How to Code for Immunizations and Administration
What codes should you use to bill for vaccines and immunization administration? Do you bill per-shot, or per-antigen within a single shot?
Immunizations are a major part of a pediatric practice’s overhead, and they have a huge impact on the health and well-being of patients and families. Your practice needs to bill for immunizations and immunization administration in the correct way in order to get paid fairly.
Read the notes below to learn how to code immunizations and immunization administration for billing.
Why is Immunization Billing Important?: On average, vaccines make up 22% of a practice’s incoming revenue. Depending on how you bill and how well payers pay, this revenue may not meet the expense of procuring, storing, and administering the vaccine. If a practice “breaks even” on the cost of a vaccine, they are in fact losing money. Your practice should adjust pricing and review proper coding to get paid properly from insurance payers.
Procedure Code Guidance: The procedure code recommendations in this article are intended only as examples. You should consult the AMA’s CPT Coding Guide and work with your insurance payers to verify what codes you should use on claims. Your practice updates and maintains your procedure list, codes, and prices in the Procedures table in the Table Editor on your PCC system.
Contents
- 1 Overview: What Codes Do I Use to Bill for an Immunization?
- 2 Should I Be Using the “With Counseling” Codes?
- 3 Get the Correct, Up-To-Date CPT
- 4 Examples of Immunization Billing
- 5 How Do I Post Immunization Administration?
- 6 Configure Your PCC System For Immunization Administration
- 7 Are Your Insurance Companies Properly Reimbursing?
- 8 Are Insurance Carriers Ready for the New Codes?
Overview: What Codes Do I Use to Bill for an Immunization?
When you bill an immunization procedure, such as a 90707 for an MMR, you should also bill one or more immunization administration codes.
For every immunization injection a patient receives, with counseling by a qualified medical professional, you should bill the correct immunization procedure code (90476-90749) and a single unit of 90460.
When a single shot immunizes against multiple diseases, such as in the case of MMR, DTaP, Comvax, Pentacel, or any other combination vaccine, you should bill an additional 90461 for each antigen.
The coding guidelines say that administration coding should reflect the number of diseases immunized against as well as the number of shots. The work and the responsibility of administering a vaccine is now measured by both the antigens and the supplies, personnel, and other expenses inherent to the task.
The January 2011 Change: In January of 2011, immunization administration CPT codes changed. The administration w/ counseling codes that pediatricians used previously (90465-90468) became invalid for billing. Two new codes (90460 and 90461) replaced them, and the replacement includes a change in the coding method, from per-shot to per-antigen. Before January 1st, 90465 and 90468 indicated immunization administrations with counseling.
Should I Be Using the “With Counseling” Codes?
If you provide and document immunization counseling and provide an opportunity for questions, then you should be billing administration codes that include counseling. Prior to 2011, counseling had to be by an M.D. to qualify, and was only applicable for certain ages. Now counseling can be by any medical professional and applies for all children under 19.
If you provide vaccines and do not talk to your patients about the immunizations, then you can use the codes without counseling: 90471-90474. This is unusual.
Check your CPT Coding Guide for more details.
Get the Correct, Up-To-Date CPT
The primary CPT codes for vaccines change over time. You should periodically review your immunization CPT codes. You can check the AAP’s Pediatric Vaccine Coding Table, or use another resource.
Examples of Immunization Billing
Immunization billing requires that you understand the immunization and its antigens.
If you administer a Rotavirus vaccine to a patient and provide counseling, you should bill 90680 for the immunization, followed by 90460 for the administration. If you administer an MMR, you should bill 90707, 90460, and two units of 90461. If you administer the new Pentacel vaccine, you should bill 90698, 90460, and four units of 90461.
Review the table below for more examples.
| Vaccine | Included Antigens | What to Bill (w/ Counseling) |
What to Bill (No Counseling) |
|---|---|---|---|
| Rotavirus |
|
|
|
|
Comvax |
|
|
|
| MMR |
|
|
|
| Pentacel |
|
|
|
| FluMist |
|
|
|
Intranasal and Other Non-Shots: As noted above, for all vaccines with counseling you can use the 90460 (and 90461 for each additional antigen) codes. For vaccines administered without counseling, you would use 90471 for an injection, with units of 90472 for other shots given during that visit. For intranasal or other vaccines administered without an injection, use 90473. If you gave more than one non-injection vaccine during the visit without counseling, you should use units of 90474.
How Do I Post Immunization Administration?
PCC’s Practice Management system, Partner, includes a fast text-based tool for entering diagnoses and procedures for billing.
When your biller enters charges, a typical 5 Year Well Visit might look like this:
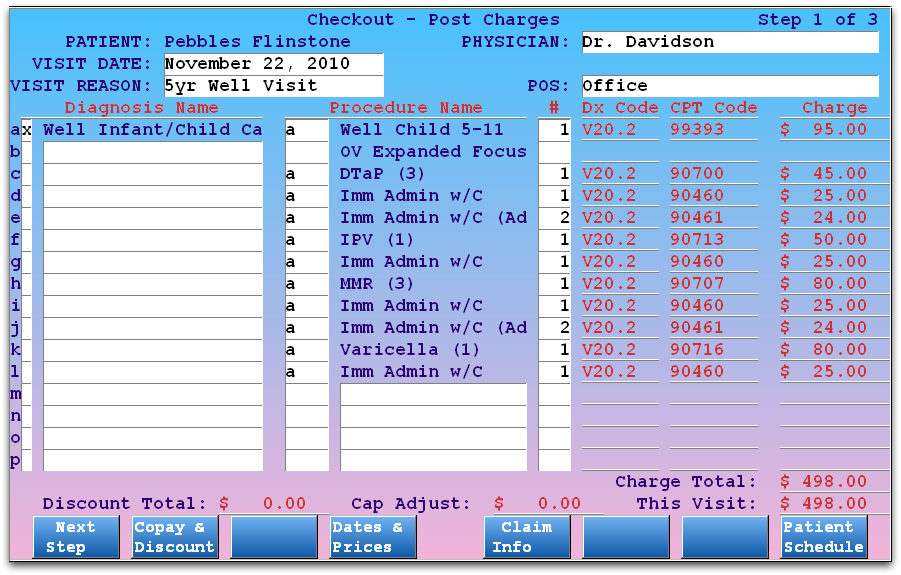
As described in the section above, each immunization receives both its own code, a 90460, and a total number of additional antigens for 90461. That means that for both DTaP and MMR, there are two units of 90461.
What About Units?: In the example above, the user is posting separate 90460 and 90461 charges for each immunization. That is the official suggestion of the AAP at the time of this documentation’s publication. If PCC discovers that insurance carriers will accept grouped units for all 90460 and 90461 procedures in a visit, the above screen would look more like this:
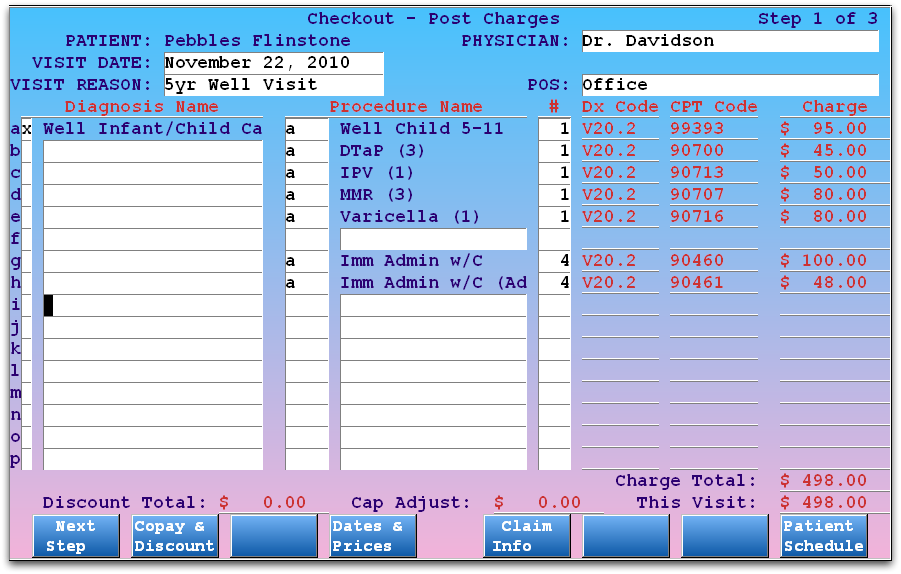
In the above example, units are grouped. Each immunization receives a 90460, and a total of four additional units of 90461 account for the additional antigens in DTaP and MMR.
Configure Your PCC System For Immunization Administration
PCC Support or your New Client Implementation specialist can help you set up your PCC system to properly bill immunizations and immunization administration. However, posting the different administration codes takes practice and over time you may need to update your procedure codes, adjust your charge screens, customize an encounter form, or adjust other tools to meet your practice’s workflow. Your billers and those who administer vaccines should understand how many additional antigens are represented in combination vaccines.
You can make a number of configuration changes in Practice Management that could help your practice implement correct immunization administration billing. Review the options below and contact PCC Support for help.
Want Help?: Contact PCC Support at support@pcc.com or 1-800-722-1082 for help configuring your immunization administration.
Adjust Codes in Your Procedure Table
Your practice’s immunization administration codes are located in your Procedures table. The two entries in ted would look something like this:
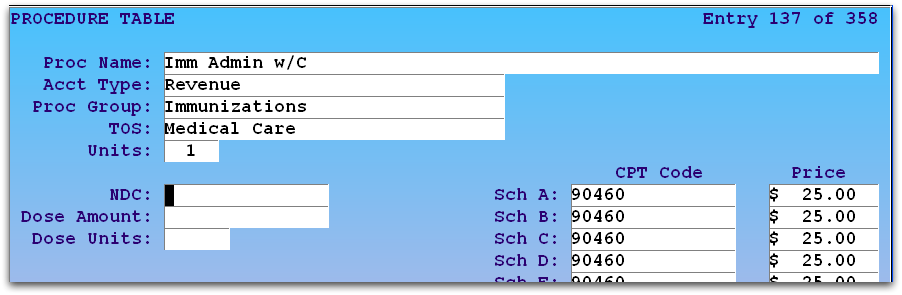
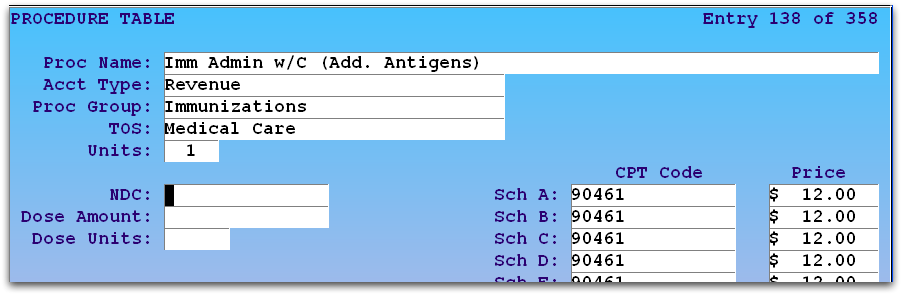
Your practice controls what codes and procedures you bill along with your prices, PCC does not update these for you. For information on using the Table Editor (ted), read Editing Partner Tables.
Do Not Overwrite Old Codes: When you create new table entries, you should not overwrite existing entries. Old codes are an important part of your billing history, and changing them can affect a patient’s billing record.
Pricing: You can look up Medicare values for 90460 and 90461, and PCC recommends that practices bill procedures based on a chosen percentage of Medicare reimbursement. The prices shown in the image above are only a sample and do not reflect pricing recommendations.
Optional: Add Antigen Indicator to Immunization Procedure Names
Whoever posts charges for a claim needs to add administration codes based on the number of antigens in a shot. Your provider might do the work themselves and note it on an encounter form, but your checkout staff or billers may also need to figure out the admin codes later, after the visit. To help them, you can edit your immunization names to indicate the total number of antigens.
Consult PCC Support: If you decide to change your procedure names, contact PCC Support (800-722-1082, support@pcc.com) and tell them about the change. We will check your immunization and charge screen configuration to ensure that immunizations will still track correctly to patient records.
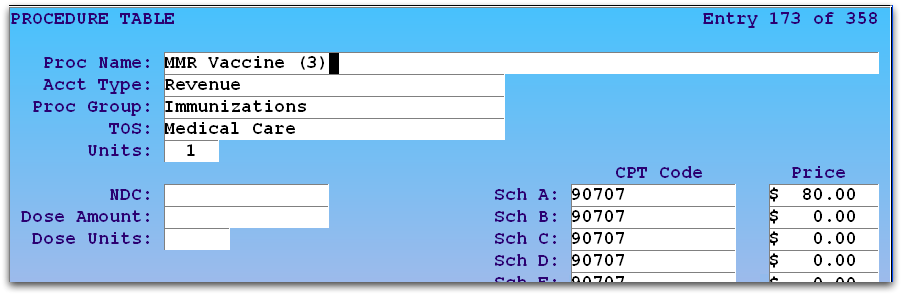
Run the Table Editor (ted), select the Procedures table, find an immunization, and add the number of antigens to the procedure name. For example, for an MMR vaccine, which would need a 90460 and two units of 90461, you might name your procedure “MMR (3)”.
For more information on using the table editor, read Editing Partner Tables.
Use Allowables to Make Flag Bad Payments
You can use PCC’s Contract Fee Schedule Editor to enter an expected reimbursement for any code. That way, if an insurance company reimburses $0.00, charges will not autopost and/or you will see the contract rate when you post the payments manually.
For more information, read the Contract Fee Schedule Editor help articles.
Are Your Insurance Companies Properly Reimbursing?
Immunizations are an important revenue source for pediatric offices, and PCC recommends you keep a close eye on administration code reimbursement. Insurance carriers make mistakes and require follow-up.
Allowables: Watch for the Expected Payment
If you set up contract fee schedules as mentioned above, then underpayments will be dropped to the Manual Post report during auto-posting of ERAs. When posting payments manually underpayments are visible while posting.
Insurance Reimbursement Analysis
You can run the Insurance Reimbursement Analysis report (ira) and display reimbursement for selected procedures (90460, 90461). That can show you any insurance group that is not properly reimbursing.
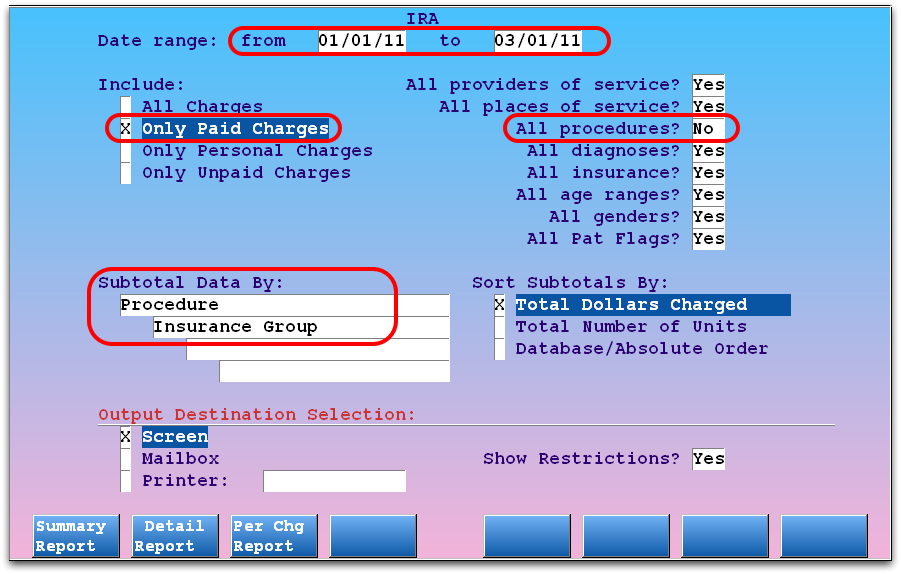
Contact PCC Support for help finding a report or creating a custom report to help you track problematic carriers.
