurance payment or adjustment, select them in the Payment History and click “Edit”.
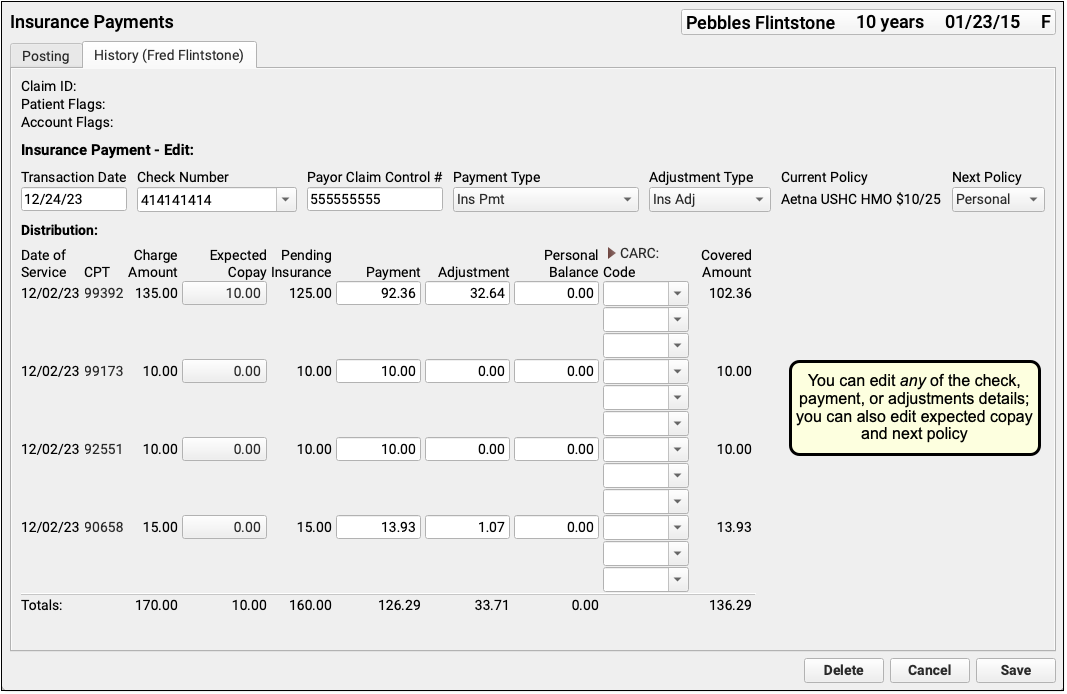
You can edit any aspect of the insurance payments and adjustments, including the transaction date and other payment information, amounts, and CARC information. You can also change the expected copay amount for a procedure. If you’ve learned the patient had another policy for the date of service, you can also update the Next Policy field to change the responsible party for the charges.
As you update payment amounts, PCC EHR will provide calculation support, filling out the adjustment and balance fields based on what you enter. You can edit and override those amounts.
You can click “Delete” to delete the entire payment and adjustment, removing them from the patient and account records.
When you have completed your edits, click “Save”. PCC will update the insurance payment and adjustment amounts, pend the charges to the next responsible party, queue up a claim if appropriate, and return you to the Payment History screen.

Back on the Payment History screen, you can review the changes you made and then use the buttons or the Posting tab to take additional action on the account.
Autopost Insurance Payments (Reference Manual)
The sections below contain additional reference information about using the Autopost program (autopip) to automatically post insurance payments and adjustments sent electronically to your practice from carriers.
ERA Select List (Screen Reference)
The ERA Select List screen in Autopost (autopip) displays incoming ERA checks. Your insurance carrier may send a single ERA detailing many claim responses and several different checks. PCC splits that information into individual check and then displays them in the order received.
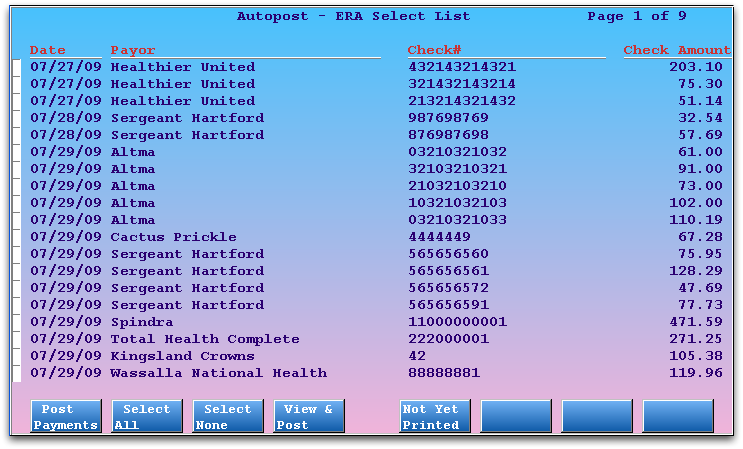
For each check, you can see the Date, Payor identity, Check Number (or payor reference number), and Check Amount.
You can select all or some of your incoming ERA checks and then press F1 – Process to begin posting. If you prefer to review the outcome of each check file individually, as you post, you can press F4 – Preview to post check-by-check while previewing the result. The F5 – Not Yet Printed key provides access to two tools for working with older and unposted claim responses.
F1 – Post Payments
F2 – Select All
F3 – Select None
F4 – Preview
F5 – Not Yet Printed
autopip determined may need additional attention and did not post. Since it is very important that a biller review (and possibly resubmit) these claims and remittance information, the Not Yet Printed screen can help insure that Manual reports are at least initially addressed. Press F5 – Not Yet Printed and then F7 – Daily View to visit the Daily View screen, a tool for reviewing a history of ERA Checks and autoposting activity.
F7 – Remove
autopip and press F7 to remove them. You can safely autopost all files, even those with errors, and autopip will drop them to the Manual report. You may wish to remove them pre-emptively, however, to avoid confusion. For example, you may already know that a set of files are a duplicate, or have already been posted. Mark the files that need to be removed and press F7. A confirmation screen will appear, asking you to press F1 to continue. The payment files will still be accessible later, in the erareports program.
Confirm Selection (Screen Reference)
After you select ERA checks on the ERA Select List screen in autopip and press F1 – Process, Autpost will display the Confirm Selection screen.
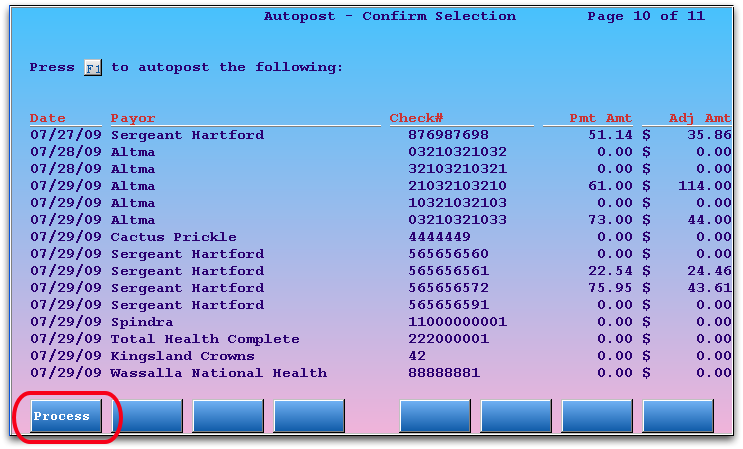
For each check, Autopost estimates the total Payment Amount and Adjustment Amount that autopip will post.
Press F1 – Process to confirm that you selected the correct checks and autopost the payments to the appropriate claims.
If you made an error in your selection, press F12 to return to the ERA Select List screen.
The Manual Post Report in autopip
If autopip can not post something that appears in any of the ERA check files, it will create a Manual Post report and ask you to review it on the Manual Post Report screen.
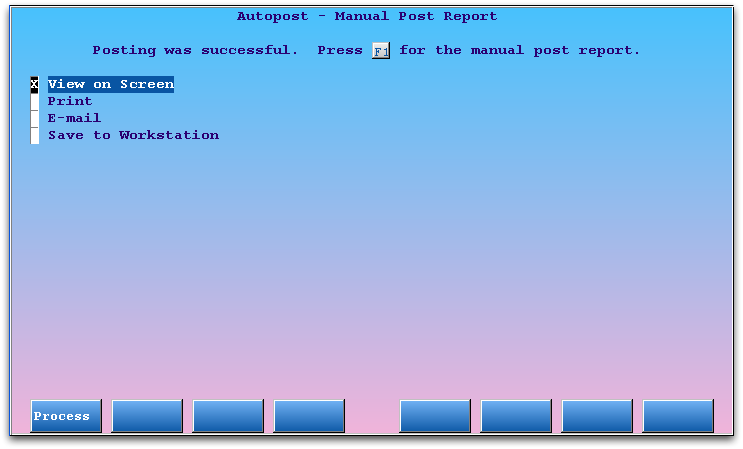
Press F1 – Process to take a quick look at the Manual report. Select Print, E-Mail, or Save to redirect the Manual report so you can work on each of the unposted items. If you do not make a selection at this time, you may retrieve the manual report later, on the Not Yet Printed screen or in erareports.
Why Do I Need to Print, E-Mail, or Save the Manual Reports?: ERAs may contain denials, reversals, and insurance interest payments. After autoposting finishes, any items in an ERA that autopip was unable to post are placed in a “Manual” report. A biller needs to review each Manual report and follow up on the included remittance information for the claims. In many cases, a biller needs to resubmit claims or post payments and adjustments in the Post Insurance Payments (pip) program.
The Manual Post report contains a complete record of the unposted payments and adjustments, including messages from the carrier or explanations of why the items could not be posted automatically.
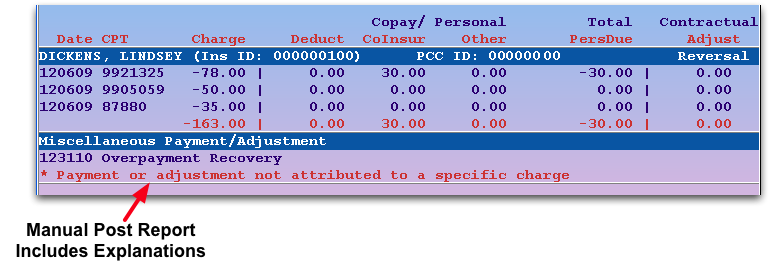
Specific explanations for each unposted item appear with asterisks (*), underneath the general description of the payment or adjustment message that was in the ERA.
Manual Report Reasons: What ERA Items Will Not Post Automatically?
PCC’s Autopost program will post ERA items that match charges in your system. If something can not be posted, it will appear on the Manual Report. From there, you can review details, post the adjudication manually, or take other appropriate actions.
What items, by default, will not post automatically? Inside the Manual Report, you can read the specific reason why each item was not posted. Below is a list of reasons that may appear on a manual report.
- Adjustment reason not configured for autoposting (Adjustment Reason: ________)
- PCC can configure which adjustment reasons should be allowed to post automatically and which should drop to the Manual Report.
- Charge amount listed did not match charge history (CPT #####)
- If the insurance carrier’s EOB lists a different charge amount than what appears on your PCC system records, the item will drop to the Manual Report for your review. You can compare your practice’s charges with what appeared on the EOB to better understand the discrepancy.
- Charge not pending insurance (CPT #####)
- If the EOB indicates an item that is not currently pending the insurance company, the item will drop to the Manual Report for your review. This may have happened because your practice changed the status of a charge after the claim was submitted.
- Claim ID did not match a PCC Claim ID
- PCC creates a unique claim ID number when it processes each claim. When insurance carriers respond, they use the same Claim ID number. When auto-posting, PCC attempts to match claim ID #s. If it can’t find a claim ID that matches, it will drop any other communication from the insurance carrier to the Manual Report.
- Claim ID not found in PCC’s charge history (######)
- If the insurance carrier returns a claim ID that does not match one in your PCC database, the item will drop to the Manual Report for your review.
- Claim total was negative
- Any claim with a negative total payment, such as an insurance take-back, will drop to the Manual Report.
- Claim was denied or had a status other than “Claim Processed”
- All denied claims are dropped to the Manual Report for your review.
- Copay listed did not match charge history (CPT #####)
- PCC double-checks the copay amount attached to the visit. If the amount reported by the carrier does not match the amount on the visit charge in your PCC system, the item will drop to the Manual Report.
- Procedure code (#####) not found in charge history for this claim (#####)
- PCC double-checks that the procedure codes indicated on the claim match the procedure codes on the account’s charge history. If there is a problem, the item drops to the Manual Report for your consideration. This could happen if a charge was deleted after a claim was sent.
- Patient Had Secondary Insurance
- If the patient has a secondary insurance (or medicaid), and your office has turned on the configuration that prevents posting for claims with a secondary responsible party, then the payments and adjustments will drop to the Manual Report and you will see this error.
- Payment or adjustment not attributed to a specific charge
- Any interest payments, overpayments, unusual adjustments, or other items that are not attached to a specific charge in your PCC system will drop to the Manual Report.
- Payment was less than the allowed amount (CPT #####)
- If you use PCC’s Contract Fee Schedules (allowables) features to enter the expected payment from an insurance carrier, and the payment in the EOB is less than the expected amount, the items will drop to the Manual Report for your review.
- Total of payments and adjustments was greater than the pending amount (CPT #####)
- If the total amount of all payments and adjustments is greater than the amount pending the insurance carrier, then the items will drop to the Manual Report for your review.
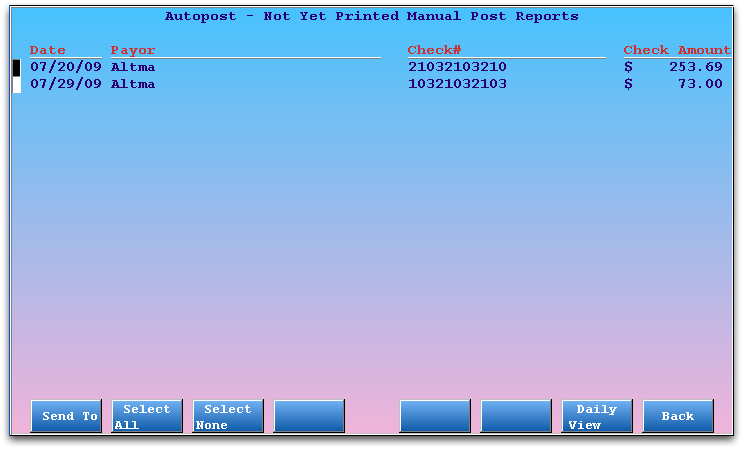
Not Yet Printed Manual Reports (Screen Reference)
The Not Yet Printed screen in autopip displays all Manual reports that have not been printed, e-mailed, or saved to a workstation.
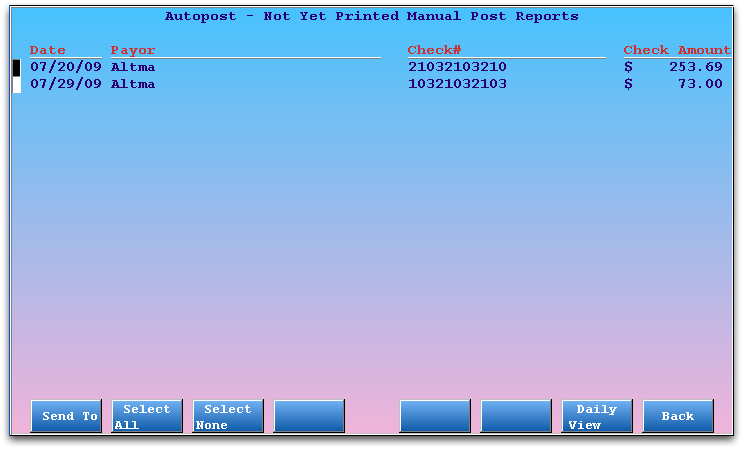
Select manual reports using the arrow keys and then press F1 – Send To to review, save, print, or e-mail them.
Press F7 – Daily View to see all daily Manual reports, including the date and user who printed, saved, or e-mailed them.
Why Do I Need to Print, E-Mail, or Save the Manual Reports?: ERAs may contain denials, reversals, and insurance interest payments. After autoposting finishes, any items in an ERA that autopip was unable to post are placed in a “Manual” report. A biller needs to review each Manual report and follow up on the included remittance information for the claims. In many cases, a biller needs to resubmit claims or post payments and adjustments in the Post Insurance Payments (pip) program.
Daily View (Screen Reference)
The autopip Daily View screen displays all incoming ERA check files for each day. You can use the screen to review autoposting activity by date.
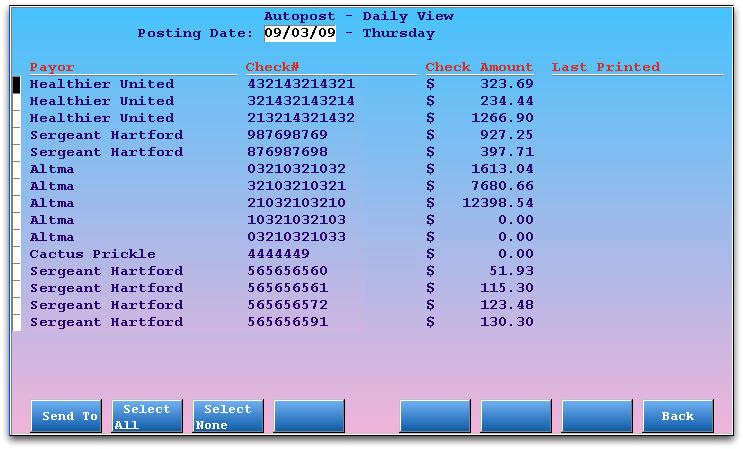
For each autoposted ERA check file, you can see the Payor, Check #, Check Amount, and the Last Printed date. Note that if you e-mail or save a copy of the check file, it will also be indicated in the “Last Printed” column.
Use the Daily View screen to find out who printed or otherwise took responsibility for each Manual Post report.
Press the right or left arrow keys to select a different day. If a check file had manual, unposted items, you can press F1 – Send To to print, save, or e-mail the details.
